Abstract
Chronic disseminated candidiasis (CDC) is an invasive fungal infection typically affecting patients with hematological diseases and severe neutropenia, associated with increased mortality. However, there is a global shortage of clinical evidence on CDC. We retrospectively analyzed clinical data from 49 CDC patients over the past decade. Clinical characteristics of primary hematological diseases, CDC diagnosis, treatment and response evaluations were included. Clinical factors associated with CDC remission and patients’ survival were analyzed. The majority of patients had hematological malignancies (n = 43, 87.8%), and 27 patients (55.1%) had persistent severe neutropenia for more than 10 days prior to CDC. CT scans revealed liver lesions in 44 patients, spleen lesions in 34 patients, and kidney lesions in 9 patients. Proven, probable and possible CDC was diagnosed in 5 (10.2%), 3 (6.1%) and 41 patients (83.7%), respectively, and treatment outcomes at 3 months included 5 complete response (CR, 10.2%), 34 partial response (PR, 69.4%) and 10 treatment failure (20.4%). Caspofungin treatment showed a trend towards improving CR/PR rate, while severe neutropenia > 20 days and proven diagnosis were significantly associated with 3-month treatment failure. Kaplan–Meier curve showed achieving CR/PR within 3 months did not significantly prolong OS compared to treatment failure patients (1197.6 days vs. 564.8 days, P = 0.074). Additionally, no patient deaths were directly attributed to CDC infection. Age > 45 years old and malignancy non-remission were prognostic factors of overall survival (OS). Furthermore, a prediction model identified severe neutropenia > 20 days, proven/probable diagnosis and concomitant bacteremia as risk factors to effectively predict treatment failure. Also, patients with a risk score < 0.203 in the model exhibited more rapid treatment response. After CDC symptoms onset, lymphocyte levels remained consistently higher in treatment failure patients, while the neutrophil-to-lymphocyte ratio was persistently higher in CR/PR patients. Our findings recommend CT scans for diagnosis and caspofungin as first-line therapy while continuing scheduled chemotherapy or bone marrow transplantation. Notably, risk factors identified by the prediction model could be used to predict treatment response.
Similar content being viewed by others
Introduction
Chronic disseminated candidiasis (CDC), also known as hepatosplenic candidiasis (HSC), is a rare invasive fungal infection occurring in immunocompromised population and patients with hematological disorders, including acute leukemia, aplastic anemia and other hematological conditions. The incidence of CDC has been reported to be 3 to 29% in acute myeloid leukemia (AML) patients1,2,3 and 4.3 to 6.6% in acute lymphoblastic leukemia (ALL) patients4,5. Cases have also been reported in patients with aplastic anemia (AA), lymphoma, myelodysplastic syndrome (MDS) and solid tumor5,6,7. Commonly involved organs are liver, spleen and kidney, and risk factors include central venous catheterization, antibiotic usage, previous bacteremia, severe neutropenia and etc.8,9. Although severe neutropenia is widely recognized as a significant risk factor for CDC8,10, its impact on mortality remains controversial according to different reports2,6,11.
Common symptoms include fever of unknown origin that does not respond to broad-spectrum antibiotics and left upper quadrant tenderness, nausea and vomiting could also occur12,13. Due to the subtility of symptoms, initial diagnosis of CDC in susceptible patients requires mycological (1,3-beta-D-glucan (BDG), T2 Candida) and typical imaging examinations (bull’s eye lesion). Although candidemia within the previous 2 weeks is defined as a clinical criteria for diagnosis by European Organization for Research and Treatment of Cancer/Mycoses Study Group (EORTC/MSG)14, the incidence of prior candidemia remains relatively low, ranging from 29.9 to 56%6,15,16. As for the treatment, the Infectious Diseases Society of America (IDSA)9 recommends initial treatment with amphotericin B or echinocandin for several weeks followed by oral fluconazole, and European Society of Clinical Microbiology and Infectious Diseases (ESCMID)17 suggests the usage of fluconazole or amphotericin B followed by prolonged fluconazole. Nonetheless, both guidelines indicate that treatment recommendations are based on inadequate research results4,13,18,19,20,21. Furthermore, the benefit of steroids is undetermined, as both the IDSA9 and ESCMID17 guidelines only weakly recommend using steroids for fever reduction. Although several previous studies reported resolution of symptoms following steroid therapy16,22, it seems to have no significant impact on improving survival23.
Although CDC has a relatively low incidence rate, it is reported to increase mortality in patients with hematological disorders6,13. Also, CDC researches and related reports are insufficient in China and Asia area. In this retrospective study, we reviewed clinical data of 49 patients diagnosed with possible, probable or proven CDC and documented patients’ characteristics, diagnosis, treatment and analyzed clinical factors for CDC remission and patient survival.
Methods
Patients
We retrospectively reviewed electronic medical record system and collected clinical data of 49 patients diagnosed with CDC at the Institute of Hematology and Blood Diseases Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, between January 2014 and December 2023. Chest CT with upper abdominal cuts were performed in patients with fever of unknown origin. Abdominal CT scans were conducted in patients with abdominal pain or signs of intra-abdominal infection, and some patients also received abdominal ultrasound. Patients with risk factors and imaging results indicating CDC were included. Besides, patients with no symptoms but who received routine examination showing indicative hepatosplenic lesions were also included. Patients were later categorized as having proven, probable or possible CDC dependent on mycological, radiological and biopsy evidence. Severe neutropenia was defined as neutrophil count < 500 cells/µL24. To analyze the impact of immune status on CDC, patients were stratified into two groups based on risk factors at the time of CDC onset. Patients receiving intensive chemotherapy, intensive immunosuppressive therapy (cyclosporin A + anti-thymocyte globulin), prolonged corticosteroid treatment (≥ 0.3 mg/kg corticosteroids for ≥ 3 weeks), or those without neutrophil recovery were classified into the immunosuppressed status group. Patients without these risk factors were classified into the preserved immune status group. This research was approved by the ethical committee of the Institute of Hematology and Blood Diseases Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, and informed consent forms were obtained from all patients.
