Abstract
Liver cancer remains a significant public health issue in China, exhibiting high incidence, mortality, and burden. Understanding its temporal trends and projections is essential for designing targeted prevention and treatment strategies. This study analyzes long-term trends in liver cancer incidence, prevalence, mortality, and burden from 1990 to 2021, assessing age, period, and cohort effects, and projecting future trends. Data on liver cancer incidence, prevalence, mortality, disability-adjusted life years (DALYs), years lived with disability (YLDs), and years of life lost (YLLs) were analyzed from 1990 to 2021. Joinpoint regression analysis, age-period-cohort (APC) analysis, and BAPC modeling were applied to examine trends and project future trends. Decomposition analysis examined contributions of aging, epidemiological changes, and population growth. The study also compared China’s liver cancer trends with global data. From 1990 to 2021, China experienced a decrease in age-standardized rates for liver cancer incidence, prevalence, mortality, and burden. Notably, Age-standardized incidence rates (ASIR) exhibited a decline after 2016, with a significant reduction in the male population. In 2021, there were 196,637 new cases of liver cancer in China, with a higher burden in males. ASIR were 14.34 per 100,000 for males and 4.89 per 100,000 for females. Mortality also followed a declining trend, with a notable decrease in age-standardized mortality rates. The age-standardized mortality rate (ASMR) for males was 12.4 per 100,000, significantly higher than for females (4.57 per 100,000) in 2021. Additionally, the age-standardized prevalence rate (ASPR) was 20.0 for males and 6.64 for females, with 265,539 total cases. The burden, measured by DALYs, YLDs, and YLLs, also showed a notable decline in age-standardized rates and significant gender disparities. Despite this, the absolute number of cases, deaths, and DALYs has continued to rise due to population growth and aging, with males bearing a significantly higher burden than females. The study also highlights the impact of aging, population growth, and epidemiological changes on liver cancer incidence and mortality in China. Projections for 2030 suggest a continued decrease in liver cancer incidence, especially among females, reflecting the effectiveness of public health interventions and medical advancements. However, gender disparities remain significant, and further efforts are needed to reduce the overall liver cancer burden, with an emphasis on early detection and prevention strategies.
Similar content being viewed by others
Introduction
Liver cancer, particularly hepatocellular carcinoma (HCC), is a major global health burden, ranking as the sixth most commonly diagnosed cancer and the third leading cause of cancer-related deaths worldwide1. In 2022, an estimated 865,269 people were diagnosed with liver cancer, and 757,948 deaths were attributed to it1. The highest incidence and mortality rates are observed in East Asia, particularly China, which alone accounts for nearly half of the global cases2. The primary risk factors for liver cancer include chronic infections with hepatitis B virus (HBV) and hepatitis C virus (HCV), excessive alcohol consumption, aflatoxin exposure, and metabolic disorders such as obesity and diabetes3. The epidemiology of liver cancer in China has shown significant changes over recent decades, influenced by public health interventions and socio-economic developments. The implementation of the universal HBV vaccination program in the early 1990s, integrated into the national immunization schedule by 2002, has led to a marked reduction in HBV prevalence among younger populations4. Additionally, efforts to control aflatoxin contamination in food and reduce alcohol consumption have contributed to the observed trends5. Despite these measures, liver cancer remains a prominent health issue in China, with substantial regional disparities in incidence and mortality rates, particularly affecting rural and less-developed areas6.
Epidemiological studies reveal evolving trends in cancer mortality across different regions. An analysis of gastrointestinal cancer mortality in Babol, North Iran, from 2013 to 2021 reported a rising trend in both crude and age-standardized mortality rates7. Notably, while mortality from small intestine cancer declined, significant increases were observed in colon, pancreatic, and gallbladder cancers, emphasizing the critical need for enhanced screening and prevention measures. Another study utilizing joinpoint regression projected a 6.43% rise in cancer-related deaths over the next five years, further underscoring the necessity for improved healthcare services and targeted interventions8. Conversely, liver cancer mortality in China has shown a downward trend. Between 2000 and 2014, incidence and mortality declined annually by 2.3% and 2.6%, respectively6. Despite these advancements, liver cancer remains a major public health concern, particularly in rural and western regions, where disparities persist. This highlights the need for region-specific prevention strategies to further mitigate the disease burden.
This study aims to provide a comprehensive analysis of the long-term trends in liver cancer burden in China from 1990 to 2021, utilizing data from the Global Burden of Disease (GBD) Study 2021. We employed joinpoint regression and age-period-cohort (APC) analysis to examine temporal trends and the influence of demographic factors on liver cancer incidence, prevalence, mortality, disability-adjusted life years (DALYs), years lived with disability (YLDs), and years of life lost (YLLs) for liver cancer. The findings from this research will offer valuable insights into the current state of liver cancer in China and support the development of targeted public health strategies to mitigate its impact.
