Abstract
Neurological abnormalities are frequent after cerebral malaria (CM) resolves. The identification of survivors that should be prioritized during follow-up after CM is necessary for post-hospitalization care. We analysed social, clinical, and immune determinants of malarial retinopathy (MR) and short-term neurological outcomes after CM. Children aged 24 to 71 months with CM were prospectively followed-up until 28 days after admission at two hospitals in Benin. Direct ophthalmoscopy was performed shortly after admission. Plasma biomarkers were measured at admission. A neurocognitive deficit screener was administered at discharge and 21–28 days after admission. Of 70 children, 20 died before discharge (28.6%). Neurological deficits decreased from 100% on admission to 48.9% at discharge, and to 16.7% at 21–28 days after admission. MR was found in 58% of children. In multivariate analysis, factors associated with MR were a traditional consultation before admission and study site. In addition, neurological deficits were associated with MR (Odds Ratio 5.54 95% CI (1.30–23.54)). In univariate analysis, higher plasma levels of angiopoietin-2 were associated with neurological deficit at discharge and at days 21–28 post-admission. Therefore, MR and endothelium activation may be markers of neurological deficit, the former at hospital discharge and the latter at discharge and at D21–D28 post-admission.
Similar content being viewed by others
Background
Since 2015, the progress observed so far in terms of malaria prevalence and mortality with implementation of the World Health Organization Roll Back Malaria program has stalled1. Cerebral malaria (CM) is by far the most common cause of non-traumatic coma in Benin, West Africa, and has been associated with a poor prognosis even during the artesunate era2. Although malaria eradication within a generation is the goal, the number of deaths related to malaria remains high, especially in areas of West and Central Africa3.
Neurological sequelae are also observed after CM in paediatric survivors and its incidence in African children varies widely among studies, from 6 to 31% of cases4,5. Neurocognitive impairments include motor, speech, language, and memory domains6,7. Seizures may also occur months after a CM episode5.
All children with CM should therefore be followed-up for several months after discharge4,8 but it is logistically difficult to do so in areas with few resources. Some studies have reported decreases in the proportion of children with CM-related gross deficits 3–8 weeks after discharge5,9. As the epidemiology of severe malaria may shift10, the extent to which disabilities change within weeks after discharge needs to be reassessed. Furthermore, predicting which children admitted with CM would be most likely to have short-term, post-discharge disabilities would be helpful to prioritize such individuals for follow-up.
Although malarial retinopathy (MR) may improve the specificity of CM diagnosis11,12 and predict the risk of sequelae in children with CM8, it is rarely performed in routine practice in malaria-endemic areas, even in tertiary care hospitals. MR is associated with reduced perfusion of the retina and may mirror reduced brain perfusion possibly related to sequestration of parasitised erythrocytes12,13. Modifications of the brain blood barrier may explain retinal haemorrhage12. MR is also related to markedly increased brain volume as evidenced by MRI imaging14. Few studies have reported an association between MR and increased mortality15, and even fewer have explored MR as a predictor of neurological outcomes in survivors8,16.
Biological markers of clinical outcomes including neurological deficits would be useful for identifying children most at risk of developing neurological deficits. Few studies have focused on biological prognostic markers for neurologic sequelae following CM. However, inflammatory and oxidative responses are associated with mortality and severity during malaria17,18,19,20. Cytokines, including chemokines, are highly relevant biomarkers of inflammation, displaying pro- or anti-inflammatory properties, recruiting and activating immune cells, and thus modulating their microenvironment21. Leukotrienes (LTB4, LTC4, LTD4, LTE4), lipoxins (LXA4, LXB4), prostaglandins (PGD2, PGE2, PGF2, PGI2), and all products of the arachidonic acid metabolism pathway are also involved in pro- and anti-inflammatory equilibrium22,23,24. LXA4, an anti-inflammatory mediator that inhibits LTB4 and thus neutrophil function and migration, limits endothelial dysfunction and prevents breakdown of the blood brain barrier when administered to infected mice25. Regarding the oxidant response, isoprostane and glutathione (in its reduced and oxidized forms, GSH and GSSG, respectively) are involved in the arachidonic acid metabolism pathway and associated with disease resolution in CM19,20. In this work, we studied the plasma levels of pro- and anti-inflammatory cytokines, along with urine biomarkers of the inflammatory and oxidative response, in relation to MR in children with CM and to neurocognitive deficits at discharge and 21–28 days post-admission.
This work is part of a larger project called NeuroCM26, whose main goal was to identify the causative and remedial factors of neuroinflammation in the context of CM. In this study, we studied the determinants of MR observed early after admission and neurological deficits observed at discharge and 21–28 days post-discharge.
