Abstract
Dual-energy X-ray absorptiometry (DXA) is the standard for bone mineral density (BMD) assessment but is often inaccessible to cognitively or physically impaired care home patients. Radiofrequency echographic multi-spectrometry (REMS), a portable and radiation-free alternative, enables effective BMD evaluation in this vulnerable and underserved population. This cross-sectional study assessed BMD using REMS in 260 patients aged ≥ 70 years (39 males, 221 females; mean age 82.29 years) between April 2023 and July 2024. Osteoporosis diagnosis was based on T-scores < − 2.5 SD or history of fragility fractures, with severe osteoporosis defined by WHO criteria and high fracture risk by lumbar T-scores < − 3.3 SD. Care home patients had significantly lower BMD and T-scores than outpatients, with 56.3% diagnosed with severe osteoporosis and 71.8% exhibiting lumbar T-scores < − 3.3 SD. Despite high fracture risks, only 12.7% of care home patients received treatment. These trends were consistent across all age groups, revealing a high prevalence and severity of osteoporosis in care home residents. REMS has unveiled a substantial treatment gap in this population, emphasizing the critical need for improved osteoporosis management and proactive interventions to reduce fracture risks among care home patients worldwide.
Similar content being viewed by others
Introduction
Osteoporosis is a common skeletal disorder characterized by decreased bone mineral density (BMD) and altered bone microarchitecture, which increases the risk of fragility fractures1,2,3. These fractures often result in reduced daily living activities and increased mortality rates, thereby placing a significant burden on healthcare systems4,5. Although the site and method of measurement may vary, substantial evidence indicates that BMD measurement is a reliable predictor of fragility fractures6,7. BMD assessment using dual-energy X-ray absorptiometry (DXA) is widely regarded as the gold standard for assessing the risk of fragility fractures8. Early measurement of BMD using DXA and initiation of osteoporosis treatments are considered essential for extending healthy life expectancy, particularly in aging populations9.
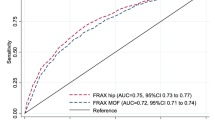
Despite its vital role in clinical settings, DXA has limited availability for osteoporosis screening in many nursing facilities such as care homes10,11. BMD measurement using DXA requires transportation to a radiologic facility and patient understanding and cooperation, which can be challenging for cognitively or physically impaired individuals residing in care homes12. Nevertheless, falls and fragility fractures are prevalent among care home residents. Ooms et al. demonstrated that institutionalized elderly individuals have a five- to eight-fold greater risk of hip fractures than independently living elderly individuals of the same age and sex13. Fracture risk assessment tool (FRAX) is a simple method for assessing the risk of fragility fracture. However, a notable limitation is that it may underestimate fracture risk when BMD is not included in the assessment. While the inclusion of BMD improves the predictive accuracy of FRAX, the measurement of BMD itself still relies on existing instruments such as DXA, which are often bulky and not readily accessible in all settings. In addition, its applicability may be constrained in certain populations due to insufficient epidemiological data14,15. Therefore, there is a high demand for devices that can effectively screen individuals with limited mobility and high fracture risk.
Recently, radiofrequency echographic multi-spectrometry (REMS) has emerged as a revolutionary tool for BMD measurements owing to its radiation-free and portable nature16. The diagnostic accuracy of REMS for osteoporosis is comparable to that of DXA, and its use as an alternative to DXA is expanding17,18. Beyond diagnostic accuracy, REMS has been shown to be unaffected by internal artifacts, such as degenerative changes and calcification, which pose significant challenges in DXA19,20,21. REMS has the potential to provide appropriate BMD assessment for patients with limited opportunities to undergo DXA because of reduced mobility. However, there are currently no reports on the effectiveness of REMS in care home settings. We hypothesized that the REMS is a feasible and effective method for assessing BMD in elderly individuals, including those with limited mobility in care homes. This study aimed to investigate the prevalence and trends of osteoporosis by evaluating BMD in care home patients using REMS, compared to orthopaedic and internal medicine outpatients.
