Abstract
The in-house ELISA SARS-CoV-2 serological assay, developed by the Armauer Hansen Research Institute (AHRI) in Ethiopia, measures anti-SARS-CoV-2 receptor binding domain (RBD) antibodies. This study aimed to compare the performance of our cost-effective in-house ELISA with two established commercially available SARS-CoV-2 antibody detection assays during the pre-Omicron COVID-19 pandemic. In April 2021, serum samples were collected from 1441 students across 60 schools in Oromia, from 15 hotspot districts and towns. Socio-demographic data were gathered using CSentryCSProDataEntry7.2.1. Performance agreements between AHRI’s in-house ELISA and the two commercial assays were analyzed in these serum samples. Statistical analyses, including Cohen’s kappa (κ), overall percentage agreement, positive percent agreement (PPA), and negative percent agreement (NPA), were performed using STATA software. Diagnostic parameters were presented with 95% confidence intervals (CI), calculated using the Clopper-Pearson method. The performance comparison of the in-house ELISA showed substantial agreement with the two commercial assays. The overall concordance rate between in-house ELISA and Elecsys CLIA was 80.8% (95% CI 75.0–86.5), while the agreement between in-house ELISA and the Rapid LFA test (IgG + IgM) was 75.8% (95% CI 70.1–81.5). The kappa coefficients were: in-house ELISA vs. Elecsys CLIA (κ = 0.61, 95% CI 0.55–0.67), in-house ELISA vs. Rapid LFA test (IgG + IgM) (κ = 0.52, 95% CI 0.46–0.58), and Elecsys CLIA vs. Rapid LFA test (IgG + IgM) (κ = 0.73, 95% CI 0.67–0.78). The in-house ELISA demonstrated strong agreement with the Elecsys CLIA, showing a PPA of 81.7% and an NPA of 80.1%. Compared to the Rapid LFA test (IgG + IgM), which had a PPA of 83% and an NPA of 70.4%, the in-house ELISA exhibited better overall agreement with Elecsys CLIA. This study’s findings indicate substantial agreement between the in-house ELISA and Elecsys. However, only modest agreement was observed between the in-house ELISA and the rapid test (IgG + IgM). Together, these results suggest the utility of the in-house ELISA as a cost-effective tool for sero surveillance studies and monitoring the effect of interventions in resource-poor settings.
Similar content being viewed by others

Introduction
Children are less likely than adults to be infected and develop severe disease by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)1,2. Throughout the COVID-19 pandemic, serological assays have been essential in guiding pandemic responses3. Serological assays have multiple clinical applications, such as analyzing the immune response, detecting asymptomatic cases, and identifying individuals with potential immunity4.
Various SARS-CoV-2 binding antibody assays have been developed, targeting different antigens and utilizing various assay formats5. Serological assays are particularly effective in the later stages of infection when the RT-PCR results may be inconclusive6. Specific antibodies such as IgM, IgA, and IgG serve as diagnostic markers during this phase, appearing within 5–15 days of infection. While IgM and IgA antibodies generally remain detectable for 3–6 weeks, IgG antibodies can persist for several months7. Therefore, IgG antibodies can be valuable for the diagnosis of past infections.
Most serological assays target the receptor-binding domain (RBD) of the spike (S) protein, S protein, nucleocapsid (N) protein, or a combination of these antigens due to their high expression and immunogenicity8,9. Serological assays use various methodologies, including Enzyme-Linked Immunosorbent Assay (ELISA), Chemiluminescent Immunoassay (CLIA), and lateral flow immunoassay (LFIA)10. LFIAs are quick but less sensitive, making them ideal for rapid testing11. ELISA and CLIA offer higher sensitivity and the ability to test multiple samples simultaneously. Although CLIA provides more precise quantification, it is also more expensive compared to ELISA12,13.