Results
Study population
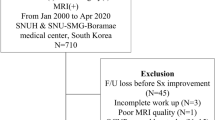
From March 1 to November 30, 2018, 326 children aged between 2 and 6 years were admitted with coma to the hospital (Fig. 1). Of these, one child had pre-existent neurological disease, six were in a non-malarial coma, and a further eight had a coinfection, all of which were excluded. Overall, 70 children met the inclusion criteria; 38 were at Calavi Hospital and 32 were at CHUMEL. Female/male repartition was 41/29, with a male–female sex ratio of 0.7. The median age was 43.3 (36.1–54.1) months. The median duration between the start of symptoms and admission at the hospital was 4 days (SD = 1.84). Among survivors at discharge, the median duration between inclusion in the study and discharge from the hospital was 6.9 days (SD = 3.1). The case fatality rate was 28.6% (20/70). Study population characteristics according to vital status at discharge are provided in Table 1. A Blantyre coma score below 2, jaundice, hypoglycaemia, and acidosis were associated with a fatal outcome in univariate analyses.
Assessment of neurological status
Of the 50 children who survived CM, 49 had a neurological assessment (withdrawal of one child happened on the day before scheduled discharge). Neurological assessment at discharge (Table 2) was carried out in 49 children and 7 children were lost to follow-up by D21–28. Findings describing neurological assessments are detailed in Table 2. In the 42 children with questionnaires available both at discharge and at D21–28, neurological deficits were found more frequently at discharge than at D21–28 post-admission (48.9% vs. 16.7%, p < 0.001).
Factors associated with MR
Fundoscopy was carried out on D1 of hospitalization in 55 children with CM. Missing data in 15 children were due to death within 18 h after admission. Of these 55 children, 32 had at least one item defining MR. As shown in Fig. 2, the MR characteristics present in children were haemorrhages (30 children), whitening (4 children), and vascular changes (one child). Baseline characteristics associated with MR in univariate analysis are provided in Table 3 and Supplemental Table 1. The three factors significantly associated with an increased risk of MR were a traditional consultation before admission (81.8% of MR in children given traditional medicine vs. 42.4% of MR in children were not; p = 0.003), the absence of antiepileptic drug intake before admission (73.3% vs. 40.0%, p = 0.013), and severe anaemia at admission (77.3% vs. 44.1%, p = 0.014). In multivariate analysis, MR was associated with the admission site and a traditional consultation before admission (Table 4).
Factors predictive of neurological sequelae at day of discharge and at D21–28 post-admission
In univariate analysis, jaundice and MR were significantly associated with neurological deficit at discharge (Table 3). By contrast, no baseline characteristic was significantly associated with MR at D21–D28 post-admission. In multivariate analysis, none of the exposure variables tested (antibiotic intake prior to admission, multiple convulsions, jaundice) showed a significant association with neurocognitive deficit at hospital discharge. On the other hand, neurological deficits at discharge were associated with MR (Table 4). Multivariate analyses at D21–D28 were not possible given the low number of observations.
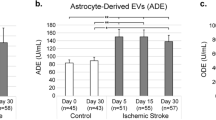
Association between immune factors and MR and neurocognitive deficit
Immune markers of inflammation, the oxidative response, and endothelium activation were measured in plasma and urine at inclusion to study their association with MR and neurologic impairment through univariate analysis. MR was associated with a lower urine LXA4/LTB4 ratio and plasma level of CXCL5, CCL17, and CCL22 (Fig. 3). Although both urine LXA4 and LTB4 levels were higher in the MR group, the lower ratio was due to higher levels of proinflammatory LTB4 (Table S1). Neurocognitive deficit at discharge was associated with lower urinary levels of glutathione (GSH), a known marker of the antioxidant state, and with higher plasma levels of angiopoietin-2, a marker of endothelium activation (Table S2). At D21–28 post-inclusion, only higher plasma levels of angiopoietin-2 were still associated with neurocognitive deficit.
Association of urinary and plasma immune markers with fundoscopy status (A) and neurological deficits at discharge (B) and between 21 and 28 days post-admission (C). The heatmap presents the means of normalized values to the maximum value of each biomarker x 100. Detailed values are presented in Supplementary Tables 1 and 2. The Mann–Whitney U-test was used to test associations, * indicates p < 0.05.
Discussion
The high proportion of MR at admission, along with the high proportion of neurological deficits at discharge, which substantially decreased by D21–28 post-admission, are the main findings of our study. Although no baseline characteristic was associated with a post-discharge deficit, MR at admission was associated with a neurocognitive deficit at discharge.
This study presents a cohort of severe comas in African children, the only one performed in West Africa. Although children were provided with emergency treatments including intravenous artesunate, a high fatality rate was observed (28.6%). This could be due to the fact that these children were in deep comas, possibly with multiorgan failure, and had no access to intensive care. No brain imaging was available and we may have missed, for example, cerebral tumours or bleeding as a cause of coma, as nonmalarial causes may coexist with parasitaemia27. However, we are confident that the diagnoses of CM were exhaustive and reliable, due to the high quality of laboratory testing and the use of a panel of experts to ensure the best classification of the patients2.