Diagnosis
The diagnosis of CDC was based on the 2020 EORTC/MSG criteria14. Proven diagnosis was defined as a positive microscopic examination, with or without tissue nucleic acid diagnosis, of candidiasis in a normally sterile site. Probable diagnosis was defined as imaging detection of small, target-like lesions, combined with mycological findings, in patients with susceptibility factors following candidemia within the previous 2 weeks. Patients with positive radiological detection and host factors but no mycological evidence were diagnosed with possible CDC according to criteria of EORTC/MSG14,25 and other previous publications6,16,26.
Treatment and response evaluation
Following probable and possible diagnoses of CDC, patients were treated with antifungal monotherapy (azole, caspofungin or amphotericin B) or combination regimens (azole + amphotericin B, azole + echinocandin, echinocandin + amphotericin B or azole + echinocandin + amphotericin B) depending on the patient’s medication history, physician’s judgment, and the severity of the disease. For patients with proven diagnosis, antifungal treatments were initiated following abnormal imaging results before diagnosis confirmation by biopsy. Treatment response would firstly be evaluated by abdominal CT scans within 3 months following initiation of antifungal, the specific individual follow-up schedule was determined by physicians. Response to antifungal therapy was assessed according to 2008 EORTC/MSG response criteria27. Complete response (CR) was defined as resolution of clinical symptoms, mycological and radiological findings. Partial response (PR) was defined as resolution of symptoms and signs of diseases, with radiological stabilization or improvement. Failure of treatment was defined as patient death or persistent symptoms and mycological signs, or progression of lesions radiologically.
Statistical analysis
IBM SPSS (v.26) and R programming language (v 4.3.3) were used to perform statistical analysis. Quantitative variables were presented as median (range), and categorical variables were expressed as rate and percentage. Kaplan–Meier method and log-rank test were conducted for survival estimation. Logistic regression model and Cox proportional hazards regression model were performed for univariable analyses, clinical factors with a P < 0.05 were selected for multivariable analysis. The prediction model was developed using parameters identified as clinically significant from logistic regression analysis. Discrimination analysis was conducted using the area under the curve (AUC) of the receiver operating curve (ROC). Calibration was evaluated using a biased-corrected calibration curve, generated through 1000 bootstrap re-sampling. The calibration curve was constructed based on the Hommer-Lemeshow goodness-of-fit test. All statistical tests were bidirectional, and statistical significance was determined when P < 0.05.
Results
Baseline patients’ characteristics
Patients’ characteristics were displayed in Table 1. Forty-nine patients (male = 19, female = 30) diagnosed with CDC were included and median age was 23 (2–61) years old. The majority of patients were diagnosed with hematological malignancies (n = 43, 87.8%), including AML (n = 21, 42.9%), ALL (n = 18, 36.7%), MDS (n = 2, 4.1%) and invasive B-cell lymphoma (n = 2, 4.1%), and median ECOG score was 1 (0–3). MDS diagnoses included 1 myelodysplastic syndrome with excess blasts-1 (MDS-EB1) and 1 myelodysplastic syndrome with multilineage dysplasia (MDS-MLD). For invasive B-cell lymphoma, there were 1 diffuse large B-cell lymphoma and 1 high grade B-cell lymphoma, not otherwise specified, transitioned from follicular lymphoma. Six patients suffered from other hematological disorders, including 4 very severe aplastic anemia (VSAA), 1 paroxysmal nocturnal hemoglobinuria (PNH) and 1 clonal cytopenia of uncertain significance (CCUS). The PNH patient was receiving steroids and immunosuppressant for treatment. The CCUS patient had undergone allo-HSCT due to transfusion dependency and pancytopenia refractory to drug therapy, the patient was receiving immunosuppressant at the time of CDC diagnosis. Eleven patients had hematological malignancy with non-remission status. Among the four patients with previous bone marrow transplantation (allo-HSCT = 3, cord blood transplantation = 1), the median duration from transplantation to CDC diagnosis was 386 (129–1116) days, with only one patient receiving immunosuppressants at CDC diagnosis. Among acute leukemia patients (n = 39), 30 were in complete response, 5 had no response, and 4 had relapse after response. More patients with acute leukemia were in the phase of induction chemotherapy (n = 26) compared to intensification chemotherapy (n = 12) and 1 patient had CDC after umbilical blood transplantation. All 4 VSAA patients remained none response after immunosuppressant therapy. Common risk factors were antibiotic exposure within 3 months (n = 41, 83.7%), central venous catheterization (n = 33, 67.3%) and severe neutropenia (n = 30, 61.2%). Median duration of severe neutropenia was 23 (6–138) days and median neutrophil count at CDC diagnosis was 4.25 (0.01–12.65) *109/L. Five patients (10.2%) had confirmed candidemia more than 2 weeks prior to CDC diagnosis, and 32 patients (65.3%) received prior antifungal medications within 3 months as treatment for confirmed or possible fungal infection (n = 29) or solely prophylaxis (n = 3). Number of patients with various hematological disorders diagnosed with CDC from 2014 to 2023 was presented in Fig. 1.