While data on the early immune response and seroconversion are limited, the available binding antibody assays vary significantly, despite ongoing research on their clinical relevance and performance5,14,15. Despite increasing use in SARS-CoV-2 seroprevalence research, qualitative antibodies can be challenging to interpret and apply for clinical and public health decision-making16,17,18. Due to the varying levels of sensitivity and specificity among assays, interpreting serology results requires caution. In this study, we used multiple detection methods to compare SARS-CoV-2 antibody test results from a sample of children across 60 schools in the Oromia Region. The three assays compared included: in-house ELISA anit-SARS-CoV-2 RBD, developed by Armauer Hansen Research (AHRI) and Oregon Health and Sciences University (OHSU), hereafter called in-house ELISA19, the Elecsys® anti-SARS-CoV-2 anti-nucleocapsid assay (Roche Diagnostics, Basel, Switzerland)20, and a pan-Ig Rapid LFA test kit (Hangzhou Covid-19 IgG/IgM rapid test device)21. The in-house ELISA detects antibodies against the RBD of the SARS-CoV-2 spike protein, specifically targeting IgG in serum or plasma specimens. This assay has a reported sensitivity of 100% when analyzing serum samples collected two weeks after symptom onset, with a specificity of 97.7% in pre-pandemic samples19. In contrast, the Elecsys CLIA anti-SARS-CoV-2 assay, which detects anti-nucleocapsid antibodies using the Cobas 6000 e601 system, has a specificity of 99.80% and a sensitivity of 99.5% in samples collected more than 14 days after PCR confirmation22. The Rapid LFA test (IgM & IgG) demonstrated a sensitivity of 96.7% and a specificity of 93.7%11. Antibody tests possess the potential to elucidate prior SARS-CoV-2 infections within populations, and may subsequently facilitate the assessment of immune responses to vaccination.
Furthermore, antibody assays can contribute to the clinical diagnosis of COVID-19 patients in instances where qRT-PCR yields negative results despite a strong clinical suspicion. The present study entails a comparative evaluation of an in-house ELISA to determine its utility for SARS-CoV-2 testing. It used samples collected before the omicron pandemic, in parallel with two commercially available antibody assays that utilize different assay formats and directed at several antigens.
Methods
Study design and settings
A longitudinal, school-based cohort study was conducted between December 2020 and April 2021 in hotspot zones and towns of the Oromia Region in Ethiopia before the emergence of the omicron variant23. The Armauer Hansen Research Institute (AHRI), Additionally, engages in disease and genomic surveillance, and policy studies, and provides training across various research and development programs in collaboration with both domestic and international research institutes.
Human sera (n = 1441) for this study were collected in December 2021 from students at 60 randomly selected schools in the top 15 hotspot areas within the Oromia Region, encompassing eight zones and seven town administrations.
Data collection and laboratory procedures
In April 2021, a standardized questionnaire was used to collect demographic data, information on COVID-19-related symptoms, and details about prevention practices. To ensure accuracy and efficiency, the data collectors, sample collectors, and supervisors underwent two days of training: one day focused on the survey tools and another on the laboratory components. The questionnaires were pre-tested before implementation, and investigators supervised the supervisors and data collectors throughout the process. The collected data were promptly sent online to the central server at Oromia Health Bureau for storage. Additionally, GPS coordinates were recorded for all schools.
Blood specimen collection and laboratory antibody testing
Specimen collection, transportation and storage
Approximately 5 ml venous blood was collected in a serum separator tube (SST) following standard laboratory practices and the manufacturer’s instructions. The collected serum was stored at − 20 °C or below until it was ready for use, with care taken to avoid repeated freezing and thawing cycles. When shipping the specimens, they were packaged and labelled correctly per local and international regulations for transporting clinical specimens and pathogenic agents. The in-house ELISA and Rapid LFA Test (IgM and IgG) were performed on similar freeze–thaw serum samples in duplicates. Due to the unavailability of the reader for Elecsys CLIA at the Adam Regional Laboratory, frozen aliquots were shipped to Jimma University. Consequently, the testing of freshly thawed serum samples in duplicates using CLIA was conducted at Jimma University.