Materials and methods
Study design and participants
This cross-sectional study included 70 or older outpatients who underwent BMD measurements using the REMS at an orthopedic hospital and family clinic between April 2023 and July 2024, as well as patients admitted to a care home in September 2023. Patients who were unable to lie in a supine position because of spinal deformities or comorbid conditions, and were excluded from the study. This study was approved by the local ethics committee of Iwamizawa Hokushokai Hospital (approval number 0023-001), and informed consent was obtained from all participants. For patients who were unable to provide informed consent due to severe intellectual disabilities or other conditions impairing decision-making capacity, proxy consent was obtained from a close relative. The care home patients who participated in this study had not undergone any osteoporosis screening after entering the care home.
The following data were collected from each participant: age, sex, weight, height, body mass index (BMI), smoking status, alcohol consumption, comorbid conditions (e.g., rheumatoid arthritis [RA], diabetes mellitus [DM], and chronic kidney disease [CKD]), presence of malignant tumors, medication use (including glucocorticoids [GC], sleeping aids, antidepressants, methotrexate, warfarin, and osteoporosis drugs), and history of fragility fractures (including vertebral fractures and proximal femoral fractures). Patients who had an estimated glomerular filtration rate < 60 ml/min/1.73m2 for more than 3 months in the past were considered to have CKD. Patients presenting with comorbidities or lifestyle factors that could contribute to secondary osteoporosis were not classified as having primary osteoporosis. BMD assessments for all participants were conducted using REMS (Echolight SPA, Lecce, Italy). All REMS measurements were performed by a trained doctor or radiologist, whose competence was verified by a third-party organization after demonstrating a stable learning curve through appropriate training. The measurement precision of the REMS has been previously reported in recent literatures22. REMS demonstrates high reproducibility and accuracy comparable to DXA, with precision errors falling within clinically acceptable limits for assessments of the lumbar spine and femoral neck. It has been reported that both the intra-operator and inter-operator coefficients of variation are low23. Finally, the measurements and the real echography images taken in this study were also quality checked by a third-party organization to ensure accuracy and validity.
The diagnostic criteria for osteoporosis were defined as a T-score of < − 2.5 standard deviations (SD) or a history of fragility fractures. According to the World Health Organization (WHO) criteria, patients with a T-score < − 2.5 SD and a history of fragility fractures were diagnosed with severe osteoporosis. We also examined whether patients met the criterion of a lumbar spine T-score < − 3.3 SD, which has been reported as an independent indicator of high fracture risk osteoporosis24,25. This threshold was selected because it is recognized in the Japanese guidelines for primary osteoporosis as one of the criteria that can be used independently to identify high fracture risk osteoporosis. Moreover, this criterion does not require additional imaging, such as plain radiography.
Statistical analysis
Categorical variables are presented as frequencies (percentages) and compared using the chi-square test, whereas continuous variables are presented as the mean (standard error of the mean) and compared using Student’s t test. We confirmed that the normality of distribution for all continuous variables was assessed using the Shapiro–Wilk test. Univariate and multivariate analyses were performed to calculate the odds ratios (OR) and their 95% confidence intervals (CI) for severe osteoporosis and lumbar T-score < − 3.3 SD in primary osteoporosis patients.
Multivariate analyses were performed using a logistic regression model. In this study, a lumbar spine T-score < − 3.3 SD was used as a categorical threshold to define high fracture risk osteoporosis, in accordance with the Japanese guidelines for primary osteoporosis. Therefore, the Lumbar spine T-score was treated as a binary variable (< − 3.3 vs ≥ − 3.3) rather than a continuous one, and logistic regression was applied accordingly. The number of adjusting factors was carefully determined based on the sample size and finalized using the Akaike and Bayesian Information Criteria within the multivariate analysis framework to ensure the most robust model fit. All statistical analyses were performed using JMP Pro version 17.0.0 (SAS Institute, Cary, NC, USA), and the significance level was set at P < 0.05.