Methods
Data sources
This study is a population-based epidemiological study that utilized data from the GBD study 2021, which provides comprehensive estimates of global health metrics, including incidence, prevalence, mortality, DALYs, YLDs, and YLLs for liver cancer. The GBD study compiles data from multiple sources, including national health registries, cancer surveillance programs, hospital records, and published literature, ensuring a standardized approach to estimating disease burden. However, in regions with incomplete or missing data, statistical modeling is used to generate estimates, incorporating covariates and data from comparable locations. The GBD study employs a Bayesian hierarchical modeling framework to estimate disease burden across populations, adjusting for uncertainty using uncertainty intervals (UIs)9. The age-standardized rates (ASR) are calculated using the World Health Organization’s World Standard Population, allowing for comparability across different regions and time periods. The chosen study period (1990–2021) enables a long-term assessment of liver cancer trends, capturing the effects of major public health interventions such as the introduction of HBV vaccination programs, improved screening, and advancements in antiviral therapies. Liver cancer in the GBD study is defined as “Malignant neoplasms of the liver”, corresponding to ICD-10 codes C22.0 to C22.8 and a proportion of C22.9 reflecting primary liver cancer. Data were accessed through the Global Health Data Exchange (GHDx) query tool, which allows for detailed extraction of disease-specific metrics stratified by age, sex, and geographical location.
Statistical analysis
Joinpoint regression analysis
Joinpoint regression analysis was conducted to identify significant changes in the trends of age-standardized rates of liver cancer incidence, prevalence, mortality, DALYs, YLDs, and YLLs from 1990 to 2021. The Joinpoint Regression Program (Version 5.2.0, National Cancer Institute, Bethesda, MD, USA) was used for this analysis. This method involves fitting a series of joined straight lines on a log scale to the trends, identifying points (joinpoints) where a significant change in the trend occurs. The analysis allows for up to three joinpoints to capture potential changes in trend patterns over the study period. The annual percentage change for each segment between joinpoints was calculated, and the statistical significance of these changes was assessed using the Monte Carlo permutation method, which provides robust estimates of trend changes and their significance10,11.
Age-period-cohort (APC) analysis
APC analysis was performed to assess the individual effects of age, time period, and birth cohort on NPC incidence, prevalence, and DALYs rates. This approach enables the independent evaluation of how each factor influences the observed trends. To address the collinearity issue inherent in APC models, we used the intrinsic estimator (IE) method, which provided more accurate estimates of the effects for age, period, and cohort12,13. For this analysis, we retrieved data from the GBD database, focusing on incidence and mortality figures by five-year age groups from 1990 to 2021, along with corresponding annual population estimates. Individuals aged under 5 and over 95 were grouped together, while age intervals were defined as 0–4, 5–9, 10–14, etc., with the "0" category representing the under-five group. Cumulative incidence and mortality rates for each age group were calculated over five-year periods (1992–1996, 1997–2001, and so on). The Epi package (version 2.46) in R (version 4.3.1) was employed to fit the APC model, and we compared residual deviations and Akaike Information Criterion (AIC) values to determine the optimal model.
Bayesian age-period-cohort (BAPC) analysis
To project future trends in liver cancer incidence up to 2030, a BAPC analysis was employed. The BAPC method combines Bayesian inference with APC modeling, allowing for probabilistic projections and incorporating prior information. The analysis was conducted using the R package “BAPC” package in R (version 0.0.36), which utilizes Markov Chain Monte Carlo (MCMC) simulations to generate projections and quantify uncertainty. This method provides a comprehensive framework for understanding future trends and the potential impact of interventions. To evaluate the robustness of the BAPC analysis, sensitivity analyses were performed to assess the impact of different prior distributions and model assumptions. The results were also compared across various model specifications, and uncertainty intervals (UIs) were considered to account for variability in the projections. This method provides a comprehensive framework for understanding future trends and the potential impact of interventions14,15.
Decomposition analysis
Decomposition analysis was performed to quantify the contributions of aging, epidemiological changes, and population growth to observed changes in liver cancer incidence and mortality. This method decomposes the total change into components attributable to each factor, providing insights into the underlying drivers of these trends. The analysis followed the standard demographic techniques described by Preston et al.16, which facilitate a detailed examination of demographic and epidemiological influences on liver cancer trends17,18.
Statistical software and significance
All charts were made using R software (version 4.3.1) (R Foundation for Statistical Computing, Vienna, Austria). Data visualization was performed using ggplot2 (version 3.5.1). P values less than 0.05 were considered statistically significant.
