Abstract
Testicular torsion (TT) in children is a common urological emergency, and timely and accurate management is crucial for prognosis. Orchiectomy is one of the severe complications of this condition, and accurately predicting its risk is of great significance for clinical decision-making. This study aims to develop a nomogram to predict risk factors for orchiectomy after TT in children. This study retrospectively collected clinical data from 327 cases of TT at the Children’s Hospital of Fudan University and 141 cases at Anhui Provincial Children’s Hospital, which were classified into the training and validation cohorts, respectively. Multivariate logistic regression analysis was performed to identify independent predictors of orchiectomy in TT patients, and a nomogram was constructed. The model’s effectiveness in both the training and validation cohorts was evaluated using the area under the receiver operating characteristic curve (AUC), calibration curves, and decision curve analysis (DCA). A total of 468 cases were included, of which 230 (49.15%) ultimately underwent orchiectomy. Duration of symptoms, neutrophil count, eosinophil count, degree of torsion, undescended testis(UDT), Testicular Workup for Ischemia and Suspected Torsion(TWIST) score grading, and ultrasound blood flow signal were identified as independent risk factors for orchiectomy in children with TT and were used to construct the nomogram. The AUCs of the nomogram were 0.93 (95% CI: 0.91–0.96) in the training cohort and 0.86 (95% CI: 0.79–0.92) in the validation cohort. The calibration curves demonstrated good agreement between predicted and observed values, and DCA indicated that the constructed nomogram had a high clinical net benefit. The nomogram developed in this study effectively predicts the risk of orchiectomy after TT in children, providing clinicians with a valuable decision-making tool. Future multicenter clinical studies are needed to optimize and validate the model’s effectiveness.
Similar content being viewed by others
Introduction
Testicular torsion (TT) is a common urological emergency in pediatric patients, involving the twisting of the spermatic cord, which leads to impaired blood flow to the testis. If not treated promptly, it can result in ischemic damage1. Therefore, timely and accurate diagnosis is crucial to preserving testicular viability and preventing complications. One of the most severe consequences of TT is orchiectomy, which can have profound physical and psychological effects on both the child and their family. Thus, the ability to predict the risk of orchiectomy is essential for guiding clinical management and ensuring better outcomes.
Several clinical factors have been identified as closely related to testicular survival after torsion, including the duration of symptoms, degree of torsion, and certain hematological parameters1,2. However, accurately predicting the risk of orchiectomy in emergency situations remains a challenge. A reliable and easily interpretable risk assessment tool could provide families with a clearer understanding of the expected surgical outcomes.
Nomograms, which integrate multiple clinical variables into a simplified chart, are widely used in medical research3. By incorporating various risk factors, nomograms offer personalized predictions of clinical outcomes and can serve as practical tools for clinicians. Although nomograms have been extensively applied in the medical field, large-scale, multicenter predictive models specifically for the risk of orchiectomy after TT in children remain limited.
This study aims to develop and validate a nomogram model to predict the risk of orchiectomy in children after TT. By collecting clinical data from two tertiary pediatric medical centers, we will identify independent risk factors associated with orchiectomy and construct a reliable model to assist clinicians in their decision-making process.
Materials and methods
Patient selection and data collection
This retrospective study collected clinical data from 468 children diagnosed with TT between January 2009 and June 2024 at the Children’s Hospital of Fudan University (training cohort) and Anhui Provincial Children’s Hospital (validation cohort). To ensure consistency across study sites, we standardized the definitions of all clinical variables before data collection and strictly adhered to these definitions throughout the study. All included patients were aged <18 years and met the diagnostic criteria for TT. Exclusion criteria were: (1) neonatal TT; (2) acute scrotal emergency without surgical exploration; (3) confirmed torsion of the testicular appendage during surgery; (4) incomplete medical records. This study was approved by the Ethics Committees of Medical Research at Anhui Provincial Children’s Hospital (No. EYLL-2024-014) and Children’s Hospital of Fudan University (No. 2024 − 366), and informed consent was waived by both committees. All procedures involving human participants in this study were conducted in accordance with the ethical standards of the relevant institutional and/or national research committees, and with the 1964 Helsinki Declaration and its subsequent amendments or comparable ethical standards. The study report follows the Strengthening the Reporting of Cohort Studies in Surgery (STROCSS) criteria4.
