Abstract
Cardiovascular disease (CVD) are the leading cause of death globally and often go undetected. Modifiable risk factors for CVD include diet and physical activity. This study aimed to evaluate the health status of Polish patients without a prior diagnosis of CVD, diabetes, or chronic kidney disease (CKD), focusing on healthy dietary choices, dietary harm avoidance, daily routine, organized physical exercise, and social and mental balance (HLPCQ). The multicenter study involved patients without previous CVD, CKD, or diabetes, analyzing anthropometric measurements, blood pressure, heart rate, and laboratory test results. Participants also completed the HLPCQ questionnaire. The study included 836 patients, with a mean age of 48 ± 9.3 years. On the SCORE2 risk analysis, 173 (20.6%) met the criteria for very high risk. The average HLPCQ score was 65.6 ± 26.0. Regression analysis revealed that higher scores on the healthy food choices subscale correlated with lower serum non-HDL cholesterol levels (B = −0.009, SE = 0.003, t = −3.196, p = 0.001) and higher HDL cholesterol levels (B = 0.027, SE = 0.008, t = 3.529, p < 0.001). Similar correlations were observed with the Organized Exercise subscale. The study concluded that lifestyle choices significantly impact biochemical parameters, including blood lipid panels, highlighting the importance of educating both patients and medical professionals on the health impacts of lifestyle.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) remains the leading cause of death worldwide, including Poland1. According to Global burden of cardiovascular disease and risks report global death counts due to CVD increased from 12.4 million in 1990 to 19.8 million in 2022 which reflects global population growth and aging as well as the contributions from preventable risk factors2. Early diagnosis and identification of modifiable risk factors and their development is key to reducing mortality, also from complications3. The World Health Organization (WHO) indicates that the national mortality rate from CVD in Poland is 223.8 per 100,000 person-years, which according to the 2021 ESC guidelines qualifies Poland as a high cardiovascular risk country4,5,6. Additionally, the years 2020–2022 mark a period of increasing health debt, to which the COVID-19 pandemic has undeniably contributed7. This increase should not be attributed solely to the effects of the disease itself, but also to the impact of the pandemic on worsening access to diagnostics and treatment of chronic diseases. Moreover, it is known that social isolation and loneliness have long been identified as risk factors for worse physical and mental health and increased mortality8. In the first year of the pandemic, the level of mortality due to CVD in Poland increased by 8.8% compared to expected, and by 12.6% in the following year7. According to data from the Central Statistical Office (GUS) of 2022, in 2020, there was the largest decline in expected life expectancy since post-war times (by 1.46 years for men and 1.04 for women). This is also the largest drop in expected life expectancy among European countries. The increase in the number of deaths among young men is also concerning information9.
There is currently the possibility of diagnostics towards cardiovascular diseases and detecting risk factors for their development as part of two preventive programs in Poland: the cardiovascular disease prevention program (CHUK) dedicated to people aged 35–65 years (without previously diagnosed cardiovascular diseases, diabetes, chronic kidney disease, and familial hypercholesterolemia) and the “Prevention 40 Plus” program—for all people from the age of 4010,11. Despite inconsistent data regarding the impact of screening tests on reducing mortality and morbidity from cardiovascular diseases, they seem to have an impact on the identification of risk factors for these diseases and are an essential element in combating health inequalities worldwide12,13,14,15,16. Screening programs in Poland, in addition to assessing physical activity, smoking, alcohol consumption and diet do not take into account other important components of lifestyle such as: daily routine, psychosocial conditions, or mental health.
According to the 2020 Global Burden Of Disease report, high blood pressure, tobacco use, and improper diet were the leading factors contributing to the global disease burden. Unfavorable dietary patterns were associated with 22% of all deaths in 2017, and CVD was the main cause of deaths related to diet1,3. What is more, Global burden of cardiovascular diseases and risks report points high systolic blood pressure, dietary risks and air pollution as main contributing factors to change in attributable age-standardized CVD disability-adjusted life years (DALYs)2. In the 2023 update of the report “Heart Disease and Stroke Statistics” published by the American heart association (AHA), about 2 million major cardiovascular incidents in the USA can be prevented through lifestyle changes focused on cardiovascular health17. Although improper diet might be one of the main and modifiable risk factors for CVD, epidemiological studies conducted in many countries have shown that the number of people with overweight and obesity is increasing year by year18.
