Abstract
IL-35 is known to enhance tumor progression by promoting angiogenesis, increasing cancer cell proliferation, and facilitating immune suppression. Elevated levels of IL-35 have been correlated with the severity of malignancy and clinical stage in various cancers. The aim of this study was to investigate the relationship between serum IL-35 levels and the presence and clinicopathological features of primary benign and malignant ovarian tumors. This case-control study consisted of 60 women diagnosed with primary benign and malignant ovarian tumors and 60 age-matched healthy controls. The demographic and clinicopathological data were also collected. The serum level of IL-35 was evaluated using an ELISA kit, and the results were analyzed using SPSS software. The patients had a mean age of 47.93 ± 14.52 which was similar to that of the controls (53.43 ± 11.69) (P = 0.519). The mean serum level of IL-35 was 7.01 ± 0.843 pg/ml in the control group and 7.24 ± 0.811 pg/ml in the patient group (P = 0.213). There was no significant difference in serum IL-35 levels between the tumor types (P = 0.991). There was also no significant association between serum IL-35 levels and disease stage (P = 0.559), grade (P = 0.635), lymph node involvement (P = 0.091), or tumor size (P = 0.564). No significant difference in serum IL-35 levels was observed between the patient and control groups, nor was there a significant association between IL-35 levels and tumor characteristics (stage, grade, size, lymph node involvement. However, further studies with more cases at different stages of the disease are necessary.
Similar content being viewed by others
Introduction
Ovarian cancer remains a significant cause of cancer-related deaths among women1. While the disease is relatively rare in women under 40, its incidence increases after age 65–702,3. Ovarian tumors are often asymptomatic in early stages, leading to late diagnoses4. The tumor microenvironment, and the host’s immune response, play critical roles in ovarian cancer progression and treatment outcomes5. Therefore, understanding the role of key immune mediators in ovarian cancer is crucial.
Interleukin-35 (IL-35) is an immunosuppressive cytokine belonging to the IL-12 family6. It is secreted by regulatory T cells (Tregs) and other immunoregulatory cells, and can inhibit the function and proliferation of T cells7. IL-35 is known to enhance tumor progression by promoting angiogenesis, increasing cancer cell proliferation, and facilitating immune suppression. It achieves this by inhibiting CD8 + T cells and recruiting regulatory T cells (Treg cells) into the tumor microenvironment, which helps tumors evade immune responses8. Elevated levels of IL-35 have been correlated with the severity of malignancy and clinical stage in various cancers, including colorectal, breast, and non-small cell lung cancer9. This suggests that IL-35 could similarly indicate the severity or progression of ovarian tumors. IL-35 acts by inducing immunosuppressive forces, which can lead to immune evasion of tumors. This mechanism is crucial for tumor growth and metastasis, making IL-35 a potential marker for monitoring tumor progression10.IL-35’s role in cancer is complex and context-dependent, with studies showing both tumor-promoting and tumor-suppressive effects. For example, IL-35 derived from Tregs can suppress anti-tumor T cell responses, thus promoting tumor growth14, while in other contexts, it may contribute to the generation of anti-tumor immune memory and directly inhibit tumor cell growth7,11. The expression of the EBI3 gene (which codes for an IL-35 subunit) promotes the growth of lung cancer, with its silencing offering therapeutic potential12.
Given its involvement in tumor progression and its correlation with disease prognosis in other cancers, IL-35 could serve as a valuable biomarker for assessing ovarian tumor progression and prognosis. Its ability to recruit Treg cells and suppress immune responses makes it a promising candidate for monitoring immune-related changes in ovarian cancer13. Therefore, we investigated the serum concentration of IL-35 in patients with ovarian tumors and compared it with that of a healthy population. We also aimed to determine the relationship between serum IL-35 levels and patients’ clinicopathologic characteristics.
Methods
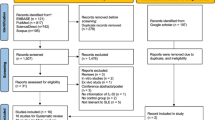
Study design
This case-control study was conducted from May 2018 to January 2021 at Shahid Faghihi, Hazrate Zeinab, Namazi, and Ghadir Mother and Child Hospitals in Shiraz, Iran, which are affiliated with Shiraz University of Medical Sciences.
Sixty consecutive women with newly diagnosed ovarian tumors (confirmed both clinically and pathologically) who met the eligibility criteria were enrolled. In addition, 60 consecutive age-matched women were considered as controls. Inclusion criteria were consent to participate, lack of infectious or inflammatory diseases during the last three months, and lack of undergoing treatment for the ovarian tumor (surgery, anti-cancer medications, or radiotherapy).