Some limitations of this study should be mentioned. Because most of children who died had missing fundoscopic data, the proportion of children with MR may have been biased and potentially underestimated. Indeed, it is likely that children who died were at higher risk of MR. Data on clinical history, based on interviews with parents/guardians at admission and a health booklet review may not have been exhaustive. Neurodevelopmental deficits were assessed through a questionnaire derived from the TQ. This screener was associated with the Mullen Scales of Early Learning at 1 year of age28 and the Kaufman Assessment Battery for Children – Second edition – at 6 years of age in a Beninese cohort study (R. Zoumenou, personal communication). However, in our study, we included only a subsample of the TQ questions and referred to the child’s state before CM. In addition, although the TQ is efficacious for screening for neurodevelopmental deficits, it reflects caregiver perception and is not an objective test administered by a trained psychologist. Therefore, declared neurological deficits may be affected by caregiver perception, especially in the context of CM. Our study used the TQ, a screener for neurodevelopmental deficits, but a robust measure of neurocognitive deficits would have been useful, like the Kaufman Assessment Battery for Children. A study in Uganda validated the TQ and reported a positive rate of 27%29. The TQ screen is considered positive if any 1 of 10 TQ questions is positive. The rate of neurological deficits was 48.9% at discharge and 16.7% at 21–28 days post-admission. Given that we included only 8 of the 10 TQ questions, the percentage of neurological deficits in our study may have been slightly higher if we had included all questions. The questions related to seizures and learning were not included. Therefore, our results seem consistent with the study in Uganda. Finally, our study may have lacked power to extensively identify the factors associated with death and neurological outcomes. For several variables, confidence intervals were large and should be interpreted with caution. Seventy-two participants would have been needed to be able to detect an association between MR and neurological deficits at D21–28 with an Odds Ratio of 5 and a power of 80%.
Depth of coma and some established biological criteria for severe malaria at admission were associated with a fatal outcome in this cohort. We have no explanation as to why boys died more frequently, however, male sex has been associated with a greater risk for new neurodisability in MR-positive paediatric CM survivors4. Death occurred shortly after admission in most cases, before any emergency antimalarial prescription could have been effective and may explain why mortality remains high in the artesunate era.
MR was first described about 30 years ago30 and fundoscopy is rarely a part of CM management in routine practice11. We decided not to include MR in the definition of CM, in line with the current WHO criteria for CM31. While performing a fundoscopy within 24 h after admission was planned for each admitted child, a substantial proportion of children could not be assessed for MR because they died very early after admission and before the research clinician was available at the study site. This illustrates the difficulties of efficiently implementing fundoscopy in the field to help manage CM. Most children had an MR and the most common feature was haemorrhage. An autopsy study in Malawi found that severity of haemorrhage in the retina correlates with that in the brain32. Our data enabled us to explore the association between characteristics observed at admission and MR in patients with CM. A consultation with a traditional practitioner before admission was associated with MR. However, there was no association between the duration from the onset of symptoms to hospital admission and consultations with a traditional practitioner, which could explain this association. In addition, MR was independent of any delay between the first symptoms and admission. This result could therefore suggest either that traditional consultations contributed to the development of retinopathy, or that retinopathy itself influences the need for traditional consultations. Interestingly, not taking antiepileptic drugs was associated with MR. As the onset of multiple convulsions (treated with antiepileptic drugs) was not associated with MR, this result may reflect the difficulty of accessing conventional care, which is in line with traditional medicine consultations and favours MR. MR was also associated with severe anaemia, an established severe malaria criterion, in univariate analysis. Lewallen et al.. found a significantly lower haematocrit level in children with retinal haemorrhage33. Furthermore, Chillaverde et al.. showed that children with MR have a significantly lower haemoglobin level at admission than children without it34. Overall, our results add to the already described association between MR and established criteria for severe malaria.
Our findings corroborate previous reports9,35, showing that disabilities are much less prevalent a few weeks after discharge than at discharge. Most reported issues at admission were related to motor function. These are also the functions that seemed to have improved by D21–28. Therefore, the acute phase of CM had an important impact on motor function. Future studies should include neuropsychological tests administered by trained assessors to be able to capture detailed cognitive abilities that may be affected by CM. Because epidemiological studies performed in malaria-endemic areas have found some neurological disabilities in children with no history of severe malaria29,36, all of the neurological deficits detected in our study may not be attributable to malaria. Some of them likely pre-existed before CM.