Considering the significant impact of lifestyle on the development and course of CVD, it is important to raise public awareness, including medical professionals, about the need to identify individuals at risk and empower them to change their behavior. To obtain a significant impact on reducing cardiovascular risk, these actions must be conducted at the population level, with the implementation of systemic solutions19,20.
Despite creating the public health debt, the pandemic has also brought new platforms for interacting with patients, creating a unique opportunity to reorganize the approach to the prevention of cardiovascular diseases.
Consequently, the aim of this study was to assess the health status of Polish Patients without previous diagnosis of CVD or diabetes or chronic kidney disease. And in particular, the assessment of Healthy Dietary Choices, Dietary Harm Avoidance, Daily Routine, Organized Physical Exercise and Social and Mental Balance (HLPCQ) with use of a dedicated questionnaire and their impact on the CVD risk factors.
Material and methods
Our study was designed as a multicentered, retrospective cross-sectional study. We included patients aged at least 40 years without prior diagnosis of CVD, diabetes and chronic kidney disease. We performed an analysis of medical data such as laboratory results, anthropometric measurements and healthy lifestyle and personal control questionnaire (HLPCQ) questionnaires filled by patients. The data was collected between September 2022 and May 2023. The inclusion criteria were as follows:
-
Written consent to participate in the study.
-
Age ≥ 40 y.o.
-
Lack of CVD, diabetes and chronic kidney disease when entering the study.
-
Performed laboratory tests within 4 weeks before or after entering the study: blood lipids panel (serum total cholesterol, HDL, LDL, non-HDL, triglycerides) and serum fasting glucose level
Omitting at least 1 of those criteria resulted in exclusion from the study. There were 10 primary care facilities involved in the recruitment process and the data collection. The four of them were located in rural areas and six of them in the cities.
The analyzed data was: age, sex, dwelling place, educational status and professional activity. The information about family history (mother and father) of myocardial infarction and stroke, including the age of disease presentation was collected. Participants were also asked about smoking habits and a level of physical activity. The anthropometric measurements were performed (height and weight with BMI calculation, waist circumference) as well as heart rate and blood pressure.
The next step was the analysis of laboratory results as mentioned in inclusion criteria: blood lipids panel (serum total cholesterol, HDL, LDL, non-HDL, triglycerides) and serum fasting glucose level.
The participants were asked to fill the HLPCQ questionnaire. The HLPCQ was designed as a 26 question tool to assess the frequency of some lifestyle habits. The stratification was based on Likert 4 degree scale: 1- never or rarely, 2- sometimes; 3- often; 4- always. From 26 questions—12 address dietary choices and habits and 2 evaluate the level of physical activity. There are 4 questions which assess social factors and mental balance and 8 questions in the area of daily routine and time management. The evaluation of the questionnaire is based on total score. The higher number of points correlates with a healthier lifestyle. The maximum score is 104. In addition to the total score analysis, there is possibility to evaluate the scores in 5 subscales:
-
1)
Healthy dietary choices – questions – 1,3,4,5,13,14,16 – maximum score – 28
-
2)
Dietary harm avoidance – questions – 8,9,10,11 – maximum score – 16
-
3)
Daily routine – questions – 2,6,7,12,15,17,19,22 – maximum score – 32
-
4)
Organized physical exercise – questions – 20,23 – maximum score – 8
-
5)
Social and mental balance – questions – 18, 21,24, ok 25,26 – maximum score – 20
The HLPCQ was originally created in Greece. It was translated and validated for the Polish population in 2021, similar to the original tool psychometric quality21,22.
Data analysis
Based on obtained medical data (age, sex/gender, current smoking), results of laboratory tests (serum non-HDL level) and level of systolic blood pressure, risk of cardiovascular events was estimated (using SCORE2 tool). Three groups of different levels of cardiovascular events risk were created accordingly to the ESC guidelines from 2021:
-
1)
Low to medium risk of cardiovascular events:
-
a.
SCORE2 < 2.5% for population < 50 y.o.
-
b.
SCORE2 < 5% for population between 50–69 y.o.
-
c.
SCORE2 < 7.5% for population ≥ 70 y.o.
-
a.