Individuals with a history of autoimmune diseases, immunodeficiency, metabolic diseases, cardiovascular diseases, atopy, asthma, or tumors other than ovarian tumor were excluded.
For experiments involving human participants (including the use of tissue samples), informed consent must have been obtained. So, all participants completed written informed consent, the study questionnaire, underwent anthropometric measurements, and provided peripheral blood samples. The questionnaires included demographic information, family history, and past medical history. A sterile blood sample (5 ml) was prepared from the peripheral vein. Then, the samples were centrifuged at 2500 rpm for 10 min, and the sera were separated. The obtained sera were stored in the freezer at -70 °C until testing. These specimens were examined for IL-35 concentration using an ELISA IL-35 detection kit (eBioscience, San Diego, CA, USA) via the sandwich ELISA method following the manufacturer’s supplied protocol. The following techniques were used for intra- and inter-assay variability for ELISA: (1) Intra-assay Variability: To evaluate intra-assay variability, each sample was tested in triplicate within the same plate. The mean coefficient of variation (CV) for all samples was less than 10%, demonstrating high reproducibility of the assay; (2) Inter-assay Variability: To assess inter-assay variability, control samples were tested across three different plates on separate days. The mean CV for the control samples was less than 15%, indicating consistent and reliable performance of the assay over time.
Participation in this study was entirely voluntary, and all participants could withdraw at any stage. The study protocol was approved by the Ethics Committee of Shiraz University of Medical Sciences (IR.SUMS.MED.REC.1398.439) prior to the enrollment of participants. Throughout this study, we adhered to the principles outlined in the Declaration of Helsinki.
Statistical analysis
Data were analyzed using SPSS version 22 (IBM Corp, Armonk, NY, USA). The results are presented as mean and standard deviation for quantitative variables and as frequency and percentage for categorical variables. To check the distribution of data, we used the Kolmogorov Smirnov test. Categorical variables were compared using the chi-square test or Fisher’s exact test as appropriate, while continuous variables were compared with the independent t-test or Mann–Whitney U test as appropriate. A multiple linear regression model was employed to adjust for the most significant clinical factors and evaluate their potential influence on IL-35 levels.
Results
Our study included 60 patients with a mean age of 47.93 ± 14.52 (range 18–85) years and 60 controls with a mean age of 53.43 ± 11.69 (range 23–73). These two groups were matched in terms of age and Body Mass Index (BMI) (P > 0.05). Other characteristics of the participants are provided in Table 1.
The mean serum level of IL-35 was 7.01 ± 0.843 pg/ml in the control group and 7.24 ± 0.811 in the patient group, the results did not reveal statistically significant differences in IL-35 levels between patients with ovarian tumors (both benign and malignant) and healthy controls. (P = 0.213) (Fig. 1).
Out of 60 patients with ovarian tumor, 20 (33.3%) had serous carcinoma, 9 (15%) had benign mucinous, 9 (15%) had benign serous, 7 (11.6%) had borderline serous adenocarcinoma, 7 (11.6%) had sex-cord tumor, 5 (8.3%) had mucinous carcinoma, and 3 (5%) had endometrioid carcinoma. There was no significant difference in the serum level of IL-35 between the tumor types (P = 0.991) (Table 2), and mucinous tumors were similar to serous tumors in terms of IL-35 levels (5.94 ± 2.06 vs. 6.54 ± 1.98 pg/ml, P = 0.745). There was no significant difference in serum IL-35 levels between benign (6.04 ± 1.39 pg/ml), borderline (6.98 ± 3.53 pg/ml) and malignant tumors (5.92 ± 2.94 pg/ml) (P = 0.903).
We also evaluated the relationship of demographic and clinicopathologic factors with serum IL-35 levels. The IL-35 levels had a significant inverse relationship only with the age at onset of menstruation (P = 0.040). When considering IL-35 levels in patients and controls over and under 50 years of age, no significant relationship was found in either group (P = 0.360 and P = 0.965, respectively).
Table 3 summarizes the relationship between the serum IL-35 levels and ovarian tumor parameters. As evident, there was no significant relationship between IL-35 serum levels and disease stage (P = 0.559), grade (P = 0.635), lymph node involvement (P = 0.091), or tumor size (P = 0.564).
The results of multiple linear regression model showed that after adjusting for key factors such as tumor size (Coefficient = − 0.91, 95% CI − 6.04, 4.22, P = 0.72), lymph node involvement (Coefficient = − 0.58, 95% CI − 7.83, 6.67, P = 0.87), and tumor types (Coefficient = − 0.28, 95% CI − 3.87, 3.32), none of these factors showed a significant relationship with IL-35 levels.
