Abstract
The objective of this study was to investigate whether eyeliner use is associated with an increase in dry eye symptoms. A survey was conducted to collect data on cosmetic usage and Ocular Surface Disease Index (OSDI) scores from a diverse public sample. Additionally, eyecare professionals were queried regarding their practice of inquiring about cosmetic use during patient consultations. The survey included specific questions about eyeliner application and the calculation of OSDI scores, with a score of 13 or higher indicating the presence of dry eye symptoms. Individuals who reported using eyeliner had a significantly higher rate of OSDI scores above 13 compared to non-users (42.93% vs. 33.38%, p < 0.001). Notably, subjects who applied eyeliner to the lid margins exhibited an even more pronounced increase in high OSDI scores (48.17%, p < 0.001). Furthermore, a significant proportion of patients (23.37%) expressed reluctance to discontinue cosmetic use when advised in medical contexts, while only 48.19% of healthcare providers routinely inquired about cosmetic use during patient consultations. The usage of eyeliner is associated with higher OSDI scores, underscoring the need for both eyecare practitioners and eyeliner users to be more cognizant of the potential impact of eyeliner on the ocular surface.
Similar content being viewed by others
Introduction
The Tear Film & Ocular Surface Society recently published a report emphasizing the influence of cosmetics on ocular surface diseases, and that several eye cosmetic products may have the potential to damage the ocular surface and adnexa1,2,3. Eyeliner is one of the most-used eye cosmetics, which can be either permanent or rinsed off4,5,6. The most common purpose for using eyeliner is to enhance the definition of the eye, and its history can be traced back thousands of years7,8,9. A recent report demonstrated the impact of eyeliner tattoos on ocular surface homeostasis, but it remains unclear whether rinse-off eyeliners also impact the ocular surface10,11,12,13.
We hypothesize that the use of rinse-off eyeliner is a risk factor for increased dry eye symptoms14,15,16. To test this hypothesis, we conducted a survey that included questions about cosmetic use and the Ocular Surface Disease Index (OSDI) questionnaire. The OSDI questionnaire consisted of 12 questions, and the total score was positively correlated with the severity of dry eye and its impact on daily activities17. The combination of clinical signs of dry eye and OSDI scores provided a comprehensive evaluation of ocular surface disease18,19. As many individuals with mild dry eye symptoms do not typically seek medical consultation, we conducted our survey among the general population rather than in clinical settings.
Methods
Questionnaire collection
This study strictly adheres to the principles outlined in the Declaration of Helsinki. The study protocol was approved by the Medical Ethics Committee of Zhongnan Hospital, Wuhan University, China (2022130). Electronic informed consent was obtained in the questionnaires from all subjects and/or their legal guardian(s). A total of two questionnaires were collected. The first questionnaire aimed to assess the general cosmetic usage patterns among both healthcare and non-healthcare professionals. The questionnaire detailed the types and frequencies of skincare and cosmetic products used (Table 1). Non-healthcare participants were queried about their willingness to temporarily discontinue cosmetic use based on medical recommendations. In contrast, healthcare professionals were surveyed on their practices regarding the inquiry of cosmetic use among their patients during the diagnostic and treatment processes.
The second part of the study was a survey of the general population regarding eyeliner usage and the Ocular Surface Disease Index (OSDI). This survey included basic information about the population, such as age, gender, occupation, general health conditions, etc., as well as information about eyeliner use, including the brand, frequency, location, etc. We asked about other factors that may cause dry eye symptoms, such as contact lens wear, previous ocular surface disease, refractive surgery, topical ocular medications, prolonged screen use, air-conditioned use and other conditions that may affect the ocular surface. These factors were used as exclusion criteria in the questionnaire. We did not specifically ask about screen time, as the age and occupational types of the eyeliner and non-eyeliner groups in the questionnaire were matched, and we assumed their screen time would be similar. The OSDI scale was incorporated into the questionnaire (Table 2). Participants who had used eyeliner for over 1 year with a usage frequency of at least 3 times per week were categorized as the eyeliner group, while those who did not meet this criterion were placed in the non-eyeliner user group. An OSDI score of 13 or higher was defined as an indicator of the presence of dry eye symptoms20.
