Abstract
While the relationship between albumin corrected calcium (ACC) levels and unfavourable outcomes has been previously investigated, existing studies have been limited in their specific application to patients undergoing maintenance hemodialysis (MHD) in intensive care unit (ICU). This retrospective cohort study aimed to explore the association between baseline ACC and 28-day in-hospital mortality in ICU patients undergoing MHD. Logistic regression model, smooth curve fitting, piecewise linear regression, subgroup analyses, and a series of sensitivity analyses were employed. Of the 2114 patients with a median age of 64 years, 290 (13.72%) died within 28 days after ICU admission. Multivariate regression analysis revealed that, in comparison with the lowest tertile, the highest tertile of ACC was associated with a higher mortality rate (OR 1.69, 95% CI 1.09–1.53, P = 0.0032). When the ACC levels were < 8.04 mg/dL, the mortality rate decreased with an adjusted OR of 0.44 (95% CI 0.20–0.98, P = 0.0438) for every 1 mg/dL increase in the ACC levels. When the ACC levels were ≥ 8.04 mg/dl, the mortality rate increased with an adjusted OR of 1.36 (95% CI 1.13–1.64, P = 0.0011) for every 1 mg/dl increase in the ACC levels. Non-linear relationship between ACC and 28-day in-hospital mortality were identified in patients undergoing MHD in the ICU. However, the findings of this study need to be confirmed through prospective studies.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is a major global health problem, with an estimated 697.5 million cases worldwide in 2017, representing a prevalence of 9.1%1. In China, the prevalence of CKD among adults was estimated to affect approximately 82 million individuals between 2018 and 20192. As CKD progresses to end-stage renal disease (ESRD), maintenance hemodialysis (MHD) becomes a critical treatment modality3,4,5. However, MHD is associated with multiple complications that increase the likelihood of hospitalization, intensive care unit (ICU) admission, and mortality6,7.
CKD-mineral and bone disorder (CKD-MBD) is a clinical syndrome characterized by laboratory abnormalities, vascular or soft tissue calcifications, and bone disease3. It is a prominent complication in patients undergoing MHD, significantly contributing to all-cause and cardiovascular mortality8,9,10. Among these abnormalities, elevated serum calcium levels have been linked to a higher risk of mortality in hemodialysis patients11,12. Albumin, the most abundant plasma protein, plays a crucial role in regulating calcium homeostasis13. In MHD patients, hypoproteinemia and acid–base disturbances are common, potentially leading to underestimation of uncorrected serum calcium levels14,15. When ionised calcium measurement is unavailable, ACC serves as an appropriate substitute16.
Several studies have demonstrated significant associations between ACC levels and disease severity or prognosis in conditions such as chronic obstructive pulmonary disease (COPD)17, diabetes mellitus18, diabetic kidney disease19, and ischemic stroke20. In ICU settings, ACC levels have been associated with a nonlinear relationship to the risk of all-cause mortality within 30 days21. For dialysis patients, elevated ACC levels are associated with increased risks of cardiovascular events, infections, and overall mortality12,22,23. A large cohort of patients with incident ESRD demonstrated a linear relationship between lower pre-ESRD ACC levels and greater post-ESRD survival, even at ACC concentrations below the normal range24.
Despite these findings, previous studies have primarily focused on the associations between ACC levels and outcomes in various diseases, ICU mortality in general populations, or long-term prognosis in ESRD or dialysis patients. However, there remains a significant gap in evidence regarding the relationship between ACC levels and short-term mortality specifically in MHD patients admitted to the ICU. Our study uniquely addresses this gap by exploring the association between ACC levels and 28-day mortality in this high-risk, specialized patient population. Artificial Intelligence models hold great potential for improving prediction accuracy and guiding clinical decision-making. Our study investigated the association between ACC levels and 28-day mortality, which may provide a basis for developing predictive models for high-risk populations in the future.
We hypothesized that elevated ACC levels are associated with an increased risk of 28-day in-hospital mortality in this patient population. In this retrospective, multicenter cohort study, we utilized the eICU Collaborative Research Database v2.0 (eICU-CRD v2.0) to (1) determine the prevalence and distribution of ACC abnormalities among ICU patients undergoing MHD in the United States and (2) investigate the relationship between ACC levels and 28-day in-hospital mortality in this cohort.