Demographic data for the included children consisted of age and body mass index (BMI). Clinical data included duration of symptoms, Testicular Workup for Ischemia and Suspected Torsion(TWIST) score5, affected side, season of occurrence, time of occurrence, presence of undescended testis(UDT), ultrasound findings, intraoperative type, degree, and direction of torsion. Hematological parameters recorded within two hours of admission included white blood cell count (WBC), neutrophils, lymphocytes, monocytes, eosinophils, basophils, platelet count, mean platelet volume (MPV), plateletcrit (PCT), platelet distribution width (PDW), and C-reactive protein (CRP).
Surgical management
Upon admission, all children underwent a thorough physical examination, TWIST scoring, ultrasound examination, and hematological tests. If TT was suspected, emergency surgical exploration was performed immediately. During surgery, the child was placed in the supine position, and after adequate anesthesia, the inguinal or scrotal approach was chosen for exploration based on the location of the testis. After detorsion of the twisted testis, warm saline compresses were applied for 20 min to assess its vascularity. The tunica albuginea was then incised to observe the bleeding time from the testicular parenchyma: immediate bleeding was classified as grade I, bleeding within 10 min as grade II, and no bleeding within 10 min as grade III6. For grade I and II cases, orchiopexy was performed and considered as successful salvage, whereas for grade III cases, the necrotic torsed testis was excised. Contralateral orchiopexy was performed in all patients.
Statistical analysis
Statistical analyses were performed using R (version 4.4.0) and SPSS (version 26.0.0). Categorical data were presented as counts (percentages) and analyzed using the chi-square test or Fisher’s exact test. Continuous variables that followed a normal distribution were expressed as mean ± standard deviation, while non-normally distributed variables were presented as median (interquartile range). Parametric tests (t-test) and non-parametric tests (Mann-Whitney U test) were used for the analysis of normally and non-normally distributed continuous variables, respectively. Variables with more than 20% missing data were directly excluded, while the remaining missing values were imputed using the mean or median. Initially, univariate logistic regression was conducted to assess the association between each independent variable and orchiectomy. Significant factors identified in the univariate analysis (P <0.05) were included in a multivariate logistic regression model. The final model was determined using backward selection based on the Akaike Information Criterion (AIC), and the selected factors were used to construct the nomogram. The model’s discrimination ability was evaluated using sensitivity, specificity, accuracy, positive predictive value, and negative predictive value, as well as the receiver operating characteristic (ROC) curve, with the area under the ROC curve (AUC) calculated. A calibration curve was used to assess the model’s calibration, and the results of the Hosmer-Lemeshow test were presented visually. Additionally, decision curve analysis (DCA) was performed to evaluate the net clinical benefit of the model. A value of P <0.05 was considered statistically significant.
Results
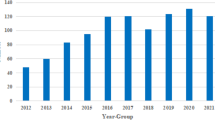
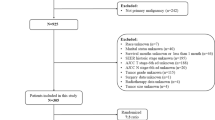
Demographic characteristics
The study flowchart is shown in Fig. 1. A total of 468 cases were included, with 230 cases (49.15%) eventually undergoing orchiectomy. The clinical characteristics of children with TT in the training and validation cohorts are presented in Table 1. There were no statistically significant differences in the variables between the two groups (P > 0.05), indicating good comparability between the groups.