Results
Incidence, prevalence, mortality, and burden of liver cancer in China, 2021
In 2021, liver cancer in China showed significant gender disparities. As depicted in Fig. 1 and detailed in Table 1, the age-standardized incidence rate (ASIR) in males was approximately three times higher than in females (14.34 vs. 4.89 per 100,000), and similarly, the prevalence rate in males was three times that in females (20.0 vs. 6.64 per 100,000). Mortality rates also reflected these disparities, with males experiencing a death rate of 12.4 per 100,000 compared to 4.57 for females. The total number of new liver cancer cases was 196,637, with 143,788 in males and 52,848 in females. The total prevalence was 265,539 cases, with 198,826 in males and 66,713 in females. In terms of overall burden, as depicted in Supplementary Fig. 1 and detailed in Table 1, the total DALYs due to liver cancer in 2021 were 4,890,023, with males contributing 3,702,093 and females 1,187,930. The age-standardized DALY rate was significantly higher in males (368.19 vs. 111.91 per 100,000). YLLs accounted for the majority of DALYs, with males experiencing 3,667,951 YLLs compared to 1,175,469 in females. YLDs totaled 46,603, with males contributing 34,142 and females 12,461. Although YLDs were lower than YLLs, they still represent a significant component of the disease burden, affecting the quality of life of liver cancer patients.
Distribution and rates of incidence, prevalence, and death of liver cancer in China, 2021. (A) Number of new liver cancer cases by age and sex. (B) ASIR of liver cancer per 100,000 population by age and sex. (C) Number of prevalent liver cancer cases by age and sex. (D) ASPR of liver cancer per 100,000 population by age and sex. (E) Number of deaths due to liver cancer by age and sex. (F) ASMR of liver cancer per 100,000 population by age and sex. ASIR age-standardized incidence rates, ASMR age-standardized mortality rates, ASPR age-standardized prevalence rates.
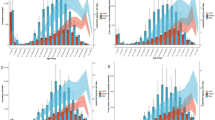
Temporal trends in liver cancer burden in China from 1990 to 2021
The trends in liver cancer burden in China from 1990 to 2021 reveal significant changes across multiple indicators, including incidence, prevalence, mortality, and disability metrics, with variations by sex. While the absolute numbers for liver cancer cases have increased, the ASIR showed a declining trend, particularly among males (Fig. 2A). Similarly, the age-standardized prevalence rate decreased steadily over time, reflecting the success of prevention and treatment strategies, despite the increase in the number of prevalent cases (Fig. 2B). Mortality rates, represented by the number of deaths and the ASMR, also exhibited a significant decline, pointing to improvements in medical care and effective public health policies in controlling liver cancer (Fig. 2C). Although the absolute numbers of DALYs, YLDs, and YLLs have all increased, their age-standardized rates have decreased, suggesting a reduced overall burden of liver cancer in terms of the population’s health (Fig. 2D–F). The decrease in age-standardized YLDs indicates that the quality of life for liver cancer patients has improved over time, while the reduction in age-standardized YLLs reflects a decrease in premature mortality and extended survival times for liver cancer patients.
Temporal trends in liver cancer indicators in China from 1990 to 2021, by sex. The bars depict the absolute numbers (e.g., number of new cases, prevalent cases, deaths, DALYs, YLDs, and YLLs) for each indicator over the years. The continuous line represents the age-standardized rates (ASIR, ASMR, ASPR, DALY rates, YLD rates, and YLL rates per 100,000 population). (A) Number of new liver cancer cases (incidence) and ASIR per 100,000 population, by sex. (B) Number of prevalent liver cancer cases and ASIR per 100,000 population, by sex. (C) Number of deaths due to liver cancer and ASMR per 100,000 population, by sex. (D) Number of DALYs due to liver cancer and age-standardized DALY rates per 100,000 population, by sex. (E) Number of YLDs due to liver cancer and age-standardized YLD rates per 100,000 population, by sex. (F) Number of YLLs due to liver cancer and age-standardized YLL rates per 100,000 population, by sex. ASIR age-standardized incidence rates, ASMR age-standardized mortality rates, ASPR age-standardized prevalence rates, DALYs disability-adjusted life years, YLDs years lived with disability, YLLs years of life lost.