Methods
Data source
This multicenter retrospective cohort study utilized data from the eICU-CRD, which has been widely employed in observational research. The database contains medical records for 200,859 ICU patients from 335 ICUs across 208 U.S. hospitals, encompassing both academic and non-academic institutions, from 2014 to 2015. It comprises 31 tables with detailed information on demographics, medical history, vital signs, laboratory results, ICD-9-CM codes, and treatments25. The data are freely available after completing the Collaborative Institutional Training Initiative (CITI) program “Data or Specimens Only Research” and certification. All the data sources are deidentified, informed consent was waived from all patients and/or their legal guardians. The use of this database was approved by the institutional review board of Massachusetts Institute of Technology (Cambridge, MA), which approved this data collection and waived informed consent requirements. Two authors (Shili Zhao and Yue Xu) obtained the access (record IDs: 65166974 and 66676691). The authors are appreciative of the original study group for the provision of data for the present analysis. All methods were carried out in accordance with relevant guidelines and regulations. The study was conducted in accordance with the Declaration of Helsinki.
Study population
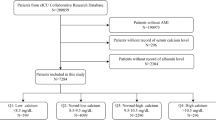
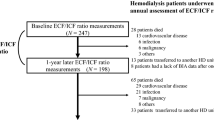
A total of 2114 eligible individuals were included after applying the following exclusion criteria: (1) non-first-time ICU admissions (n = 42,417); (2) no history of MHD (n = 153,107); (3) ICU stay < 24 h (n = 1492); (4) missing serum calcium or albumin data (n = 1603); (5) extreme Body Mass Index (BMI) values (> 50 kg/m2, n = 108); and (6) extreme ACC values (mean ± 3 SD, n = 18). ACC was calculated using the formula26: ACC (mg/dL) = serum calcium (mg/dL) + 0.8 × [4.0-serum albumin (g/dL)]. Ultimately, 2114 participants (954 men and 1160 women) were included. The study design and participant flowchart are illustrated in Fig. 1.
Variables
The primary exposure was the baseline ACC assessed within the first 24 h of ICU admission. Adjustments were made for the following covariates: (1) Demographics: age, gender, ethnicity, BMI, and hospital discharge year (2014 or 2015). (2) Comorbidities: congestive heart failure (CHF), diabetes, hepatic failure, cirrhosis, sepsis, immunosuppression, and metastatic cancer. (3) Vital Signs: temperature, respiratory rate, heart rate, and mean arterial pressure (MAP). (4) Laboratory Parameters: serum potassium, anion gap, total protein, albumin, blood urea nitrogen (BUN), serum creatinine, white blood cell count (WBC), red blood cell count (RBC), hemoglobin, and platelets. (5) Severity Scores: Acute Physiology and Chronic Health Evaluation IV (APACHE-IV) and Sequential Organ Failure Assessment (SOFA).
Baseline characteristics such as age, gender, ethnicity, weight, height, hospital discharge year, length of hospital stay and prognosis were collected from the patient table and apachePatientResult table. The physiological variables, including temperature (°C), respiratory rate, heart rate (HR) and MAP, were obtained from the apacheApsVar table and vitalAperiodic table. Laboratory indices, including serum calcium, albumin, potassium, BUN, creatinine, WBC, RBC, hemoglobin, and platelets, were extracted from the lab table. Comorbidities including CHF, diabetes, hepatic failure, cirrhosis, sepsis, immunosuppression, metastatic cancer and sepsis were extracted from the apachePredVar table and diagnosis table. Severity at admission was measured using the SOFA score and APACHE IV score, which were obtained from the apacheApsVar and apachePatientResult tables. We excluded data with extreme values, including BMI > 50 kg/m2 and ACC mean ± 3 SD.
Outcomes
The primary endpoint was 28-day in-hospital mortality.
Ethics statement
This study used data from the eICU-CRD under a data use agreement (record ID: 65166974 and 66676691) approved by the PhysioNet Review Committee. The database adheres to the Health Insurance Portability and Accountability Act (HIPAA) safe harbor provision. As the data were de-identified, local ethics committee approval was not required.
