Abstract
The increasing rate of obesity in children and adolescents is alarming, worldwide. This population-based study, conducted in 2024 in Fars Province, Iran, aimed to assess the prevalence of overweight and obesity among primary school students. In the 1st phase, the weight and height of 9853 students who were selected by multi-stage cluster random sampling from 36 districts were measured standardly. Then using World Health Organization AnthroPlus software, body mass index-for-age z-score (BAZ) of each subject was calculated and exported to the SPSS. Analysis showed the overall prevalence of overweight/obesity was 26.5% (n = 2616), including 14.7% (n = 1450) as overweight, 9.4% (n = 927) as obese, and 2.4% (n = 239) as severe obese. Logistic regression showed older students, who with normal height, and who lived in the cities or educated in private schools were more overweight/ obese. In the 2nd phase, an online-based checklist was sent to the parents of overweight/obese children, to query about family, demographic and socioeconomic status. Logistic regression on the data of 440 students who participated in this phase revealed that obesity was more common in males, while overweight was more common in female students (OR 2.5, 95% CI 1.5–3.9). Furthermore, 79% of overweight and 21% of obese students’ parents did not know about their children’s excess body weight, before attending this study (OR 7.2, 95% CI 3.8–13.9). In the 3rd phase, mapping with Bayesian model showed a higher prevalence of obesity in the western and southern counties. Setting public health strategies including massive screening and multidisciplinary interventions (at the individual, family, community, and micro, meso, and macro level of policy-making) to address childhood overweight /obesity, particularly in the high-prevalence areas, is recommended.
Similar content being viewed by others
Introduction
Children overweight or obesity is an increasing global public health problem that along with undernutrition and micronutrient deficiencies, causes a triple burden of disease, especially for low- and middle-income countries1. According to the World Health Organization (WHO), over 390 million children and adolescents aged 5–19 years were overweight in 2022, including 160 million who were living with obesity2. Over the past two decades, the rates of overweight and obesity in developing countries have risen from 10 to 25% and 2 to 10%, respectively3; showing a 30% higher prevalence of overweight/obesity in children and adolescents in developing countries compared to the developed countries 3. This increasing trend is observed in almost all Middle Eastern countries during recent decades4,5. Iran ranks among the top countries for childhood obesity and witnessed a doubling rate of obesity rate among its children from 2000 to 20166,7. This rise in childhood overweight has led to approximately 20% of children being classified as overweight8.
Health risks of obesity include fatty liver, diabetes, hypertension, cardiovascular diseases, orthopedic problems, sleep disorders, cancer, and mental health issues that ultimately result in long-term complications and premature death9,10,11,12,13,14. Childhood obesity is caused by or is associated with a variety of factors including genetic, environmental, socio-economic, cultural, and life behavioral styles such as nutrition, physical activity, and media exposure9.
There are 500,000 primary school children between the ages of 7–12 years old in Fars province of Iran, which consists 10% of the total population in this province. Unlike less than 7-year-old children whose growth is monitored regularly in healthcare centers, primary school students do not receive consistent monitoring of their weight and height, therefore there is no provincial information about the prevalence of overweight /obesity and its determinants in this group. As such, this study aimed to fill this gap and present evidence about these items and also to compare the prevalence of obesity among this group of population with previous studies.
Subjects and materials
Statistical population
Fars province with five million population is the fourth populous province of Iran. It is located in south west of Iran and consisted of 37 counties including 124 cities (Fig. 1). This population includes about one million school students including a half million primary school students with nearly an equal boy to girl’s ratio (1.06). All primary school students consisted the statistical population in this study.
Study design, sample size and sampling method
This cross-sectional study was conducted in 2024. Considering 20% estimated prevalence of overweight /obesity in children of Iran15, confidence interval 95% and error up to 3%, the initial calculated sample size was 686. Furthermore, by considering the effect of gender, urban versus rural place of residency, education in the public versus private schools and design effect 2, final sample size was calculated as 10,976. As a multi-stage cluster random sampling, 36 districts were selected as clusters and the proportional sample size of each cluster was defined. In the next step, in each cluster, at least one boy and one girl elementary school in the cities and one elementary school with both boys and girls in the villages were selected randomly as the sample units. Sample size of each selected school was defined, then according to the population of 1-6 th grades in the selected schools and using systematic randomization method, students were selected from the different grades.