Few studies have explored the interactions between MR and neurological outcomes after CM. In studies in Malawi that carried out 18 months of follow-up for neurological assessment after CM, a high proportion of deficits (epilepsy, other neurobehavioral sequelae) was found in both children with and without MR4,16 but there was no trend toward a higher risk of obvious neurological sequelae in those with MR (132 children) compared to those without it (35 children)16. By contrast, another study also in Malawi, where fundoscopy was performed in 49 children and severity of MR was scored, reported a relationship between MR severity and persistent neurocognitive problems8, suggesting a link between MR at admission and neurological outcomes. While jaundice at admission, a characteristic associated with death over the whole cohort, was associated with neurological deficits at discharge in univariate analysis, MR was the only baseline characteristic associated with neurological deficits at discharge in both univariate and multivariate analyses. Thus, our data add to previous evidence of an association between MR and neurological outcomes, assessed at discharge in this population, suggesting that MR may be a marker of brain injury32.
We also focused on immune biomarkers of both neurological sequelae after CM and MR, measured in plasma and urine. Only a few studies have evaluated links between immunologic markers and neurologic deficits after CM. John et al.. reported a correlation between elevated levels of TNF in cerebrospinal fluid (CSF), but not in serum, and increased risk of neurologic deficit 3 months after admission in children with CM37. This association was confirmed by two studies reporting neurologic deficits at discharge and 3 months after CM (in the first study38) and 2 years after a severe malaria episode, including CM (in the second study39). Plasma and serum proinflammatory cytokines have also been studied in relation to neurologic deficits in many clinical pathologies in children and newborns. Elevated serum levels of proinflammatory cytokines (IL-1β, IL-6, TNF) and markers of central nervous system impairment (enolase, S-100 protein) have been described in hypoxic–ischemic conditions in newborns at high risk for neurologic sequelae40. Elevated plasma IL-6 levels are also associated with neuromotor abnormalities in children 6 months after open-heart surgery, an intervention known to cause frequent long-term neurodevelopmental sequelae41. In our study, no such relation was found between proinflammatory cytokines (TNF, IL-1β, IL-8, IL-12, IL-6) and neurological deficit studied at discharge or 28 days after inclusion. This could be due to our short follow-up of less than 1 month. However, Shabani et al.. observed a correlation between CSF levels of TNF and neurological deficits at discharge in CM children. Cytokines in the CSF may better reflect neuroinflammation than those in the plasma, although CSF sampling is not easy, particularly in CM children, and difficult to implement in routine clinical practice. Interestingly, we found that elevated plasma levels of angiopoietin-2, a marker of endothelial activation, were associated with neurologic deficit in children at discharge and at D21–28. Angiopoietin-2 was previously found to be associated with cognitive injury over 2 years after a severe malaria episode in children42, and it is widely accepted as a biomarker of malaria severity19,43,44. In our study, at discharge, but not at D21–28, urine levels of reduced glutathione (GSH) were lower in children with neurologic deficit. To the best of our knowledge, this is the first report of such an association after severe malaria. This result highlights the importance of the antioxidant response in resolving neuroinflammation during CM. A study carried out in children presenting with acute lymphoblastic leukaemia, a disease associated with a high risk for cognitive impairment, also reported that higher initial GSH levels, measured in CSF, were associated with better cognition over 1 year of follow-up45, underlining the weight of the antioxidant response in the neurologic state.
In addition, plasma and serum markers are inconsistently related to MR. Villaverde et al.. reported similar plasma levels of proinflammatory cytokines (TNF, IFNϒ, IL-1β, IL-10) and oxidative stress markers in both MR-positive and MR-negative children with CM46. In contrast, in nonmalarial retinopathy such as retinopathy of prematurity and diabetic retinopathy, the inflammatory response is consistently associated with retinopathy47,48,49. In a murine model of diabetic retinopathy, M2 polarization of macrophages via IL-10 was even found to reduce retinopathy49. In line with this, we found that MR was associated with a lower anti-inflammatory response, which resulted in a lower LXA4/LTB4 ratio, CCL17 and CCL22 levels (two chemokines implicated in Th2 responses), and regulatory T cell migration21. The CXCL5 level, which is implicated in neutrophil trafficking, was also lower in MR-positive patients. This result is surprising, because the neutrophil response participates in the inflammatory response to limit infection but also contributes to neuroinflammation and tissue damage and is a therapeutic target in ocular diseases50. However, a study conducted in Malawi demonstrated impaired neutrophil chemotaxis in MR-positive versus MR-negative patients, despite higher levels of inflammatory cytokines and neutrophil activation51. The authors attributed this failure to the presence of free haem in plasma, known to decrease neutrophil migratory capacity via haem-oxygenase activity52,53,54. Such a paradoxical result may be due to the specificity of malarial infection.