Statistical analysis
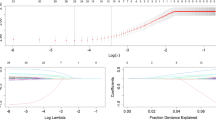
Patients were categorized into three groups based on baseline ACC levels: (1) Low (< 9.04 mg/dL, n = 704); (2) Middle (9.04–< 9.64 mg/dL, n = 690); (3) High (9.66–< 11.92 mg/dL, n = 720) (Table 1). Continuous variables were expressed as mean ± standard deviation (SD) or interquartile range (IQR) and compared using the Mann–Whitney U-test. Categorical variables were expressed as frequencies or percentages and compared using the Chi-squared test. Univariate analysis was performed to determine potential variables related to mortality (Table 2). The association between ACC levels and 28-day in-hospital mortality was assessed using a logistic regression model. Analyses were performed in three models: Crude model (no adjustments), Model I (adjusted for age, gender, hospital discharge year, and ethnicity), and Model II (adjusted for all potential confounders, including age, gender, hospital discharge year, ethnicity, BMI, CHF, diabetes, hepatic failure, metastatic cancer, sepsis, immunosuppression, SOFA, BUN, serum creatinine, albumin, and hemoglobin) (Table 3). ACC was also analyzed as a categorical variable, and subgroup analyses were conducted to explore interactions across various strata, including age, gender, BMI, ethnicity, CHF, diabetes, sepsis, phosphate, albumin, and SOFA scores (Fig. 2). We used a generalized additive model (GAM) to investigate the dose–response relationship between the ACC levels and mortality (Fig. 3). We then used a two-piece-wise linear regression model to examine the threshold effect of ACC levels on mortality (Table 4). The turning point for the ACC level was determined using “exploratory” analyses, which is to move the trial turning point along the pre-defined interval and pick up the one which gave maximum model likelihood. We also performed a log-likelihood ratio test and compared the one-line linear regression model with the two-piece-wise linear model, as described in the previous analysis21.
Effect size of albumin corrected calcium level and 28-day in-hospital mortality in different subgroups. Adjusted for hospital discharge year, Ethnicity, Immunosuppression, Blood urea nitrogen (mg/dL), and serum creatinine (mg/dL). CI, confidence interval; OR, odds ratio; BMI, body mass index; CHF, congestive heart failure; SOFA, Sequential Organ Failure Assessment.
Non-linear relationship between albumin corrected calcium levels and 28-day hospital mortality. Adjusted for age, gender, ethnicity, CHF, diabetes, BMI, hospital discharge year, hepatic failure, albumin, metastatic cancer, blood urea nitrogen, serum creatinine, hemoglobin, SOFA score, immunosuppression, and sepsis.
Sensitivity analysis involved adjusting for confounding factors across different subgroups to examine the relationship between ACC and mortality in various models (Table 3).
All analyses were conducted using R (http://www.R-project.org) and EmpowerStats (http://www.empowerstats.com). Statistical significance was defined as a two-sided P value < 0.05.
Results
Participants
A total of 2,114 participants were included in the study, with 290 deaths observed during the follow-up period (Fig. 1). The median age of participants was 64 years (IQR: 55–73), and 54.5% (n = 1,160) were female. Table 1 summarizes patient demographics, vital signs, laboratory results, and comorbidities across tertiles of ACC levels. Patients in the highest tertile were generally older and exhibited lower MAP, albumin, and serum creatinine levels, while showing higher WBC and platelet counts compared to those in the lowest tertile.
Of the total cohort, missing values for covariates included: ethnicity (13, 0.61%), comorbidities (27, 1.28%), heart rate (27, 1.28%), MAP (28, 1.32%), respiratory rate (33, 1.56%), temperature (143, 6.76%), serum potassium (3, 0.14%), BUN (1, 0.05%), serum creatinine (5, 0.24%), WBC (62, 2.93%), RBC (62, 2.93%), hemoglobin (51, 2.41%), platelets (73, 3.45%), and APACHE-IV score (257, 12.15%).
28-Day In-Hospital Mortality
The overall 28-day in-hospital mortality rate was 14.52% (290/2114). Stratified by ACC tertiles, mortality rates were 10.37%, 13.91%, and 16.81% for the lowest, middle, and highest tertiles, respectively (Table 1).
Unadjusted association between baseline variables and 28-day mortality
Univariate analysis identified multiple factors that were significantly associated with 28-day mortality (Table 2). The mean ACC was 9.36 ± 0.82 mg/dL. Increased mortality was observed with rising calcium levels: middle tertile (OR 1.40, 95% CI 1.01–1.93, P = 0.0433) and high tertile (OR 1.75, 95% CI 1.28–2.38, P = 0.0004). Advanced age was a strong independent risk factor (OR 2.17, 95% CI 1.56–3.02, P < 0.0001). Additional significant risk factors included elevated heart rate (OR 2.10, 95% CI 1.54–2.87, P < 0.0001), infection (OR 1.71, 95% CI 1.31–2.23, P < 0.0001), and high APACHE-IV (OR 8.83, P < 0.0001) and SOFA (OR 5.84, P < 0.0001) scores.