Variable selection
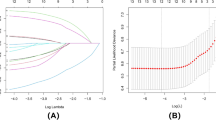
In the training cohort, 24 variables were collected from 327 children. The variable coding was as follows: TWIST score grading (Intermediate risk = 2, High risk = 3), TT of UDT (Yes = 1, No = 2), and blood flow signal (Visible = 1, Invisible = 2). Orchiectomy status was used as the dependent variable, and the statistically significant variables were included in the univariate and multivariate analyses (Table 2). The results showed that duration of symptoms (OR, 1.02; 95% CI: 1.01–1.03; P = 0.001), neutrophil (OR, 0.84; 95% CI: 0.74–0.95; P = 0.005), eosinophil (OR, 27.51; 95% CI: 2.53–298.88; P = 0.006), degree of torsion (OR, 1.01; 95% CI: 1.01–1.01; P <0.001), TT of UDT (OR, 0.12; 95% CI: 0.04–0.43; P = 0.001), TWIST score grading (OR, 3.10; 95% CI: 1.54–6.23; P = 0.002), and blood flow signal (OR, 37.12; 95% CI: 8.82–156.24; P <0.001) were independent risk factors for orchiectomy in children with TT.
Nomogram construction and validation
Based on the results of the multivariate logistic regression analysis, we constructed a nomogram to predict the likelihood of orchiectomy in children with TT (Fig. 2). The nomogram assigns a score to each value of the variables, allowing clinicians to quickly assess risk by vertically matching the total score of all variables to the estimated probability of orchiectomy. The higher the total score, the greater the risk of orchiectomy.
The nomogram demonstrated good predictive performance in both the training and validation cohorts, with AUC values of 0.93 (95% CI: 0.91–0.96) and 0.86 (95% CI: 0.79–0.92), respectively (Fig. 3A, B). The calibration curves showed good agreement between the predicted and actual probabilities, with Hosmer-Lemeshow test P-values of 0.347 and 0.218 for the training and validation cohorts, respectively (Fig. 4A, B). Additionally, DCA was plotted for both the training and validation cohorts to assess the clinical utility of the predictive model. In the DCA curves of the training and validation cohorts, patients achieved higher net benefits when the predicted probability thresholds were between 2% and 97% for the training cohort and between 12% and 98% for the validation cohort, respectively (Fig. 5A, B).
In this study, the optimal cut-off value was determined to be 0.58, based on ROC curve analysis. This cut-off value balances sensitivity and specificity, providing a threshold to classify patients at higher risk of testicular excision after torsion. When the predicted probability exceeds 58%, it indicates a significantly increased risk of testicular loss, suggesting that more aggressive clinical intervention or monitoring may be necessary. The AUC, sensitivity, specificity, accuracy, positive predictive value, negative predictive value, and cut-off values for the training and validation cohorts are listed in Table 3.
Discussion
To our knowledge, this is the first nomogram established to predict the risk of orchiectomy after TT in children through a large-scale multicenter retrospective data analysis. The results showed that the duration of symptoms, levels of neutrophils and eosinophils, degree of torsion, presence of UDT, TWIST score grading, and ultrasound blood flow signal were key factors influencing the risk of orchiectomy. The nomogram constructed based on these findings demonstrated excellent discriminatory ability, with AUC values of 0.93 and 0.86 in the training and validation cohorts, respectively, indicating satisfactory predictive performance. DCA further confirmed that the model provides significant net clinical benefit. Additionally, the indications for orchiectomy after TT were comprehensively assessed by experienced urologists from two tertiary pediatric medical centers, ensuring the accuracy of surgical management. This predictive model not only offers surgeons a valuable tool to assess testicular viability but also facilitates effective communication with parents, helping to clarify treatment expectations and optimize the clinical decision-making process.