Data collection and standard measurements
At first, one health-care teacher was chosen from each selected district. These health-care teachers are the staff of department of education and monitor the health status of students, periodically. We held an in-person workshop for them. In the workshop, they were justified about objectives of this study, standard protocols of weight and height measurement and checklists that they were asked to fill them. Their access to the standard digital balances and tapes was checked and in case of any deficiency, we resolved the problem. They were trained to measure height and weight of students while they were wearing light clothes without shoes. Weight was measured by digital balance which its scale could be read to the nearest 1 kg. Balances were calibrated at the beginning of each working day and at frequent intervals throughout the day. Height was measured to the nearest 0.5 cm, using a measuring tape. To measure height, the measuring tape was fixed to the wall. Height was measured while the subject stood with heels, buttocks, shoulders and occipital touching the vertical tape. The head was held erect with the external auditory meatus and the lower border of the orbit in one horizontal plane16. Checklist consisted of students’ gender, date of birth, weight, height, grade, the type of school (urban/rural, public/private) and mobile number of parents. Teachers attended in the selected schools and measured weight and height of students and filled the checklists. In the next step, and after checking the quality of all data one by one, students who had overweight or obesity were defined by statistical analysis. Then, we had phone contacts with one of the parents of those children who their parents’ mobile number had been defined. We explained for them about this study, its objectives, findings of the 1st step and upcoming next steps. We asked them if they were willed to participate in the next steps or not? If they willed to participate, the link of the 2nd checklist which was designed on an online platform called Porsline, was sent to them to fill it. This checklist consisted of questions about number of children, birth order of the studied child, how often parents measure the weight and height of their children, and if they and their spouses know and having concern about complications of overweight or obesity in their children and have willingness to be referred to specialists to control the weight of their children or not? We also asked them, if they knew before participation in this study that their children were overweight or obese, and if they did any attempt for controlling the weight of their children and if these attempts had any positive effect or not? They were also queried about their and their spouses’ age, relativity, weight, height, level of education, job status, income to cost balancing and coverage by basic and supplementary insurances.
Data analysis
Data analysis was performed in three phases. At 1st phase, the quality of weight and heights’ data of 10,976 students were checked and data of 9853 students were qualified finally to enter into the analysis. The quality checking process involved assessing the quality of measurements (including devices and tools) through prior training on these measurements, as well as ensuring the completeness of checklists to avoid any confounding factors. Additionally, 10% of the questionnaires were randomly selected for review, and the information on the checklists was compared with the data in the software for consistency. These data were entered into the World Health Organization (WHO) AnthroPlus software 1.0.4 to define the Body Mass index (BMI)-for-age z-score (BAZ). WHO AnthroPlus is a software application that was created to support the tracking of growth for both individuals and populations of children from birth up to 19 years old and identifying issues such as thinness, underweight, overweight, and obesity within this age group. For this pupose three pertinent indicators have been introduced : weight-for-age, height-for-age, and BMI-for-age17. According to this application manual, children aged 5–19 years who fall at the + 1 standard deviation in the WHO reference (equivalent to the 85th percentile) coincide at 19 years with the adults’ cut-off for overweight, which is BMI = 25 [kg/m2]. Similarly, those at the + 2 standard deviation (equivalent to the 97th percentile), coincide at 19 years with the adults’ cut-off for obesity which is BMI = 30 [kg/m2. Additionally, individuals at the + 3 standard deviation will be classified as severely obese (corresponding to a BMI of above 35 [kg/m2])17. In the analysis in this phase, we categorized students into two groups; group with excess body weight (overweight/obese/severe obese) as one group and other states as another group. In the 2nd phase, using IBM SPSS Statistics 25.0, univariable analysis with parametric and if indicated (non-normal distribution of variables) with non-parametric tests was done. Variables with p < 0.2 were selected and entered into the multivariable analysis (logistic regression: Backward LR method) which in this model, p < 0.05 was considered as the significance level. In this phase comparisons were made between two groups of overweight and obese/severe obese. In the 3rd phase, the geographical variations of the prevalence of overweight/obesity (as one group) in the 36 selected counties were analyzed and depicted. The observed number of overweight and obese cases in a geographic unit (county) was assumed to follow a Poisson distribution. We used the BYM (Besag York Mollié) spatial model which is a useful tool for analyzing areal data, where an outcome variable is aggregated into areas that make up a study region. These models can be customized to account for the variability in the response variable based on known covariates that impact the outcome, along with random effects to capture unexplained variation18. It was coded in the Open BUGS software (package for performing Bayesian inference using Gibbs sampling) version 3.2.3 for estimating the parameters. Aeronautical Reconnaissance Coverage Geographic Information System (ArcGIS) version 10.1 was also used to display the results on maps. We ran two chains with 1000 samples as burn-in and 10,000 samples as iteration. Convergence for the chains was confirmed by auto-correlations, trace, and densities plots.