Diagnosis of chronic disseminated candidiasis
Patients’ symptoms, examinations, diagnosis and concomitant infections were presented in Table 2. Symptoms were documented in 42 patients (85.7%), while 7 patients (14.3%) were found to have hepatosplenic lesions during routine CT examinations despite being asymptomatic. CT scan and ultrasound were utilized to assess hepatosplenomegaly, revealing hepatomegaly in 14 cases and splenomegaly in 9 cases. While all patients in this research underwent CT imaging with positive detection, abdominal ultrasound were performed in 37 patients (75.5%), with positive lesions detected in only 22 cases (22/37, 59.5%). CT scans identified more liver (n = 44), spleen (n = 34) and kidney lesions (n = 9) compared to ultrasound (liver = 17, spleen = 12, kidney = 1). Pulmonary lesions were also detected in 18 patients via CT scans. BDG, Candidiasis IgG and IgM tests were performed in 44, 17 and 23 patients, and positive rates were 50.0%, 35.3% and 47.8%, respectively. A total of 6 patients (12.2%) underwent biopsy and microscopic analysis of spleen (n = 1) or liver tissues (n = 5), with tissue nucleic acid diagnosis performed in 4 patients. Invasive candidiasis infection was confirmed in 5 patients by positive microscopic examination, with 3 of whom receiving DNA sequencing to determine fungal species (Candida tropicalis = 2, Candida albicans = 1). In summary, CDC diagnosis was proven in 5 patients (10.2%), probable in 3 patients (6.1%) and possible in 41 patients (83.7%). Candidemia within previous 2 weeks was reported in 8 patients. Two of the 8 patients with candidemia within 2 weeks underwent liver tissue biopsy and their previous blood cultures and hepatic biopsy microbiology results were consistent (Candida tropicalis = 1, Candida albicans = 1). Additionally, concomitant bacteremia of Klebsiella pneumoniae (n = 3), Enterococcus faecium (n = 1), Aeromonas veronii (n = 1), Bacillus cereus (n = 1), Escherichia coli (n = 1) and Enterobacter cloacae (n = 1) was recorded in blood samples from 6 patients. At CDC onset, 25 patients were receiving antifungal therapy, including azole (n = 20) and caspofungin monotherapy (n = 5). Of these, 16 patients were receiving azoles as prophylactic treatment, and 9 patients were receiving antifungal therapy as empirical treatment for suspected fungal infection (caspofungin = 5, azole = 4).
Treatment and clinical outcomes
Treatment and patient outcomes were summarized in Table 3. A smaller proportion of patients were treated initially with antifungal combination (n = 21, 42.9%) compared to antifungal monotherapy (n = 28, 57.1%). Monotherapy regimens included azoles (n = 16, 32.7%), caspofungin (n = 6, 12.2%) and amphotericin B monotherapy (n = 6, 12.2%). Monotherapy with azoles was the most common treatment regimen (n = 16, 32.7%), followed by azole + echinocandin combination treatment (n = 12, 24.5%). Overall, azoles were used in the initial treatment of 33 patients (67.3%), followed by echinocandins (n = 24, 49.0%) and amphotericin B (n = 15, 30.6%). Combined corticosteroid treatment was only utilized in 2 patients. Median time from symptoms onset to treatment initiation was 10 (0–41) days. Thirty-one patients (63.3%) underwent a switch of antifungal regimen, primarily transitioning to azole monotherapy after disease improvement (12/31, 38.7%). Modifications in treatment plans for the remaining 19 patients were due to poor treatment response (n = 17) or adverse effects of amphotericin B (n = 2). Of note, although echinocandin was recommended by IDSA as a first-line treatment, 7 patients developed CDC infection despite having received caspofungin within 3 months prior to CDC diagnosis. Six of these patients were treated with caspofungin monotherapy or combination regimen and all achieved only PR at 3 months. The other one patient initially received voriconazole but later switched to caspofungin and had treatment failure. CT examination was performed in every patient to assess disease response status. At three months following the antifungal treatment, CR, PR and treatment failure rate was 10.2% (n = 5), 69.4% (n = 34) and 20.4% (n = 10). At 6 months, CR and PR rate increased to 16.3% (n = 8) and 71.4% (n = 35), respectively. Median follow-up time from diagnosis was 183 (11–1424) days. No deaths directly related to CDC were observed, and no candidiasis infection relapse was recorded. At the last follow-up, 8 patients had died due to primary disease relapse (n = 4) or bacterial infection (n = 4). The 1-month and 2-month mortality rate was 8.2% (n = 4) and 12.2% (n = 6), respectively. Delayed or modified chemotherapy of primary hematological diseases occurred in 8 patients (16.3%), while no postponements of HSCT were recorded. Five patients (10.2%) received HSCT (auto-HSCT = 1, allo-HSCT = 4) after CDC diagnosis, median time from CDC to transplantation was 70 (31–219) days.
Clinical factors for remission and survival
Clinical factors for response at 3 months was displayed in Table 4. Although risk factors including bacteremia, antibiotic usage, central venous catheterization, severe neutropenia and etc. were reported to increase CDC incidence, they were not found to be associated with treatment failure. Nevertheless, history of persistent severe neutropenia for more than 20 days significantly decreased response in univariate logistic regression analysis (OR = 5.250 (95% CI 1.155–23.856), P = 0.032). Furthermore, univariate analysis also demonstrated that patients with proven diagnosis tended to experience treatment failure or death compared to possible or probable cases (OR = 25.333 (95% CI 2.405–266.803), P = 0.007), while patients with possible CDC commonly responded well to antifungals (OR = 0.083 (95% CI 0.015–0.461), P = 0.004). Initial treatment including caspofungin showed a potential trend towards improving CR/PR rate at 3 months (OR = 0.193 (95% CI 0.036–1.030), P = 0.054), whereas similar effects were not observed in patients treated with azoles or amphotericin. Cox proportional regression model was utilized to evaluate risk factors for 1-month survival and overall survival (OS) (Table 5). In univariable analysis, concomitant bacteremia was found to significantly decrease 1-month survival (HR = 7.281 (95%CI 1.024–51.753), P = 0.047) but not OS (HR = 2.372 (95%CI 0.476–11.822), P = 0.292). Conversely, non-remission status of malignancy significantly increased risk of OS (HR = 5.730 (1.375–23.881), P = 0.017) but not 1-month survival (HR = 3.855 (95% CI 0.546–27.623), P = 0.175). Furthermore, multivariate analysis demonstrated that age > 45 years old predicted poor prognosis at one month (HR = 11.301 (95% CI 1.090–117.149), P = 0.042) and long-term follow-up (HR = 5.756 (95% CI 1.409–23.523), P = 0.015). Patients’ OS was shown in Fig. 2. CR or PR at 3 months had a trending effect in improving OS (1197.6 (1010.0–1385.3) days vs. 564.8 (322.6–807.0) days in treatment failure patients, P = 0.074), 3-month OS rate was 92.3% (36/39) and 70.0% (7/10) in CR/PR and treatment failure patients, respectively (P = 0.168).