Serological methods
To evaluate the concordance of the in-house ELISA developed at AHRI, Addis Ababa, Ethiopia with two commercial serological assays: the Hangzhou Covid-19 IgG/IgM rapid test device (Hangzhou Biotest Biotech Co., Ltd., Hangzhou, China); and the Elecsys CLIA (Roche Diagnostics, Basel, Switzerland), all 1,441 serum samples were tested for the presence of anti-SARS-CoV-2 antibodies using these three assays in duplicates in April 2021. The commercial serological assays were performed according to manufacturers’ protocols, while the in-house ELISA testing followed previously described procedures19. Testing of the serum samples using in-house ELISA and Rapid LFA Test (IgM and IgG) were performed at the Adma Regeion Laboratory in similar freeze–thaw serum samples in duplicates. However, due to the unavailability of the reader for Elecsys CLIA at the Adam Regional Laboratory, frozen aliquots were shipped to Jimma University. Consequently, the testing of freshly thawed serum samples in duplicates using CLIA was conducted at Jimma University.
In-house AHRI ELISA
The in-house indirect ELISA is semi-quantitative and measures serum immunoglobulin G (IgG) against the RBD of the SARS-CoV-2 spike protein. Optimization and validation of this assay were performed using pre-pandemic sera collected between 2012 and 2018 and plasma or serum samples collected from confirmed COVID-19 at different time points post-onset of symptoms19. The present serum samples were tested following the previously described in-house indirect ELISA procedures19. Briefly, the microtiter plates were coated with purified recombinant proteins of receptor binding domain of the spike protein of SARS-CoV-2 (100 μl/well) diluted in phosphate-buffered saline, PBS (pH 7.4) at concentration 1 μg/mL and incubated overnight at 4 °C. Next day, excess unbound antigen was removed and thereafter microtiter plates were blocked with 300 μl/well of 4% skimmed milk with PBS plus 0.1% Teween-20 (w/v) for 2 h at room temperature (RT). Following the blocking step, microtiter plates were washed 3X with PBS plus 0.05% Tween-20 (PBST) and thereafter 100 μl/ml of serum sample diluted at 1:200 in blocking buffer was added and incubated at RT for 60 min. Following incubation and 5X washes with PBST, 100 μl/well of horseradish peroxidase-conjugated anti-human IgG (Invitrogen, USA) diluted at 1:5000 in blocking buffer was added and incubated for 1 h at RT. After 5X washes, the reaction was visualized by adding 75 μl/well 3,3′,5,5′-Tetramethylbenzidine (TMB) liquid substrate (Bio-Rad, USA) and incubating at RT in the dark for 10–15 min. The reaction was then stopped with 75 μl/well TMB stop solution. The optical density (OD) was measured at 450 nm filter on an ELISA LT-45000 microplate reader. Each sample was tested in duplicate.
Quality control
To ensure quality control, AHRI provides hands-on training for all laboratory personnel involved in serum sample testing using in-house ELISA at the study site. The training covers procedures and protocols for in-house ELISA testing, including the preparation of coating, blocking, and washing buffers, the interpretation of test results, and ongoing competency assessments. AHRI also supplies the necessary materials for training, processing, and testing serum samples using in-house ELISA. These materials include SARS-CoV-2 RBD antigen-coated ELISA plates, secondary antibodies, substrate solutions, and true-positive and true-negative serum samples for anti-SARS-CoV-2 antibodies to be included in each in-house ELISA run as internal quality control. Two professors from Jimma University supervised the serology tests. Sample results underwent a double data entry process by two data managers, and no discrepancies were found.
Data management and analysis
The data was exported from CSentry CSPro DataEntry 7.2.1 to Microsoft Excel for cleaning and then transferred to Stata version 14.2 for analysis. We calculated various diagnostic parameters such as categorial variables as absolute numbers and percentages and Cohen’s kappa coefficient (κ). Kappa statistics were interpreted as follows: less than 0.2 represents poor agreement; 0.2–0.4 represents fair agreement; 0.41–0.6 represents moderate agreement; 0.61–0.8 represents substantial agreement; and greater than 0.8 represents a great agreement24. We also assessed the Total Percent Agreement (TPA), Positive Percent Agreement (PPA), and Negative Percent Agreement (NPA) between the three serology assays. The diagnostic parameters were presented with a 95% Confidence Interval (CI) determined using the Clopper-Pearson method.
Ethical considerations
Ethical approval for the study was obtained from the Oromia Health Bureau Review Board and Jimma University Institute of Health (Ref # BEFO/HBTFH/1-16/234 and JUIH/IRB/333/21). Support letters from the Oromia Education Bureau were also secured for selected schools. Written informed consent was obtained from parents and/or legal guardians. All information collected during the study was kept confidential through anonymity. Participants suspected of having COVID-19 were referred to the nearest health facility for appropriate care. All methods were performed in accordance with the Ethiopian Public Health Institute guidelines and regulations.
Results
SARS-COV-2 seroprevalence varied by location, age, and sex, with results differing between assays
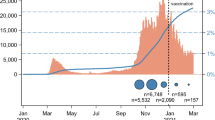
The serological investigation was carried out in 1441 serum samples collected from fifteen districts and towns that reported the highest prevalence of SARS-CoV-2 cases within the specified period. The highest positivity rate was observed in Gasera District, with a 74.3% positivity rate determined by the Rapid LFA test (IgG & IgM). There is a statistically significant association among various zones and towns in relation to sero prevalence (P Value = 0.001) while in-house ELISA was employed. Dukem and Sebata towns also showed positivity rates exceeding 50% across all SARS-CoV-2 antibody assays (Fig. 1).
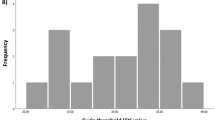
The mean age of the participants was 15.8 years (SD: 2.6). Among all age groups, the highest positivity rate was observed in individuals over 18 years of age regardless of the testing method used, ranging from 49.9% for in-house ELISA to 58.7% for Rapid LFA test (IgM & IgG.) However, there was no statistically significant difference in positivity rates between different age groups (P value = 0.409) compared with the in-house ELISA. Similarly, there was no significant association between having underlying health conditions (P value = 0.154) or contact with confirmed cases and antibody positivity (P value = 0.608) and having contact with confirmed cases by in-house ELISA. Differently, there was a statistically significant difference in seropositivity rates between males and females (P value = 0.045) seroprevalence. In-house ELISA revealed that the overall seroprevalence, or the proportion of people in a community who had contracted SARS-CoV-2 at a given point in time in the past, was 42.7% (95% CI 39.8–45.6) (Table 1).
Kappa agreements of in-house ELISA with two commercially available SARS-CoV-2 serologic assays
The overall percentage agreement between in-house ELISA and Elecsys CLIA was 80.8% (95% CI 75–86.5), indicating strong agreement. The percentage agreement with the Rapid LFA test (IgG + IgM) was slightly lower, at 75.8% (95% CI 70.1–81.5) (Table 2). The kappa coefficients (κ), which measure agreement beyond chance, were: κ = 0.61 (95% CI 0.55–0.67) for in-house ELISA and Elecsys CLIA, indicating substantial agreement; κ = 0.52 (95% CI 0.46–0.58) for in-house ELISA and the Rapid LFA test (IgG + IgM), indicating moderate agreement; and κ = 0.73 (95% CI 0.67–0.78) for Elecsys CLIA and the Rapid LFA test (IgG + IgM), indicating substantial agreement. Additionally, the concordance rate between the rapid LFA test (IgG only) and Elecsys CLIA was 89.9% (95% CI 83.2–94.8), with a κ of 0.79 (95% CI 0.73–0.85), indicating substantial agreement (Table 2).
Positive and negative percent agreement
The positive percent agreement (PPA) and negative percent agreement (NPA) between the in-house ELISA and the two commercial assays are summarized in Table 3. The in-house ELISA demonstrated strong agreement with the Elecsys CLIA, showing a PPA of 81.7% and an NPA of 80.1%. Compared to the Rapid LFA test (IgG + IgM), which had a PPA of 83% and an NPA of 70.4%, the in-house ELISA exhibited better overall agreement with Elecsys CLIA.
Interestingly, although the PPA between the Rapid LFA test (IgG + IgM) and Elecsys CLIA (81.1%) was comparable to that between the in-house ELISA and Elecsys CLIA, the Rapid LFA test (IgG + IgM) displayed a relatively higher NPA of 91.9%. This indicates that while both the in-house ELISA and the Rapid test (IgG + IgM) had similar PPA with Elecsys CLIA, the Rapid LFA test (IgG + IgM) was more consistent in correctly identifying negative samples when compared to Elecsys CLIA.