Results
Phase one
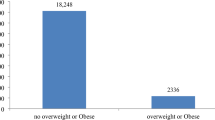
Data of 9853 students, which were captured in the 1st phase of data collection, has been entered into the analysis, showing 89.7% of the calculated sample size (10,976). This reduction of sample size was due to non-qualified (incomplete, confounded, duplicated) data of 1123 students. Analysis showed an overall prevalence of overweight/obesity was 26.5% (n = 2616); including 14.7% (n = 1450) as overweight, 9.4% (n = 927) as obese and 2.4% (n = 239) as severe obese. In the univariable analysis in this step; gender, age, height, place of residency, type of school and grade in school were found to be associated significantly with overweight/obesity (Table1). As shown in Table 1; female students, who with normal height, who lived in the urban areas, who educated in the private schools, who were older or were in higher grades were significantly more overweight/obese than their counterpart groups (p < 0.05). Furthermore, the prevalence of overweight/obesity was on increasing slope from 1st grades (18.5%) to the 5th grades (32.9%), while to some extent it decreased in the 6 th grades (30.6%) (Table 1). Logistic regression, showed that those students who had normal height, older ones, those who lived in urban areas and those who educated in private schools had a more odds of being overweight or obesity compared to the counterpart groups (Table 1).
Phase two
In the 2nd phase, 440 parents (368 mothers and 72 fathers) filled the checklists through messaged link. As presented in Table2, data was belonged to two groups of students: those who were overweight (n = 205, 46.6%) and those who were obese/severe obese (n = 235, 53.4%). Univariable analysis showed that among studied variables, overweight (55% vs. 34.4%) was more common in female while obesity (65.6% vs. 45%) was more prevalent in male students (p < 0.001) (Table 2).
As demonstrated in Table3, multivaribale analysis revealed that male students had a more prevalence of obesity compared to the female students (OR 2.5, 95% CI 1.5–3.9). Furthermore, 79% of overweight and 21% of obese students’ parents did not know about their children’s excess body weight, before attending this study (OR 7.2, 95% CI 3.8–13.9); showing a high detection rate of new cases of overweight and remarkable proportion of new cases of obese ones in this massive screening (Table 3). In this phase, out of 2616 participants with overweight/obesity, 105 parents filled nutrition-related questions (response rate: 4.01%). This ratio about physical activity was 88 parents out of 2616 (response rate: 3.36%).
Phase three
Figure 1, illustrates the mapping of overweight /obesity prevalence in the Fars province. Shades are prevalence ratio (PR), as darker areas show a higher prevalence compared to the mean of prevalence of overweight /obesity in this province. It is highlighted that 12 counties with higher PR were mostly located in the western and southern regions of this province. These counties are predominantly neighboring areas, which suggests the potential influence of similar environmental and socioeconomic factors.
Discussion
This study found that at least one-fourth of primary school students were overweight or obese, with approximately 1 in 7 classified as overweight and 1 in 9 as obese. It was also revealed that those students who had normal height, older ones, those who lived in urban areas and those who educated in the private schools had a more odds of being overweight/obesity compared to the counterpart groups. We also found that overweight was more prevalent among female students, while obesity was more prevalent among male students. Furthermore, it was revealed that massive screening yielded a high detection rate of new cases of overweight and remarkable proportion of new cases of obesity in primary school students.