The duration of symptoms is one of the important predictive factors in this study. Previous studies have shown that the longer the duration of symptoms, the significantly lower the likelihood of testicular survival7. It is generally believed that surgical intervention within 6 h of symptom onset is crucial for saving the testicle. If the testicle twists within 0–4 h of pain onset, the salvage rate can be as high as 95%. However, if it persists for 8–10 h, the salvage rate drops to 45–60%, and thereafter decreases sharply8. Research by Yi et al.9 indicated that the orchiectomy rate for patients undergoing surgery within 6 h of symptom onset was 5.9%, while it rose to 82.1% within 24 h. Notably, only 23.8% of patients received timely treatment within 6 h of symptom onset, emphasizing the importance of early medical intervention, especially in children and adolescents, as delays in treatment not only affect testicular survival but may also have long-term implications for future fertility1,10. Factors contributing to prolonged symptom duration include being younger than 6 years old, lack of alternative diagnoses, history of previous treatments or symptom progression, distance from major urban areas, and abdominal pain11,12. Additionally, Bayne et al.13 pointed out that delays related to distance from the hospital and transfer time are major factors in the delayed treatment of pediatric TT. Therefore, our model highlights the duration of symptoms as a key indicator for predicting outcomes, indicating that patients with prolonged symptoms should be regarded as high-risk individuals in urgent need of prompt diagnosis and surgical intervention. Future research should continue to explore mechanisms to reduce delays in care, such as through telemedicine or optimizing referral systems, to improve treatment outcomes for these high-risk patients14.
Another significant predictive indicator is the degree of TT. Numerous studies have confirmed that the higher the degree of torsion, the greater the severity of ischemic injury to the testicle, thereby increasing the risk of orchiectomy15,16. Yi et al.9 found through a cross-sectional study that a degree of TT exceeding 180° is one of the risk factors for orchiectomy. Dias et al.17 pointed out that a torsion degree between 360° and 540° is a critical point for significant obstruction of arterial blood flow, posing a risk of testicular damage. However, as the degree of torsion increases, the blood supply to the affected testicle decreases, which also means that the time required to cause damage to the testicular vasculature is significantly reduced18. Therefore, when assessing testicular viability, relying solely on the degree of torsion is insufficient; a comprehensive evaluation must include other factors such as the duration of symptoms19.
Currently, an increasing number of scholars have successfully incorporated hematological parameters into the construction of clinical predictive models19,20,21. In this study, we found that hematological parameters, particularly changes in neutrophils and eosinophils, are also important predictive indicators of the risk of orchiectomy. Although several studies have indicated a certain association between monocytes and the salvage of testicular torsion2,19, He et al.22 further discovered that MPV could serve as a marker for assessing testicular viability. While monocytes showed some correlation in univariate analysis (p = 0.030, OR = 1.99, 95% CI: 1.07 ~ 3.70) in our study, multivariate analysis results indicated that neutrophils (p = 0.005, OR = 0.84, 95% CI: 0.74 ~ 0.95) and eosinophils (p = 0.006, OR = 27.51, 95% CI: 2.53 ~ 298.88) are more effective in predicting the risk of orchiectomy. Additionally, we observed a significant correlation between lower neutrophil levels and increased risk of orchiectomy, in contrast to the eosinophil response. The literature indicates that during ischemia-reperfusion, neutrophils migrate from the bloodstream to tissues, releasing reactive oxygen species that lead to tissue damage23,24. After the detorsion of TT, the massive influx of neutrophils and the reactive oxygen species they release are primary contributors to ischemia-reperfusion injury25. Since our hematological parameters were obtained before surgery and did not include the ischemia-reperfusion process, we hypothesize that in the early stages of TT, blood can still perfuse, leading to higher levels of neutrophils; however, as the duration of torsion increases, blood perfusion gradually ceases, resulting in lower neutrophil levels. Future research could further explore the specifics of this mechanism and its clinical significance to enhance management strategies for patients with TT.