Discussion
Our study investigated the potential of serum IL-35 as a biomarker for ovarian tumors. However, we did not find a significant difference in serum IL-35 levels between patients and healthy controls, nor did we find any significant correlations with clinicopathological features. Therefore, based on our results, serum IL-35 is unlikely to be a useful biomarker for ovarian tumor diagnosis or prognosis.
Although IL-35 is recognized for its role in modulating immune responses and has been implicated in various cancers and autoimmune diseases, the current study contributes to a limited body of literature exploring its role in gynecological conditions, particularly ovarian tumors. Immune-suppressive cytokines like IL-35 can influence tumorigenesis by regulating immune responses and promoting tumor cell survival14,15. This lack of correlation may be attributed to the fact that our cohort consisted of patients with primary ovarian tumors without evidence of metastasis, differing from other studies that documented elevated IL-35 levels in metastatic diseases16.
Previous studies in different cancer models have indicated that tumor microenvironments often yield increased IL-35 levels7,17. For example, Lee et al. demonstrated that IL-35 secretion in a breast cancer metastasis model facilitated the colonization of metastatic cells through mechanisms involving the JAK2-STAT6 signaling pathway18. In contrast, our study found no elevation of IL-35 levels in the serum of patients with ovarian tumors compared to healthy controls, further suggesting a potential tissue-specific expression that might not be visible in peripheral blood measurements.
Interestingly, studies in other cancer types, such as non-small cell lung cancer (NSCLC), reported varying results. Liu et al. found significantly elevated IL-35 levels in bronchoalveolar fluid from NSCLC patients, indicating that local microenvironmental factors may greatly influence IL-35 expression7. Comparisons with these studies suggest that while serum IL-35 may not serve as a reliable biomarker for ovarian tumors, it could still be relevant in local tumor settings, warranting further investigation into tissue-specific IL-35 levels.
The observed differences in serum IL-35 levels across different cancer types—such as colorectal cancer and prostate cancer—highlight the need for caution when interpreting these results6,19,20. For instance, studies have indicated that IL-35 production in tissue samples correlates with tumor stage and prognosis in colorectal cancers, whereas we found no such correlation in our ovarian tumor cohort16. This discrepancy may arise from inherent differences in tumor biology or immunological contexts specific to each cancer type.
While our study did not assess intratumoral IL-35 levels, existing literature suggests that evaluating IL-35 expression within tumor tissues could reveal its true clinical significance21. Emerging data indicate that IL-35 may promote tumor progression and metastasis through various mechanisms, including enhancing vascularization and supporting immune evasion22. For example, Liu et al. reported increased IL-35 levels in pancreatic cancer tissues associated with poor prognosis, underscoring the potential for IL-35 as a target for therapeutic interventions7.
Our study had several limitations. First, it was a case-control design without longitudinal follow-up, limiting our ability to assess changes in IL-35 levels over time. Second, we were unable to analyze intratumoral IL-35 levels, which may provide a more comprehensive understanding of its role in tumor biology. Lastly, our sample size was relatively small, necessitating further studies to validate our findings.
Conclusion
In conclusion, our data indicate that serum IL-35 is unlikely to serve as a useful biomarker for ovarian tumors. Our findings demonstrate a lack of correlation between serum IL-35 levels and the presence or characteristics of ovarian tumors. No significant differences in serum IL-35 were observed between patients with ovarian tumors and healthy controls, nor were there significant correlations between serum IL-35 levels and tumor stage, grade, size, or lymph node involvement. Future research should focus on analyzing IL-35 levels within the tumor microenvironment itself, as opposed to peripheral blood serum, to ascertain whether local IL-35 expression plays a role in ovarian tumorigenesis or progression. Furthermore, longitudinal studies are warranted to investigate potential changes in IL-35 levels over time in patients with ovarian cancer, considering the dynamic nature of the disease and its response to therapy.
Data availability
The data supporting our findings are available from the corresponding author upon reasonable request.
References
Zhang, S. et al. The global burden and associated factors of ovarian cancer in 1990–2019: findings from the global burden of disease study 2019. BMC Public. Health. 22 (1), 1455 (2022).
Ali, A. T., Al-Ani, O. & Al-Ani, F. Epidemiology and risk factors for ovarian cancer. Menopause Review/Przegląd Menopauzalny. 22 (2), 93–104 (2023).
Dumas, L., Bowen, R., Butler, J. & Banerjee, S. Under-treatment of older patients with newly diagnosed epithelial ovarian cancer remains an issue. Cancers 13 (5), 952 (2021).
Žilovič, D., Čiurlienė, R., Sabaliauskaitė, R. & Jarmalaitė, S. Future screening prospects for ovarian cancer. Cancers 13 (15), 3840 (2021).