Conclusion
In a population of children with CM admitted in tertiary care hospitals, a high fatality rate was found. MR at admission was associated with the use of traditional medicine and with the study site. These factors may translate into difficulties accessing conventional care. Neurological deficits were strikingly more prevalent at discharge than a few weeks later. MR at admission was predictive of neurological deficit at discharge, while endothelium activation was associated with neurological deficit both at discharge and at D21–28. The NeuroCM study mainly explored inflammation in comatose vs. non-comatose children infected with malaria and therefore included a large battery of immunological indicators2. This allowed the study of associations between these indicators and health outcomes, MR, and neurological deficit. Further studies on neurological outcomes of CM should be adequately powered to provide more robust analysis of determinants of disabilities observed early after discharge and also to explore cognitive abilities that may be affected by CM.
Methods
Study design and participants
This prospective study was conducted at two university hospitals from March 1 to November 30, 2018: the Centre Hospitalier Universitaire de Zone d’Abomey Calavi/Sô-Ava (CHUZ-AS) and Centre Hospitalier Universitaire de la Mère et de l’Enfant Lagune (CHU-MEL) in Cotonou, Benin. A clinical research physician in each hospital was specifically trained to manage the NeuroCM study. Patient management and the investigations performed to assess the aetiology of coma are detailed elsewhere2.
The inclusion criteria were children aged 24–71 months with nontraumatic coma, evidence of P. falciparuminfection in blood smears and/or PCR, a negative result in human immunodeficiency virus (HIV) rapid RDT, and a Blantyre Coma Score (BCS) ≤ 2. The exclusion criteria were the absence of parental consent, any coinfection (as detected via blood and cerebrospinal fluid culture, serology tests, and multiplex PCR), pre-existent neurological disease, and traumatic or toxic or nontraumatic nonmalarial coma (see details in reference2).
Ethics review and approval
Ethics approval for the NeuroCM study was obtained from the Comité National d’Ethique pour la Recherche en Santé of Benin (n°67/MS/DC/SGM/DRFMT/CNERS/SA; 10/17/2017). The study was approved by the Comité consultatif de déontologie et d’éthique of Institut de Recherche pour le Développement (IRD; 10/24/2017). Written informed consent was obtained from the parents or guardians of all included children. All study procedures were performed in accordance with the institutional policies, guidelines and regulations pertaining to research involving human subjects.
Fundoscopy
Within 24 h after admission, direct ophthalmoscopy was performed by a trained clinical research physician, with an EyePax 1.0 Dioptrix® ophthalmoscope, to determine MR status. Imaging of the exam was made possible with an adaptor on a mobile phone. Images were interpreted retrospectively and independently by two experienced ophthalmologists; in cases of disagreement, the expertise of a third ophthalmologist was required. MR was defined as the presence of retinal whitening, haemorrhage, or vascular changes with or without papilledema11.
Neurocognitive deficits screener
A questionnaire was administered by a research clinician to the caregiver at discharge and between days 21 and 28 post-discharge (D21–28), using a questionnaire derived from the Ten Question questionnaire (TQ), a screening tool already used in Benin55. The questionnaire was administered to the child’s parents/guardians to gather information on their perception of neurodevelopmental deficits compared to before CM. The questionnaire included 8 of the 10 questions of the TQ. It included the following neurodevelopmental dimensions: standing, walking, sitting, vision, hearing, receptive language, tonus, epileptic crisis, expressive language, and mental retardation. A neurological deficit was considered as present when at least one difficulty among these was present. For the assessments on days 21–28, the parents/guardians were invited to come back to the hospital but the assessment was performed at home if necessary.
Plasma biomarkers
Plasma levels of 17 biomarkers were measured as described previously19, using Luminex technology and the Human Premixed Multi-Analyte Kit (LXSAHM-17, R&D Systems, Lille, France). For plasma soluble EPCR, concentration was determined via ELISA according to the manufacturer’s recommendations (DuoSet, R&D Systems).
Statistical analysis
In descriptive analysis, qualitative variables are expressed as numbers (%), and quantitative variables are given as mean ± standard deviation (SD) when they followed a normal distribution and as median (interquartile range) when they did not. In comparative analysis, comparison of proportions was performed using Pearson’s chi-square test or Fisher’s exact test. The Mann–Whitney U-test was used to compare quantitative variables without a normal distribution. The McNemar test was used to compare the results of neurological assessments performed at discharge and at D21–28 post-discharge (neurocognitive deficits screener) to determine whether the proportions of the paired data obtained were statistically different. To identify predictive factors of health outcomes (MR and neurological deficits), a logistic regression model was performed. Variables associated with a p-value < 0.20 in univariate analyses were included in the model. The threshold of significance was set to 5% (p < 0.05). SAS 9.4 software was used.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
References
WHO. World malaria report (2023). https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2023
Brisset, J. et al. Non-traumatic coma in young children in Benin: Are viral and bacterial infections gaining ground on cerebral malaria? Infect. Dis. Poverty 11, 29 (2022).