Change in age-standardized rates for liver cancer between China and global level
From 1990 to 2021, the age-standardized rates for liver cancer in China exhibited distinct trends compared to global patterns (Table 2, Fig. 3). In China, the ASIR decreased from 10.58 per 100,000 to 9.52 per 100,000, reflecting an annual rate of change of -0.31%, whereas globally, the incidence rate increased slightly from 5.9 per 100,000 to 6.15 per 100,000, with an annual rate of change of 0.11%. ASPR in China remained relatively stable, changing from 13.51 per 100,000 to 13.29 per 100,000, indicating an annual rate of change of 0.02%, while global ASPR increased from 7.76 per 100,000 to 8.68 per 100,000, with an annual growth rate of 0.35%. ASMR in China showed a significant decline, with ASMR decreasing from 10.75 per 100,000 to 8.35 per 100,000, corresponding to an annual rate of change of -1.14%. In contrast, the global death rate decreased slightly from 5.86 per 100,000 to 5.65 per 100,000, with an annual rate of change of -0.22%. The burden of liver cancer, measured by DALYs, also declined notably in China, with the age-standardized DALY rate decreasing from 334.52 per 100,000 to 239.91 per 100,000, reflecting an annual rate of change of -0.96%. Globally, the DALY rate declined from 172.86 per 100,000 to 149.29 per 100,000, indicating an annual rate of change of -0.46%. YLLs due to premature mortality in China showed a significant decline, with age-standardized rates decreasing from 332.05 per 100,000 to 237.63 per 100,000, representing an annual rate of change of -1.42%. Globally, YLL rates decreased from 171.47 per 100,000 to 147.81 per 100,000, with an annual rate of change of -0.55%. YLDs in China showed a slight decline from 2.47 per 100,000 to 2.27 per 100,000, corresponding to an annual rate of change of -0.23%, whereas global YLD rates increased from 1.39 per 100,000 to 1.47 per 100,000, with an annual growth rate of 0.18%.
Comparative trends in age-standardized rates for liver cancer indicators between China and the global context from 1990 to 2021. (A) Global age-standardized rates for incidence, prevalence, mortality, DALYs, YLDs, and YLLs from 1990 to 2021. (B) Age-standardized incidence, prevalence, mortality, DALYs, YLDs, and YLLs rates in China from 1990 to 2021. DALYs disability-adjusted life years, YLDs years lived with disability, YLLs years of life lost.
Joinpoint regression analysis of age-standardized rates for liver cancer in China
Joinpoint regression analysis of liver cancer trends in China from 1990 to 2021 revealed significant changes in age-standardized rates for incidence, prevalence, and mortality. For the total population, the ASIR declined from 2000 to 2005 at -3.39% annually, increased from 2005 to 2016 at 0.83% annually, and declined again from 2016 to 2021 at -1.70% annually. The gender-specific trends show that males experienced a notable increase in ASIR from 1995 to 2000 (2.32% annually), followed by a significant decline from 2000 to 2005 (-3.27% annually), and a steady decrease from 2015 to 2021 (-1.14% annually). Females, in contrast, saw a consistent decline in ASIR from 2000 to 2005 (-3.10% annually) and again from 2016 to 2021 (-1.95% annually) (Fig. 4A, Supplementary Table 1). Similar trends were observed in ASPR and ASMR, where males had higher rates of liver cancer incidence and mortality compared to females. For males, the ASMR declined significantly from 2001 to 2005 (-4.30% annually) and again from 2015 to 2021 (-1.49% annually), while for females, the ASMR decreased from 2001 to 2006 (-3.49% annually) and from 2015 to 2021 (-2.39% annually) (Fig. 4B, Fig. 4C, Supplementary Table 1).
Joinpoint regression analysis of the sex-specific age-standardized rates for liver cancer in China from 1990 to 2021. (A) ASIRs for males (gray line) and females (green line), with the overall population trend represented by the blue line. (B) ASPRs for males, females, and the overall population. (C) ASMRs for males and females, along with the total population trend. (D) DALYs for both sexes and the overall population. (E) YLDs for both sexes and the overall population. (F) YLLs for both sexes and the overall population. ASIR age-standardized incidence rates, ASMR age-standardized mortality rates, ASPR age-standardized prevalence rates, DALYs disability-adjusted life years, YLDs years lived with disability, YLLs years of life lost.
The analysis of DALYs, YLDs, and YLLs further highlighted the gender disparities in liver cancer burden. DALYs for both males and females showed significant declines in age-standardized rates, with a -5.32% annual decline from 2001 to 2005 and another decrease of -1.92% annually from 2015 to 2021 for the total population (Fig. 4D, Supplementary Table 2). Males had a higher absolute burden in terms of DALYs, YLDs, and YLLs compared to females, reflecting both higher incidence rates and mortality. YLDs showed a slight decrease from 2000 to 2005 at -3.48% annually with a further decline from 2016 to 2021 at -1.38% annually (Fig. 4E, Supplementary Table 2). Similarly, YLLs for both genders exhibited substantial reductions, with a -5.33% annual decline from 2001 to 2005 and a further decline from 2015 to 2021 at -1.92% annually (Fig. 4F, Supplementary Table 2). These trends underscore the impact of gender-specific public health interventions and medical care in reducing the liver cancer burden, with males continuing to face a significantly higher disease burden than females in terms of both incidence and mortality.