Statistical analysis
The data analysis was conducted using SPSS 23.0 (IBM, Armonk, New York, United States). The OSDI scores were presented as mean ± standard deviation (SD). The Kolmogorov-Smirnov test was used to test for normality, with a P-value > 0.05 indicating a normal distribution. For non-normally distributed data, the nonparametric Mann-Whitney U test was used for two independent samples, while the nonparametric Kruskal-Wallis test was used for more than two independent samples. To explore the association between the presence of dry eye symptoms in the population and potential predictive factors such as gender, age distribution, the use of eyeliner, and the presence of eyeliner tattoos, odds ratios (OR) and univariate, unadjusted logistic regression models were applied (Table 3). Furthermore, binary logistic regression analysis was conducted to pinpoint potential predictive factors for the population exhibiting symptoms of dry eye disease, focusing on eyeliner use, eyeliner tattoos, and gender (Table 4). The Chi-square tests were employed to assess the impact of various risk factors on the prevalence of the disease in the statistical analysis.
Results
A total of 654 questionnaires were gathered for the initial survey, with 354 from non-healthcare practitioners and 300 from healthcare practitioners (https://www.wjx.cn/wjx/activitystat/verifyreportpassword.aspx?viewtype=1&activity=172487561&type=1). The respondents included 158 males and 496 females aged 16–73 years old from various countries, with a mean age of 33.9 ± 8.1.
In the follow-up survey focusing on eyeliner usage behaviors and OSDI scores, 1344 samples from 28 different countries were collected, including 169 males and 1175 females aged 16–60 years old, with a mean age of 19.4 ± 10.8 (https://www.wjx.cn/wjx/activitystat/verifyreportpassword.aspx?viewtype=1&activity=158522950&type=1). The results showed that the general public and healthcare practitioners reported cosmetics usage frequencies of 75.42% and 63.67% (p < 0.01), respectively (Fig. 1A and B). Additionally, 23.37% of patients were unwilling or hesitant to comply if advised to discontinue using cosmetics in medical situations (Fig. 1C), and only 48.19% of healthcare practitioners asked their patients about their cosmetic usage behavior during consultations (Fig. 1D).
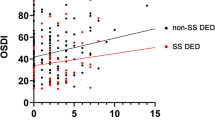
There were 722 individuals in the control group (non-eyeliner users) with an average age of 23.86 ± 5.21, and 622 individuals in the eyeliner group with an average age of 21.25 ± 4.89. When using analysis of variance to compare the percentage of populations with an OSDI score higher than 13 between the eyeliner group and the control group, it was found to be 42.93% in the eyeliner group and 33.38% in the control group (p = 0.0004, p < 0.001, Fig. 2A and Supp Fig. 1A). After adjusting for confounding factors such as eyeliner tattooing, the percentage of individuals with an OSDI score higher than 13 was significantly higher in the eyeliner users (p = 0.0086, Fig. 2B and Supp Fig. 1B), but there was no significant difference between whether the participants applied eyeliner on the inner side of the lash line or the outer side (p = 0.14, Fig. 2C and Supp Fig. 1C). The proportions of individuals with an OSDI score higher than 13 were significantly higher in those who applied eyeliner on the inner side of the lash line compared to the non-eyeliner users (p = 0.0006, p < 0.001, Fig. 2D and Supp Fig. 1D), and significantly higher in those with eyeliner tattoos compared with the control group (p < 0.0001) (Fig. 3 and Supp Fig. 1E). In Supplementary Fig. 1, we plot the results mentioned above as a stacked bar chart to show the differences between groups more intuitively. It is important to note that the small sample size of the eyeliner tattoo population may impact the statistical significance. As the frequency of eyeliner increases, dry eye symptoms appear to increase (Fig. 4A). In addition, the longer the eyeliner was applied, the easier dry eye symptoms increase (Fig. 4B), which may be related to the inability to clean thoroughly and the residue of eyeliner ingredients.
Survey of eyeliner usage behaviors and OSDI scores. (A) Comparison of the prevalence of population with OSDI score >13 between the control and the eyeliner group. (B) Comparison of the two groups after excluding individuals with the eyeliner tattoos. (C) Comparison between population who draw eyeliner on the inside and outside of the lash line. (D) Comparison of inner eyeliner and control group. Chi-square test #p<0.05, ##p<0.01, ###p< 0.005, ####p< 0.001.