-
2)
High risk of cardiovascular events:
-
d.
SCORE2 2.5%—< 7.5% for population < 50 y.o.
-
e.
SCORE2 5%—< 10% for population 50–69 y.o.
-
f.
SCORE2 7.5%—< 15% for population ≥ 70 y.o.
-
d.
-
3)
Very high risk of cardiovascular events:
-
g.
SCORE2 ≥ 7.5% for population < 50 y.o
-
h.
SCORE2 ≥ 10% for population 50–69 y.o
-
i.
SCORE2 ≥ 15%for population ≥ 70 y.o
-
g.
The analysis of the results of laboratory (serum) test were performed, once again based on cut off points indicated in ESC 2021 guidelines:
-
1)
Fasting glucose: ≥ 100 mg/dl
-
2)
Triglycerides: ≥ 150 mg/dl
-
3)
Total cholesterol: ≥ 190 mg/dl
-
4)
HDL cholesterol:
-
1.
≥ 40 HDL cholesterol for females
-
2.
≥ 45 HDL cholesterol for males
-
1.
-
5)
LDL cholesterol :
-
1.
< 100 mg/dl for patients with low to medium risk of CV events
-
2.
< 70 mg/dl for patients with high risk of CV events
-
3.
< 55 mg/dl for patients with very high risk of CV events
-
1.
-
6)
non-HDL cholesterol:
-
1.
< 130 mg/dl for patients with low to medium risk of CV events
-
2.
< 100 mg/dl for patients with high risk of CV events
-
3.
< 85 mg/dl for patients with very high risk of CV events
-
1.
-
7)
Systolic blood pressure ≥ 140 mmHg
-
8)
Diastolic blood pressure \(\ge\) 90 mmHg
-
9)
Heart rate ≥ 100 bpm23.
This study was conducted in accordance with the Declaration of Helsinki and the approval of the Bioethics Committee of Wroclaw Medical University was obtained.
Statistical analysis
The variables analyzed are qualitative and quantitative. Normality of distribution was assessed using the Shapiro-Wilks test. Comparison of qualitative variables was performed using the chi-square test. For quantitative variables, non-parametric Mann–Whitney U or Kruskal Wallis tests were used. To assess the impact of lifestyle on individual laboratory results, univariate linear regression analysis was first performed. The dependent variable was the laboratory test score, and the independent variables included subscale scores and the HLPCQ final score. Subsequently, compound linear regression models were built, where the dependent variable was the laboratory test score, while the independent variables included the patient’s age in addition to the subscale scores and HLPCQ final score.
Statistical significance was assumed at the level of < 0.05.
The analysis was conducted using Statistica 13.0 (TIBCO Software, Palo Alto, CA, USA).
Results
Characteristic of the studied group
A total of 836 patients were enrolled in the study after meeting the inclusion criteria. Each of them underwent risk assessment of CV events based on the SCORE2 tool. Median of age was 48 ± 9.3 y.o. The predominance of female gender (64.4%), urban dwelling place and white-collar workers (41.2%) was observed. 25.0% of participants were current smokers and 15.7% of the studied group declared smoking in the past.
In SCORE2 analysis 381 (45.5%) participants were classified as a low to medium risk group and 173 (20.6%) had met the criteria of a very high risk group of CV events.
Prevalence of high and very high CV events risk was significantly higher among participants with lower educational status (p < 0.001).
Detailed description of the studied population with the division to SCORE2 risk groups is presented in (Table 1). In the analysis of the results of our study, we managed to establish mean levels of serum total cholesterol at 204 mg/dl, which in 62.6% of cases was above the upper limit of normal. Moreover more than a half of the studied group presented with serum non-HDL (50.1%) and LDL (66.1%) cholesterol levels above recommended. 22.1% of participants presented with levels of serum fasting glucose above the upper limit of normal. In comparison of groups divided by SCORE2 CVD risk assessment, correlation between increased SCORE2 risk and increased median levels of serum total cholesterol, non-HDL and LDL cholesterol was found. What is more, in each CVD risk group almost 1 at 4 patients had abnormal levels of serum fasting glucose. In the very high SCORE2 risk group the mean level of serum fasting glucose was at 102 mg/dl. The detailed comparison of analyzed data is presented in (Table 2).