Age, period, and cohort effects on liver cancer incidence and mortality in China
The analysis of age, period, and cohort effects on liver cancer incidence and mortality in China from 1990 to 2021 reveals significant and insightful trends. As shown in Fig. 5, the ASIRs exhibit a consistent increase with age, reaching their highest point in the 80–85 years age group across various time periods (Fig. 5A). The period effect highlights a steady decline in the incidence rates of younger age groups, while the rates for older age groups have shown a consistent increase over the same period (Fig. 5C). Cohort analysis further reveals a rising incidence rate among older birth cohorts, particularly those born between 1900 and 1940, while cohorts born after 1950 experienced a noticeable decline in incidence rates (Fig. 5D). Similarly, Supplementary Fig. 2 presents the trends for liver cancer mortality, where ASMRs also increase with age, peaking in the 80–85 years age group (Supplementary Fig. 2A). The period effect indicates a decreasing mortality trend in younger age groups, contrasted by a rise in mortality rates for older age groups (Supplementary Fig. 2C). The cohort analysis reveals that older cohorts exhibit higher mortality rates, with the peak seen in those born between 1900 and 1940, followed by a decline in the cohorts born after 1950 (Supplementary Fig. 2D).
Age, period, and cohort effects on the incidence of liver cancer in China. (A) ASIR of liver cancer according to time periods; each line connects the age-specific incidence for a 5-year period. (B) ASIR of liver cancer according to birth cohort; each line connects the age-specific incidence for a 5-year cohort. (C) Period-specific incidence rates of liver cancer according to age groups; each line connects the birth cohort-specific incidence for a 5-year age group. (D) Birth cohort-specific incidence rates of liver cancer according to age groups; each line connects the birth cohort-specific incidence for a 5-year age group. ASIR age-standardized incidence rates.
Decomposition of factors influencing liver cancer incidence and mortality in China
Figure 6 illustrates the decomposition of factors contributing to changes in liver cancer incidence and mortality in China from 1990 to 2021. The analysis reveals that both aging and population growth are key contributing factors, particularly among males, while epidemiological changes have acted as mitigating factors. For incidence, aging was the predominant driver of increases across both sexes, with significant contributions from epidemiological changes, which have helped reduce incidence rates, and population growth, which continues to elevate the absolute number of cases (Fig. 6A). For mortality, aging again emerged as the leading factor, especially among males, where demographic shifts in the aging population exacerbated liver cancer mortality rates. Epidemiological changes, reflecting improvements in liver cancer prevention and treatment, acted as mitigating factors, offsetting some of the increases, while population growth continued to contribute to higher mortality rates (Fig. 6B).
Decomposition of factors contributing to changes in liver cancer incidence and mortality in China from 1990 to 2021. (A) Contributions to changes in liver cancer incidence by sex: aging, epidemiological changes, and population growth. (B) Contributions to changes in liver cancer mortality by sex: aging, epidemiological changes, and population growth.
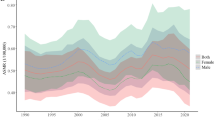
BAPC analysis of liver cancer incidence trends in China
Figure 7 presents the BAPC analysis of liver cancer incidence trends in China from 1990 to 2030. The analysis reveals projections of ASIRs for females and males separately. The incidence rates for females show a decreasing trend over time, with a noticeable decline projected through 2030 (Fig. 7A). Similarly, the incidence rates for males also exhibit a downward trajectory, with rates higher than those for females but following a similar decreasing trend (Fig. 7B). These projections indicate a gradual reduction in the burden of liver cancer incidence in China, highlighting the potential effectiveness of ongoing public health efforts and the importance of sustaining these interventions to further manage and reduce liver cancer incidence.
Discussion
Our study provides a comprehensive analysis of liver cancer trends in China from 1990 to 2021, revealing several significant findings. The ASIR of liver cancer in China exhibited a declining trend among both males and females. Similarly, the ASMR also decreased, reflecting improvements in disease management and outcomes. The burden of liver cancer, measured by DALYs, showed a notable reduction, primarily due to decreases in YLLs from premature mortality. Meanwhile, YLDs also declined slightly. These trends suggest that public health interventions, such as HBV vaccination programs, improved screening, and treatment strategies, have contributed to better liver cancer control in China. Although significant positive trends are observed, liver cancer remains a major public health challenge in China, particularly among males, who continue to have higher incidence and mortality rates.
