Abstract
We visualized the entry point (EP) of the anterior interosseous nerve (AIN) into the pronator quadratus (PQ) in the distal forearm with ultrasonography and examined its location to identify the safe zone for approaching the PQ on the volar side. The forearms of healthy volunteers without any musculoskeletal problems of the upper extremities were examined. Using high-resolution ultrasonography, the volar aspects of the forearms were scanned with elbows flexed at 90°. Using the images obtained, several parameters for distance were measured. Overall, 20 forearms were examined. The means ± standard deviations of the forearm length (A) and the distance from the wrist to the EP of the AIN (B), from the lateral margin of the ulna to the medial margin of the radius on the interosseous membrane (IOM) (C), from the lateral margin of the ulna to the AIN on the IOM (D), from the AIN to the skin surface (E) were 25.50 ± 1.56 cm, 4.18 ± 0.61 cm, 12.99 ± 1.99 mm, 6.63 ± 1.46 mm, and 18.85 ± 3.03 mm, respectively. The mean values of B/A and D/C were 0.16 ± 0.02 and 0.51 ± 0.08, respectively. We utilized high-resolution ultrasound to locate the EP of the AIN in the distal forearm in a three-dimensional space. These findings may provide insights into the nerve’s course and assist in establishing a safety zone to minimize the chances of accidental nerve injuries when inserting a needle toward the PQ.
Similar content being viewed by others
Introduction
The pronator quadratus (PQ) is one of the muscles of the deep compartment of the distal forearm. The function of the PQ is to pronate the forearm, along with the pronator teres. It is the most distal muscle innervated by the anterior interosseous nerve (AIN), which is a branch of the median nerve1. The AIN arises from the median nerve in the proximal forearm and runs distally between the deep surface of the PQ and the interosseous membrane (IOM), along with the anterior interosseous artery (AIA). After passing the proximal border of the PQ, the AIN enters the PQ muscle through its dorsal surface and divides into small branches2.
Approaching the PQ with a needle is not frequently necessary, except on some occasions when a detailed evaluation of the AIN is needed. For example, it is required in AIN syndrome, which can be caused by traumatic injury, compressive neuropathy, or Parsonage–Turner syndrome of the AIN3. Moreover, when addressing spasticity in the forearm pronator muscles of individuals who have experienced a stroke or children with cerebral palsy, it is occasionally necessary to inject botulinum toxin into these muscles, including the PQ4,5. Hence, precise targeting of the PQ during needle insertion techniques is of paramount importance to avoid inadvertently damaging nearby structures. However, the PQ cannot be palpated because it is located deeply within the anterior muscle group of the forearm6; therefore, it is not easy to approach the PQ with blind needling.
Despite these challenges, there are certain situations where blind needling may be inevitable, particularly when ultrasound is unavailable or impractical. For example, when access to ultrasound equipment is limited due to time constraints, equipment malfunction, or lack of trained personnel, blind needling may be the only option. In these circumstances, clinicians must rely on their knowledge of the anatomy and their clinical experience to perform the procedure safely.
Previous studies have suggested several different needle approach techniques for the PQ. Perotto et al. and Preston et al. suggested a dorsal approach7,8, while Lee and Delisa suggested a medial approach9. However, both of these approaches carry the risk of causing injury to the numerous neurovascular structures in the distal forearm.
As an alternative to the dorsal and medial approaches, Lee et al. suggested in their ultrasonographic study that for a safe examination of the PQ in needle electromyography, the needle should be inserted from the volar side of the forearm, just on the medial border of the palmaris longus tendon10. Park et al. confirmed this result by providing evidence through a cadaveric study11. However, previous studies have focused on avoiding injury to the median nerve and the ulnar artery and have not considered the possibility of damaging the AIN10,11. Moreover, as a considerable proportion of the population is born without the palmaris longus12, there are instances where using the palmaris longus tendon as a landmark is not possible. Therefore, even with the volar approach, there still exists a chance of damaging the AIN if the needle is deeply inserted close to the IOM, as the AIN runs on the anterior surface of the IOM.
The PQ, innervated by the AIN, is primarily responsible for forearm pronation, which is assisted by the pronator teres, and stabilization of the distal radioulnar joint6,13. Therefore, damage to the AIN at the distal forearm level can disrupt the active pronation of the forearm and cause instability of the distal radioulnar joint. Moreover, since the AIN is purely a motor nerve14, it is difficult for the patient to notice any sensory symptoms even when the AIN is contacted by the needle. Therefore, it is necessary to investigate the optimal needle insertion technique using the volar approach to avoid AIN injury.
To date, only a few studies have visualized the AIN in the distal forearm with ultrasonography. Therefore, we used ultrasonography to investigate the optimal approach for safely and precisely directing a needle towards the pronator quadratus muscle from the volar side without ultrasound guidance.