Results
Patient characteristics
A total of 260 patients who underwent BMD measurements using REMS participated in this study. The patient characteristics are presented in Table 1. The sex distribution included 39 males and 221 females, with an average age of 82.29 years at the time of measurement. The participants had the following average anthropometric measurements: a body weight of 49.97 kg, height of 148.67 cm, and BMI of 22.67 kg/m2. The prevalence rates of preexisting medical conditions were as follows: RA, 3.5%; DM, 7.7%; CKD, 10.0%; and malignant tumors, 13.1%. Regarding medication use, 4.6% of patients were on GC, 27.3% used sleeping pills, 3.8% took antidepressants, 3.5% were on warfarin, and 1.2% used methotrexate. The average daily dose of GC was 4.58 mg. Osteoporosis treatments were administered to 64.2% of patients, including bisphosphonates in 29.3%, denosumab in 32.3%, parathyroid hormone (PTH) in 1.8%, selective estrogen receptor modulator in 12.6%, romosozumab (ROMO) in 4.8%, and vitamin D3 alone in 3.6% of the patients. Smoking and alcohol consumption were reported in 8.5% and 13.8% of the patients, respectively. A history of fragility fractures was present in 45.0% of the patients.
Comparison of clinical characteristics between outpatients and care home patients
We showed the comparison of clinical characteristics between outpatients and care home patients in Table 2. Care home patients had significantly more male patients than outpatients (P < 0.001). Care home patients were older and leaner than outpatients (P < 0.001 and P < 0.001). Regarding comorbidities, only DM showed significant differences between the groups (P = 0.009), with care home patients being more affected than outpatients. Care home patients more medicated antidepressants and warfarin than outpatients (P < 0.001 and P = 0.007). Care home patients used osteoporosis treatments significantly less frequently than outpatients (P < 0.001), with only 12.7% using osteoporosis treatments. Smoking also differed significantly between the groups (P = 0.046), with smoking being significantly less common in outpatients than care home patients. The history of fragility fractures was less common in outpatients than care home patients (P = 0.024).
Age-specific analyses of the number of severe osteoporosis patients, patients with lumbar T-score < − 3.3SD, and non-osteoporosis patients, and BMD between outpatients and care house patients
The BMD and T-scores were evaluated using REMS in both groups, and the results were compared according to patients’ age (Table 3). In addition, we compared the number of severe osteoporosis patients, patients with a lumbar T-score < − 3.3 SD, and non-osteoporosis patients in both groups. In all patients ≧ 70 years old, the BMD and T-score of all sites were significantly lower than in care home patients than in outpatients (lumbar BMD and T-score, P = 0.001 and P = 0.015; femoral neck BMD and T-score, P = 0.008 and P = 0.007; total hip BMD and T-score, P < 0.001 and P < 0.001, respectively), and more patients, over half of patients, met the criteria of severe osteoporosis in care home patients (P = 0.020).
In 70–79 years old patients, care home patients showed significantly lower femoral neck and total hip BMD and femoral neck T-score than in outpatients (P = 0.047, P = 0.038, and P = 0.049, respectively), and more patients met the criteria of severe osteoporosis in care home patients (P = 0.009). On the other hand, in 80–89 years old patients and 90- years old patients, there were no significant difference between the groups.