China was categorized as a “remain stable or minor decrease” country in liver cancer trends19. The decrease in ASIR and ASPR in China contrasts with global trends, where liver cancer incidence and prevalence rates have generally increased. The decline in liver cancer rates in China can be attributed to several factors, including the implementation of nationwide HBV vaccination programs in the early 1990s and enhanced screening and treatment strategies4. The introduction of antiviral therapies for HBV and HCV infections has also played a crucial role in reducing liver cancer risk5. Furthermore, public health efforts to control aflatoxin contamination and reduce alcohol consumption have contributed to the observed trends6. In addition, advances in targeted therapy and immunotherapy, such as tyrosine kinase inhibitors (TKIs) and immune checkpoint inhibitors (ICIs), have improved survival outcomes for advanced liver cancer patients20. Combination regimens like atezolizumab plus bevacizumab have demonstrated superior efficacy compared to traditional sorafenib monotherapy21. Treatment strategies that integrate systemic therapy with locoregional interventions have shown improved effectiveness in clinical trials22. Despite these improvements, liver cancer remains a significant public health concern in China, particularly among males. The gender disparity in liver cancer incidence and mortality is evident, with males experiencing higher rates compared to females. This disparity can be partially explained by greater HBV and HCV infection prevalence among males, as well as higher exposure to risk factors such as alcohol and tobacco use2,23. Additionally, socio-cultural factors may influence healthcare-seeking behavior, resulting in later-stage diagnoses and poorer outcomes in males24.
Geographical variations must also be considered. There were significant regional disparities in the burden of liver cancer in China. Rural areas, especially those in the less—developed western regions, had higher incidence and mortality rates than urban and eastern areas. In 2014, liver cancer ranked 2nd in incidence and mortality in the western areas but 5th in incidence and 2nd in mortality in the eastern areas6. For example, the period and cohort effects of liver cancer risk in Hong Kong have declined due to epidemiological shifts25. However, in Hubei Province, both the number of liver cancer cases and ASIR have shown a clear upward trend due to various causative factors. This suggests that broad prevention policies aimed at mitigating liver cancer may have had a limited impact in certain regions26. Similar findings have been reported in other regions, such as Iran, where the incidence and mortality rates of gastrointestinal cancers, including liver cancer, have increased over time8. Furthermore, non-alcoholic steatohepatitis (NASH)-related liver cancer showed significant increases in Australasia, Southern Latin America, and High-income North America27. The trends in China highlight the success of certain public health measures while emphasizing the need for region-specific strategies to address persistent and emerging risk factors.
Our study employed several robust analytical methods to elucidate long-term trends in liver cancer burden in China. The APC analysis confirmed that older age groups and earlier birth cohorts face a higher liver cancer risk, aligning with prior research3. The cohort effect demonstrated a higher incidence rate among individuals born between 1900 and 1940, followed by a notable decline in those born after 1950. This pattern reflects the historical prevalence and transmission patterns of HBV and HCV infections, as well as the subsequent impact of large-scale vaccination and antiviral therapy programs28. The period effect identified sharp fluctuations in liver cancer rates at certain time points, emphasizing the influence of policy interventions, healthcare advancements, and environmental risk factors on disease trends. The BAPC analysis projects a continued decline in liver cancer incidence through 2030, reinforcing the effectiveness of current prevention strategies. However, the emerging burden of non-alcoholic fatty liver disease (NAFLD) and metabolic syndrome presents new challenges, as these conditions are increasingly recognized as major risk factors for liver cancer29,30. Additionally, China’s ongoing demographic transition and aging population contribute to the rising absolute burden of liver cancer, as both incidence and mortality rates remain significantly higher among older adults17,24,31. These findings highlight the need to sustain and enhance current public health efforts while adapting strategies to address emerging metabolic and demographic risk factors.
Our decomposition analysis provided deeper insights into the key factors influencing liver cancer incidence and mortality trends. The analysis revealed that demographic changes, particularly population aging, were significant contributors to the rising liver cancer incidence and mortality. This finding aligns with the broader aging trend in China, which increases the pool of individuals at risk for developing liver cancer32. However, epidemiological changes, such as reductions in HBV and HCV prevalence due to widespread vaccination and antiviral treatments, played a critical role in mitigating the effects of aging on liver cancer trends. These improvements in epidemiological factors have significantly reduced liver cancer incidence among younger cohorts, underscoring the effectiveness of public health interventions5. This contrasts with findings from Hong Kong, where demographic factors, especially aging, continued to drive liver cancer incidence, particularly among females, as stable epidemiological factors could not counterbalance the demographic impacts25. These observations underscore the importance of sustained and adaptive public health strategies to address both demographic and epidemiological factors in liver cancer prevention and control.