The prevalence of TT in UDT ranges from 5.9 to 10.2% of all TT cases16,26,27. In our study, UDT cases accounted for 11.3% (53/468) of all TT cases, slightly higher than previously reported. The testicular salvage rate for UDT is generally lower; Zvizdic et al.16 reported a salvage rate of 35% in their series, which is similar to the 36.4% reported by Zhong et al.28. However, in our study, the testicular salvage rate for UDT was only 30.2% (16/53), significantly lower than the rate for normally descended testicles (53.5%, 222/415). Zilberman et al.29 also found that the surgical salvage rate for cryptorchid torsion patients was only 10%, far lower than the salvage rate for normally descended testicles (56%). The low salvage rate for UDT may be due to atypical symptoms, misdiagnosis as other diseases (such as gastrointestinal disorders), and delayed presentation16,28,30.
Another significant predictive factor for orchiectomy is the absence of blood flow signals on Doppler ultrasonography (DUS). The use of preoperative Doppler ultrasound is controversial, as the results are highly operator-dependent and may delay surgical exploration31. Pinar et al.31 evaluated 2,922 cases of TT and found that 32.7% of patients underwent DUS prior to surgery, with a sensitivity of 85.2% and a specificity of 52.7%. They concluded that, in early torsion or partial/intermittent torsion, DUS may misleadingly show arterial blood flow, and continuous blood flow does not necessarily exclude the possibility of TT. It must be compared with the contralateral side32. In late-stage torsion, if DUS shows the absence of blood flow, it indicates prolonged testicular ischemia, further decreasing the possibility of salvage and increasing the risk of orchiectomy9.
Another important predictor is the TWIST score. This 7-point scoring system is specifically used for the preoperative evaluation of scrotal emergencies and includes the following parameters: testicular swelling (2 points), hard testicle (2 points), absent cremasteric reflex (1 point), nausea/vomiting (1 point), and high riding testis (1 point). The cutoff for low-risk and high-risk categories is 2 and 5 points, respectively5. Although several studies have demonstrated the decision-making value of the TWIST score in evaluating acute scrotal symptoms5,33,34, few have applied this scoring system to the decision for orchiectomy in TT. In our study, all patients were assessed as being in the intermediate-to-high-risk range, and the results showed that the TWIST score was significantly associated with the risk of orchiectomy. A high TWIST score typically indicates a longer symptom duration and more pronounced clinical manifestations35, suggesting that the testicle may already be in an ischemic state, thus reducing the possibility of salvage. It is worth noting that, although the TWIST score was confirmed as an independent risk factor in this study, its accuracy still depends on the clinical experience and judgment of healthcare professionals34.
Although this study provides valuable insights into predicting the risk of orchiectomy after TT in children, there are several limitations. First, as a retrospective cohort study, the results may be influenced by selection bias and incomplete data, especially given potential variations in the standardization of data collection across different medical institutions. Second, the data collection spanned a long period (2009–2024), during which diagnostic and surgical techniques may have evolved. These technological advancements could introduce heterogeneity into the data, potentially affecting the results and generalizability of the model. Finally, although this study explored the salvage rate for torsion in UDT, the small number of UDT cases (only 53) may limit the generalizability of these findings. Additionally, while we identified some independent predictors, we did not thoroughly investigate factors contributing to delayed diagnosis and treatment, such as family economic status, health insurance policies, and the educational level of guardians, which could provide more information for optimizing the model. Therefore, despite the multicenter validation, large-scale prospective studies are still needed in the future to further validate and refine the predictive model.
Conclusion
This study successfully developed a nomogram model to predict the risk of orchiectomy after TT in children and identified several independent risk factors, including duration of symptoms, degree of torsion, hematological parameters, and UDT. The model demonstrated good predictive performance in both the training and validation cohorts, providing a robust decision-support tool for clinicians managing cases of TT. However, larger-scale multicenter prospective studies are needed in the future to further validate the model’s reliability and applicability, ultimately optimizing the management strategies for pediatric TT.