Methods
The forearms of healthy volunteers (aged > 19 years), without any history of trauma or musculoskeletal problems of the upper extremities, were examined between June 2022 and July 2022. The study was approved by the Institutional Review Board (IRB) of Korea University Guro Hospital (IRB No. 2020GR0360). Participation was voluntary, and written informed consent was obtained from all participants before participation in the study. This study was conducted in accordance with the tenets of the Declaration of Helsinki.
Ultrasonographic evaluation
Figure 1 shows a schematic of a cross-sectional image of the distal forearm. The PQ originates from the anteromedial surface of the distal ulna and inserts on the anterolateral surface of the distal radius, lying on the anterior surface of the IOM (Fig. 1)15. The AIN and the AIA are located between the PQ and the IOM.
Using a high-resolution real-time ultrasound system (RS80A; Samsung Medison, Seoul, Korea), the volar side of the distal forearm was scanned in a seated position, with the elbow flexed at 90° and the forearm supinated with the palm facing upward. A 3–12-MHz linear array transducer was placed perpendicular to the long axis of the forearm, and the IOM connecting the ulna and the radius was identified. The transducer was cautiously moved along the length of the forearm, such that the distal-most site where the AIN was visualized on the anterior surface of the IOM, which is the entry point (EP) of the AIN into the PQ, and a cross-sectional image of the forearm was obtained. The primary frequency of the ultrasound used in this study was approximately 8.0 to 10.0 MHz. Since the AIN is difficult to visualize because of its deep location and small diameter, a power doppler was used to identify the AIA as a landmark that courses along the AIN14,16. After locating the AIA, we identified the adjacent AIN, and in cases where the AIN was not clearly visible, we traced the nerve distally from the proximal forearm level, where the AIN bifurcates from the median nerve, to identify the AIN17. During the examination, the examiner applied the least possible pressure to the transducer.
Five distance parameters were defined using manual measurements and ultrasonographic images. The forearm length (A) was defined as the distance from the elbow crease to the distal wrist flexion crease, which is the most distal fold in the skin that appears when the wrist is flexed. The distance from the wrist to the EP of the AIN (B) was defined as the distance from the point at which the image was obtained to the distal wrist flexion crease. Assuming that the IOM was parallel to the local skin surface, the distances from the lateral margin of the ulna to the medial margin of the radius on the IOM (C), from the lateral margin of the ulna to the AIN on the IOM (D), and from the AIN to the skin surface (E) were measured (Fig. 1).
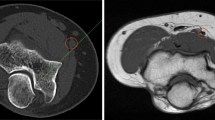
After measuring the distances, two additional parameters were defined using the distances measured above. The ratios of B to A (B/A) and D to C (D/C) indicate the relative position of the EP of the AIN in the entire forearm and the relative position of the AIN between the ulna and the radius, respectively. Figure 2 shows an example of the ultrasonographic images obtained from a participant’s forearm.
Ultrasonographic image of the distal volar forearm at the level of the entry point of the AIN into the PQ. AIA: anterior interosseous artery; AIN: anterior interosseous nerve; FCR: flexor carpi radialis; FDP: flexor digitorum profundus; FDS: flexor digitorum superficialis; FPL: flexor pollicis longus; PL: palmaris longus; PQ: pronator quadratus; R: radius; U: ulna.
Statistical analysis
Statistical analyses were performed using SPSS, version 20.0 software (IBM Corp., Armonk, NY, USA). The data were assessed for normal distribution using the Shapiro–Wilk test. As all measured parameters, including A, B, C, D, E, B/A and D/C, followed a normal distribution, the results are presented as means ± standard deviations (SDs).
Results
In total, 20 forearms were examined using high-resolution ultrasonography. The data are presented in Table 1. The means and SDs of forearm length (A), the distance from the wrist to EP of the AIN (B), the distance from the lateral margin of the ulna to the medial margin of the radius on the IOM (C), the distance from the lateral margin of the ulna to the AIN on the IOM (D), and the distance from the AIN to the skin surface (E) were 25.50 ± 1.56 cm, 4.18 ± 0.61 cm, 12.99 ± 1.99 mm, 6.63 ± 1.46 mm, and 18.85 ± 3.03 mm, respectively. Meanwhile, the mean values of B/A and D/C were 0.16 ± 0.02 and 0.51 ± 0.08, respectively.
Discussion
To our knowledge, this is the first study to address the anatomical location of the AIN in the distal volar forearm using high-resolution ultrasonography. In this study, we observed the level of the EP of the AIN into the PQ, its location in relation to the ulna and the radius, and its depth from the skin surface using ultrasonography. The average site of the AIN penetrating the PQ was approximately 4.18 cm proximal to the distal wrist flexion crease, and considering the anatomical variation, it was approximately 16% of the forearm length proximal to the distal wrist flexion crease. Moreover, the relative location of the AIN between the ulna and the radius at the level of the EP of the AIN was almost halfway between the two bony margins.