Despite the robustness of our findings, this study has several limitations. Firstly, the accuracy of our estimates depends on the quality of the data sources, which may vary over time and between regions. As a part of the GBD study, some data points were estimated rather than derived from actual reported values, especially in regions with limited data availability. Additionally, the modeling approach used in GBD involves assumptions that could influence the accuracy of the estimates, particularly when applied to countries with varying healthcare infrastructure and data quality. Secondly, while we included a comprehensive set of indicators (incidence, prevalence, mortality, DALYs, YLDs, and YLLs), other factors such as socioeconomic status, healthcare access, and environmental exposures were not explicitly analyzed. Thirdly, our study was observational, limiting our ability to infer causality from the identified trends. Lastly, the projections made using the BAPC model are based on historical data and may not account for future changes in risk factors or healthcare interventions. Future research should focus on addressing these limitations by incorporating more detailed data and exploring causal relationships.
Conclusions
In conclusion, our study underscores the significant progress made in reducing the burden of liver cancer in China over the past three decades, highlighting the impact of effective public health interventions such as the hepatitis B vaccination program and improved medical care. Despite these advancements, liver cancer remains a critical public health issue, particularly among males who continue to exhibit higher incidence and mortality rates. The findings emphasize the necessity of sustaining and enhancing current prevention and treatment strategies, addressing both demographic and epidemiological factors. Future research should focus on the emerging challenges posed by NAFLD and metabolic syndrome, which are becoming significant risk factors for liver cancer. Additionally, there is a need for more detailed studies on the socioeconomic and environmental determinants of liver cancer, as well as the development of gender-specific prevention and control strategies. Continued efforts in early detection, targeted therapies, and comprehensive public health campaigns will be crucial in further reducing the liver cancer burden and improving outcomes for affected populations in China.
Data availability
Data are available in a public, open access repository. All data used are publicly available from the IHME’s online platform, found at https://vizhub.healthdata.org/gbd-results/.
References
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 74(3), 229–263 (2024).
Chen, W. et al. Cancer statistics in China, 2015. CA Cancer J. Clin. 66(2), 115–132 (2016).
McGlynn, K. A., Petrick, J. L. & El-Serag, H. B. Epidemiology of hepatocellular carcinoma. Hepatology (Baltimore, Md) 73(Suppl 1), 4–13 (2021).
Liang, X. et al. Epidemiological serosurvey of hepatitis B in China–declining HBV prevalence due to hepatitis B vaccination. Vaccine 27(47), 6550–6557 (2009).
Wang, M. et al. Contribution of hepatitis B virus and hepatitis C virus to liver cancer in China north areas: Experience of the Chinese National Cancer Center. Int. J. Infect. Dis. 65, 15–21 (2017).
Zheng, R. et al. Liver cancer incidence and mortality in China: Temporal trends and projections to 2030. Chin. J. Cancer Res. = Chung-kuo yen cheng yen chiu 30(6), 571–579 (2018).
Ebrahimi, P. et al. Investigating the mortality trend of gastrointestinal cancers in Babol, North Iran (2013–2021). BMC Gastroenterol. 24(1), 100 (2024).
Ebrahimi, P. et al. Utilization of a joint point regression model for predicting mortality rates of common cancers in Babol City. Cancer reports (Hoboken, NJ) 8(1), e70107 (2025).
Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet (London, England) 402(10397):203–234 (2023).
Kim, H. J., Fay, M. P., Feuer, E. J. & Midthune, D. N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 19(3), 335–351 (2000).
Kim, H. J., Chen, H. S., Byrne, J., Wheeler, B. & Feuer, E. J. Twenty years since Joinpoint 1.0: Two major enhancements, their justification, and impact. Stat. Med. 41(16), 3102–3130 (2022).
Yang, Y., Fu, W. J., Land, K. C. A Methodological Comparison of Age-Period-Cohort Models: The Intrinsic Estimator and Conventional Generalized Linear Models. 34(1):75-110 (2004).
Cao, F. et al. Global, regional and national temporal trends in prevalence for musculoskeletal disorders in women of childbearing age, 1990–2019: An age-period-cohort analysis based on the Global Burden of Disease Study 2019. Ann. Rheum. Dis. 83(1), 121–132 (2024).
Carlin, B. P. & Louis, T. A. Bayes and empirical Bayes methods for data analysis. Stat. Comput. 7(2), 153–154 (1997).
Kiyoshige, E. et al. Projections of future coronary heart disease and stroke mortality in Japan until 2040: A Bayesian age-period-cohort analysis. Lancet Region. Health Western Pac. 31, 100637 (2023).