Prevalence studies
The rising prevalence of obesity among children is alarming and has been changed to a global public health concern. Being overweight or obese, affects children’s immediate and long term outcomes. From 1990 to 2022, the percentage of children and adolescents aged 5–19 years living with overweight/obesity had been risen dramatically from just 8% in 1990 to 20% in 2022. This rise had been occurred similarly among both boys and girls: in 2022 19% of girls and 21% of boys were overweight. When consider only the obesity, it was prevalent among just 2% of children and adolescents aged 5–19 in 1990 (31 million young people), while it was increased four-fold and was 8% (160 million young people) in 2022. Furthermore, once it was considered a problem only in high-income countries, today some middle-income countries have the highest prevalence of overweight/obesity worldwide2.
Different studies were conducted around the world about body weight in children. In the United States, an overweight rate of 16.1% in children aged 2–19 years old, and an obesity rate of 20.3% in the elementary school age group (6–11 years old) was reported 18. In Croatia, and among primary school students, the findings showed an increase in the prevalence of overweight /obesity from 23.4% in the first to 30.2% in the fifth grade, returning back to 23.4% in the eighth grade. This finding was nearly similar to our findings that revealed some decreasing in the prevalence of overweight/obesity in the 6 th grades compared to the 5 th grades students, despite its increasing from the 1st toward 5 th grades19. A systematic review in in 2022, concluded that the overall prevalence of obesity and overweight in primary school children of Iran was 14.3% (3.1–14.3%), and 18.8% (5.5–18.8%), respectively20. A meta-analysis in 2022 estimated the prevalence of obesity in the age group of 2–15 years of Iran to be 11.4%8. Another meta-analysis reported 18.7% obesity rates in the primary school students of Iran7. In the Fars province, Iran, which our study was conducted, only one study was done before (in 2007) that showed obesity rate 9.4% in the same age group21. Our findings in this study more or less are similar to the other studies’ findings, however increasing trend of childhood obesity in the recent decades8,22 and variabilities in the methodologies and studied age groups could justify some of the differences in findings of reported studies.
Demographic factors
Age and gender are important factors that can influence body mass. Our study found a trend of increasing overweight prevalence as children age, which is in line with another study23, however another survey rejected such relationship 24. It also believed that lifestyle-related risk factors, such as sedentary behaviors, accumulate with aging and may lead to obesity25. Older children may have less parental supervision, allowing for more autonomy and peer influence over food choices, potentially leading to unhealthy eating habits and obesity26. In the population scale of all primary school students, there was not a significant difference between the prevalence of weight excess (overweight/obesity) between boys and girls. This finding was in line with some other studies27,28. However, some other studies reported opposite findings20,29. On the other hand in comparison between overweight and obese students, girls showed a more prevalence of overweight while boys were more obese, that it was in line with the findings of another study in Iran20.
The current study also found that children with normal height had a higher odds of being overweight/obesity compared to children with moderate to severe stunting. This finding may show that the second group may suffer from chronic undernutrition, however, this hypothesis needs to be investigated by another study. In opposite, another study revealed a positive association between obesity and stunting30.
Some studies showed that the number of siblings and birth order are associated with children’s obesity31,32,33. Families with fewer siblings may have different dynamics, leading to less shared responsibility in parenting and decision-making around nutrition and physical activity. This can result in more permissive eating behaviors and less emphasis on physical activity34. Smaller families may also experience unique stressors that impact children’s eating habits and access to food. Stress can lead to emotional eating and create environments where children have more food and fewer physical activity opportunities35. We did not find any significant correlation between number of siblings or birth order and child obesity in our study. Our study also found that pupils in the urban areas were more overweight/obese than those who were lived in the rural areas. This finding was similarly addressed in other studies36,37, while other studies revealed an opposite finding38,39. This result may be attributed to more access to junk foods, more limited physical activity, sedentary life style rising of technology and screen time, which might be dominant in rural students.
Socioeconomic factors
Socioeconomic status is known as one of the factors affecting childhood obesity40. In our study, indicators such as type of school (private or public), parent’s education and occupation, and family’s income-to-expenditure ratio were assessed. Among them, only attending in private schools was associated significantly with a higher likelihood of childhood obesity. There are conflicting conclusions about the role of these factors in childhood obesity in the other studies20.
Some studies show that socioeconomic status was positively related to childhood obesity41, while others show a negative correlation in this regard19,42. A study concluded that regardless of household socioeconomic status, children attending public schools have higher BMI than those attending private schools. That study argued that eligibility for free or reduced-cost lunch or breakfast programs at public schools was positively correlated with children’s BMI43. Another study in Tehran, Iran did not show any significant association between primary school students’ obesity and the type of their schools44.