The participants of the study presented with mean 65.6 ± 26.0 points at the HLPCQ. In each subscale the mean points were as follows: 16.9 ± 3.8 in healthy dietary choices subscale, 11.0 ± 2.8 in dietary harm avoidance subscale, 20.7 ± 5.4 in daily routine assessment, 4.1 ± 1.8 in physical exercise subscale and 12.8 ± 3.00 in social and mental balance assessment. In analysis of particular questions our attention was drawn by the high prevalence of healthy dietary habits among participants. 78,8% respondents read the food labels before purchasing products, 85.8% stuck to fixed time of consuming meals during the day and only 14.2% did not avoid fats in their diet. What is more, 1 of 3 participants always avoided sweetened beverages and 32.9% of patients declared that they always avoid fast-foods. It’s worth mentioning that 79.5% of the respondents made an effort not to omit any meal during the day. In the physical activity subcategory, only 6,7% of respondents had a planned exercise routine. Over 90% of participants declared the ability to maintain work-life balance. The detailed comparison of analyzed data is presented in Table S1 (in the supplementary).
In the analysis of sociodemographic impact on the HLPCQ results we managed to establish the correlation between female gender and higher scores at the total count as well as in each subscale. The urban citizens presented with higher scores in HLPCQ than those from rural areas. Surprisingly, neither early stroke or myocardial infarction in the family history (mother or father) had an impact on healthy lifestyle habits of participants.
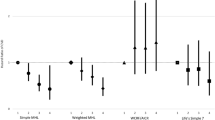
The detailed comparison of the influence of sociodemographic factors on HLPCQ results and its subscales is presented in (Table 3). The regression analysis demonstrated that higher scores in the Healthy Dietary Choices subscale of HLPCQ were correlated with lower levels of serum non-HDL cholesterol (B = -0.009, SE = 0.003, t = -3.196, p = 0.001) and higher levels of serum HDL cholesterol levels (B = 0.027, SE = 0.008, t = 3.529, p < 0.001). Similar correlation was observed in the Organized Physical Exercise subscale.
There was no correlation with the total score of the HLPCQ scale and mean levels of serum total cholesterol. Nonetheless, the regression analysis indicates that higher total score of the HLCPQ scale was associated with higher levels of serum HDL cholesterol (B = 0.070, SE = 0.026, t = 2.747, p = 0.006), lower levels of serum non-HDL cholesterol (B = −0.024, SE = 0.009, t = −2.464, p = 0.006) and lower levels of serum LDL cholesterol (B = −0.024, SE = 0.009, t = −2.243, p = 0.025). The linear regression analysis did not show statistical significance for correlation between subscales scores or total score of HLPCQ scale and serum fasting glucose levels.
In a comparison of participants based on the SCORE-2 risk scale, patients in the very high CVD risk group had the worst results (p = 0.005). Moreover, the patients from this group had also the worst results in the subscales which assess healthy dietary choices and physical activity. The detailed analysis presented in (Table 4).
In the multifactorial analysis with age of the patient taken into the account, the positive correlation between Healthy dietary choices, Dietary harm avoidance, Organized physical exercise, total HLPCQ score and favorable lipid profile (higher HDL cholesterol and lower non-HDL cholesterol serum levels) was found. The detailed comparison of the results of multifactorial linear regression analysis is presented in (Table 5).
Discussion
Prevalence of modifiable risk factors is high in the general population1,3,24. They account for more than half of cardiovascular disease events and cardiovascular mortality24,25,26. According to the results from framingham heart study and third national health and nutrition examination survey [NHANES III] more than 90% of coronary heart disease will occur in individuals with at least 1 elevated risk factor. The other alarming issue is that CVD risk factors are also highly prevalent in the younger population27,28. In contrast to the declining incidence of CVD in adults aged > 50 years, the incidence of CVD has either been steady or has increased for the younger population28,29. In the comparison of National Health and Nutrition Examination Survey data for population aged 20 to 44 years from two periods: 2009–2010 to 2017–2017, increase in prevalence of diabetes (from 3.0 to 4.1%), obesity (form 32.7 to 40.9%) was observed30.