Model development and performance analysis
Clinical factors with a P value < 0.1, selected from univariable logistic regression analysis for 3-month treatment response, were used to construct a model for predicting patients’ response to CDC treatment. To ensure the model’s applicability at the time of diagnosis, only factors available prior to and at the point of diagnosis were included. The factors included in the model were neutropenia > 20 days (P = 0.032), possible diagnosis (p = 0.004) and concomitant bacteremia (p = 0.074). Proven diagnosis (P = 0.007) was excluded from the analysis due to its strong correlation with the factor possible diagnosis. The AUC for the model including all parameter (Fig. 3A) was 0.8551 (95%CI 0.7134–0.9968), indicating good discriminative ability. The calibration curve (Fig. 3B) showed consistency between predicted and actual probability. The formula constructed from logistic regression model was utilized to calculate risk score for patients as follows:
Performance of the prediction model. (A) AUC for the model including all factors was 0.8551. The AUC for the model including single factor of neutropenia > 20 days, possible diagnosis and concomitant bacteremia was 0.6962, 0.7115 and 0.6115, respectively. (B) The calibration curve indicated agreement between predicted and actual survival outcomes. (C) Time from treatment to CDC remission of patients with a risk score ≥ 0.203 versus those with a risk score < 0.203.
The risk score was calculated for every patient and ranged from 0.0379 to 3.342. Univariable logistic regression analysis demonstrated that higher risk score significantly predicted treatment failure at 6 months (OR = 2.134 (95% CI 1.104–4.127), P = 0.024), thereby validating the effectiveness of the model. In addition, we further investigated association between the risk score and time to CDC remission. The third quartile of the calculated risk scores, 0.203, was selected as the cutoff value, and patients with a risk score < 0.203 exhibited significantly reduced time to CR or PR (61.9 (95% CI 42.7–81.1) days vs. 108.3 (95% CI 67.7–148.8) days, P = 0.020) (Fig. 3C).
Immune response patterns in CDC
For patients with available neutrophil data, at 20 days prior to CDC diagnosis, 23 patients (23/36, 63.9%) were in severe neutropenia status, which decreased to 11 patients (11/43, 25.6%) at 10 days prior to CDC, and 9 patients (9/49, 18.4%) at diagnosis. Among patients who were in severe neutropenia 10 days prior to CDC diagnosis but had recovered neutrophil levels at the time of diagnosis, all 8 (100%) presented with symptoms, compared to 33/41 (82.9%) of other patients (P = 0.478). These patients also had a lower CR/PR rate at 3 months (62.5% vs. 82.9% in other patients), although logistic regression did not show a significant association (OR = 0.343 (95% CI 0.066–1.780), P = 0.203). C-reactive protein levels, tested in 32 patients (after excluding concomitant bacteremia), showed no significant difference between patients with neutrophil recovery (n = 3, 68.703 ± 53.156 mg/L) and those without (n = 29, 68.273 ± 67.806 mg/L, P = 0.974). Moreover, patients were stratified based on immune status at CDC diagnosis for analysis. Immunosuppressed status group (n = 13) included 11 possible (84.6%), 1 probable (7.7%) and 1 proven CDC (7.7%). Preserved immune status groups (n = 36) included 30 possible (83.3%), 2 probable (5.6%) and 4 proven CDC (11.1%). No significant significance in diagnostic category was found (P = 0.913). Immunosuppressed patients had lower CR/PR rate at 3 months (69.2% vs. 83.3% in preserved immune status group), while statistical significance was not found (OR = 0.450 (95% CI 0.104–1.954), P = 0.286). Thirty-day mortality was also higher in immunosuppressed patients (15.4%) compared to patients with preserved immune status (5.5%), while cox regression analysis did not show significance (HR = 2.941 (95%CI 0.414–20.882), P = 0.281). Neutrophil and lymphocyte counts were further analyzed at symptom onset, imaging, and 10, 20, and 30 days post-imaging, categorized by remission status (Fig. 4A). Neutrophil counts fluctuated in both remission and treatment failure groups, with no distinct pattern (Fig. 4B). However, lymphocyte counts were consistently higher in the treatment failure group across all time points, suggesting potential immune activation or unresolved inflammation in these patients (Fig. 4C). Neutrophil to lymphocyte ratio (NLR) values were higher in remission patients persisted over time (Fig. 4D), and at the initial imaging, the median NLR was 0.555 in treatment failure patients compared to 2.79 in remission patients, with the difference approaching significance (P = 0.080).
Neutrophil and lymphocyte counts in patients with remission and treatment failure. (A) Neutrophil and lymphocyte count values (109/L) at different time points in patients grouped by remission status. Neutrophil count (B), lymphocyte count (C) and neutrophil-to-lymphocyte ratio (D) in patients with complete response (CR)/partial response (PR) and no response (NR) at various time points.