Véron, J., Preston, S. H., Heuveline, P., Guillot, M. Demography: Measuring and Modeling Population Processes. (2000).
Cheng, X. et al. Population ageing and mortality during 1990–2017: A global decomposition analysis. PLoS Med. 17(6), e1003138 (2020).
Global, regional, and national burden of neck pain, 1990–2020, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 6(3):e142-e155 (2024).
Liu, Z. et al. The trends in incidence of primary liver cancer caused by specific etiologies: Results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J. Hepatol. 70(4), 674–683 (2019).
Zheng, J. et al. Hepatocellular carcinoma: Signaling pathways and therapeutic advances. Signal Transduct. Target. Ther. 10(1), 35 (2025).
Kudo, M. et al. Impact of Bevacizumab being skipped due to adverse events of special interest for Bevacizumab in patients with unresectable hepatocellular carcinoma treated with Atezolizumab plus Bevacizumab: An exploratory analysis of the phase III IMbrave150 study. Liver Cancer 13(4), 401–412 (2024).
Zhong, B.-Y. et al. Combination locoregional and systemic therapies in hepatocellular carcinoma. Lancet Gastroenterol. Hepatol. https://doi.org/10.1016/S2468-1253(24)00247-4 (2025).
El-Serag, H. B. & Rudolph, K. L. Hepatocellular carcinoma: Epidemiology and molecular carcinogenesis. Gastroenterology 132(7), 2557–2576 (2007).
Qin, Y., Tang, C., Li, J. & Gong, J. Liver cancer in China: The analysis of mortality and burden of disease trends from 2008 to 2021. BMC Cancer 24(1), 594 (2024).
Ma, T., Wei, X., Wu, X. & Du, J. Trends and future projections of liver cancer incidence in Hong Kong: A population-based study. Arch. Public Health 81(1), 179 (2023).
Liu, H. et al. Long-term trends in incidence, mortality and burden of liver cancer due to specific etiologies in Hubei Province. Sci. Rep. 14(1), 4924 (2024).
Li, S. et al. Burden of NASH related liver cancer from 1990 to 2021 at the global, regional, and national levels. Front. Nutr. 12, 1510563 (2025).
Cui, F. et al. Prevention of chronic hepatitis B after 3 decades of escalating vaccination policy, China. Emerg. Infect. Dis. 23(5), 765–772 (2017).
Zou, Z., Zhang, Z., Lu, C. & Wang, H. Comparison of time trends in the incidence of primary liver cancer between China and the United States: An age-period-cohort analysis of the Global Burden of Disease 2019. Chin. Med. J. 135(17), 2035–2042 (2022).
Xiao, J. et al. Global liver disease burdens and research trends: Analysis from a Chinese perspective. J. Hepatol. 71(1), 212–221 (2019).
Chang, A. Y., Skirbekk, V. F., Tyrovolas, S., Kassebaum, N. J. & Dieleman, J. L. Measuring population ageing: An analysis of the Global Burden of Disease Study 2017. Lancet Public Health 4(3), e159–e167 (2019).
Feng, Z. et al. Long-term care system for older adults in China: Policy landscape, challenges, and future prospects. Lancet 396(10259), 1362–1372 (2020).
Funding
This work was sponsored by Fujian Provincial Natural Science Foundation of China (Grant No. 2024J011064) and Clinical research funding project initiated by researchers of Fujian Cancer Hospital (No. 202413003). This work was also sponsored by Startup Fund for scientific research, Fujian Medical University (Grant No. 2022QH1146), Fujian Clinical Research Center for Radiation and Therapy of Digestive, Respiratory and Genitourinary Malignancies (Grant No. 2021Y2014), and the High-level Talent Project (Category C) of Fujian Cancer Hospital (Grant No. 2024YNG02).
Author information
Authors and Affiliations
Contributions
Zhouwei Zhan and Bijuan Chen contributed equally to this work and share first authorship. They were responsible for the study conception and design, data analysis, and manuscript drafting. Rui Huang, Wei Lin, Shuangting Lan, Xintong Yao, Shuqi Huang, Wenlong Lin, Shaohua Xu, and Sijing Zhou contributed to data acquisition and statistical analysis. Jiami Yu and Xiaojie Wang contributed to the literature review and manuscript preparation. Xiaoyan Lin and Zengqing Guo, as the corresponding authors, supervised the study, provided guidance throughout the research process, and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhan, Z., Chen, B., Huang, R. et al. Long-term trends and future projections of liver cancer burden in China from 1990 to 2030. Sci Rep 15, 13120 (2025). https://doi.org/10.1038/s41598-025-96615-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-96615-1