Effects of peers, schools, marketing, and the media on children’s food habits and choices was reported by a study45, however, we did not assess these items in our study.
Parental factors
Family factors play a significant role in children’s obesity46. Previous studies showed that the risk of obesity in children increases about three times if only one of the parents is obese47. Moreover, children’s food habits and choices are influenced by family, and successful interventions for preventing childhood obesity should include family-based programs45.
In our study, no significant association was found between father or mothers’ weight or their awareness about complications of obesity and their children’s obesity. However, another survey concluded that parents’ concerns about the health status of their obese children have led to better nutritional knowledge toward their youngsters48.
Regarding the association between childhood abnormal weight and parental awareness about their children’s weight status, previous studies’ findings were in line with the current study and higher rate of misperception was reported in parents of overweight/obese children49,50. However, according to these reports, underestimation had a direct relation with the severity of overweight, while in this study unawareness among parents of overweight children was more prevalent compared to obese ones51. Although the trend of this problem has been decreasing over time51, its rate remains concerning and further cause finding and interventional surveys are required.
Nutrition
The role of nutrition in childhood obesity was determined in the other studies20,45,52. In our study and for nutritional assessment of the studied children, we sent two online-based 24-h dietary recall (24HR) forms, one for non-holiday and one for holiday, to parents. However, only a small number participated in this part of the study. Therefore, we preferred not to include this part in the data analysis.
Physical activity
Some studies found a significant association between childhood obesity and physical activity20,45. In Croatia, and among primary school students, it was revealed that participation in the sport had only a significant and direct association with BMI of boys in the 1st grade19. In our study and for physical activity assessment of studied children, we sent an online-based questionnaire (PAQ-C) for parents. However, only a small number filled it. Therefore, we preferred to not include this part in the data analysis.
Geographical distribution
In this study, maps indicated that counties with a high prevalence of childhood overweight/obesity are clustered together, mainly in the western and southern parts of Fars province. Various factors including varying levels of socioeconomic status, urban versus rural population ratios, and also cultural diversity may contribute to this issue. As another study concluded, cultural diversity influences physical activity levels, traditional recipes and snacks, and meal sizes and composition in different regions53. The availability of raw materials also impacts the dietary patterns of a region. These factors can affect calorie intake and consequently contribute to the overweight issues in those areas54. However, these hypotheses need to be scrutinized by other studies in our region.
Strengths, limitations, recommendations
As a population-based survey with large scale sample size which was based on multi-stage cluster random sampling method, we tried to present a representative picture of the prevalence of overweight /obesity in primary school students and its demographic, socioeconomic and family factors. A standardized and consistent protocol for data collection further enhanced the validity of this study’s findings. Furthermore, this research can provide a solid foundation for future longitudinal studies on childhood obesity and offer valuable insights for public health interventions in this region. As a substantial limitation in this study, the role of nutrition, physical activity, peers and media were not be assessed, which potentially limiting a comprehensive outlook to the all-related factors related to obesity in children. Only a few respondents filled the questionnaires regarding nutrition and physical activity. However, this limitation was not far from expectations as conducting an online-based survey in large scale and about all factors related to obesity, needs a high logistic, a long list of questionnaires, vast time spending by parents that may lead to survey fatigue, causing respondents to lose interest, and resulted in increasing attrition rate of participation and confounds the validity and reliability of data. As a recommendation, further analytical studies should be implemented to investigate the effects of other probable underlying factors such as puberty, and also interventional studies to correct BMI of children via addressing different factors including diet and physical activity, with a focus on the contextual factors, especially in areas with high prevalence is suggested. Regarding parental awareness, additional root cause analysis is recommended.
Conclusion
This study revealed the importance of massive screening in detection of new cases of overweight and obesity in primary school students, the high prevalence of overweight/obesity among them, and association of some of the demographic, socioeconomic and familial factors with it. Therefore, considering childhood obesity as a growing priority in public health and setting a comprehensive national strategy targeting individuals, families, and community, and Targeted, multidisciplinary interventions at the micro, meso, and macro level of policy-making —such as school nutrition programs, increased physical activity initiatives, and parental education campaigns—should be prioritized, especially in high-prevalence regions.