Discussion
As a rare invasive fungal infection, CDC commonly complicates patients with hematological malignancies or immunocompromising diseases. The overall incidence of CDC has been reported to range from 1.53 to 3% in hematological centers6,28. It is possible that CDC incidence has decreased in recent years due to the widespread use of antifungal prophylaxis, as evidenced by the reduction in incidence compared to the last century (3–29%)1,3. Recent history of severe neutropenia was a common risk factor (n = 30, 61.2%) in our study, with a median duration of 23 (6–138) days. Most patients had neutropenia recovery and only 9 patients remained in severe neutropenia status at CDC diagnosis. This seemingly paradoxical phenomenon of concomitant CDC infection and neutrophil recovery was consistent with previous studies16,26,29,30 and was hypothesized to reflect the two-phase development of CDC. First, during neutropenia and in the presence of other risk factors, Candida may translocate across mucosal barrier and spread hematogenously to deep organs, potentially remaining asymptomatic. Second, following neutrophil recovery, ongoing fungal infection, combined with immune reconstitution inflammatory response (IRIS), results in the clinical manifestation of CDC28,29,31. Overall, proven, probable and possible CDC was diagnosed in 5 (10.2%), 3 (6.1%) and 41 (83.7%) patients, respectively. The rate of probable diagnosis was relatively low, ranging from 0 to 21.3% in recent researches2,5,6,26. In our study, the limited number of probable diagnoses was attributed to the relatively low rates of BDG positivity (50% in 44 tested patients) and candidemia within the preceding 2 weeks (n = 8), whereas another 5 patients had candidemia more than 2 weeks prior to CDC diagnosis. Several previous studies have raised concerns regarding the sensitivity and specificity of BDG in diagnosing invasive candidiasis, emphasizing the need for caution when interpreting negative results32,33. Nonetheless, while admitting its low sensitivity, Guitar et al.34 recommended monitoring BDG for treatment planning as it correlated with invasive candidiasis outcomes.
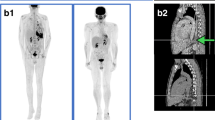
Ultrasound showed suboptimal sensitivity in our research, as CT scans identified involvement of more organs in 24 out of the 37 patients who underwent both CT and ultrasound examinations. Previous reports have also suggested that ultrasound may lack accuracy and its effectiveness could depend on physicians’ awareness of patients’ clinical susceptibility2,35. Unfortunately, no patient received PET-CT scans for CDC detection in our study, even though the novel utilization of this technology in diagnosis and follow-up was encouraged by some researches as it could detect lesions unapparent on CT scans and assist in designing suitable antifungal treatment16,36,37,38. A recent clinical trial compared conventional imaging and PET-CT and concluded that PET-CT could not replace conventional imaging for the initial assessment of CDC but might be used for discontinuation of antifungal after 3 months39. Although IDSA9 and ESCMID17 recommended monotherapy with azole, caspofungin or amphotericin B, based on low-quality evidence, these guidelines did not explicitly specify either the choice of antifungal agents or whether monotherapy is preferable to combination treatment. In our research, a strong trend toward CR/PR at 3 months was observed in patients treated with caspofungin (OR = 0.193 (95% CI 0.036–1.030), P = 0.054), while such effects were not demonstrated in patients receiving azoles or amphotericin B. Several systemic reviews comparing efficacy between caspofungin and other antifungals have prioritized caspofungin for the treatment of invasive candidiasis40, but evidence regarding its utilization in CDC still remained to be studied. Furthermore, 3-month response, 1-month survival and OS were of no difference between patients receiving monotherapy or combination treatment. Median time to response was 46 (13–319) days and patients were sequentially treated with oral azoles after improvement or discharge until full radiological and symptomatic resolution. To sum up, our results recommend CT scans for diagnosis and suggest that monotherapy or combination therapy including caspofungin could be potentially beneficial for CDC remission and should be followed by long-term oral antifungal therapy. However, further researches are required for confirmation.
Age ≥ 45 was identified as a prognostic factor for 1-month and overall mortality by multivariable Cox regression analysis, consistent with previous reports revealing a negative association between older age and OS in CDC6, or 1-month mortality in candidemia7. Our results showed hematological malignancy non-remission did not have significant impact on 1-month survival, while this factor significantly decreased OS (HR = 5.730 (95% CI 1.375–23.881), P = 0.017), supporting conclusion from prior researches6,11. Combined with our observation that no patient died directly from CDC infection and there was no significant difference in survival between patients achieving CR/PR or experiencing treatment failure, the data suggested that treatment of primary disease was of higher urgency for patients’ long-term survival. The delay or modification of chemotherapy occurred in 16.3% (n = 8) of cases in our study, compared to 13.8% and 79% in previous studies6,11. Four of the 8 patients remained unresponsive to primary disease treatment at the last follow-up, with one death due to malignancy relapse. Although Cox regression analysis of our data did not demonstrate significance, the impact of delayed treatment on survival outcome was widely recognized by researchers4,16,28. Therefore, in accordance with IDSA guideline, we recommend continuing chemotherapy or bone marrow transplantation while receiving treatment or monitoring for CDC.