Moreover, it is important to remember that the more various risk factors appear at a younger age, the more the risk of developing chronic conditions in the future increases. Identifying those risk factors in the younger population and addressing them, may lead to decline in morbidity and mortality27. The assessment should encompass both traditional cardiovascular disease (CVD) risk factors and lifestyle-related risks28. In comparison to lifestyle factors between young and middle-aged population, younger patients in our study were less likely to consume fruits and vegetables, have higher levels of psychological stress and low functional capacity31. The different CVD risk factors may be more attributable to the presence of CVD in the younger population31,32. Thus, prevention programs may be key to improve early detection of modifiable CVD risk factors29,33.
CVD risk factors evaluation is also crucial in estimating the risk of cardiovascular events and managing therapy of dyslipidemia, hypertension, obesity and diabetes. Based on some established risk factors of CVD the assessment tools were designed: Framingham risk score (FRS), systematic coronary risk evaluation (SCORE)23,34,35. American college of cardiology/American heart association (ACC/AHA) Atherosclerotic Cardiovascular Disease Risk Estimator, Reynolds risk score and United Kingdom score QRISK36,37,38. The purpose of those tools is to help clinicians implement some interventions to reduce the cardiovascular events risk39. All CVD risk assessment models are subject to limitations. They do not describe a person’s long-term CVD risk which may underestimate this risk in younger populations (as age has the highest impact on risk level in aforementioned calculators)40. Those models have been shown beneficial in identifying high-risk individuals, but they underestimate low risk groups which may present with marginal, but multiple risk factors39,40. Another limitation is that changes in populations due to migrations may influence accuracy of assessment tools which were validated on different cohorts41. What is more, they do not take into account some factors that are more challenging to measure, such as dietary habits (both the positive and the potentially harmful), level of physical activity or mental status and socioeconomic status42. Subjectivity of those parameters may raise some questions about their clinical importance.
A study by Czapla et al., published in 2021, evaluated the psychometric properties and cultural adaptation of the Polish version of the HLPCQ on a sample of 2433 participants. It was confirmed that the reliability and validity of the five dimensions are acceptable, which made it useful for clinical and research use in Poland21. However, to our knowledge this is the first Polish study using this tool in practice after the evaluation. The HLPCQ was originally developed in Greece and published in 2014. It was created from the need to address the assessment of lifestyle interventions that take into account not only physical activity and nutrition, but also mental well-being and social support. Thus, the authors intended that this questionnaire would measure the lifestyle pattern of individuals who have increased control over their health, indicating their degree of empowerment. However they encouraged the readers to use it also to address health-related daily activities. A Greek report from 2020 assessed Pythagorean Self-Awareness Intervention (PSAI) and its effect on daily habits with use of HLPCQ together with the perception of stress, depression, positive or negative emotions, and sense of coherence measured by other tools. It was found that PSAI had beneficial effects on healthy lifestyle and personal control choices, indicating that the influence of lifestyle intervention (in this example—a stress management technique) could be measured by HLPCQ.
We hypothesized that Healthy Dietary Choices, Dietary Harm Avoidance, Daily Routine, Organized Physical Exercise and Social and Mental Balance measured by HLPCQ are associated with CVD risk factors and may provide more insight in risk stratification. As a result of our research, we have indeed found, for instance, an association between Healthy Dietary Choices and SBP as well as DBP and an association between this domain, Dietary Harm Avoidance, Organized Physical Exercise and non-HDL as well as HDL cholesterol levels. Moreover, Organized Physical Exercise was significantly associated with TG levels. Social and Mental Balance was significantly associated with HR. We have also managed to establish correlation between high and very high CVD-risk in SCORE2 and the level of patient’s education. The educational status may influence a person’s individual CVD risk on many levels. Starting from dietary choices, smoking habits, attitude to physical exercise, daily routine and the working environment. The lower level of education can be linked to lower economic status which can affect dietary choices, medical care availability and adherence to the pharmacological and nonpharmacological interventions43,44.