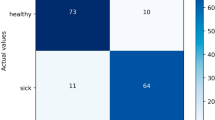
Univariate and multivariate analyses of factors influencing severe osteoporosis and lumbar T-score < − 3.3 SD in patients without possibility of secondary osteoporosis
Univariate and multivariate analyses for severe osteoporosis and lumbar T-score < − 3.3 SD were conducted on 79 patients without possibility of secondary osteoporosis in Tables 4 and 5. In univariate analyses, age and admission in care homes were significant factors influencing severe osteoporosis, and age, BMI, and history of fragility fractures were significantly influenced lumbar T-score < − 3.3 SD. Multivariate analyses indicated that only age was significantly associated with increased rates of severe osteoporosis (OR: 1.150, 95% CI 1.063–1.256, P < 0.001), whereas female, age, and BMI was significantly associated with increased rates of lumbar T-score < − 3.3 SD (OR: 15.350, 95% CI 2.417–142.797, P = 0.003; OR: 1.202, 95% CI 1.073–1.387, P < 0.001; OR: 0.762, 95% CI 0.620–0.908, P = 0.002, respectively). Admission in care homes did not have a significant effect on severe osteoporosis or lumbar T-score < − 3.3 SD in the multivariate analyses.
Discussion
This multicenter cross-sectional study included 260 patients who underwent BMD measurement using the REMS and compared care home patients with orthopedic and internal medicine outpatients. The results revealed that care home patients had significantly lower BMD and T-scores in the lumbar spine, femoral neck, and total hip than outpatients. Notably, all care home residents met the diagnostic criteria for osteoporosis, with over half meeting the criteria for severe osteoporosis, as defined by a T-score of < − 2.5 SD or a history of fragility fractures. Despite these findings, only 12.7% of care home patients received treatment for osteoporosis, highlighting a critical gap in the management of osteoporosis in this vulnerable population. This was a valuable paper that quantified the prevalence of osteoporosis and its severity in care home patients, which until now was only vaguely known, by using REMS.
The care home patients who participated in this study had not undergone any osteoporosis screening after entering the care home, even for patients who have been prescribed osteoporosis medication. This was thought to be due to the characteristics of care home patients and Japan’s comprehensive healthcare system. The application of REMS in this study was instrumental in assessing patients who would otherwise be challenging to evaluate using DXA, such as those with low physical ability or cognitive impairment. REMS offers a portable, radiation-free alternative with a diagnostic accuracy comparable to that of DXA26,27. Its ability to be used at the bedside without the need for special positioning makes it ideal for care home settings, where patient transfer to a radiological facility is often impractical. Previous studies have demonstrated the utility of the REMS in long-term care facilities, even in patients with severe motor and intellectual disabilities28. Additionally, the potential for REMS to be utilized in primary care, emergency settings, and even patient homes suggests its broader applicability in osteoporosis screening in diverse clinical environments29.
Falls and subsequent fragility fractures are particularly common in nursing facilities and contribute significantly to emergency department visits and hospital admissions30. Nearly one-quarter of patients who sustained hip fractures in nursing facilities died within 90 days due to complications from these fractures31. Despite the high risk of falls and fractures, the rate of osteoporosis treatment in such settings remains alarmingly low. Consistent with previous findings, our study showed that care home residents, although meeting the osteoporosis criteria, were rarely treated for the condition, similar to earlier reports in which only a small fraction of nursing facility residents received appropriate osteoporosis medications32. The high prevalence of severe osteoporosis and lumbar T-scores < − 3.3 SD underscores the urgent need for targeted interventions. On the other hand, although anti-osteoporosis medications have demonstrated efficacy in reducing fracture risk even among the oldest old33,34, their use in frail elderly individuals should be carefully weighed against potential adverse effects, comorbidities, and limited life expectancy. In particular, the time to benefit of certain therapies may exceed the remaining lifespan of some patients, emphasizing the importance of individualized treatment decisions.
On the other hand, this result was likely to be greatly influenced by background factors such as age. We showed lower BMD and T-score and higher prevalence of severe osteoporosis in care home patients, but in age-specific analyses, there was no difference in 80–89 years old patients and 90- years old patients compared to outpatients. This was a result that supported the fact that care home patients were more likely to be elderly. On the contrary, in 70–79 years old patients, care home patients had significantly lower femoral neck and total hip BMD, and many of them met the criteria for severe osteoporosis. In addition, care home patients who met the criteria for severe osteoporosis and lumbar T-scores < − 3.3SD were present in similar numbers in all age groups. This suggests that patients who enter care homes at a relatively young age have a higher risk of bone fragility than those of the same age. While it is true that care home patients tend to be very old, we thought it important to note that even relatively young patients can have the same bone fragility.