Furthermore, a prediction model that exhibited strong discrimination and calibration was developed. The prediction model constructed using risk factors selected from logistic analysis is, to our knowledge, the first model to evaluate treatment response in CDC. Our model demonstrated an association between severe neutropenia, concomitant bacteremia, diagnosis type and treatment response. Of particular concern were patients presenting with both severe neutropenia > 20 days and concomitant bacteremia, who exhibited poor responses to antifungals within 6 months (OR = 10.250, (95% CI 1.122–93.678), P = 0.039), coupled with a significant decrease in OS (627.3 (45.4–1209.1) days vs. 1186.6 (1006.0–1367.3) days, P = 0.034). The study revealed a notable contrast in treatment outcomes based on the diagnostic certainty of CDC. While possible diagnosis of CDC was found to predict positive treatment responses, proven/probable diagnosis was associated with unfavorable outcomes, with no patient achieving CR at evaluation within 3-month. Specifically, among the 5 patients diagnosed with proven CDC, four experienced PR, while 1 patient had treatment failure at 3 months. Among the 3 patients with probable CDC diagnosis, two achieved PR and 1 experienced treatment failure at 3 months. These findings suggest biopsy could enhance diagnostic and prognostic accuracy, but healthcare providers must carefully balance these benefits against the inherent risks and potential complications associated with biopsy procedure. Unfortunately, due to CDC’s rarity and the limited clinical data from a single center, we were unable to include more cases or conduct external validation tests of the prediction model. Prospective researches and clinical trial are needed to improve antifungal treatment and verify related risk factors. Moreover, considering the diagnostic and prognostic benefits, the role of biopsy warrants further exploration.
The EORTC/MSG criteria for possible CDC raise concern about misclassification in diagnosis, treatment and research. At our institution, CDC was diagnosed collaboratively by experienced radiologists and physicians. In comparison to other studies, except one on pediatric CDC using 2008 guideline (where a single positive β-D-glucan is sufficient for a probable diagnosis)16, other studies all reported relatively high proportion of possible CDC (65.7%–78.3%)5,6,26. Our study found 43.9% of possible CDC patients had at least one episode of β-D-glucan positivity, and 3 had candidemia within 2 weeks. Additionally, 87.8% of patients with possible CDC achieved CR/PR within 3 months of antifungal therapy, reinforcing the validity of CDC diagnosis. The reasons for relatively low number of proven and probable CDC diagnoses included: biopsy confirmation was often not performed due to financial constraints faced by patients and the invasive nature of the procedure; the 2020 EORTC/MSG guideline requires stricter mycological criteria for probable CDC14, including T2Candida or at least two consecutive β-D-glucan positivity. However, β-D-glucan test was not routinely tested and repeated for every patient and T2Candida was not available at our institution. Besides, empirical treatment or prophylaxis were initiated prior to mycological examination in many patients. Additionally, for the concomitant bacteremia detected in 6 patients, one patient underwent biopsy, which ruled out bacterial abscess, supporting a CDC diagnosis. The remaining 5 patients were diagnosed with CDC based on specific imaging features and β-D-glucan positivity (4/5 cases), with clinical responses to antifungal treatment further supporting the diagnosis (3/5 CR/PR cases). Although histopathology remains the gold standard and its limited feasibility means we cannot completely exclude non-fungal abscesses, but the overall evidence favors CDC diagnosis. We believe the rigorous inclusion and exclusion process, combined with biomarker correlation and clinical response, support the validity of the CDC diagnosis and reduces misclassification risks. Despite limitations, we believe that adherence to the EORTC/MSG guidelines remains essential for cross-study comparisons and guiding early empirical therapy in clinical practice.
IRIS following invasive fungal infection has been reported in some studies41,42,43, but its exact mechanism and pathogenesis in CDC remained underexplored. Due to the abnormal immune and inflammatory status involved in IRIS, several studies utilized steroids for CDC treatment22,29,44. In our cohort, only 2 patients received steroids, and no significant impact on treatment response was observed. Besides, while no significant differences of C-reactive protein, treatment response and clinical outcomes were observed between patients stratified as having immunosuppressed status and preserved immune status, our findings suggest that neutrophil recovery may be associated with an increased likelihood of CDC symptoms and a potentially lower response to treatment. Previous studies showed that neutrophil recovery often coincided with IRIS and disease deterioration45,46, while IRIS was also reported in neutropenic patients47. On the other hand, lymphocytes reconstitution was widely discussed in the context of fungal infections in HIV patients, but data remained insufficient in the field of Candida infection. One previous research has demonstrated elevated neutrophil and monocyte counts in CDC patients, along with increased T-cell activation compared to neutropenic patients controls, although the number of Candida-specific T cells was not significantly different between the two groups48. Additionally, single nucleotide polymorphism in interleukin-1B, an important cytokine involved in T cell activation and inflammatory response, was significantly associated with IRIS-CDC development43. These findings suggest that both the quantity and function of immune cells may contribute to CDC. They also partially align with a hypothesis proposing that IRIS in CDC may stem from Th1/Th17-driven pro-inflammation following neutropenia recovery, with insufficient regulation by Th2/Treg cells28. In our cohort, the observation of elevated lymphocytes and reduced NLR in treatment failure patients may reflect similar immune dysregulation, where abnormal lymphocyte activation or impaired neutrophil-mediated regulation of inflammation could contribute to worse clinical outcome. However, due to the limited number of studies on CDC given its rarity, along with the restricted data on cytokine profiles, immune cell subsets, and their functions in our cohort, we are unable to draw definitive mechanistic conclusions. Further studies could incorporate more comprehensive markers of infection, inflammation and immune status to better understand the dynamic immune changes during CDC development and refine treatment strategies.
In conclusion, this retrospective study reviewed clinical data, treatment planning and clinical factors for remission and survival in 49 CDC patients diagnosed in the past 10 years, offering perspectives into the epidemiology, disease characteristics and treatment response for both researchers and physicians. Our findings suggest the use of CT scans for diagnosis and recommend caspofungin as first-line therapy while continuing scheduled chemotherapy or bone marrow transplantation. Notably, risk factors including proven/probable diagnosis, severe neutropenia > 20 days and concomitant bacteremia could be used to predict treatment failure.
Data availability
The data is available from the corresponding authors on reasonable request.
References
Blade, J. et al. Chronic systemic candidiasis in acute leukemia. Ann. Hematol. 64(5), 240–244 (1992).