Studies evaluating lifestyle choices in relation to biochemical and metabolic parameters are scarce. There are however some studies on the Polish population that might shed some light into the topic. Mierzecki et al. evaluated 124 young adult individuals with family history of premature ischemic stroke (fathers younger than 55 years, mothers younger than 65 years). They found that mean blood cholesterol levels, including LDL cholesterol, were above the recommended value in the studied group and observed a significant decrease of this parameter after folic acid supplementation. Therefore, it was demonstrated that improvement in the quality of diet composition resulted in a beneficial outcome in terms of blood lipids panel. What’s interesting is that the biggest change in LDL cholesterol was observed in overweight males45,46. A more recent study on the Polish population was an evaluation of the effect of lifestyle choices on biochemical parameters in schizophrenia patients by Kalinowska et al. They found significant correlations of the amount of consumed sweets and sugar with total cholesterol and LDL cholesterol (positive linkage) levels and HDL cholesterol (negative linkage) levels. What’s interesting is that, identically as in our study, the level of physical activity was significantly negatively correlated with TG mean concentration. A very important, practical conclusion from the research of these authors was that simply collecting a nutritional history resulted in a change of behavior regarding dietary choices and subsequent improvement in biochemical parameters47.
The aforementioned studies were conducted before the outbreak of COVID-19 pandemic. Available reports, especially the ‘Health Status of Polish Population and Its Determinants’, 2022, edited by Bogdan Wojtyniak and Paweł Goryński published by National Institute of Public Health (NIH)—National Research Institute stated that in 2021, life expectancy for men was 2.3 years shorter than in the pre-pandemic year 2019 (71.75 years) and life expectancy for women 2.1 years shorter (79.68 years)7. A significant excess mortality from diabetes, CVD and causes directly related to alcohol consumption was noted. Deterioration of cardiovascular care, both inpatient and outpatient, was observed in the first year of the COVID-19 pandemic. At the same time consumption of fats, especially butter, and in addition sugar and confectionery increased affecting the calories intake and resulting in an increase of the proportion of overweight men by almost 3 p.p. and women by 0.5 p.p. Thus, the prevalence of obesity among men increased by 3 p.p., while among women it remained virtually unchanged7. The data described show the health debt that has accumulated in the Polish population as a result of the COVID-19 pandemic. This is a public health challenge that needs to be addressed in the near future. The use of tools such as HLPCQ may allow not only to assess the effectiveness of lifestyle interventions implemented to improve population health, but also to even better stratify individuals according to cardiovascular risk.
The authors are aware of the limitations of this study, which is undoubtedly the lack of representativeness of the analyzed group for the Polish population, resulting from setting this study in primary care and people aged 40–65. It is therefore necessary to carry out research on a larger group of people.
Conclusions
Lifestyle choices have a significant impact on biochemical parameters including blood lipids panel. As lifestyle is also a modifiable risk factor for cardiovascular disease and both patients and medical professionals should be actively educated about its impact on health. HLPCQ is a useful tool in providing additional information facilitating CVD risk assessment.
Data availability
The data will be available upon contacting the corresponding author.
References
Abbafati, C. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396, 1204–1222 (2020).
Global Burden of Cardiovascular Diseases and Risks Collaboration. 1990–2021. J. Am. Coll. Cardiol. 80, 2372–2425 (2022).
Abbafati, C. et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396, 1223–1249 (2020).
Mortality and global health estimates. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates.
SCORE2-OP Working Group and ESC Cardiovascular Risk Collaboration. SCORE2-OP risk prediction algorithms: estimating incident cardiovascular event risk in older persons in four geographical risk regions. Eur. Heart J. 42, 2455–2467 (2021).
McDonagh, T. A. et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European society of cardiology (ESC) with the special contribution of the heart failure association (HFA) of the ESC. Eur Heart J 42, 3599–3726 (2021).
Raport: Sytuacja zdrowotna ludności Polski i jej uwarunkowania - NIZP PZH - PIB. https://www.pzh.gov.pl/raport-sytuacja-zdrowotna-ludnosci-polski-i-jej-uwarunkowania/.
Heinberg, L. J. & Steffen, K. Social isolation and loneliness during the COVID-19 pandemic: Impact on weight. Curr. Obes. Rep. 10, 365–370 (2021).
Kuropka, I., Rossa, A., Wróblewska, W., Wojtyniak, B. & Śleszyński, P. Pandemia i jej skutki zdrowotne i demograficzne. 2AD https://doi.org/10.24425/140474 (2021).
Rozporządzenie Ministra Zdrowia z dnia 24 czerwca 2022 r. zmieniające rozporządzenie w sprawie świadczeń gwarantowanych z zakresu podstawowej opieki zdrowotnej. https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20220001355.