Relationship Between ACC and 28-day in-hospital mortality in different models.
Multivariable models confirmed the association between ACC levels and mortality risk (Table 3). In the unadjusted model, each unit increase in ACC was associated with higher mortality risk (OR 1.27, 95% CI 1.09–1.48, P = 0.0024). This relationship persisted after adjusting for confounders (Adjusted Model I: OR 1.29, 95% CI 1.10–1.51, P = 0.0020; Adjusted Model II: OR 1.24, 95% CI 1.05–1.47, P = 0.0129).
Stratified analysis revealed significantly increased mortality risk in the high-calcium group. In Model II, the high-calcium tertile had an OR of 1.69 (95% CI 1.09–2.53, P = 0.0032). Elevated ACC levels were significantly associated with 28-day in-hospital mortality, and the results remain robust after adjusting for multiple confounders.
Subgroup analyses of the relationship between ACC and 28-day mortality
Subgroup analyses evaluated the modifying effects of demographic and clinical variables on the relationship between ACC levels and mortality (Fig. 2). Age emerged as a significant effect modifier (P-interaction = 0.0239). Among younger patients (< 65 years), higher calcium levels significantly increased mortality risk (OR 1.49, 95% CI 1.17–1.89, P = 0.0013), whereas no significant association was observed in older patients (≥ 65 years, OR 1.03, 95% CI 0.83–1.27, P = 0.8149). Male patients showed a modestly elevated risk (OR 1.27, 95% CI 1.00–1.62, P = 0.0477). Patients without CHF (OR 1.26, P = 0.0070) or diabetes (OR 1.30, P = 0.0119) had significantly increased risks. Elevated mortality risk was also noted in patients with sepsis (OR 1.40, P = 0.0126), low albumin (OR 1.37, P = 0.0171), and low phosphate levels (OR 1.48, P = 0.0317). The results indicated that younger age, male gender, middle BMI, absence of chronic comorbidities, low albumin level, and lower disease severity were associated with a stronger effect. This underscores the importance of individualized risk assessments in clinical practice.
Nonlinear relationship between ACC and 28-day mortality
We observed a nonlinear dose–response relationship between ACC and mortality (Fig. 3 and Table 4). Using the GAM, a nonlinear association between the ACC and 28-day mortality was detected (Table 4). The linear regression model and a two-piece-wise linear regression model were compared, and the P value of the log-likelihood ratio test was 0.020. This result indicates that a two-piece-wise linear regression model would be more appropriate to characterize the relationship.
When the ACC levels were < 8.04 mg/dL, the mortality rate decreased with an adjusted OR of 0.44 (95% CI 0.20–0.98, P = 0.0438) for every 1 mg/dL increase in the ACC. When the ACC levels were ≥ 8.04 mg/dL, the effect size was 1.36 (95% CI 1.13–1.64, P = 0.0011), and the risk of 28-day in-hospital mortality increased by 36% for every 1 mg/dL increase in the ACC level.
A dose–response relationship was observed, with distinct patterns based on age (Supplementary Figure 1). In younger patients, a linear relationship was more appropriate (P = 0.121), while in older patients, a piecewise linear model was more suitable (P = 0.020) (Supplementary Table 1).
Discussion
This multicenter retrospective cohort study of 2,114 MHD patients admitted to the ICU revealed a significant and intricate association between ACC levels and 28-day in-hospital mortality. We also clarified the association between ACC and 28-day in-hospital mortality. The risk of 28-day in-hospital mortality increased by 43% in the 9.06–9.64 mg/dl subgroup and 69% in the 9.66–11.92 mg/dl subgroup when the ACC increased by 1 mg/dl after adjustment. The major finding was that the association between the ACC level and the risk of all-cause mortality was non-linear, and the risk was highest in those with very low or very high ACC levels. After a series of sensitivity analyses, stability existed in this relationship. These findings underscore the critical importance of precise calcium management in MHD patients. To our knowledge, this is the first study to report an association between ACC and 28-day mortality in this patient population.