Chang, H., Kuo, M. C., Tang, T. C., Lin, T. L. & Wu, J. H. Clinical feature, image findings and outcome of hepatosplenic candidiasis in patients with acute myeloid leukemia. Biomed. J. 44(6 Suppl 2), S252–S257 (2021).
Sallah, S. et al. Hepatosplenic candidiasis in patients with acute leukaemia. Br. J. Haematol. 106(3), 697–701 (1999).
Chen, C. Y. et al. Hepatosplenic fungal infection in patients with acute leukemia in Taiwan: Incidence, treatment, and prognosis. Ann. Hematol. 82(2), 93–97 (2003).
Chen, C. Y. et al. Chronic disseminated candidiasis manifesting as hepatosplenic abscesses among patients with hematological malignancies. BMC Infect. Dis. 19(1), 635 (2019).
Boussen, I. et al. Hepatosplenic candidiasis in patients with hematological malignancies: A 13-year retrospective cohort study. Open Forum Infect. Dis. 9(4), ofac088 (2022).
Bergamasco, M. D., Garnica, M., Colombo, A. L. & Nucci, M. Epidemiology of candidemia in patients with hematologic malignancies and solid tumours in Brazil. Mycoses 56(3), 256–263 (2013).
Kontoyiannis, D. P., Luna, M. A., Samuels, B. I. & Bodey, G. P. Hepatosplenic candidiasis. A manifestation of chronic disseminated candidiasis. Infect. Dis. Clin. North Am. 14(3), 721–739 (2000).
Pappas, P. G. et al. Clinical practice guideline for the management of candidiasis: 2016 update by the infectious diseases society of America. Clin. Infect. Dis. 62(4), e1-50 (2016).
Sallah, S., Wan, J. Y., Nguyen, N. P., Vos, P. & Sigounas, G. Analysis of factors related to the occurrence of chronic disseminated candidiasis in patients with acute leukemia in a non-bone marrow transplant setting: A follow-up study. Cancer 92(6), 1349–1353 (2001).
De Castro, N. et al. Hepatosplenic candidiasis in the era of new antifungal drugs: A study in Paris 2000–2007. Clin. Microbiol. Infect. 18(6), E185–E187 (2012).
Thaler, M., Pastakia, B., Shawker, T. H., O’Leary, T. & Pizzo, P. A. Hepatic candidiasis in cancer patients: The evolving picture of the syndrome. Ann. Intern. Med. 108(1), 88–100 (1988).
Pagano, L. et al. Chronic disseminated candidiasis in patients with hematologic malignancies. Clinical features and outcome of 29 episodes. Haematologica 87(5), 535–541 (2002).
Donnelly, J. P. et al. Revision and update of the consensus definitions of invasive fungal disease from the European organization for research and treatment of cancer and the mycoses study group education and research consortium. Clin. Infect. Dis. 71(6), 1367–1376 (2020).
van Prehn, J. et al. Hepatosplenic candidiasis without prior documented candidemia: An underrecognized diagnosis?. Oncologist 22(8), 989–994 (2017).
Madney, Y. et al. Clinical features and outcome of hepatosplenic fungal infections in children with haematological malignancies. Mycoses 63(1), 30–37 (2020).
Ullmann, A. J. et al. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: Adults with haematological malignancies and after haematopoietic stem cell transplantation (HCT). Clin. Microbiol. Infect. 18(Suppl 7), 53–67 (2012).
Poon, L. M., Chia, H. Y., Tan, L. K., Liu, T. C. & Koh, L. P. Successful intensive chemotherapy followed by autologous hematopoietic cell transplantation in a patient with acute myeloid leukemia and hepatosplenic candidiasis: Case report and review of literature. Transpl. Infect. Dis. 11(2), 160–166 (2009).
Queiroz-Telles, F. et al. Micafungin versus liposomal amphotericin B for pediatric patients with invasive candidiasis: Substudy of a randomized double-blind trial. Pediatr. Infect. Dis. J. 27(9), 820–826 (2008).
Kanji, J. N. et al. Treatment of invasive candidiasis in neutropenic patients: Systematic review of randomized controlled treatment trials. Leuk. Lymphoma 54(7), 1479–1487 (2013).
Cornely, O. A., Marty, F. M., Stucker, F., Pappas, P. G. & Ullmann, A. J. Efficacy and safety of micafungin for treatment of serious Candida infections in patients with or without malignant disease. Mycoses 54(6), e838–e847 (2011).
Shkalim-Zemer, V. et al. Response of symptomatic persistent chronic disseminated candidiasis to corticosteroid therapy in immunosuppressed pediatric patients: Case study and review of the literature. Pediatr. Infect. Dis. J. 37(7), 686–690 (2018).
Jang, Y. R. et al. Clinical characteristics and outcomes of patients with chronic disseminated candidiasis who need adjuvant corticosteroid therapy. Med. Mycol. 56(6), 782–786 (2018).
Boxer, L. & Dale, D. C. Neutropenia: Causes and consequences. Semin. Hematol. 39(2), 75–81 (2002).
De Pauw, B. et al. Revised definitions of invasive fungal disease from the European organization for research and treatment of cancer/invasive fungal infections cooperative group and the national institute of allergy and infectious diseases mycoses study group (EORTC/MSG) consensus group. Clin. Infect. Dis. 46(12), 1813–1821 (2008).
Cohen, N., Orenbuch-Harroch, E., Olshtain-Pops, K., Lachish, T. & Korem, M. Epidemiology, clinical characteristics and risk factors for severity of chronic disseminated candidiasis in Jerusalem, Israel. Mycopathologia 188(6), 873–883 (2023).