Discussion
The main goal of this study was to compare the performance of in-house ELISA with two established serological assays for detecting SARS-CoV-2 antibodies, LFA, and CLIA, using large (n = 1441) serum samples crossectionally collected from students in various districts and towns in Oromia region, Ethiopia. These areas were considered hotspots for SARS-CoV-2 transmission based on RT-PCR-positive COVID-19 cases reported before the Omicron pandemic. Our study showed significant variability in SARS-CoV-2 seroprevalence by location, age, and sex of study students who submitted the serum samples. The overall seroprevalence was 42.9% by in-house ELISA, 47.1% by Rapid LFA Test, and 46.3.7% by Elecsys CLIA. Statistically significant higher SARS-CoV-2 seropositivity rates (49.3%, 52.2%, and 58.7%) were found in students over 18 years old compared to students under 18 years old (42.9%, 49.6%, and 54.2%). Higher seropositivity rates were especially noted in males and those with direct contact with confirmed cases, underscoring the impact of exposure on transmission dynamics.
The performances of the three serological assays in this study were compared based on seropositivity, percentage agreement, and level of concordance using the Kappa value scale (Landis and Koch, 1977). The percentage agreement between the Elecsys CLIA and in-house ELISA was relatively high at 80.8%, with substantial kappa agreement (κ = 0.61), indicating significant diagnostic accuracy. In contrast, κ values between the in-house ELISA and the Rapid LFA test (IgG only) was 0.52, highlighting moderate variability in diagnostic accuracy. Although the percentage agreement observed between the Elecsys CLIA and the Rapid LFA test (IgG + IgM) was higher at 86.2% compared to the agreement between in-house ELISA and Elecsys CLIA, the kappa (κ = 0.73) values still demonstrated within the range of substantial agreement (k = 0.61–0.80). This overall agreement supports the performance of the in-house ELISA is comparable to the two commercial serological assays, highlighting its potential as a reliable, cost-effective alternative for large-scale seroepidemiological surveys.
Existing literature supports these findings, indicating that laboratory-based assays like Elecsys CLIA tend to have higher diagnostic accuracy than Rapid LFA test, particularly for detecting IgG antibodies25,26. Similarly, research findings emphasize that assays targeting spike and nucleocapsid proteins may be more effective in identifying past infections. Our results align with these studies, suggesting the utility of IgG-based assays for long-term serological surveys in regions with high prior exposure27,28.
The modest disagreement among the compared serology assays may be attributed to the differences in their target proteins; the In-house ELISA is designed to target the RBD of the SARS-CoV-2 spike protein, whereas the Elecsys targets the nucleocapsid protein of SARS-CoV-2. The assay methods differed: the in-house ELISA is a colorimetric assay, while Elecys is CLIA. Various studies have compared serology assays for SARS-CoV-2, highlighting differences in performance and results. Another study compared four quantitative SARS-CoV-2 serological assays and found poor correlation in quantitative, semi-quantitative, and qualitative measurements, emphasizing the need for assay harmonization29. Additionally, research on SARS-CoV-2 antibody levels post-vaccination revealed dynamic changes across different assay systems, offering valuable insights for standardization efforts30. An external quality assessment among laboratories in EU/EEA countries demonstrated a solid capacity to detect SARS-CoV-2 antibodies; however, performance varied based on the assay method used.
The in-house ELISA exhibits better agreement (k ≥ 0.6) with the Rapid LFA test (IgG only) and Elecys CLIA. This can be due to the similarity of the three serology assays targeting similary antibodies (IgG). Overall, assay methods that detect total immunoglobulins, neutralizing antibodies, or IgG have demonstrated better performance than IgA- or IgM-specific31,32,33,34,35.
Furthermore, the moderate to high agreement between the in-house ELISA and commercial assays supports the feasibility of locally developed assays as cost-effective alternatives, especially in resource-limited settings where imported kits may not always be accessible.
These findings have important public health implications. Serological assays are crucial for understanding the epidemiology of SARS-CoV-2, particularly in areas with high vaccination rates or limited diagnostic capabilities for qRT-PCR. In resource-constrained regions, reliable and cost-effective antibody assays can guide public health measures, including monitoring population immunity and evaluating vaccine effectiveness36. The substantial agreement between the in-house ELISA and Elecsys CLIA highlights the potential utility of the in-house ELISA as a feasible and reliable serological tool for large-scale seroepidemiological surveys.