However, contrary to expectations, multivariate analysis showed that admission in care homes did not significantly affect severe osteoporosis or lumbar T-score < − 3.3SD. As the factors identified by multivariate analysis were age, female sex and BMI, it was found that the basic background factors of the patients who were admitted to the care homes were the problem, not the fact that they were admitted to the care house itself.
This study has several limitations. First, the differences in osteoporosis treatments used at each facility may be due to the reimbursement system in Japan. Second, it remains unclear whether BMD measured using the REMS accurately reflects conventional osteoporosis criteria, including the WHO criteria for severe osteoporosis. Some studies have reported discrepancies in BMD measurements when compared with DXA21. Therefore, we are skeptical as to whether the results of this study can be directly linked to the risk assessment of fragility fractures, and we believe that further verification is necessary. Third, this study did not assess certain critical factors such as the presence of non-clinical vertebral fractures using spinal X-rays. This limitation was due to the study design. However, the potential impact of this omission should not be overlooked. Fourth, we were unable to examine the effects of differences in the treatments or the length of treatments due to the small number of cases and the nature of cross-sectional studies. Fifth, the care home patients in this study were less likely to have been treated for osteoporosis, and it is possible that they are a slightly different group of patients from care home patients in other countries. Sixth, in some countries, osteoporosis treatments are reimbursed only when BMD is measured by DXA, not by REMS. As such, REMS is currently positioned more as a screening tool rather than a definitive diagnostic modality for treatment decisions. Future research should conduct more detailed analyses to address these limitations and enhance our understanding of the assessment and management of osteoporosis in diverse patient populations.
This study showed REMS has the potential to become a useful osteoporosis screening device for elderly people with limited mobility. We highlighted a substantial gap in osteoporosis treatment among care home residents, despite their high risk of fractures.
Data availability
The dataset of this study is not publicly available. However, on reasonable request, derived data supporting the findings of this study are available from the corresponding author after approval from the Ethical Committee of the Hokkaido University Hospital.
References
Adami, G. et al. Osteoporosis in rheumatic diseases. Int. J. Mol. Sci. https://doi.org/10.3390/ijms20235867 (2019).
Curtis, E. M., Moon, R. J., Harvey, N. C. & Cooper, C. The impact of fragility fracture and approaches to osteoporosis risk assessment worldwide. Bone 104, 29–38. https://doi.org/10.1016/j.bone.2017.01.024 (2017).
Song, S., Guo, Y., Yang, Y. & Fu, D. Advances in pathogenesis and therapeutic strategies for osteoporosis. Pharmacol. Ther. 237, 108168. https://doi.org/10.1016/j.pharmthera.2022.108168 (2022).
Gupta, A. et al. Digital health interventions for osteoporosis and post-fragility fracture care. Ther. Adv. Musculoskelet. Dis. https://doi.org/10.1177/1759720x221083523 (2022).
Keen, R. Osteoporosis: strategies for prevention and management. Best Pract. Res. Clin. Rheumatol. 21, 109–122. https://doi.org/10.1016/j.berh.2006.10.004 (2007).
Huang, C. et al. Prediction of fracture risk by radiographic absorptiometry and quantitative ultrasound: a prospective study. Calcif. Tissue Int. 63, 380–384. https://doi.org/10.1007/s002239900544 (1998).
Miller, P. D. et al. Prediction of fracture risk in postmenopausal white women with peripheral bone densitometry: evidence from the National Osteoporosis Risk Assessment. J. Bone Miner. Res. 17, 2222–2230. https://doi.org/10.1359/jbmr.2002.17.12.2222 (2002).
Carey, J. J., Chih-Hsing, Wu. & P. & Bergin, D.,. Risk assessment tools for osteoporosis and fractures in 2022. Best Pract. Res. Clin. Rheumatol. 36, 101775. https://doi.org/10.1016/j.berh.2022.101775 (2022).