Serum calcium levels have been associated with both morbidity and mortality in the general healthy population as well as in various diseases. ACC exhibited a U-shaped relationship with all-cause and cardiovascular mortality rates in the general healthy population27. A meta-analysis of eight cohort studies involving 89,165 participants demonstrated a 16% increased diabetes risk per 1 mg/dL rise in ACC18. Similarly, a cross-sectional study of 3,016 type 2 diabetes patients found a 0.1 mmol/L increase in ACC associated with a 44% higher risk of diabetic nephropathy19. For instance, a retrospective study of 11,446 acute myocardial infarction patients reported that ACC levels below 9.12 mg/dL or above 9.86 mg/dL independently predicted increased in-hospital mortality28.
ACC levels were also strongly associated with clinical outcomes in critically ill patients. A multicenter retrospective cohort study of 102,245 ICU patients identified a U-shaped relationship between ACC and 30-day in-hospital mortality, with an inflection point at 8.9 mg/dL. Each 1 mg/dL increase below this threshold reduced mortality risk by 10%, while increased above this threshold heightened risk by 10%21. A five-year retrospective study of 129,076 dialysis patients, including 10,066 on peritoneal dialysis and 119,010 on hemodialysis, revealed that ACC ≥ 10.2 mg/dL was linked to increased mortality risk, regardless of dialysis modality11. However, our study population, consisting of ICU-admitted MHD patients, represented a sicker cohort with a focus on short-term outcomes. Using GAM, we explored the nonlinear relationship between ACC and mortality. Notably, our findings align with those of a multicenter retrospective cohort study of 2,869 MHD patients, which identified elevated ACC levels as significantly associated with infection-related and all-cause mortality12. While both studies demonstrated increased mortality risks with high ACC levels, our study introduced additional insights, including age-specific variations, threshold effects, and short-term prognostic implications. Moreover, our analysis incorporated detailed clinical and laboratory data from the eICU database to account for potential confounders.
The observed association between elevated ACC levels and poor prognosis in ICU-admitted MHD patients may be explained by several mechanisms. Elevated calcium levels increase intracellular calcium concentrations, disrupt adherens junctions, induce reactive oxygen species (ROS) release, heighten endothelial permeability, and cause dysfunction29,30. Additionally, serum calcium stimulates vascular smooth muscle cells to produce pro-calcific factors, accelerating vascular calcification under pathological conditions31. Abnormal calcium concentrations impair neutrophil function, reducing immunity and increasing infection susceptibility32. Calcium dysregulation may also contribute to cardiac arrhythmias. These mechanisms collectively suggest that abnormal serum calcium exacerbates endothelial dysfunction, vascular calcification, immune suppression, and cardiac complications, culminating in increased mortality risk.
Strengths
This study’s strengths lie in its rigorous design and innovative analytical approach. First, we utilized the eICU-CRD database, a large multicenter dataset encompassing 335 ICUs, 200,859 patients, and 208 hospitals, ensuring broad representativeness and external validity. Second, advanced statistical methods, including GAM and segmented regression models, allowed for nuanced exploration of the nonlinear relationship between ACC and mortality. Third, subgroup analyses, particularly those stratified by age, shed light on age-specific interactions, offering valuable insights into personalized medicine. Finally, comprehensive adjustments for confounders such as demographics, comorbidities, inflammatory markers, and organ function scores enhanced the internal validity of the study.
Limitations
Despite its strengths, this study has limitations. First, the study population, derived from the eICU-CRD database, was limited to U.S. MHD patients, potentially restricting generalizability to other populations. Second, as an observational study, we acknowledge the limitations in establishing causal relationships. Third, unmeasured confounders, such as unrecorded clinical parameters or lifestyle factors, may have influenced the results. Fourth, the inability to differentiate specific causes of death hindered deeper exploration of mortality drivers. Finally, the lack of long-term follow-up data precluded assessment of ACC’s impact on extended prognosis.
Future research directions
The observational study identified that ACC levels may be significantly relevant to short-term prognosis in ICU patients undergoing MHD. Although our findings do not provide direct clinical guidance, they suggest that clinicians need to pay attention to ACC levels in this patient group. When considering calcium supplementation or adjusting the calcium concentration in dialysate, clinicians can refer to these findings to optimize patients’ACC levels. However, further prospective studies are necessary to validate these associations and explore the potential benefits of targeted interventions. Recent advancements in artificial intelligence and machine learning have significantly enhanced predictive accuracy across various healthcare applications. Specifically, advanced optimization techniques, such as hybridized gradient boosting and optimized neural networks, have been widely applied to enhance model performance and improve outcome prediction33,34,35. Future research could incorporate such AI-based models, which may help improve risk stratification and provide opportunities for early intervention.