Luo, X., Xu, J., Yu, J. & Yi, P. Shaping immune responses in the tumor microenvironment of ovarian cancer. Front. Immunol. 12, 692360 (2021).
Ye, C., Yano, H., Workman, C. J. & Vignali, D. A. Interleukin-35: structure, function and its impact on immune-related diseases. J. Interferon Cytokine Res. 41 (11), 391–406 (2021).
Liu, K. et al. IL-35 regulates the function of immune cells in tumor microenvironment. Front. Immunol. 12, 683332 (2021).
Xue, W., Yan, D. & Kan, Q. Interleukin-35 as an emerging player in tumor microenvironment. J. Cancer. 10 (9), 2074–2082 (2019).
Mirlekar, B. Tumor promoting roles of IL-10, TGF-β, IL-4, and IL-35: its implications in cancer immunotherapy. SAGE Open. Med. 10, 20503121211069012 (2022).
Kourko, O., Seaver, K., Odoardi, N., Basta, S. & Gee, K. IL-27, IL-30, and IL-35: A cytokine triumvirate in cancer. Front. Oncol. 9, 969 (2019).
Friedman, A. & Liao, K-L. The role of the cytokines IL-27 and IL-35 in cancer. Math. Biosci. Eng. 12 (6), 1203–1217 (2015).
Cirella, A. et al. Novel strategies exploiting interleukin-12 in cancer immunotherapy. Pharmacol. Ther. 239, 108189 (2022).
Wyciszkiewicz, A., Lach, M., Kalinowska, A., Michalak, S. & Nowakowski, B. Multiplexed immunobead-based cytokine profiling in patients with ovarian cancer. Eur. J. Transl. Clin. Med. 4 (2), 31–43 (2021).
Teymouri, M., Pirro, M., Fallarino, F., Gargaro, M. & Sahebkar, A. IL-35, a hallmark of immune‐regulation in cancer progression, chronic infections and inflammatory diseases. Int. J. Cancer. 143 (9), 2105–2115 (2018).
Liu, X., Ren, H., Guo, H., Wang, W. & Zhao, N. Interleukin-35 has a tumor-promoting role in hepatocellular carcinoma. Clin. Exp. Immunol. 203 (2), 219–229 (2021).
Zeng, J-C. et al. Assessing the role of IL-35 in colorectal cancer progression and prognosis. Int. J. Clin. Exp. Pathol. 6 (9), 1806 (2013).
Yi, P. et al. IL-35: new target for immunotherapy targeting the tumor microenvironment. Mol. Cancer Ther. 23 (2), 148–158 (2024).
Lee, C-C. et al. Macrophage-secreted interleukin-35 regulates cancer cell plasticity to facilitate metastatic colonization. Nat. Commun. 9 (1), 3763 (2018).
Calu, V. et al. Key biomarkers within the colorectal cancer related inflammatory microenvironment. Sci. Rep. 11 (1), 7940 (2021).
Novysedlak, R. et al. The immune microenvironment in prostate cancer: a comprehensive review. Oncology. 1–37 (2024).
Long, J. et al. IL-35 over-expression increases apoptosis sensitivity and suppresses cell growth in human cancer cells. Biochem. Biophys. Res. Commun. 430 (1), 364–369 (2013).
Wang, Z. et al. Tumor-derived IL-35 promotes tumor growth by enhancing myeloid cell accumulation and angiogenesis. J. Immunol. 190 (5), 2415–2423 (2013).
Funding
This work was supported by a grant from Shiraz University of Medical Sciences Grant No. 17867 and in part by Shiraz Institute for Cancer Research Grant No. ICR-100-502.
Author information
Authors and Affiliations
Contributions
L.K.: Study design, data collection, data analysis, manuscript drafting, and revision. M.M. and M.J.F. Study design, supervision, data interpretation, manuscript revision. A.G. Study design, supervision, data interpretation, manuscript revision. M.J.F., R.A., S.H.M. and A.H. Data interpretation, manuscript drafting, and revision. All authors read and approved the final manuscript.All authors agree to be accountable for all aspects of the work ensuring integrity and accuracy. All data were generated in-house, and no paper mill was used.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted in line with the ethical principles of Shiraz University of Medical Sciences (Ethics Committee Approval No. IR.SUMS.MED.REC.1398.439) and the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kiani, L., Momtahan, M., Shiravani, Z. et al. Role of serum IL-35 levels in patients with benign and malignant primary ovarian tumors: a case-control study. Sci Rep 15, 12827 (2025). https://doi.org/10.1038/s41598-025-97349-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-97349-w