Data availability
The dataset for this study is held and managed by the authors. Due to privacy and ethical restrictions, the data are not publicly available. Any requests for further information about the dataset and queries concerning data-sharing arrangements may be directed to Jian Shen and Yongsheng Cao, who is presumably the corresponding author of the original study.
References
Jacobsen, F. M. et al. The impact of testicular torsion on testicular function. World J. Mens Health. 38(3), 298–307 (2019).
Chen, P. et al. Predictive value of hematological parameters in testicular salvage: A 12-year retrospective review. Front. Pediatr. 10, 989112 (2022).
Jiang, H. et al. Multimodal imaging-based prediction of recurrence for unresectable HCC after downstage and resection-cohort study. Int. J. Surg. 110(9), 5672–5684 (2024).
Rashid, R. et al. The STROCSS 2024 guideline: strengthening the reporting of cohort, cross-sectional, and case-control studies in surgery. INT. J. SURG. 110(6), 3151–3165 (2024).
Barbosa, J. A. et al. Development and initial validation of a scoring system to diagnose testicular torsion in children. J. Urol. 189(5), 1859–1864 (2012).
Arda, I. S. & Ozyaylali, I. Testicular tissue bleeding as an indicator of gonadal salvageability in testicular torsion surgery. BJU Int. 87(1), 89–92 (2001).
Beher, A. et al. A survey of preoperative, perioperative, and postoperative management practices for testicular torsion in pediatric patients among European surgeons. Eur. J. Pediatr. Surg.(2024).
Jefferies, M. T. et al. The management of acute testicular pain in children and adolescents. BMJ 350, h1563 (2015).
Yi, H. et al. Analysis of factors associated with delayed diagnosis and treatment of testicular torsion in 1005 cases from Chongqing City, China: a cross-sectional study. Sci. Rep. 13(1), 22765 (2023).
Anderson, M. J. et al. Semen quality and endocrine parameters after acute testicular torsion. J. Urol. 147(6), 1545–1550 (1992).
Yu, C. et al. Demographic, clinical, and socioeconomic factors associated with delayed diagnosis and management of pediatric testicular torsion in West China: a retrospective study of 301 cases in a single tertiary children’s hospital. BMC Pediatr. 21(1), 553 (2021).
Vasconcelos-Castro, S. & Soares-Oliveira, M. Abdominal pain in teenagers: beware of testicular torsion. J. Pediatr. Surg. 55(9), 1933–1935 (2019).
Bayne, A. P. et al. Factors associated with delayed treatment of acute testicular torsion-do demographics or interhospital transfer matter? J. Urol. 184(4 Suppl), 1743–1747 (2010).
Patel, V., Marescaux, J. & Covas Moschovas, M. The humanitarian impact of telesurgery and remote surgery in global medicine. Eur. Urol. 86(2), 88–89 (2024).
Feng, S. et al. Clinical characteristics of testicular torsion and identification of predictors of testicular salvage in children: A retrospective study in a single institution. Urol. Int. 104(11–12), 878–883 (2020).
Zvizdic, Z. et al. Clinical characteristics and outcome of children with acute Cryptorchid testicular torsion: A single-center, retrospective case series study. Am. J. Emerg. Med. 82, 4–7 (2024).
Dias, A. C. et al. The amount of spermatic cord rotation magnifies the timerelated orchidectomy risk in intravaginal testicular torsion. Int. Braz J. Urol. 42(6), 1210–1219 (2016).
Castañeda-Sánchez, I. et al. Testicular torsion: A retrospective investigation of predictors of surgical outcomes and of remaining controversies. J. Pediatr. Urol. 13(5), 516e1–516e4 (2017).
Chen, P. et al. A nomogram for predicting risk factors of testicular salvage after testicular torsion in children. Int. J. Urol. 31(5), 568–574 (2024).
Li, S. et al. Development and validation of a nomogram for pneumonia risk in burn patients with inhalation injury: a multicenter retrospective cohort study. Int. J. Surg. 110(5), 2902–2909 (2024).