Rozporządzenie Ministra Zdrowia z dnia 14 czerwca 2021 r. w sprawie programu pilotażowego ‘Profilaktyka 40 PLUS’. https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20210001081.
Bryła, M., Maciak, A., Marcinkowski, J. T. & Maniecka-Bryła, I. Programy profilaktyczne w zakresie chorób układu krążenia przykładem niwelowania nierówności w stanie zdrowia. Probl. Hig. Epidemiol. 90, 6–17 (2009).
Krogsbøll, L. T., Jørgensen, K. J. & Gøtzsche, P. C. General health checks in adults for reducing morbidity and mortality from disease. Cochrane Database System. Rev. https://doi.org/10.1002/14651858.CD009009.pub3 (2019).
Mistry, H. et al. Determining optimal strategies for primary prevention of cardiovascular disease: systematic review of cost-effectiveness analyses in the United Kingdom. Health Technol. Assess. https://doi.org/10.3310/QOVK6659 (2022).
Kennedy, O., Su, F., Pears, R., Walmsley, E. & Roderick, P. Evaluating the effectiveness of the NHS health check programme in South England: a quasi-randomised controlled trial. BMJ Open 9, e029420 (2019).
Jørgensen, T. et al. Effect of screening and lifestyle counselling on incidence of ischaemic heart disease in general population: Inter99 randomised trial. BMJ 348, g3617 (2014).
Tsao, C. W. et al. Heart disease and stroke statistics-2023 update: A report from the American heart association. Circulation 147, E93–E621 (2023).
Świadomość wybranych czynników ryzyka chorób układu sercowo-naczyniowego w populacji młodych osób | Surma | Choroby Serca i Naczyń. https://journals.viamedica.pl/choroby_serca_i_naczyn/article/view/55239/44245.
Hyseni, L. et al. The effects of policy actions to improve population dietary patterns and prevent diet-related non-communicable diseases: scoping review. Eur. J. Clin. Nutr. 71, 694–711 (2016).
Jørgensen, T. et al. Population-level changes to promote cardiovascular health. Eur. J. Prev. Cardiol. 20, 409–421 (2013).
Czapla, M. et al. Psychometric properties and cultural adaptation of the polish version of the healthy lifestyle and personal control questionnaire (HLPCQ). Int. J. Environ. Res. Public Health 18, 9190 (2021).
Darviri, C. et al. The healthy lifestyle and personal control questionnaire (HLPCQ): A novel tool for assessing self-empowerment through a constellation of daily activities. BMC Public Health 14, 1–10 (2014).
McDonagh, T. A. et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European society of cardiology (ESC) With the special contribution of the heart failure association (HFA) of the ESC. Eur. Heart J. 42, 3599–3726 (2021).
Yusuf, P. S. et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet (Lond. Engl.) 364, 937–952 (2004).
Yusuf, S. et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet (Lond. Engl.) 395, 795–808 (2020).
Magnussen, C. et al. Global effect of modifiable risk factors on cardiovascular disease and mortality. N. Engl. J. Med. 389, 1273–1285 (2023).
Sun, J., Qiao, Y., Zhao, M., Magnussen, C. G. & Xi, B. Global, regional, and national burden of cardiovascular diseases in youths and young adults aged 15–39 years in 204 countries/territories, 1990–2019: a systematic analysis of Global Burden of Disease Study 2019. BMC Med. 21, 1–15 (2023).
Andersson, C. & Vasan, R. S. Epidemiology of cardiovascular disease in young individuals. Nat. Rev. Cardiol. 15, 230–240 (2018).
Clark, C. J. et al. Predicted long-term cardiovascular risk among young adults in the national longitudinal study of adolescent health. Am. J. Public Health 104, e108–e115 (2014).
Worsening Cardiovascular Risk Factors in U.S. Young Adults. https://www.jwatch.org/na55885/2023/03/07/worsening-cardiovascular-risk-factors-us-young-adults.
Garshick, M. S. et al. Cardiovascular risk factor control and lifestyle factors in young to middle-aged adults with newly diagnosed obstructive coronary artery disease. Cardiology 142, 83–90 (2019).
Wang, T. et al. Age-specific modifiable risk factor profiles for cardiovascular disease and all-cause mortality: a nationwide, population-based, prospective cohort study. Lancet Region. Health Western Pac. 17, 100277 (2021).