Univariate logistic regression revealed that the following factors were significantly correlated with a population having a higher OSDI score (Table 3): gender (reference: male; female, crude OR = 1.643 (1.123–1.832), p = 0.003), eyeliner use (reference yes, crude OR = 1.467 (1.174–1.826), p = 0.001), and eyeliner tattoo (reference yes, crude OR = 23.507 (11.698–47.235), p = 0.001). And age (reference: ≤40; >40 years old, crude OR = 1.255 (0.833–1.783), p = 0.206) was not significantly correlated which maybe because of only 143 participants older. A final multivariate model was performed including gender, eyeliner use, and eyeliner tattoo as predictors which were statistically significant in the univariate analysis (Table 3). To further explore the contribution of different potential influential factors, binary logistic regression was used (Table 4). In binary logistic regression, the regression coefficient for the use of eyeliner was 0.46, which indicated that the use of eyeliner was positively correlated with dry eye symptoms, and the p < 0.0001 was statistically different which further validates our suspicions. Eyeliner tattoo was found to significantly impact populations that have higher OSDI scores (B = 3.728, p < 0.0001).
Discussion
In this questionnaire survey, it was observed that individuals who regularly use eyeliner tend to exhibit higher OSDI scores, suggesting a potential link between the use of this cosmetic product and the health of the ocular surface. This finding underscores the importance of considering cosmetics use as a potentially impactful factor on ocular health, which is often overlooked in routine assessments and discussions.
Eye makeup use is an omnipresent lifestyle choice and exerts a considerable influence on ocular health. Our research revealed a notable increase in the prevalence of dry eye symptoms among individuals who use eyeliner whether it’s pencil or liquid, as opposed to those who do not. Specifically, we found that 42.93% of eyeliner users reported experiencing dry eye symptoms, which is significantly higher than the 33.38% observed among non-eyeliner users.
The analyses conducted in our study, including univariate and multivariate logistic regression as well as binary logistic regression (Tables 3 and 4), consistently demonstrated that the use of eyeliner is a significant predictor of dry eye symptoms21. These findings underscore the importance of considering cosmetic use, particularly eyeliner, as a contributing factor when assessing and managing dry eye conditions. This is consistent with the risk factors for dry eye mentioned in previous articles including gender, age, cosmetic use, etc1,22,23,24. It is essential for both healthcare providers and the general public to be aware of the potential ocular health implications associated with the regular use of eye makeup products.
Individuals who apply eyeliner, especially on the inner side of the lash line, have been found to exhibit a significantly higher rate of elevated OSDI scores when compared to the general population (p < 0.001). The inner side of the eyelash line is closer to the eye surface, and the application of eyeliner in this area increases the likelihood of the cosmetic’s particles interacting with the ocular surface and tear films with each blink. Such contact can potentially lead to irritation and compromise the integrity and function of the ocular surface and the meibomian glands25,26,27. Using eyeliner on the inner side of the eyelashes is more likely to cause dry eye symptoms compared to the outer side. Although our questionnaire also showed this result, there was no statistical difference, possibly because only 164 participants who used eyeliner on the inner side of the eyelashes were included, and the sample size was small or unevenly distributed. Moreover, our study found that individuals with eyeliner tattoos exhibited significantly higher OSDI scores compared to the control group. This result is consistent with a previous report on the impact of eyeliner tattoos on mice, which showed reduced tear secretion, ocular surface damage, and increased inflammation levels in both the meibomian gland and lacrimal gland10,28. While our survey mainly focused on rinse-off eyeliner, we found that approximately 4.91% of participants who use eyeliner also have eyeliner tattoos. The presence of both temporary eyeliner applications and permanent eyeliner tattoos may exert a synergistic effect, potentially exacerbating the adverse impact on the ocular surface.
Interestingly, we observed 75.42% of the general public and 63.67% of healthcare practitioners reported daily cosmetic use, respectively (p < 0.01). And approximately half of the healthcare practitioners did not inquire about their patients’ cosmetic usage habits during medical consultations. The proportion of women among healthcare practitioners is 74.33%, which is slightly lower than that in the general participant population (77.12%). Additionally, the average age of healthcare practitioners is 35.7 ± 6.9 years, compared to 32.1 ± 7.4 years in the general population. Given that the proportion of men who wear makeup is relatively low and some are reluctant to admit to it and complete the questionnaire, the differences in gender and age distribution may partially explain the variations in cosmetic usage observed between the two groups. However, these findings indicate that the use of makeup is an aspect that is often overlooked in clinical consultations. It is possible that healthcare professionals who use fewer cosmetics themselves may not fully recognize the prevalence of makeup use as a prominent lifestyle choice among their patients and its potential impact on eye health. Furthermore, our findings revealed that approximately 23.37% of patients were hesitant or unwilling to cease cosmetic use even when medically advised. This reluctance underscores the importance of patient education regarding the potential impact of cosmetics on the health of the ocular surface29,30.
To be noted, this study primarily focused on the questionnaire, and we did not assess the objective signs of ocular surface disease. The reason for this is that the questionnaire was designed for the general population rather than patients visiting the hospital for consultation. Our goal was to include as many participants as possible, particularly healthy individuals or those with mild symptoms, as most hospital visitors tend to have more severe symptoms or other medical conditions. And it was impractical for us to collect objective data from 1,344 participants across various countries. It is worth noting that several studies have shown that the associations between signs and symptoms of dry eye are often low and inconsistent31,32,33. Given that the primary objective of our study is to investigate the impact of eyeliner usage on dry eye symptoms, we chose to focus solely on questionnaire data. However, a small subset of participants underwent tests such as fluorescein tear film break-up time, tear meniscus height, ocular surface fluorescein staining, Schirmer I test, meibomian gland function assessment, and Demodex infection screening (Data not shown). The results from these tests were consistent with previous studies, which have shown that individuals who use eyeliner for extended periods are more likely to exhibit objective signs of dry eye compared to those who do not use eyeliner21,25,34.
One limitation of our study is its primary focus on younger women, which may introduce bias. It’s important to note that the use of cosmetics is not exclusive to females35, but some of male cosmetic users are reluctant to admit and complete the questionnaire,. Beside this limitation, the basic characteristics of the collected population were matched. Although our study lacked sufficient male participants, there is a growing number of males incorporating cosmetics into their routines. Clinicians are encouraged to take note of this trend and inquire about cosmetic use during consultations with male patients as well. Furthermore, our study did not analyze the ingredients in different eyeliner brands, nor consider the various levels of impact on the homeostasis of the ocular surface. In our future study, we will conduct further research on the mechanism by which eyeliners impact the ocular surface, as well as analyze the differences between eyeliner brands and their chemical composition.
To support eyeliner users in maintaining ocular health and to assist healthcare professionals in providing informed guidance, we propose the following guidelines:
-
1.
Outer lash line application: We recommend applying eyeliner primarily on the outer side of the lash line during daily use. This technique reduces the risk of irritation and dry eye symptoms compared to applying eyeliner on the inner lash line or waterline.
-
2.
Avoid inner lash line: Refrain from applying eyeliner on the inner lash line or waterline, as this can obstruct meibomian gland orifices and exacerbate dry eye conditions.
-
3.
Timely cleaning: Ensure thorough and regular cleaning of the eyelids and lashes to remove residual makeup. Use gentle, non-irritating makeup removers or wipes specifically designed for the eye area.
-
4.
Avoid sharing: Do not share eyeliner products with others to prevent the transmission of infections and contaminants.
-
5.
Replace regularly: Replace eyeliner products regularly (i.e. every 3 months) to minimize the risk of bacterial growth and contamination.
-
6.
Product selection: Choose eyeliners that are specifically formulated to be less irritating to the skin. Look for products labeled as hypoallergenic, fragrance-free, and ideally preservative-free. Individuals with a history of dry eye or sensitive skin should consult with an ophthalmologist or dermatologist for personalized recommendations.
In conclusion, our study highlights that the widespread use of eye cosmetics is associated with higher OSDI scores. It is imperative that both clinicians and patients be more cognizant of this common lifestyle practice and its implications for eye health. Healthcare providers should consider cosmetic use as a factor in their patient assessments and engage in patient education about the potential risks associated with their cosmetic routines.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Sullivan, D. A. et al. TFOS lifestyle: impact of cosmetics on the ocular surface. Ocular Surf. 29, 77–130. https://doi.org/10.1016/j.jtos.2023.04.005 (2023).
Craig, J. P. et al. TFOS lifestyle report executive summary: A lifestyle Epidemic - Ocular surface disease. Ocular Surf. 30, 240–253. https://doi.org/10.1016/j.jtos.2023.08.009 (2023).
Ueda, S. & Koyama, T. Influence of eye make-up on the perception of gaze direction. Int. J. Cosmet. Sci. 33, 514–518. https://doi.org/10.1111/j.1468-2494.2011.00664.x (2011).