Focusing on the findings above, in this study, we identified the anatomical location of the AIN in the distal forearm with ultrasonography to suggest a valid and safe insertion technique for approaching the PQ on the volar side. The AIN entered the PQ and was thereby divided into small branches (4.18 cm proximal to the distal wrist flexion crease on average). Trowbridge et al., in their cadaveric study, demonstrated that the mean distance from the distal wrist crease to the entry point of the AIN into the PQ was 7.43 cm, which was longer than that observed in this study18. The reason for this difference could be attributed to several factors. First, they included only 10 forearms from cadavers, leading to significant measurement variation. Additionally, the study’s European population may have influenced the results. Choung et al. reported that the EP of the AIN into the PQ is located more distally in the Asian population than in other populations examined in previous works15.
As the height and forearm length may vary among individuals, we also measured the forearm length and calculated the ratio of the distance from the distal wrist flexion crease to the EP of the AIN to the forearm length, which was 16% on average. This concurs with the results of a previous study. Especially, Chough et al. reported that the EP of the AIN was located on the distal 13% of the forearm length15, which is slightly more distal than the results obtained in our work. The different definition of the forearm length might have led to the small difference.
Moreover, in this study, the average distance from the lateral margin of the ulna to the EP of the AIN on the IOM was 6.63 mm, which was 51% of the distance between the lateral margin of the ulna and the medial margin of the radius on the IOM. Previous cadaveric studies have evaluated the distance from the EP of the AIN to the medial border of the ulna or the lateral border of the radius15,18. However, these studies did not focus on the location of the EP of the AIN between the lateral margin of the ulna and the medial margin of the radius.
As the AIN is located nearly at the midpoint between the two bony margins at the level of the EP of the AIN, assuming that the examiner palpates the two bony margins on the patient’s wrist and inserts the needle at their midpoint, he or she can carefully manipulate the angle of needle insertion to avoid directing the needle vertically toward this midpoint.
If we define the point where the line containing the AIN and perpendicular to the IOM meets the skin as the insertion point (IP), and the angle between this line and the line connecting the IP to the lateral margin of the ulna as α, then tan α equals D/E. Therefore, α can be determined by calculating tan⁻¹ (D/E), which is 19.38°. Similarly, if we define the angle between this line and the line connecting the IP to the medial margin of the radius as β, then β is calculated as 18.64°. Therefore, if the examiner deviates the needle medially or laterally by a maximum of approximately 18° from the vertical line, he or she can approach the PQ while avoiding contact with the AIN.
Finally, the mean depth of the AIN at the level of the EP of the AIN was approximately 1.89 cm in our work. Lee et al. demonstrated that the deep vertical depth of the PQ at the level of the midpoint between the PQ muscle was 2.49 cm on average10, while Park et al. described that the mean distance from the skin to the deep margin of the PQ at the level 3 cm proximal to the tip of the ulnar styloid process was 1.99 mm, which was closer to our result11. These differences might have arisen from the different levels on the distal forearm where the measurement was conducted.
Based on our findings, to avoid AIN injury, we recommend inserting the needle distal to the point corresponding to 16% of the forearm length, measured proximally from the distal wrist crease, at a depth shallower than 1.89 cm, and with a medial or lateral deviation of up to approximately 18° from the midpoint between the lateral border of the ulna and the medial border of the radius.
However, our study had several limitations. First, the examination only involved 20 forearms of healthy volunteers from a single center. More reliable and widely applicable results could be obtained with a larger sample size from multiple centers. Second, the study did not consider other factors that could affect the safety and precision of needle insertion, such as anatomical variations and neuromuscular disorders. Finally, we mainly focused on the use of ultrasound for anatomical measurements. However, the practical significance and real-world utility of these findings for actual needle insertions and their impact on patient outcomes were not thoroughly explored or verified.
Conclusion
We employed high-resolution ultrasound imaging to examine the precise anatomical location of the EP of the AIN in the distal forearm within a three-dimensional context. These observations offer important information concerning the path of the nerve and assist in defining a safe zone to avoid accidental nerve injuries when inserting a needle toward the PQ.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Standring, S. & Gray, H. Gray’s Anatomy: The Anatomical Basis of Clinical Practice 42nd edn (Elsevier, 2011).
Svízenská, I., Cizmár, I. & Visna, P. An anatomical study of the anterior interosseous nerve and its innervation of the pronator quadratus muscle. J. Hand Surg. Br. 30, 635–637. https://doi.org/10.1016/j.jhsb.2005.06.017 (2005).
Caetano, E. B., Vieira, L. A., Sabongi Neto, J. J., Caetano, M. B. F. & Sabongi, R. G. Anterior interosseous nerve: Anatomical study and clinical implications. Rev. Bras. Ortop. 53, 575–581. https://doi.org/10.1016/j.rboe.2018.07.010 (2018).