Additionally, the lack of concordance between assays detecting different proteins (RBD vs. nucleocapsid) underscores the necessity of strategic assay selection based on the intended use, whether for determining past exposure or monitoring vaccine responses.
Our results demonstrated that the in-house ELISA, akin to the Elecsys CLIA, can quantify antibody levels and serves as a high-throughput assay, processing numerous samples within a few hours. Moreover, it can detect individuals who had a SARS-CoV-2 infection without previous molecular diagnostic confirmation, highlighting its potential use as a cost-effective serosurveillance tool to estimate the actual burden of SARS-CoV-2 infection in the country.
Serological surveys such as this one provide valuable insights into true infection rates in the community, especially in asymptomatic or mild cases that may not have been captured by routine diagnostic testing. They can also identify potential gaps in vaccine coverage or waning immunity, thereby informing decisions on booster campaigns and other public health interventions.
Strengths and limitations
The study’s strengths include its substantial sample size and the diverse clinical scenarios of the participants. Additional testers implemented rigorous quality control measures, and data were collected across sixty schools in eight zones and fifteen districts/towns. The survey spanned a wide geographical area, with samples gathered before the onset of the Omicron variant and the commencement of vaccination campaigns in the country. Notably, the in-house ELISA stands out as the only domestically manufactured SARS-CoV-2 testing methodology.
However, the study had limitations, including the absence of data on symptom onset dates, which hindered the assessment of serology assay performance across pre-symptomatic, asymptomatic, and symptomatic cases. Additionally, the lack of RT-PCR confirmation for samples means that the duration of post-exposure at the time of blood sample collection was unknown, limiting the ability to explain the discordance among the three assays fully.
Conclusion
This study highlights significant variability in SARS-CoV-2 antibody positivity across different regions in Ethiopia before the emergence of the Omicron variant. The findings suggest substantial agreement between the in-house ELISA and Elecsys CLIA and a modest agreement between the in-house ELISA and the Rapid LFA Test (IgG + IgM). Despite this, the in-house ELISA demonstrated strong potential as an effective and cost-efficient tool for anti-SARS-CoV-2 antibody testing. It is a valuable option for guiding public health responses and supporting seroepidemiological surveillance studies, particularly in resource-limited settings. Continued monitoring of SARS-CoV-2 exposure and immunity is essential to inform policies better and prepare for future outbreaks.
Data availability
All the data used were included in the manuscript.
References
Viner, R. et al. Transmission of SARS-CoV-2 by children and young people in households and schools: A meta-analysis of population-based and contact-tracing studies. J. Infect. 84, 361–382. https://doi.org/10.1016/j.jinf.2021.12.026 (2022).
Dawood, F. S. et al. Observations of the global epidemiology of COVID-19 from the prepandemic period using web-based surveillance: A cross-sectional analysis. Lancet Infect. Dis. 20, 1255–1262. https://doi.org/10.1016/S1473-3099(20)30581-8 (2020).
Fernández-Barat, L., López-Aladid, R. & Torres, A. The value of serology testing to manage SARS-CoV-2 infections. Eur. Respir. J. 56(2), 2002411. https://doi.org/10.1183/13993003.02411-2020 (2020).
Bermingham, W. H., Wilding, T., Beck, S. & Huissoon, A. SARS-CoV-2 serology: Test, test, test, but interpret with caution!. Clin. Med. 20(4), 365–368. https://doi.org/10.7861/clinmed.2020-0170 (2020).
Trabaud, M. et al. Comparison of eight commercial, high-throughput, automated or ELISA assays detecting SARS-CoV-2 IgG or total antibody. J. Clin. Virol. 132, 104613. https://doi.org/10.1016/j.jcv.2020.104613 (2020).
Poland, G. A., Ovsyannikova, I. G. & Kennedy, R. B. SARS-CoV-2 immunity: Review and applications to phase 3 vaccine candidates. Lancet 396, 1595–1606 (2020).
Jeong, S., Hong, Y. R. & Hwang, H. Performance comparison between Elecsys Anti-SARS-CoV-2 and Anti-SARS-CoV-2 S and Atellica IM SARS-CoV-2 Total and SARS-CoV-2 IgG assays. Kosin Med. J. 37(2), 154–162 (2022).