Liu, Q., Jing, W., Kang, L., Liu, J. & Liu, M. Trends of the global, regional and National incidence of malaria in 204 countries from 1990 to 2019 and implications for malaria prevention. J. Travel Med. 28, taab046 (2021).
Birbeck, G. L. et al. Blantyre malaria project epilepsy study (BMPES) of neurological outcomes in retinopathy-positive paediatric cerebral malaria survivors: A prospective cohort study. Lancet Neurol. 9, 1173–1181 (2010).
Severe malaria. Trop. Med. Int. Health 19(Suppl 1), 7–131 (2014).
Schiess, N. et al. Pathophysiology and neurologic sequelae of cerebral malaria. Malar. J. 19, 266 (2020).
Idro, R., Marsh, K., John, C. C. & Newton, C. R. J. Cerebral malaria: Mechanisms of brain injury and strategies for improved neurocognitive outcome. Pediatr. Res. 68, 267–274 (2010).
Boivin, M. J., Vokhiwa, M., Sikorskii, A., Magen, J. G. & Beare, N. A. V. Cerebral malaria retinopathy predictors of persisting neurocognitive outcomes in Malawian children. Pediatr. Infect. Dis. J. 33, 821–824 (2014).
Dondorp, A. M. et al. Artesunate versus quinine in the treatment of severe falciparum malaria in African children (AQUAMAT): An open-label, randomised trial. Lancet 376, 1647–1657 (2010).
Coulibaly, D. et al. Shifts in the clinical epidemiology of severe malaria after scaling up control strategies in Mali. Front. Neurol. 13, 988960 (2022).
Beare, N. A. V., Lewallen, S., Taylor, T. E. & Molyneux, M. E. Redefining cerebral malaria by including malaria retinopathy. Future Microbiol. 6, 349–355 (2011).
Brodeur, K. R. N., Herculano, A. & Oliveira, K. Clinical aspects of malarial retinopathy: A critical review. Pathog. Glob. Health 117, 450–461 (2023).
Beare, N. A. V., Harding, S. P., Taylor, T. E., Lewallen, S. & Molyneux, M. E. Perfusion abnormalities in children with cerebral malaria and malarial retinopathy. J. Infect. Dis. 199, 263–271 (2009).
Potchen, M. J. et al. Acute brain MRI findings in 120 Malawian children with cerebral malaria: New insights into an ancient disease. AJNR Am. J. Neuroradiol. 33, 1740–1746 (2012).
Beare, N. A. et al. Prognostic significance and course of retinopathy in children with severe malaria. Arch. Ophthalmol. 122, 1141–1147 (2004).
Postels, D. G. et al. Neurologic outcomes in retinopathy-negative cerebral malaria survivors. Neurology 79, 1268–1272 (2012).
Dunst, J., Kamena, F. & Matuschewski, K. Cytokines and chemokines in cerebral malaria pathogenesis. Front. Cell. Infect. Microbiol. 7, 324 (2017).
Atiku, S. M., Louise, N. & Kasozi, D. M. Severe oxidative stress in sickle cell disease patients with uncomplicated plasmodium falciparum malaria in Kampala, Uganda. BMC Infect. Dis. 19, 600 (2019).
Royo, J. et al. Elevated plasma interleukin-8 as a risk factor for mortality in children presenting with cerebral malaria. Infect. Dis. Poverty 12, 8 (2023).
Zanini, G. M., Martins, Y. C., Cabrales, P., Frangos, J. A. & Carvalho, L. J. M. S-nitrosoglutathione prevents experimental cerebral malaria. J. Neuroimmune Pharmacol. 7, 477–487 (2012).
Griffith, J. W., Sokol, C. L. & Luster, A. D. Chemokines and chemokine receptors: Positioning cells for host defense and immunity. Annu. Rev. Immunol. 32, 659–702 (2014).
Natarajan, R. & Nadler, J. L. Lipid inflammatory mediators in diabetic vascular disease. Arterioscler. Thromb. Vasc Biol. 24, 1542–1548 (2004).
Praticò, D. et al. 12/15-lipoxygenase is increased in Alzheimer’s disease: Possible involvement in brain oxidative stress. Am. J. Pathol. 164, 1655–1662 (2004).
Wu, Z. et al. Arachidonic acid metabolism is elevated in Mycoplasma gallisepticum and Escherichia coli co-infection and induces LTC4 in serum as the biomarker for detecting poultry respiratory disease. Virulence 11, 730–738 (2020).
Souza, M. C. et al. Lipoxin A4 attenuates endothelial dysfunction during experimental cerebral malaria. Int. Immunopharmacol. 24, 400–407 (2015).