Stone, N. J. et al. Managing atherosclerotic cardiovascular risk in young adults: JACC state-of-the-art review. J. Am. Coll. Cardiol. 79, 819–836 (2022).
D’Agostino, R. B. et al. General cardiovascular risk profile for use in primary care: the Framingham heart study. Circulation 117, 743–753 (2008).
de Tamar, I. V. et al. SCORE2-OP risk prediction algorithms: estimating incident cardiovascular event risk in older persons in four geographical risk regions. Eur. Heart J. 42, 2455–2467 (2021).
Hippisley-Cox, J. et al. Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: prospective open cohort study. BMJ (Clin. Res. Ed.) 335, 136–141 (2007).
Hippisley-Cox, J. et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ (Clin. Res. Ed.) 336, 1475–1482 (2008).
Ridker, P. M., Buring, J. E., Rifai, N. & Cook, N. R. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds risk score. JAMA 297, 611–619 (2007).
Berger, J. S., Jordan, C. O., Lloyd-Jones, D. & Blumenthal, R. S. Screening for cardiovascular risk in asymptomatic patients. J. Am. Coll. Cardiol. 55, 1169–1177 (2010).
Lloyd-Jones, D. M. et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation 113, 791–798 (2006).
Dalton, J. E. et al. Accuracy of cardiovascular risk prediction varies by neighborhood socioeconomic position: a retrospective cohort study. Ann. Intern. Med. 167, 456–464 (2017).
DeFilippis, A. P. et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann. Intern. Med. 162, 266–275 (2015).
Bonaccio, M. et al. Low income is associated with poor adherence to a Mediterranean diet and a higher prevalence of obesity: cross-sectional results from the Moli-sani study. BMJ Open 2, e001685 (2012).
Domosławska-Żylińska, K., Łopatek, M., Krysińska-Pisarek, M. & Sugay, L. Barriers to adherence to healthy diet and recommended physical activity perceived by the polish population. J. Clin. Med. 13, 22 (2024).
Mierzecki, A. et al. Influence of folic acid supplementation on coagulation, inflammatory, lipid, and kidney function parameters in subjects with low and moderate content of folic acid in the diet. Polish Heart J. (Kardiologia Polska) 73, 280–286 (2015).
Mierzecki, A. et al. Association between low-dose folic acid supplementation and blood lipids concentrations in male and female subjects with atherosclerosis risk factors. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 19, 733–739 (2013).
Kalinowska, S. et al. The association between lifestyle choices and schizophrenia symptoms. J. Clin. Med. 10, 1–11 (2021).
Funding
This research was funded by the Wroclaw Medical University, SUBZ.C290.25.054 and Polish Society of Family Medicine.
Author information
Authors and Affiliations
Contributions
Conceptualization, M.B; methodology, M.B.; formal analysis, M.B.; investigation, M.B., J.L., T.Z., S.J., K.K., F.K., P.G., D.G., W.M., A.J.-K., P.J., M.Ch., A.M.-M.; resources, M.B., J.L., T.Z., S.J., K.K., F.K., P.G., D.G., W.M., A.J.-K., P.J., M.Ch., A.M.-M.; writing—original draft preparation, M.B., J.L., T.Z., S.J., K.K., F.K., P.G., D.G., W.M., A.J.-K., P.J., M.Ch., A.M.-M.; writing—review and editing, M.B., J.L., S.J., K.K., P.J., M.Ch., A.M.-M.;; visualization, M.B.,W.M.; supervision, A.M.-M., P.J., M.Ch. K.K.; project administration, M.B.; funding acquisition, A.M.-M. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
All participants were fully informed about the aims of the study and signed the informed consent form prior to completing the research instruments. Participation was voluntary, and confidentiality and anonymity were safeguarded at all times.
Institutional review board statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the independent Bioethics Committee of the Wroclaw Medical University (Decision No. KB-540/2022).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Babicki, M., Ledwoch, J., Zieliński, T. et al. Assessment of cardiovascular risk factors and effect of lifestyle in individuals without cardiovascular disease, diabetes or chronic kidney disease. Sci Rep 15, 13544 (2025). https://doi.org/10.1038/s41598-025-98215-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-98215-5