Ng, A., Evans, K., North, R. V., Jones, L. & Purslow, C. Impact of eye cosmetics on the eye, adnexa, and ocular surface. Eye Contact Lens-Science Clin. Pract. 42, 211–220. https://doi.org/10.1097/icl.0000000000000181 (2016).
Alhazzaa, S. A. F. & Krahn, P. M. KOHL - A HAZARDOUS EYELINER. Int. Ophthalmol. 19, 83–88. https://doi.org/10.1007/bf00133177 (1995).
Yazbeck, C., Cheymol, J., Dandres, A. M. & Barbéry-Courcoux, A. L. Lead exposure in pregnant women and newborns:: a screening update. Arch. Pediatr. 14, 15–19. https://doi.org/10.1016/j.arcped.2006.09.016 (2007).
Murube, J. Ocular cosmetics in ancient times. Ocular Surf. 11, 2–7. https://doi.org/10.1016/j.jtos.2012.09.003 (2013).
Draelos, Z. D. Cosmetics and skin care products - A historical perspective. Dermatol. Clin. 18, 557– (2000).
Arai, T. & Nittono, H. Cosmetic makeup enhances facial attractiveness and affective neural responses. Plos One 17. https://doi.org/10.1371/journal.pone.0272923 (2022).
Li, Z. et al. Eyeliner tattoos disturb ocular surface homeostasis. Ocular Surf. 23, 216–218. https://doi.org/10.1016/j.jtos.2021.10.008 (2022).
Lee, Y. B., Kim, J. J., Hyon, J. Y., Wee, W. R. & Shin, Y. J. Eyelid Tattooing induces meibomian gland loss and tear film instability. Cornea 34, 750–755. https://doi.org/10.1097/ico.0000000000000452 (2015).
Lu, C. W. et al. Bilateral diffuse lamellar keratitis triggered by permanent eyeliner tattoo treatment: A case report. Experimental Therapeutic Med. 14, 283–285. https://doi.org/10.3892/etm.2017.4506 (2017).
Yoon, J., Kim, A. Y., Jun, R. M. & Han, K. E. The effect of eyeliner tattoo on meibomian gland dysfunction and the ocular surface. J. Korean Ophthalmological Soc. 61, 146–152. https://doi.org/10.3341/jkos.2020.61.2.146 (2020).
Ercan, Z. E. Effect of eyeliner and Mascara use on tear film and meibomian glands. Saudi J. Ophthalmol. 36, 113–116. https://doi.org/10.4103/sjopt.sjopt_170_21 (2022).
Haddad, R., Zehetbauer, G. PROBLEMS ARISING FROM THE USE OF COSMETICS ON THE LID MARGIN. Klin. Monatsbl. Augenheilkd. 177, 829–831, doi:https://doi.org/10.1055/s-2008-1057739 (1980).
Tang, K. et al. A review on common ingredients of periocular cosmetics and their hazards. Curr. Org. Chem. 19, 30–38. https://doi.org/10.2174/1385272819666141107225726 (2015).
F, S. et al. TFOS DEWS II Epidemiology Report. Ocul Surf. 34–365 (2017).
Dougherty, B. E., Nichols, J. J. & Nichols, K. K. Rasch analysis of the ocular surface disease index (OSDI). Investig. Ophthalmol. Vis. Sci. 52, 8630–8635. https://doi.org/10.1167/iovs.11-8027 (2011).
Özcura, F., Aydin, S. & Helvaci, M. R. Ocular surface disease index for the diagnosis of dry eye syndrome. Ocul. Immunol. Inflamm. 15, 389–393. https://doi.org/10.1080/09273940701486803 (2007).
Jin, Y. et al. Prevalence and risk factors of dry eye symptoms after successful dacryocystorhinostomy for patients with lacrimal passage obstruction. Eur. J. Ophthalmol. 32, 2662–2669. https://doi.org/10.1177/11206721211069739 (2022).
Prabhasawat, P. et al. Eyeliner induces tear film instability and meibomian gland dysfunction. Cornea 39, 473–478. https://doi.org/10.1097/ico.0000000000002198 (2020).
Qian, L. & Wei, W. Identified risk factors for dry eye syndrome: A systematic review and meta-analysis. Plos One 17. https://doi.org/10.1371/journal.pone.0271267 (2022).
Wang, M. T. M., Muntz, A., Mamidi, B., Wolffsohn, J. S. & Craig, J. P. Modifiable lifestyle risk factors for dry eye disease. Contact Lens Anterior Eye 44. https://doi.org/10.1016/j.clae.2021.01.004 (2021).
Vicente Garcia-Marques, J., Talens-Estarelles, C., Garcia-Lazaro, S., Wolffsohn, J. S. & Cervino, A. Systemic, environmental and lifestyle risk factors for dry eye disease in a mediterranean Caucasian population. Contact Lens Anterior Eye 45. https://doi.org/10.1016/j.clae.2021.101539 (2022).
Wang, M. T. & Craig, J. P. Investigating the effect of eye cosmetics on the tear film: current insights. Clin. Optometry 10, 33–40. https://doi.org/10.2147/opto.S150926 (2018).
Barros, R. C., Van Kooten, T. G. & Veeregowda, D. H. Investigation of Friction-induced damage to the pig cornea. Ocular Surf. 13, 315–320. https://doi.org/10.1016/j.jtos.2015.05.004 (2015).
Ng, A., Evans, K., North, R. V. & Purslow, C. Migration of cosmetic products into the tear film. Eye Contact Lens-Science Clin. Pract. 41, 304–309. https://doi.org/10.1097/icl.0000000000000124 (2015).
Vagefi, M. R. et al. Adverse reactions to permanent eyeliner tattoo. Ophthal. Plast. Reconstr. Surg. 22, 48–51. https://doi.org/10.1097/01.iop.0000196713.94608.29 (2006).
Thummak, S., Uppor, W. & Wannarit, L. Patient compliance: A concept analysis. Belitung Nurs. J. 9, 421–427. https://doi.org/10.33546/bnj.2807 (2023).
Chuckpaiwong, V. et al. Compliance with lid hygiene in patients with meibomian gland dysfunction. Clin. Ophthalmol. 16, 1173–1182. https://doi.org/10.2147/opth.S360377 (2022).
Nichols, K. K., Nichols, J. J. & Mitchell, G. L. The lack of association between signs and symptoms in patients with dry eye disease. Cornea 23, 762–770. https://doi.org/10.1097/01.ico.0000133997.07144.9e (2004).
Kyei, S., Dzasimatu, S. K., Asiedu, K. & Ayerakwah, P. A. Association between dry eye symptoms and signs. J. Curr. Ophthalmol. 30, 321–325. https://doi.org/10.1016/j.joco.2018.05.002 (2018).
Bartlett, J. D., Keith, M. S., Sudharshan, L. & Snedecor, S. J. Associations between signs and symptoms of dry eye disease: a systematic review. Clin. Ophthalmol. (Auckland N Z) 9, 1719–1730. https://doi.org/10.2147/opth.S89700 (2015).
Coroneo, M. T., Rosenberg, M. L. & Cheung, L. M. Ocular effects of cosmetic products and procedures. Ocular Surf. 4, 94–102. https://doi.org/10.1016/s1542-0124(12)70031-9 (2006).
Byrne, A. & Milestone, K. He wouldn’t be seen using it … Men’s use of male grooming products as a form of invisible consumption. J. Consumer Cult. 23, 146–167. https://doi.org/10.1177/14695405211066314 (2023).
Acknowledgements
This study was funded by the National Natural Science Foundation of China [82201156], Hubei Provincial Natural Science Foundation [2022CFB160], Zhongnan Hospital of Wuhan University Science, Technology and Innovation Seed Fund [CXPY2022077] and Zhongnan Hospital of Wuhan University Science Startup Fund [RCYJ20220101]. The authors also express their appreciation to the Eyes Are The Story brand (USA) for circulating a survey to their global distribution.
Author information
Authors and Affiliations
Contributions
Y.L. and M.K. proposed experimental design and ideas. YR.S. and AG.S. collected of questionnaire data. Y.L. and YR.S. wrote the main manuscript text and prepared Tables 1, 2, 3 and 4; Figs. 1, 2, 3, 4 and 5 and supplementary figure 1. T.Z. revised the manuscript. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
Yang Liu – ESSIRI Labs (Personal financial interests), Amy Gallant Sullivan – ESSIRI Labs (Personal financial interests), Lµbris BioPharma (Personal financial interests). Other authors declare no conflict of interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, Y., Shen, Y., Sullivan, A.G. et al. The impact of eyeliner usage on dry eye symptoms. Sci Rep 15, 14039 (2025). https://doi.org/10.1038/s41598-025-96957-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-96957-w