Meyer, B. et al. Validation and clinical evaluation of a SARS-CoV-2 surrogate virus neutralisation test ( sVNT). Emerg. Microbes Infect. 9(1), 2394–2403. https://doi.org/10.1080/22221751.2020.1835448 (2020).
Perera, R. A. et al. Serological assays for severe acute respiratory syndrome coronavirus 2 ( SARS-CoV-2), March 2020. Eurosurveillance 25(16), 20004215. https://doi.org/10.2807/1560-7917.ES.2020.25.16.2000421 (2020).
Pieri, M. et al. Performance evaluation of four surrogate Virus Neutralization Tests ( sVNTs ) in comparison to the in vivo gold standard test. Front. Biosci. 27, 74–85 (2022).
Mekonnen, Z. A., Riley, W. J., Grant, R. F., Romanovsky, V. E. Changes in precipitation and air temperature contribute comparably to permafrost degradation in a warmer climate OPEN ACCESS Changes in precipitation and air temperature contribute comparably to permafrost degradation in a warmer climate (2021).
Liu, C., Zhou, Q., Li, Y., Garner, L. V., Watkins, S. P., Carter, L. J. et al. Research and development on therapeutic agents and vaccines for COVID-19 and related human coronavirus diseases. https://doi.org/10.1021/acscentsci.0c00272 (2020).
Fontana, E., Bizzaro, N. & Desre, L. C. Chemiluminescent immunoassay technology: What does it change in autoantibody detection ?. Autoimmun. Highlights 8, 1–8. https://doi.org/10.1007/s13317-017-0097-2 (2017).
Kohmer, N., Westhaus, S., Rühl, C., Ciesek, S. & Rabenau, H. F. Brief clinical evaluation of six high-throughput SARS-CoV-2 IgG antibody assays. J. Clin. Virol. 129, 104480. https://doi.org/10.1016/j.jcv.2020.104480 (2020).
Charlton, C. L. et al. Evaluation of six commercial mid-to high-volume antibody and six point-of-care lateral flow assays for detection of SARS-CoV-2 antibodies. J. Clin. Microbiol. 58(10), 10–1128 (2020).
Ee, S. et al. Connecting clusters of COVID-19: An epidemiological and serological investigation. Lancet Infect. Dis. 20, 809–815. https://doi.org/10.1016/S1473-3099(20)30273-5 (2020).
Gundlapalli, A. V., Salerno, R. M., Brooks, J. T., Averhoff, F., Petersen, L. R., Mcdonald, L. C. et al. SARS-CoV-2 serologic assay needs for the next phase of the US COVID-19 pandemic response. https://doi.org/10.1093/ofid/ofaa555 (2020).
Hueston, L., Kok, J., Guibone, A., Mcdonald, D., Hone, G., Goodwin, J. et al. The antibody response to SARS-CoV-2 infection. https://doi.org/10.1093/ofid/ofaa387 (2019).
Gelanew, T. et al. High seroprevalence of anti-SARS-CoV-2 antibodies among Ethiopian healthcare workers. BMC Infect. Dis. 22(1), 261. https://doi.org/10.1186/s12879-022-07247-z (2022).
Wakita, M. et al. Comparison of the clinical performance and usefulness of five SARS-CoV-2 antibody tests. PLoS ONE 16(2), e0246536. https://doi.org/10.1371/journal.pone.0246536 (2021).
COVID AA. IgG/IgM Rapid Test Device. 19AD.
For RO, Authorization EU. Elecsys Anti-SARS-CoV-2 Elecsys Anti-SARS-CoV-2 (2021).
Gobena, D. et al. PLOS ONE Escalating spread of SARS-CoV-2 infection after school reopening among students in hotspot districts of Oromia Region in Ethiopia: Longitudinal study. PLoS ONE 18(2), e0280801. https://doi.org/10.1371/journal.pone.0280801 (2023).
Landis, J. R. & Koch, G. G. The measurement of observer agreement for categorical data data for categorical of observer agreement the measurement. Biometrics 33, 159–174 (2012).