Sun, R. et al. Development of interpretable machine learning models for prediction of acute kidney injury after noncardiac surgery: a retrospective cohort study. Int. J. Surg. 110(5), 2950–2962 (2024).
He, M., Zhang, W. & Sun, N. Can haematologic parameters be used to predict testicular viability in testicular torsion? Andrologia 51 (2019).
Lysiak, J. J. et al. Essential role of neutrophils in germ cell-specific apoptosis following ischemia/reperfusion injury of the mouse testis. Biol. Reprod. 65(3), 718–725 (2001).
Arena, S. et al. Medical perspective in testicular ischemia-reperfusion injury. Exp. Ther. Med. 13(5), 2115–2122 (2017).
Wei, S. M., Huang, Y. M. & Zhou, J. Probucol reduces testicular torsion/detorsion-induced ischemia/reperfusion injury in rats. Oxid. Med. Cell Longev. 2017, 5424097 (2017).
Şener, N. C. et al. A rare emergency: testicular torsion in the inguinal canal. Biomed. Res. Int. 2015, 320780 (2015).
Chen, P. et al. Diagnosis and treatment of Cryptorchid testicular torsion in children: A 12-year retrospective study. Front. Pediatr. 10, 968997 (2022).
Zhong, H. J., Tang, L. F. & Bi, Y. L. Cryptorchid testicular torsion in children: characteristics and treatment outcomes. Asian J. Androl. 23(5), 468–471 (2021).
Zilberman, D. et al. Torsion of the Cryptorchid testis–can it be salvaged? J. Urol. 175(6), 2287–2289 (2006).
Yang, M. et al. Diagnosis, treatment, outcome, and reasons for delayed treatment of cryptorchidism with torsion in children: a 16-year retrospective study in a large pediatric medical center. Asian J. Androl. 24(4), 386–389 (2022).
Pinar, U. et al. The use of doppler ultrasound for suspected testicular torsion: lessons learned from a 15-year multicentre retrospective study of 2922 patients. Eur. Urol. 79, S1614 (2021).
Gnech, M. et al. European association of urology/european society for paediatric urology guidelines on paediatric urology: summary of the 2024 updates. Eur. Urol. (2024).
Qin, K. R. & Qu, L. G. Diagnosing with a TWIST: systematic review and Meta-Analysis of a testicular torsion risk score. J. Urol. 208(1), 62–70 (2022).
Sheth, K. R. et al. Diagnosing testicular torsion before urological consultation and imaging: validation of the TWIST score. J. Urol. 195(6), 1870–1876 (2016).
Barbosa, J. A. B. A. et al. Validation of the TWIST score for testicular torsion in adults. Int. Urol. Nephrol. 53(1), 7–11 (2020).
Funding
This study was supported by the Anhui Provincial Health Research Program (AHWJ2024Aa20225).
Author information
Authors and Affiliations
Contributions
C.M.:conceptualization, data curation,, formal analysis, investigation, visualization, writing—original draft; C.Y.: data curation, investigation; H.Z.: investigation, visualization; Q. D.: investigation. T.Z.: visualization. H.C.:writing—original draft. J.S.:writing—review and editing. Y.C.:conceptualization, supervision, writing—review and editing. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Ethics Committees of Medical Research at Anhui Provincial Children’s Hospital (No. EYLL-2024-014) and Children’s Hospital of Fudan University (No. 2024 − 366).
Informed consent
This study is a retrospective cohort study. Informed consent was waived by our ethics committee because of the retrospective nature of our study, and which will not have adverse effects on the health and rights of patients.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mao, C., Yang, C., Zhong, H. et al. Development of a nomogram to predict risk factors for orchiectomy after testicular torsion in children. Sci Rep 15, 15154 (2025). https://doi.org/10.1038/s41598-025-97911-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-97911-6