Abrahamsen, B., Osmond, C. & Cooper, C. Life expectancy in patients treated for osteoporosis: observational cohort study using national danish prescription data. J. Bone Miner. Res. 30, 1553–1559. https://doi.org/10.1002/jbmr.2478 (2015).
Cormier, C., Koumakis, E. & Souberbielle, J. C. Choosing the tool for osteoporosis risk prediction. Curr. Opin. Clin. Nutr. Metab. Care 18, 457–464. https://doi.org/10.1097/mco.0000000000000210 (2015).
Shimada, H. et al. Impact of osteosarcopenia on disability and mortality among Japanese older adults. J Cachexia Sarcopenia Muscle 14, 1107–1116. https://doi.org/10.1002/jcsm.13209 (2023).
Juby, A. G. The use of calcaneal ultrasound evaluation of bone mineral density in cognitively impaired seniors. J. Am. Med. Dir. Assoc. 5, 377–381. https://doi.org/10.1097/01.Jam.0000141956.25066.9d (2004).
Ooms, M. E. et al. The incidence of hip fractures in independent and institutionalized elderly people. Osteoporos. Int. 4, 6–10. https://doi.org/10.1007/bf02352254 (1994).
Gregson, C. L. & Compston, J. E. New national osteoporosis guidance-implications for geriatricians. Age Ageing. https://doi.org/10.1093/ageing/afac044 (2022).
McCloskey, E., Tan, A. T. H. & Schini, M. Update on fracture risk assessment in osteoporosis. Curr. Opin. Endocrinol. Diabetes Obes. 31, 141–148. https://doi.org/10.1097/med.0000000000000871 (2024).
Messina, C. et al. DXA beyond bone mineral density and the REMS technique: new insights for current radiologists practice. Radiol. Med. 129, 1224–1240. https://doi.org/10.1007/s11547-024-01843-6 (2024).
Di Paola, M. et al. Radiofrequency echographic multispectrometry compared with dual X-ray absorptiometry for osteoporosis diagnosis on lumbar spine and femoral neck. Osteoporos. Int. 30, 391–402. https://doi.org/10.1007/s00198-018-4686-3 (2019).
Diez-Perez, A. et al. Radiofrequency echographic multi-spectrometry for the in-vivo assessment of bone strength: state of the art-outcomes of an expert consensus meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Aging Clin. Exp. Res. 31, 1375–1389. https://doi.org/10.1007/s40520-019-01294-4 (2019).
Caffarelli, C. et al. Could radiofrequency echographic multispectrometry (REMS) overcome the overestimation in BMD by dual-energy X-ray absorptiometry (DXA) at the lumbar spine?. BMC Musculoskelet. Disord. 23, 469. https://doi.org/10.1186/s12891-022-05430-6 (2022).
Fassio, A. et al. Radiofrequency echographic multi-spectrometry and DXA for the evaluation of bone mineral density in a peritoneal dialysis setting. Aging Clin. Exp. Res. 35, 185–192. https://doi.org/10.1007/s40520-022-02286-7 (2023).
Ishizu, H. et al. Radiofrequency echographic multispectrometry (REMS) can overcome the effects of structural internal artifacts and evaluate bone fragility accurately. Calcif. Tissue Int. 114, 246–254. https://doi.org/10.1007/s00223-023-01167-z (2024).
Cortet, B. et al. Radiofrequency Echographic Multi Spectrometry (REMS) for the diagnosis of osteoporosis in a European multicenter clinical context. Bone 143, 115786. https://doi.org/10.1016/j.bone.2020.115786 (2021).
Amorim, D. M. R., Sakane, E. N., Maeda, S. S. & Lazaretti Castro, M. New technology REMS for bone evaluation compared to DXA in adult women for the osteoporosis diagnosis: a real-life experience. Arch Osteoporos 16, 175. https://doi.org/10.1007/s11657-021-00990-x (2021).