Müller, L. et al. Sensitivity of anti-SARS-CoV-2 serological assays in a high-prevalence setting. Eur. J. Clin. Microbiol. Infect. Dis. 40, 1063–1071 (2021).
Kontou, P. I., Braliou, G. G., Dimou, N. L., Nikolopoulos, G. & Bagos, P. G. Antibody Tests in Detecting SARS-CoV-2 Infection : A meta-analysis. Diagnostics 10(5), 319 (2020).
Geurtsvankessel, C. H. et al. An evaluation of COVID-19 serological assays informs future diagnostics and exposure assessment. Nat. Commun. 11(1), 3436 (2020).
Assay, I. et al. Performance characteristics of the Abbott Architect SARS-CoV-2 IgG assay and seroprevalence in Boise, Idaho. J. Clin. Microbiol. 58(8), 10–1128 (2020).
Chan, A. et al. Evaluation and comparison of four quantitative SARS-CoV-2 serological assays in COVID-19 patients and immunized healthy individuals, cancer patients, and patients with immunosuppressive therapy. Clin. Biochem. 116, 1–6. https://doi.org/10.1016/j.clinbiochem.2023.02.010 (2023).
Seo, J. D. et al. Comparison of four systems for SARS-CoV-2 antibody at three time points after SARS-CoV-2 vaccination. Diagnostics 12(6), 1349 (2022).
Haselmann, V. et al. Results of the fi rst pilot external quality assessment ( EQA ) scheme for anti- SARS-CoV2-antibody testing. Clin. Chem. Lab. Med. CCLM 58, 2121–2130 (2020).
Van den Beld, M. J. et al. Increasing the Efficiency of a National Laboratory Response to COVID-19: A Nationwide Multicenter Evaluation of 47 commercial SARS-CoV-2 immunoassays by 41 laboratories. J. Clin. Microbiol. 59(9), 10–1128 (2021).
Li, K. et al. Dynamic changes in anti-SARS-CoV-2 antibodies during SARS-CoV-2 infection and recovery from COVID-19. Nat. Commun. 11(1), 6044. https://doi.org/10.1038/s41467-020-19943-y (2020).
Long, Q. et al. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat. Med. 26(6), 845–848. https://doi.org/10.1038/s41591-020-0897-1 (2020).
Colavita, F., Lapa, D., Carletti, F., Lalle, E., Messina, F., Rueca, M. et al. Virological characterization of the first 2 COVID-19 patients diagnosed in italy: Phylogenetic analysis, virus shedding profile from different body sites, and antibody response kinetics. https://doi.org/10.1093/ofid/ofaa403.
Nelson-mora, J. et al. New detection method of SARS-CoV-2 antibodies toward a point-of-care biosensor. Front. Bioeng. Biotechnol. 11, 1202126. https://doi.org/10.3389/fbioe.2023.1202126 (2023).
Acknowledgements
We acknowledge Oromia Health Bureau, AHRI and Jimma University for their support.
Funding
No specific funding has been assigned to this research project. The Oromia Health Bureau purchased the rapid testing kits device. At the same time, Jimma University contributed ELesys CLIA, and AHRI supplied the in-house ELISA and offered training and supervision to laboratory professionals at the Adama regional and reference laboratory. The Oromia Health Bureau supported the team’s data collection and research activities to produce evidence to strengthen public health surveillance and combat the pandemic within educational institutions and the broader region.
Author information
Authors and Affiliations
Contributions
D.G., Te.G., Z.M., E.K., T.T., and T.G. initiated the project and developed the design and methodology. All the team contributed to designing the statistical methods and statistical analysis plan. D.G. and Te.G. performed the analysis. Te.G., A.A., F.T., and G.G. contributed to the design of the testing methodology and took responsibility for storing and analyzing samples. D.G. wrote the first draft of the manuscript. All authors provided edits and critiques of the manuscript for intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
We declare this manuscript is original, has never been published before, nor is it under consideration for publication elsewhere.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gobena, D., Gudina, E.K., Degfie, T.T. et al. Comparative evaluation of in-house ELISA and two commercial serological assays for the detection of antibodies against SARS-CoV-2. Sci Rep 15, 13853 (2025). https://doi.org/10.1038/s41598-025-97050-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-97050-y