Joste, V. et al. Identification of plasmodium falciparum and host factors associated with cerebral malaria: Description of the protocol for a prospective, case-control study in Benin (NeuroCM). BMJ Open (2019).
Taylor, T. E. et al. Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Nat. Med. 10, 143–145 (2004).
Koura, K. G. et al. Usefulness of child development assessments for low-resource settings in Francophone Africa. J. Dev. Behav. Pediatr. 34, 486–493 (2013).
Kakooza-Mwesige, A. et al. Adaptation of the ‘ten questions’ to screen for autism and other neurodevelopmental disorders in Uganda. Autism 18, 447–457 (2014).
Lewallen, S., Taylor, T. E., Molyneux, M. E., Wills, B. A. & Courtright, P. Ocular fundus findings in Malawian children with cerebral malaria. Ophthalmology 100, 857–861 (1993).
WHO Guidelines for malaria. https://www.who.int/publications/i/item/guidelines-for-malaria.
White, V. A. et al. Correlation of retinal haemorrhages with brain haemorrhages in children dying of cerebral malaria in Malawi. Trans. R Soc. Trop. Med. Hyg. 95, 618–621 (2001).
Lewallen, S. et al. Retinal findings predictive of outcome in cerebral malaria. Trans. R. Soc. Trop. Med. Hyg. 90, 144–146 (1996).
Villaverde, C., Namazzi, R., Shabani, E., Opoka, R. O. & John, C. C. Clinical comparison of retinopathy-positive and retinopathy-negative cerebral malaria. Am. J. Trop. Med. Hyg. 96, 1176–1184 (2017).
Boivin, M. J. et al. Cognitive impairment after cerebral malaria in children: A prospective study. Pediatrics 119, e360–366 (2007).
Ssemata, A. S. et al. Association of severe malaria with cognitive and behavioural outcomes in low- and middle-income countries: A meta-analysis and systematic review. Malar. J. 22, 227 (2023).
John, C. C. et al. Cerebrospinal fluid cytokine levels and cognitive impairment in cerebral malaria. Am. J. Trop. Med. Hyg. 78, 198–205 (2008).
Shabani, E. et al. Elevated cerebrospinal fluid tumour necrosis factor is associated with acute and long-term neurocognitive impairment in cerebral malaria. Parasite Immunol. 39 (2017).
Boivin, M. J. et al. Evaluating immunopathogenic biomarkers during severe malaria illness as modifiers of the neuropsychologic benefits of computer cognitive games rehabilitation in Ugandan children. Pediatr. Infect. Dis. J. 38, 840–848 (2019).
Chaparro-Huerta, V. et al. Proinflammatory cytokines, enolase and S-100 as early biochemical indicators of hypoxic-ischemic encephalopathy following perinatal asphyxia in newborns. Pediatr. Neonatology. 58, 70–76 (2017).
Gessler, P., Schmitt, B., Prètre, R. & Latal, B. Inflammatory response and neurodevelopmental outcome after open-heart surgery in children. Pediatr. Cardiol. 30, 301–305 (2009).
Ouma, B. J. et al. Plasma angiopoietin-2 is associated with age-related deficits in cognitive sub-scales in Ugandan children following severe malaria. Malar. J. 20, 17 (2021).
de Jong, G. M., Slager, J. J., Verbon, A., van Hellemond, J. J. & van Genderen, P. J. J. Systematic review of the role of angiopoietin-1 and angiopoietin-2 in plasmodium species infections: Biomarkers or therapeutic targets? Malar. J. 15, 581 (2016).
Balerdi-Sarasola, L. et al. Host biomarkers for early identification of severe imported plasmodium falciparum malaria. Travel Med. Infect. Dis. 54, 102608 (2023).
Hooke, M. C. et al. The longitudinal parallel process analysis of biomarkers of oxidative stress, symptom clusters, and cognitive function in children with leukemia. J. Pediatr. Oncol. Nurs. 37, 244–254 (2020).
Villaverde, C. et al. Retinopathy-positive cerebral malaria is associated with greater inflammation, Blood-Brain barrier breakdown, and neuronal damage than retinopathy-negative cerebral malaria. J. Pediatr. Infect. Dis. Soc. 9, 580–586 (2020).
Almutairi, M. et al. Biomarkers in retinopathy of prematurity: A systematic review and meta-analysis. Front. Pediatr. 12, 1371776 (2024).
Kaviarasan, K. et al. Low blood and vitreal BDNF, LXA4 and altered Th1/Th2 cytokine balance are potential risk factors for diabetic retinopathy. Metabolism 64, 958–966 (2015).