Conclusions
This study utilized data from the eICU-CRD database to identify a dose–response relationship between ACC levels and 28-day in-hospital mortality among ICU patients undergoing MHD. A total of 2,114 patients were included in the analysis. After adjusting for confounding factors, each 1 mg/dL increase in ACC is associated with an approximately 24%-29% increase in the risk of 28-day mortality. Additionally, the association between ACC levels and 28-day mortality risk was nonlinear, with a turning point at 8.04 mg/dL. Given the significant impact of ACC on short-term outcomes, clinicians should pay much more attention and give priority to ACC management in ICU patients undergoing MHD. Further investigation into the underlying mechanisms linking elevated ACC to mortality could provide new therapeutic targets for improving outcomes in this vulnerable patient group.
Data availability
The datasets analyzed during the study are available in the eICU Collaborative Research Database (https://eicu-crd.mit.edu/).
References
GBD Chronic Kidney Disease Collaboration &. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 395, 709–733 (2020).
Wang, L. et al. Prevalence of chronic kidney disease in China: Results from the sixth china chronic disease and risk factor surveillance. JAMA Intern. Med. 183, 298–310 (2023).
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 105, S117-S314 (2024).
Flythe, J. E. & Watnick, S. Dialysis for chronic kidney failure: A review. JAMA 332, 1559–1573 (2024).
Chen, T. K., Knicely, D. H. & Grams, M. E. Chronic kidney disease diagnosis and management: A review. JAMA 322, 1294–1304 (2019).
Lambourg, E. et al. Incidence and outcomes of patients receiving chronic kidney replacement therapy admitted to Scottish ICUs between 2009 and 2019-A National Observational Cohort Study. Crit Care Med. 51, 69–79 (2023).
Flythe, J. E. et al. Characteristics and outcomes of individuals with pre-existing kidney disease and COVID-19 admitted to intensive care units in the United States. Am. J. Kidney Dis. 77, 190-203.e1 (2021).
Naves-Díaz, M. et al. Calcium, phosphorus, PTH and death rates in a large sample of dialysis patients from Latin America. The CORES Study. Nephrol. Dial. Transplant. 26, 1938–1947 (2011).
Tentori, F. et al. Mortality risk for dialysis patients with different levels of serum calcium, phosphorus, and PTH: The Dialysis Outcomes and Practice Patterns Study (DOPPS). Am. J. Kidney Dis. 52, 519–530 (2008).
Fernández-Martín, J. L. et al. Improvement of mineral and bone metabolism markers is associated with better survival in haemodialysis patients: The COSMOS study. Nephrol. Dial Transplant. 30, 1542–1551 (2015).
Rivara, M. B. et al. Uncorrected and albumin-corrected calcium, phosphorus, and mortality in patients undergoing maintenance dialysis. J. Am. Soc. Nephrol. 26, 1671–1681 (2015).
Yamada, S. et al. Increased risk of infection-related and all-cause death in hypercalcemic patients receiving hemodialysis: The Q-Cohort Study. Sci. Rep. 10, 6327 (2020).
Fanali, G. et al. Human serum albumin: from bench to bedside. Mol. Aspects Med. 33, 209–290 (2012).
Shrimanker, I. & Bhattarai, S. StatPearls. In: Treasure Island (FL): 2025
Kalantar-Zadeh, K., Ikizler, T. A., Block, G., Avram, M. M. & Kopple, J. D. Malnutrition-inflammation complex syndrome in dialysis patients: causes and consequences. Am. J. Kidney Dis. 42, 864–881 (2003).
Aberegg, S. K. Ionized calcium in the ICU: Should it be measured and corrected. Chest 149, 846–855 (2016).
Wan, X. et al. Association of serum calcium with the risk of chronic obstructive pulmonary disease: A prospective study from UK Biobank. Nutrients 15, 3439 (2023).
Zhu, J. et al. Circulating calcium levels and the risk of type 2 diabetes: A systematic review and meta-analysis. Br. J. Nutr. 122, 376–387 (2019).