Marcus, R., Wang, O., Satterwhite, J. & Mitlak, B. The skeletal response to teriparatide is largely independent of age, initial bone mineral density, and prevalent vertebral fractures in postmenopausal women with osteoporosis. J. Bone Miner. Res. 18, 18–23. https://doi.org/10.1359/jbmr.2003.18.1.18 (2003).
Shiraki, M. et al. Design of a pragmatic approach to evaluate the effectiveness of concurrent treatment for the prevention of osteoporotic fractures: rationale, aims and organization of a Japanese Osteoporosis Intervention Trial (JOINT) initiated by the Research Group of Adequate Treatment of Osteoporosis (A-TOP). J. Bone Miner. Metab. 29, 37–43. https://doi.org/10.1007/s00774-010-0188-x (2011).
Al Refaie, A. et al. Radiofrequency Echographic Multi Spectrometry (R.E.M.S.): New Frontiers for Ultrasound Use in the Assessment of Bone Status-A Current Picture. Diagnostics (Basel). https://doi.org/10.3390/diagnostics13101666 (2023).
Ciardo, D., Pisani, P., Conversano, F. & Casciaro, S. Pulse-echo measurements of bone tissues. techniques and clinical results at the spine and femur. Adv. Exp. Med. Biol. 1364, 145–162. https://doi.org/10.1007/978-3-030-91979-5_7 (2022).
Sakai, T., Hirao, M., Takashina, Y., Kitagawa, R. & Oishi, T. Radiofrequency echographic multi-spectrometry-based measurement of bone mineral density in patients with severe motor and intellectual disability: An opportunity for patients with severe scoliosis and hip dislocation. Bone Rep 22, 101781. https://doi.org/10.1016/j.bonr.2024.101781 (2024).
Fuggle, N. R. et al. Radiofrequency echographic multi spectrometry (REMS) in the diagnosis and management of osteoporosis: state of the art. Aging Clin. Exp. Res. 36, 135. https://doi.org/10.1007/s40520-024-02784-w (2024).
Unroe, K. T. et al. Long-stay nursing facility resident transfers: Who gets admitted to the hospital?. J. Am. Geriatr. Soc. 68, 2082–2089. https://doi.org/10.1111/jgs.16633 (2020).
Leland, N. E. et al. What happens to patients when they fracture their hip during a skilled nursing facility stay?. J. Am. Med. Dir. Assoc. 16, 767–774. https://doi.org/10.1016/j.jamda.2015.03.026 (2015).
Wright, R. M. Use of osteoporosis medications in older nursing facility residents. J. Am. Med. Dir. Assoc. 8, 453–457. https://doi.org/10.1016/j.jamda.2007.04.002 (2007).
Di Lorenzo, L. Denosumab in elderly osteoporotic patients. A narrative review. Clin. Ter. 174, 545–549. https://doi.org/10.7417/ct.2023.5023 (2023).
Ström, O. et al. Real-world effectiveness of osteoporosis treatment in the oldest old. Osteoporos. Int. 31, 1525–1533. https://doi.org/10.1007/s00198-020-05380-6 (2020).
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Contributions
Conceptualization, T.S.; methodology, H.I.; validation, H.I.; formal analysis, H.I.; investigation, Y.S. and H.I.; resources, H.I.; data curation, H.I.; writing-original draft preparation, H.I.; writing-review and editing, H.I. and T.S.; visualization, H.I.; supervision, T.S., Y.S., M.M., and N.I.; project administration, T.S.; All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments and approved by the Iwamizawa Hokushokai Hospital Institutional Review Board (0023-001).
Informed consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ishizu, H., Shimizu, T., Shimizu, Y. et al. Evaluation of bone fragility in cognitively or physically impaired elderly care home patients using radiofrequency echographic multi-spectrometry. Sci Rep 15, 13373 (2025). https://doi.org/10.1038/s41598-025-97694-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-97694-w