Lee, S. J. et al. IL-10‐induced modulation of macrophage polarization suppresses outer‐blood‐retinal barrier disruption in the streptozotocin‐induced early diabetic retinopathy mouse model. FASEB J. 38, e23638. https://doi.org/10.1096/fj.202400053R
Bammidi, S. et al. Neutrophils in ocular diseases. Int. J. Mol. Sci. 25, 7736 (2024).
Feintuch, C. M. et al. Activated neutrophils are associated with pediatric cerebral malaria vasculopathy in Malawian children. mBio 7, e01300–01315 (2016).
Lin, Y. T. et al. Heme oxygenase-1 suppresses the infiltration of neutrophils in rat liver during sepsis through inactivation of p38 MAPK. Shock 34, 615–621 (2010).
Czaikoski, P. G. et al. Heme oxygenase inhibition enhances neutrophil migration into the Bronchoalveolar spaces and improves the outcome of murine pneumonia-induced sepsis. Shock 39, 389–396 (2013).
Abdalla, H. B. et al. Activation of PPAR-γ induces macrophage polarization and reduces neutrophil migration mediated by Heme Oxygenase 1. Int. Immunopharmacol. 84, 106565 (2020).
Mireku, M. O. et al. Prenatal hemoglobin levels and early cognitive and motor functions of one-year-old children. Pediatrics 136, e76–83 (2015).
Acknowledgements
We are grateful to all patients and their parents for participating in this study. We are thankful to the nurses of the CHU-MEL hospital (CHU-Mère et Enfant de la Lagune) and Hôpital de zone de Calavi for their help in the collection of samples. We thank TL and AM for implementing fundoscopy and Good Clinical Practices at study site, and Latifou Dramane for managing children’s follow-up. Finally, we thank all the members of the NeuroCM group for their contribution to the project. NeuroCM collaboration group: Dissou Affolabi (Pediatric Department, Calavi Hospital, Calavi, Benin); Nicolas Argy (MERIT UMR 261, IRD, Université de Paris, Paris, France); Bibiane Biokou (Pediatric Department, Mother and Child University and Hospital Center (CHUMEL), Cotonou, Benin); Jean-Eudes Degbelo (Institut de Recherche Clinique du Bénin (IRCB), Calavi, Benin); Philippe Deloron (MERIT UMR 261, IRD, Université de Paris, Paris, France); Latifou Dramane (Institut de Recherche Clinique du Bénin (IRCB), Abomey Calavi, Benin); Jérémy Fraering (MERIT UMR 261, IRD, Université de Paris, Paris, France); Emilie Guillochon (MERIT UMR 261, IRD, Université de Paris, Paris, France); Sayeh Jafari-Guemouri (MERIT UMR 261, IRD, Université de Paris, Paris, France); Ludivine Houzé (MERIT UMR 261, IRD, Université de Paris, Paris, France); Valentin Joste (MERIT UMR 261, IRD, Université de Paris, Paris, France); Claire Kamaliddin (MERIT UMR 261, IRD, Université de Paris, Paris, France); Anaïs Labrunie (NET, INSERM, Université de Limoges, Limoges, France); Yélé Ladipo (Pediatric Department, Mother and Child University and Hospital Center (CHUMEL), Cotonou, Benin); Achille Massougbodji (Institut de Recherche Clinique du Bénin (IRCB), Abomey Calavi, Benin); Jade Papin (MERIT UMR 261, IRD, Université de Paris, Paris, France); Bernard Pipy (PHARMADEV, Université de Toulouse, IRD, UPS, France); Pierre-Marie Preux (NET, INSERM, Université de Limoges, Limoges, France); Marie Raymondeau (NET, INSERM, Université de Limoges, Limoges, France); Darius Sossou (Institut de Recherche Clinique du Bénin (IRCB), Abomey Calavi, Benin); Brigitte Techer (MERIT UMR 261, IRD, Université de Paris, Paris, France); Bertin Vianou (Institut de Recherche Clinique du Bénin (IRCB), Abomey Calavi, Benin).
Funding
This work was funded by the French National Research Agency (ANR-17-CE17-0001). The funding organization did not play any role in the trial design, data collection, analysis of results, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
FB, AA, and JFF conceptualised or designed the study. EK and LA recruited the patients and collected the data, under JA, IDD and FB supervision. AM trained the clinical team to the assessment of children’s clinical status and to the management of severe malaria. TL trained the clinical team to perform ocular fundus and helped interpret the data. JB, KA, IB and FBL analysed, and interpreted the data. AA and JR performed the experiments and analysed the data on immune factors. JB, KAB, AA, FBL and JFF drafted the manuscript. All members of the NeuroCM group have substantially contributed to the conception, design or organisation of the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bodeau-Livinec, F., Aubouy, A., Besnard, I. et al. Determinants of retinopathy and short-term neurological outcomes after cerebral malaria. Sci Rep 15, 13610 (2025). https://doi.org/10.1038/s41598-025-97468-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-97468-4