Segal, B. H. et al. Defining responses to therapy and study outcomes in clinical trials of invasive fungal diseases: Mycoses study group and European organization for research and treatment of cancer consensus criteria. Clin. Infect. Dis. 47(5), 674–683 (2008).
Rammaert, B., Desjardins, A. & Lortholary, O. New insights into hepatosplenic candidosis, a manifestation of chronic disseminated candidosis. Mycoses 55(3), e74-84 (2012).
Chaussade, H. et al. Usefulness of corticosteroid therapy during chronic disseminated candidiasis: Case reports and literature review. J. Antimicrob. Chemother. 67(6), 1493–1495 (2012).
Legrand, F. et al. Adjuvant corticosteroid therapy for chronic disseminated candidiasis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 46(5), 696–702 (2008).
Colin-Benoit, E., Kalubi, M. & Zimmerli, S. A case of chronic disseminated candidiasis in metamizole-induced neutropaenia. Infection 51(3), 775–778 (2023).
Christner, M. et al. The added value of (1,3)-beta-D-glucan for the diagnosis of Invasive candidiasis in ICU patients: A prospective cohort study. Infection 52(1), 73–81 (2024).
Lee, Y. W. et al. Clinical sensitivity of the (1–3)-β-D-glucan test for predicting candidemia. Ann. Lab. Med. 43(4), 381–385 (2023).
Guitard, J. et al. Usefulness of ss-D-glucan for diagnosis and follow-up of invasive candidiasis in onco-haematological patients. J. Infect. 76(5), 483–488 (2018).
Anttila, V. J. et al. Hepatosplenic yeast infection in patients with acute leukemia: A diagnostic problem. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 18(6), 979–981 (1994).
Xu, B. et al. Utility of FDG PET/CT in guiding antifungal therapy in acute leukemia patients with chronic disseminated candidiasis. Clin. Nucl. Med. 35(8), 567–570 (2010).
Teyton, P. et al. Hepatosplenic candidiasis imaged with F-18 FDG PET/CT. Clin. Nucl. Med. 34(7), 439–440 (2009).
Hot, A. et al. Diagnostic contribution of positron emission tomography with [18F]fluorodeoxyglucose for invasive fungal infections. Clin. Microbiol. Inf. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 17(3), 409–417 (2011).
Rammaert, B. et al. Does 18F-FDG PET/CT add value to conventional imaging in clinical assessment of chronic disseminated candidiasis?. Front. Med. 9, 1026067 (2022).
Tang, B. H. E., Bay, J. W., Yeong, F. M. & Samuel, M. Efficacy and safety of echinocandin monotherapy and combination therapy for immunocompromised patients with systemic candidiasis: A systematic review and meta-analysis. J. Mycol. Med. 33(2), 101362 (2023).
Pourbaix, A. et al. “Chronic disseminated aspergillosis,” a novel fungal immune reconstitution inflammatory syndrome. Open Forum Infect. Dis. 7(11), ofaa175 (2020).
Dellière, S. et al. Understanding pathogenesis and care challenges of immune reconstitution inflammatory syndrome in fungal infections. J. Fungi 4(4), 139 (2018).
Rammaert, B. et al. A Functional polymorphism in IL-1B Is associated with immune reconstitution inflammatory syndrome of chronic disseminated candidiasis. Open Forum Infect. Dis. 10(3), ofad078 (2023).
Legrand, F. et al. Adjuvant corticosteroid therapy for chronic disseminated candidiasis. Clin. Infect. Dis. 46(5), 696–702 (2008).
Miceli, M. H. et al. Immune reconstitution inflammatory syndrome in cancer patients with pulmonary aspergillosis recovering from neutropenia: Proof of principle, description, and clinical and research implications. Cancer 110(1), 112–120 (2007).
Antinori, S. et al. Immune reconstitution inflammatory syndrome associated with Aspergillus terreus pulmonary infection in an autologous stem cell transplant recipient. Transpl. Infect. Dis. Off. J. Transpl. Soc. 12(1), 64–68 (2010).
Jung, J. et al. Immune reconstitution inflammatory syndrome in neutropenic patients with invasive pulmonary aspergillosis. J. Infect. 70(6), 659–667 (2015).
Candon, S. et al. Chronic disseminated candidiasis during hematological malignancies: An immune reconstitution inflammatory syndrome with expansion of pathogen-specific T helper type 1 cells. J. Infect. Dis. 221(11), 1907–1916 (2020).
Acknowledgements
All authors would like to express appreciation to all the patients for their cooperation.
Funding
This work was supported by Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2021-I2M-1-017; 2023-I2M-2-007, 2021-I2M-1-060), National Natural Sciences Foundation of China (82470208), National Key R&D Program of China (2024YFC2510500), Beijing Xisike Clinical Oncology Research Foundation (Y-SYBLD2022RWR-0017), Special Fund Project for Science and Technology Innovation Strategy of Nanjing (YKK21273), Research Personnel Cultivation Programme of Zhongda Hospital Southeast University (CZXM-GSP-RC20).
Author information
Authors and Affiliations
Contributions
S.F and X.C designed the study and revised the manuscript. Z.C collected, analyzed the data and wrote the manuscript. S.Z, J.S, T.Z, Y.S, W.G collected the data. L.Z analyzed the data. Y.Z, F.Z, Y.M, L.Q, X.Z, E.J, M.H, Z.X, J.W, S.F provided patients to study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This research was approved by the ethical committee of the Institute of Hematology and Blood Diseases Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College (reference number: IIT2022071-EC-1), and informed consent forms were obtained from all patients. The study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, Z., Zhen, S., Sun, J. et al. Clinical characteristics and treatment response of chronic disseminated candidiasis in patients with hematological disorders. Sci Rep 15, 12868 (2025). https://doi.org/10.1038/s41598-025-97004-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-97004-4