Andringa, A. et al. The effect of botulinum toxin-A on neural and non-neural components of wrist hyper-resistance in adults with stroke or cerebral palsy. PM R. 14, 486–495. https://doi.org/10.1002/pmrj.12602 (2022).
Wong, V., Ng, A. & Sit, P. Open-label study of botulinum toxin for upper limb spasticity in cerebral palsy. J. Child. Neurol. 17, 138–142. https://doi.org/10.1177/088307380201700210 (2002).
Créteur, V., Madani, A. & Brasseur, J. L. Pronator quadratus imaging. Diagn. Interv. Imaging. 93, 22–29. https://doi.org/10.1016/j.diii.2011.10.006 (2012).
Perotto, A. & Delagi, E. F. Anatomical Guide for the Electromyographer: The Limbs and Trunk. 5th edCharles C. Thomas, Springfield, Illinois,. (2011).
Preston, D. C. & Shapiro, B. E. Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic Correlations 3rd edn (Elsevier Saunders, London, 2013).
Lee, H. J. & DeLisa, J. A. Manual of Nerve Conduction Study and Surface Anatomy for Needle Electromyography 4th edn (Lippincott Wilkins and Williams, 2005).
Lee, S. J., Kim, K. H., Cheong, I. Y., Park, B. K. & Kim, D. H. Safety window for the volar needle approach for examination of the pronator quadratus using ultrasonography. Arch. Phys. Med. Rehabil.. 98, 2553–2557. https://doi.org/10.1016/j.apmr.2017.04.019 (2017).
Park, H. B. et al. A cadaveric study for the volar needle approach to the pronator quadratus using the palmaris longus tendon landmark. Muscle Nerve. 60, 582–585. https://doi.org/10.1002/mus.26677 (2019).
Dimitriou, I., Katsourakis, A., Natsis, K., Kostretzis, L. & Noussios, G. Palmaris longus muscle’s prevalence in different nations and interesting anatomical variations: Review of the literature. J. Clin. Med. Res. 7, 825–830. https://doi.org/10.14740/jocmr2243w (2015).
Alves, N., Candido, P. L. & Frazao, R. Innervation of the pronator quadratus muscle. Int. J. Morphol. 22, 253–256. https://doi.org/10.4067/S0717-95022004000400002 (2004).
Choi, S. J. et al. Ultrasonography for nerve compression syndromes of the upper extremity. Ultrasonography 34, 275–291. https://doi.org/10.14366/usg.14060 (2015).
Choung, P. W. et al. Anatomic characteristics of pronator quadratus muscle: A cadaver study. Ann. Rehabil Med. 40, 496–501. https://doi.org/10.5535/arm.2016.40.3.496 (2016).
Walsh, P. J., Walter, W. R., Burke, C. J., Adler, R. S. & Beltran, L. S. Percutaneous ultrasound-guided intervention for upper extremity neural and perineural abnormalities: A retrospective review of 242 cases. Am. J. Roentgenol. 212, W73–W82. https://doi.org/10.2214/AJR.18.20047 (2019).
Yamada, H. et al. Nerve ultrasonography for the diagnosis and evaluation of neuralgic amyotrophy. Intern. Med. 62, 1843–1847. https://doi.org/10.2169/internalmedicine.0005-22 (2023).
Trowbridge, S. et al. The intra-muscular course and distribution of the anterior interosseous nerve within pronator quadratus: An anatomical study. J. Clin. Orthop. Trauma 28, 101868. https://doi.org/10.1016/j.jcot.2022.101868 (2022).
Acknowledgements
This study was supported by the Institute of Information & Communications Technology Planning & Evaluation (IITP) grant funded by the Korean government (MSIT) (No. 2021-0-00731).
Funding
This study was supported by the Institute of Information & Communications Technology Planning & Evaluation (IITP) grant funded by the Korean government (MSIT) (No. 2021-0-00731).
Author information
Authors and Affiliations
Contributions
PHJ: Protocol development, Data collection, Data analysis, Manuscript writing, Approval of final manuscript.KKH: Manuscript editing, Approval of final manuscript.YJS: Protocol development, Funding acquisition, Manuscript editing, Approval of final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Research involving human participants
This study was approved by the Institutional Review Board (IRB) of Korea University Guro Hospital (IRB No. 2020GR0360).
Informed consent
Informed consent was obtained from all individual participants included in the study. This study was conducted in accordance with the tenets of the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Park, H.J., Kang, K.H. & Yoon, J.S. Ultrasonographic study for optimal volar needle approach technique for the pronator quadratus to avoid anterior interosseous nerve injury. Sci Rep 15, 15139 (2025). https://doi.org/10.1038/s41598-025-98308-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-98308-1