Yu, Q. et al. Association of serum calcium levels with diabetic kidney disease in normocalcemic type 2 diabetes patients: a cross-sectional study. Sci. Rep. 14, 21513 (2024).
Wu, C. et al. Association between serum calcium and prognosis in patients with acute ischemic stroke in ICU: analysis of the MIMIC-IV database. BMC Anesthesiol. 24, 139 (2024).
Qin, X. et al. Non-linear relationship between albumin-corrected calcium and 30-day in-hospital mortality in ICU patients: A multicenter retrospective cohort study. Front Endocrinol. Lausanne 13, 1059201 (2022).
Lin, Y. C. et al. Effect modifying role of serum calcium on mortality-predictability of PTH and alkaline phosphatase in hemodialysis patients: An investigation using data from the Taiwan renal registry data system from 2005 to 2012. PLoS ONE 10, e0129737 (2015).
Kimata, N. et al. Association of mineral metabolism factors with all-cause and cardiovascular mortality in hemodialysis patients: The Japan dialysis outcomes and practice patterns study. Hemodial. Int. 11, 340–348 (2007).
Obi, Y. et al. Association of pre-ESRD serum calcium with post-ESRD mortality among incident ESRD patients: A cohort study. J. Bone Miner. Res. 33, 1027–1036 (2018).
Pollard, T. J. et al. The eICU Collaborative Research Database, a freely available multi-center database for critical care research. Sci. Data 5, 180178 (2018).
Payne, R. B., Little, A. J., Williams, R. B. & Milner, J. R. Interpretation of serum calcium in patients with abnormal serum proteins. Br. Med. J. 4, 643–646 (1973).
Yang, M. et al. Serum calcium concentrations and risk of all-cause and cause-specific mortality: Results from 2 prospective cohorts. J. Clin. Endocrinol. Metab. 108, e527–e535 (2023).
Shiyovich, A., Plakht, Y. & Gilutz, H. Serum calcium levels independently predict in-hospital mortality in patients with acute myocardial infarction. Nutr. Metab. Cardiovasc. Dis. 28, 510–516 (2018).
Dalal, P. J., Muller, W. A. & Sullivan, D. P. Endothelial cell calcium signaling during barrier function and inflammation. Am. J. Pathol. 190, 535–542 (2020).
Gandhirajan, R. K. et al. Blockade of NOX2 and STIM1 signaling limits lipopolysaccharide-induced vascular inflammation. J. Clin. Invest. 123, 887–902 (2013).
Buendía, P. et al. Endothelial microparticles mediate inflammation-induced vascular calcification. FASEB J. 29, 173–181 (2015).
Reid, I. R., Gamble, G. D. & Bolland, M. J. Circulating calcium concentrations, vascular disease and mortality: a systematic review. J. Intern. Med. 279, 524–540 (2016).
Ouadi, B. et al. Optimizing silt density index prediction in water treatment systems using pressure-based gradient boosting hybridized with Salp Swarm Algorithm. J. Water Process Eng. 68, 106479 (2024).
Khatir, A., Capozucca, R., Khatir, S., Magagnini, E. & Cuong-Le, T. Enhancing damage detection using reptile search algorithm-optimized neural network and frequency response function. J. Vib. Eng. Technol. 13, 88 (2025).
Khatir, A. et al. Advancing structural integrity prediction with optimized neural network and vibration analysis. J. Struct. Integrity Maint. 9, 2390258 (2024).
Acknowledgements
We thank the eICU Collaborative Research Database for providing data and extend our gratitude to all study participants.
Funding
Beijing Administration of Traditional Chinese Medicine Project (No.2023BJSZDYNJBXTGG-008); Beijing Hospital Authority Cultivation Plan (No. PX2022042).
Author information
Authors and Affiliations
Contributions
S.L.Z conceived and designed the research. Y.X. cleaned the data. S.L.Z and S.J.Z performed statistical analysis. Q.H.Z and H.R.D prepared figures. S.L.Z. drafted the manuscript. H.L.R and B.L.L made critical revision of the manuscript for key intellectual content. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, S., Zhao, Q., Xu, Y. et al. The association between albumin corrected calcium levels and mortality in ICU patients undergoing maintenance hemodialysis. Sci Rep 15, 12086 (2025). https://doi.org/10.1038/s41598-025-96454-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-96454-0