Data availability
Raw data would be made available upon reasonable request from the corresponding author for scientific research purposes in accordance with data sharing policies and regulations of SUMS.
References
Vassilakou T. Childhood malnutrition: time for action. MDPI; 2021. p. 103.
World Health Organization. Obesity and overweight. Key Facts [Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Smith, K. & Smith, M. Obesity Statistics. Primary Care: Clinics in Office Practice (Elsevier, 2016).
Farrag, N. S., Cheskin, L. J. & Farag, M. K. A systematic review of childhood obesity in the Middle East and North Africa (MENA) region: Prevalence and risk factors meta-analysis. Adv. Pediatr. Res. 4, 8 (2017).
Mirmiran, P., Sherafat-Kazemzadeh, R., Jalali-Farahani, S. & Azizi, F. Childhood obesity in the Middle East: a review. EMHJ 16(9), 1009–1017 (2010).
Khatami, F. et al. Iranian children with overweight and obesity: an internet-based interventional study. BMC Pediatr. 21(1), 221 (2021).
Khazaei, S. et al. Obesity among Iranian primary school students: A systematic review and meta-analysis. Payesh (Health Monitor). 16(1), 17–26 (2017).
Akbari, H. & Mohammadi, M. The Prevalence of Obesity in Iranian Children: A Systematic Review and Meta-analysis. J. Pediatr. Rev. 10(2), 93–102 (2022).
Haeri, F., Shariatpanahi, S. P. & Kafeshani, M. Prevalence of obesity in the first grade primary school children in Mehriz, Iran, based on different references of body mass index. J. Health Syst. Res. 17(4), 269–274 (2022).
Apperley, L. J. et al. Childhood obesity: A review of current and future management options. Clin. Endocrinol. 96(3), 288–301 (2022).
Caprio, S., Santoro, N. & Weiss, R. Childhood obesity and the associated rise in cardiometabolic complications. Nat. Metab. 2(3), 223–232 (2020).
Park, H. et al. Metabolic complications of obesity in children and adolescents. Clin. Exp. Pediatr. 67(7), 347 (2023).
Smith, J. D., Fu, E. & Kobayashi, M. A. Prevention and management of childhood obesity and its psychological and health comorbidities. Annu. Rev. Clin. Psychol. 16(1), 351–378 (2020).
Ferreira, I. B. B. et al. Childhood obesity is associated with a high degree of metabolic disturbance in children from Brazilian semi-arid region. Sci. Rep. 14(1), 17569 (2024).
Taghizadeh, S., Khodayari-Zarnaq, R. & Farhangi, M. A. Childhood obesity prevention policies in Iran: a policy analysis of agenda-setting using Kingdon’s multiple streams. BMC Pediatr. 21(1), 250 (2021).
Greenwood, J. L., Narus, S. P., Leiser, J. & Egger, M. J. Measuring body mass index according to protocol: how are height and weight obtained?. J. Healthc. Quality (JHQ). 33(3), 28–36 (2011).
WHO AnthroPlus for personal computers Manual: Software for assessing growth of the world’s children and adolescents. Geneva: WHO, 2009.
Banerjee, S., Carlin, B. P. & Gelfand, A. E. Hierarchical Modeling and Analysis for Spatial Data (Chapman and Hall/CRC, 2003).
Stierman, B., Afful, J., Carroll, M.D., Chen, T.C., Davy, O., Fink, S., et al. National Health and Nutrition Examination Survey 2017–March 2020 prepandemic data files development of files and prevalence estimates for selected health outcomes. 2021.
Šimunović, I., Mrčela, D., Karin, Ž, Pogorelić, Z. & Markić, J. Prevalence of Overweight and Obesity among Primary School Students in Split, Croatia. Nutrients 16(20), 3488 (2024).
Saeidi, M., Naseri, M., Vakili, R. & Sistanian, F. The prevalence of obesity and overweight in iranian primary school students: A systematic review. Health Provid. 2(1), 13–22 (2022).
Ayatollahi, S. & Mostajabi, F. Prevalence of obesity among schoolchildren in Iran. Obes. Rev. 8(4), 289–291 (2007).
Mirmohammadi, S.-J., Hafezi, R., Mehrparvar, A. H., Rezaeian, B. & