Abstract
Patients with hemophilia (PWH) constantly suffer hemarthrosis due to the lack of coagulation factors, resulting in progressive deformity of the hip joint. Currently, there is a dearth of understanding on the unusual morphology of proximal femur in PWH. To explore how does the Dorr classification of proximal femur affect the total hip arthroplasty (THA) of PWH, we conducted a retrospective study on PWH with different Dorr classifications who underwent THA. The retrospective study comprises data of adult patients who received THA from 2018 to 2022 in the research center. Patients with a diagnosis of hemophilic arthritis and received THA were included and divided into three groups according to Dorr classification. The X-ray images were acquired before the surgery to determine the Dorr classification. The surgical time, surgical blood loss, laboratory examinations post-operation including hemoglobin (HB), total protein (TP), activated partial thromboplastin time (APTT), D-dimer (D2), C-reactive protein level (CRP), erythrocyte sedimentation rate (ESR), and functional evaluations 1 year after surgery including visual analogue scale (VAS), Harris hip score (HHS), range of motion (ROM) were collected. Kolmogorov–Smirnov test is used to test data normality, and t-test is performed by SPSS 20. P < 0.05 is considered statistically significant. 33 PWH are included in the study and have finished follow-up. All cases are male patients. Among the 33 hips, 19 (57.6%) are classified to Dorr A, and 12 (36.4%) are Dorr B, and only 2 (6%) are Dorr C. No significant difference is found in expanse, hospital stay, surgical time and total blood loss. PWH with Dorr A requires significant less coagulation factor than Dorr B and Dorr C. All Dorr types of hips present good recovery from the surgery according to the perioperative examinations including hemoglobin (HB), total protein (TP), activated partial thromboplastin time (APTT), D-dimer (D2), C-reactive protein level (CRP), erythrocyte sedimentation rate (ESR), and thigh circumference (TC). The 2-year follow-up demonstrates favorable functional rehabilitation according to functional evaluations including visual analogue scale (VAS), Harris hip score (HHS), and range of motion (ROM). In this study, we find that PWH tend to have higher prevalence of Dorr A than the general population. PWH with Dorr A requires smaller dosage to maintain the coagulation factor activity than the Dorr B and Dorr C. Additionally, all types of hip present favorable recovery after THA. Ultimately, the study supports that THA is an effective treatment for PWH with all Dorr classifications by alleviating the pain and improve the motor function.
Similar content being viewed by others
Introduction
Hemophilia, a rare recessive X-linked genetic disorder characterized by the deficiency of coagulation factors VIII or IX, manifests primarily as a heightened susceptibility to bleeding, particularly in the joints and muscles1. Intra-articular bleeding poses a significant risk of joint cartilage damage, resulting in the development of hemophilic arthritis. Hemophilic arthropathy is frequently observed in the ankle, knee, and elbow joints, although the hip, shoulder, and wrist joints can also be affected2,3,4. Currently, there is no definitive cure for hemophilia, and the primary treatment approach involves substitution therapy, which entails the administration of exogenous factor VIII. In cases where treatment fails to halt the progression of joint damage, total hip arthroplasty (THA) is considered the gold standard treatment for end-stage hemophilic arthropathy of the hip. THA not only provides relief of pain but also restores functionality to the affected joint5,6,7,8. Nevertheless, repeated intra-articular bleeding causes recurrent synovial inflammation and consequently destruct the normal construction of hip joint, which could increase the complexity of prothesis choosing and complication control. Except for the secondary joint deformity, it is also noticed that congenital deformities of proximal femur with larger neck-shaft angle, smaller femoral offset and smaller femoral isthmus diameter exist in PWH, indicating smaller femoral medullary cavity, thinner bone cortex9. However, no study described how these deformities affect the outcome of THA in PWH.
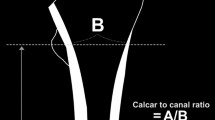
Dorr classified the proximal femur into three types10. Type A is distinguished by the robust cortex that starts at the distal end of the lesser trochanter and rapidly thicken, creating a funnel-like shape. The diaphyseal canal is narrow in this classification. In contrast, type B exhibits bone loss in proximal hip joint, and the diaphyseal canal widens, resulting in a broader canal compared to Type A. Type C is characterized by a significant loss of cortex thickness, leading to a wide medullary canal. The bone cortex appears fuzzy in this category, indicating a loss of structure.
How does the morphology of proximal femur affect the THA of PWH remains a question. By analyzing the past data, the study sought to demonstrate the relationship between the Dorr classification of proximal femur and outcome of THA in PWH.
Materials and methods
Study population
The retrospective study comprises data of PWH who received THA from 2018 to 2022 in the research center. According to previous studies, the expected standard deviation \(\left( \sigma \right)\) of isthmus diameter is 2.5 and the allowable error (\(\delta\)) was 2.211. A 2-tailed test is required with an alpha level (\(\alpha\)) of 0.05. Applying the standard formula: \(n = \frac{{\left( {Z_{\alpha } + Z_{\beta } } \right)^{2} {*}2\sigma^{2} }}{{\delta^{2} }}\) to each index, the minimum sample size (n) of our study is 28. This study is performed in line with the principles of the Declaration of Helsinki. Ethics approval has been obtained. The research is performed in accordance with relevant regulations, and informed consent has been obtained from all participants.
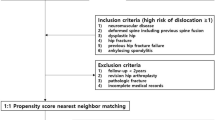
A total of 51 hemophilic patients were found in the medical records from 2018 to 2022. The inclusion criteria were as follows: 1. Diagnosed with hemophilia and received THA during the hospital stay. The exclusion criteria were as follows: 1. Patients with non-hemophilia conditions that may affect the proximal femoral morphology or bone quality, including but not limited to, a history of femoral bone tumors, hormone use, femoral osteotomy, femoral fracture, severe infection; 2. Patients without intact medical records or radiographic materials; 3. Patients who refuse to participate in the study. As a result, 3 patients were excluded due to the femoral fracture which could affect the measurements of proximal femur. 8 patients were also excluded because of incomplete radiograph materials. Subsequently, 40 patients participated in follow-up, and 7 of them were not able to contact due to unavailable telephone number. Finally, after exclusion, 33 patients were considered qualified and included in the study (Fig. 1).
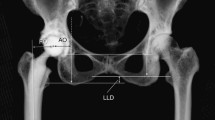
Measurements of proximal femur
The evaluation of the affected hip involved anteroposterior (AP) and lateral radiographs, along with the corresponding medical records. The radiographic materials were acquired 1 day before the surgery. To obtain standard AP and lateral radiographs of the hip, patients were positioned in a supine position with their legs internally rotated at 15º. The radiographs were taken at 4 feet (120 cm) from the x-ray machine (Philips, SRO 33100 360, permanent filtration 2, 5 AI/75, nominal voltage 150kv) to minimize the potential bias caused by hip malrotation.
The parameters of the proximal femur were assessed using a Picture Archiving and Communication System (PACS). Two resident doctors independently evaluated the parameters, under the supervision of a senior surgeon. The result was determined as the average number of the data collected by two doctors.
To determine which Dorr type does a proximal femur belong to, several indexes were measured, including medullary canal diameter at the level of lesser trochanter (MCDL) and the level of 10 cm distal to lesser trochanter (MCDL-10), and the ratio of the MCDL-10 to the MCDL. According to the description of Dossick and Dorr12, the MCDL-10 and MCDL were measured on X images. MCDL-10/MCDL < 0.5 was considered Dorr A. 0.5 < MCDL-10/MCDL < 0.75 was considered Dorr B. MCDL-10/MCDL > 0.75 was considered Dorr C.
Dorr categorized the proximal femur into three types10. Type A is identified by a sturdy cortex that initiates at the distal end of the lesser trochanter and swiftly thickens, forming a funnel-shaped structure. The diaphyseal canal is narrow in this type. In contrast, Type B displays bone loss in the proximal hip joint, with the diaphyseal canal expanding to create a wider canal than Type A. Type C is defined by a significant decrease in cortex thickness, resulting in a broad medullary canal. The bone cortex appears indistinct in Type C.
Follow-up and data collection
The same senior doctor performed the surgeries under general anesthesia through posterior approach. The most matched Uncemented biological femoral stem was used in all surgeries according to patients’ femoral condition. Before the surgery, the concentration of coagulation factors was boosted to 80% or above to meet the requirement of surgery. The surgical time, surgical blood loss, blood coagulation factor usage was collected by the surgeon. Laboratory examinations post-operation including hemoglobin (HB), total protein (TP), activated partial thromboplastin time (APTT), D-dimer (D2), C-reactive protein level (CRP), erythrocyte sedimentation rate (ESR), and thigh circumference (TC) was measured in 1 day before operation and 1 day, 1 week, 2 weeks, 1 month after the operation by a resident doctor. Functional evaluations, including visual analogue scale (VAS), Harris hip score (HHS) and range of motion (ROM), were collected in 1 day before operation and 1 day, 1 week, 2 weeks, 1 month, 3 months, 6 months, 1 year, 2 years after the operation by the same resident doctor. Blood coagulation factor usage was the sum of factor used in perioperative and surgery period. Total blood loss was calculated according to the equation as follows: total blood loss = preoperative blood volume (PBV) * (preoperative hematocrit (HCT)—postoperative HCT)/(preoperative HCT + postoperative HCT) * 2; PBV = k1 * height (m)3 + k2 * weight (kg) + k3 (k1 = 0.3669,·k2 = 0.03219,·k3 = 0.6041). This step was performed by 2 resident doctors with WINEX (1.4.2) medical system.
Statistical analysis
We performed all data analysis on the SPSS 20 (IBM, US). Descriptive statistics are utilized to summarize variables as mean ± standard deviation or frequency (percentage) based on the nature of the data. We used Shapiro–Wilk to test the normality of the data, showing abnormal distribution. Thus, rank sum test was performed between each group. We employed Cronbach’s alpha to test the inter-observer reliability and consistency. P < 0.05 is considered statistically significant.
Results
Among the 33 hips, 19 (57.6%) were classified to Dorr A, and 12 (36.4%) were Dorr B, and only 2 (6%) were Dorr C (Fig. 2). No statistical significance was found between the three groups, regarding the age, height, and BMI. All cases were male patients. 31 (93.9%) were hemophilia A, and 2 (6.1%) were hemophilia B (Table 1). Cronbach’s alpha test showed good reliability in all measurements (α > 0.7).
The total expanse (CNY) was 338,906.6 ± 147,175.7 (Dorr A), 455, 618.6 ± 248, 377.1 (Dorr B), 454, 774.4 ± 143, 888.2 (Dorr C). The average hospital stay (days) was 26.1 ± 7.9 (Dorr A), 32.1 ± 10.9 (Dorr B), 32.0 ± 11.3 (Dorr C). The average surgical time (hours) was 2.1 ± 0.9 (Dorr A), 2.0 ± 1.5 (Dorr B), 2.3 ± 0.4 (Dorr C). The average blood coagulation usage (iu) was 9631.6 ± 3188.0 (Dorr A), 16,666.7 ± 5069.2 (Dorr B), 21,000.0 ± 8485.3 (Dorr C). The total blood loss (ml) was 1273.7 ± 434.9 (Dorr A), 1468.4 ± 669.3 (Dorr B), 2020.2 ± 456.5 (Dorr C). There was no statistical significance between the groups in surgical time, total blood loss, hospital stay and total expanse. However, blood coagulation factor usage in Dorr B was significantly larger than Dorr A (Table 2). Regarding the laboratory examinations and functional evaluation, the line chart demonstrated that all groups presented analogous trend in the involved indexes (Figs. 3 and 4). No complications occurred.
Discussion
This is the first article that studies how does the proximal femoral morphology of hemophilic patients affects the outcome of THA. First, the current study finds that PWH who underwent THA had a largest portion of Dorr A, followed by Dorr B and the least in Dorr C. Second, PWH with Dorr A may require less blood coagulation factor than those with Dorr B. Finally, THA is an effective treatment for PWH with all types of Dorr classification.
There is no current study that illustrates the morphology of proximal femur regarding the Dorr classification. P N Karayiannis et al. studied 500 hips and found that only 8% Dorr A, 85% Dorr B and 7% Dorr C in normal people13. PJ Tong et al. found that PWH were prone to smaller isthmus than the others9. In this study, 57.6% Dorr A is found in PWH, which outnumbers that in normal people. It is assumable that there is more Dorr A in PWH.
Dorr A, usually described as champagne type, has slim isthmus and gradually thickening medullary cavity towards the proximal end of femur, indicating that it has smaller volume of femoral medullary cavity. In this study, PWH with Dorr A present significant smaller usage of blood coagulation factor, and although no statistical significance is found, there is less blood loss in Dorr A than the others. Subsequently, the laboratory examinations present well recovery for all groups. Common improvements of function, including alleviation of pain, increasement of mobility, are seen in all hips, regardless of morphology.
Dorr B and Dorr C have thinner cortical bone. The current evidence shows that FVIII and FIX deficiency may directly affect bone metabolism by interfering with the RANK/RANKL/OPG pathway, thus PWH with severe osteoporosis may suffer larger amount of blood loss during the THA14. Additionally, Dorr C were considered to be a significant risk factor to periprosthetic fracture in non-hemophilic people15. The osteoporosis may add to the risk of periprosthetic fracture in PWH. In this study, although no patients with Dorr C are found to suffer prothesis loosening in the last visit, their follow-ups will be continued. As a result, it is probably recommendable to apply more coagulation factor and regular anti-osteoporosis treatment to those with Dorr B and Dorr C. However, the quantitative relation between the blood loss and osteoporosis should be further established.
All PWH suffer joint pain and ankylosis in the end stage of hip coxitis. Xisheng Weng et al. performed a retrospective study on 24 PWH, reporting a preferable result in THA16. Our study has expanded the study population and further explored the influence of femoral morphology on THA. Besides, we point out that Dorr B and Dorr C might require larger dosage to maintain the coagulation factor activity than Dorr A. Thus, this is a valuable research for the reference of surgeons in this field.
There are several limitations in this study. First, the population of PWH is small, especially for Dorr C. This may cause bias in the comparison between Dorr C and other groups. Besides, the follow-up time is relatively short comparing to the life span of the prosthesis, thus potential complications may occur in the future.
Conclusion
In the current study, it was observed that individuals with PWH exhibited a higher prevalence of Dorr A compared to the general population. Among PWH, those with Dorr A might necessitate a relatively lower dosage to sustain the coagulation factor activity in contrast to those with Dorr B and Dorr C. Moreover, for all types of hips, favorable recovery outcomes were achieved following total hip arthroplasty. Overall, THA proves to be an efficacious treatment for PWH across all Dorr classifications, as it effectively mitigates pain and enhances motor function.
Data availability
The data that supports the findings of this study are available with reasonable request to the authors.
References
He, B. J. et al. Bilateral synchronous total hip arthroplasty for end-stage arthropathy in hemophilia A patients: A retrospective study. Medicine (Baltimore) 101(27), e29667 (2022).
Srivastava, A. et al. Guidelines for the management of hemophilia. Haemophilia 19, e1-47 (2013).
Beeton, K., Rodriguez-Merchan, E. C. & Alltree, J. Total joint arthroplasty in haemophilia. Haemophilia 6, 474e-e481 (2000).
Miles, J., Rodriguez-Merchan, E. C. & Goddard, N. J. The impact of haemophilia on the success of total hip arthroplasty. Haemophilia 14, 81e-e84 (2008).
Bolton-Maggs, P. H. Optimal haemophilia care versus the reality. Br J Haematol 132, 671–682 (2006).
Parsa, A., Azizbaig Mohajer, M. & Mirzaie, M. Hip arthroplasty in haemophilia: a systematic review. Hip Int 28, 459–467 (2018).
Lee, S. H. et al. Cementless total hip arthroplasty for haemophilic arthropathy: Follow-up result of more than 10 years. Haemophilia 21, e54–e58 (2015).
Wu, G. L. et al. Total hip arthroplasty in hemophilia patients: A mid-term to long-term follow-up. Orthop. Surg. 9, 359–364 (2017).
Gong, Y. et al. Bleeder’s femur: The proximal femoral morphology in hemophilic patients who underwent total hip arthroplasty. Orthop. Surg. 16(3), 718–723 (2024).
Dorr, L. D. et al. Structural and cellular assessment of bone quality of proximal femur. Bone 14, 231–242 (1993).
Parsa, A., Azizbaig Mohajer, M. & Mirzaie, M. Hip arthroplasty in haemophilia: A systematic review. Hip Int. 28, 459–467 (2018).
Mazzawi, E., Ghrayeb, N., Khury, F., Norman, D. & Keren, Y. A comparison between Austin-Moore and Corail prosthesis regarding intraoperative periprosthetic femur fractures in hip hemiarthroplasty. Sci. Rep. 12(1), 6340 (2022).
Karayiannis, P. N., Cassidy, R. S., Hill, J. C., Dorr, L. D. & Beverland, D. E. The relationship between canal diameter and the Dorr classification. J. Arthroplast. 35(11), 3204–3207 (2020).
Lin, X. et al. Pathogenesis and treatment of osteoporosis in patients with hemophilia. Arch Osteoporos. 18(1), 17 (2023).
Kheir, M. M. et al. The influence of Dorr type and femoral fixation on outcomes following total hip arthroplasty for acute femoral neck fractures: A multicenter study. J. Arthroplast. 38(4), 719–725 (2023).
Wu, G. L. et al. Total hip arthroplasty in hemophilia patients: A mid-term to long-term follow-up. Orthop. Surg. 9(4), 359–364 (2017).
Funding
This work was financially supported by Zhejiang Provincial Natural Science Foundation of China under Grant No. LQ22H270006, and Zhejiang Province Traditional Chinese Medicine Science and Technology Program under Grant No. 2024ZL044.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Y.G. and H.S.. The first draft of the manuscript was written by Y.G. and H.H., and all authors commented on previous versions of the manuscript. H.Z., S.L., and P.T. reviewed the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Approval was granted by the Ethics Committee of The First Affiliated Hospital of Zhejiang Chinese Medical University (Zhejiang Provincial Hospital of Chinese Medicine) (Date: April 12, 2023/No. 2023-KLS-130–01).
Patient consent statement
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gong, Y., Huang, H., Su, H. et al. How does the Dorr classification of proximal femur affect the total hip arthroplasty of hemophilic patients: a retrospective study. Sci Rep 15, 16575 (2025). https://doi.org/10.1038/s41598-025-97628-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-97628-6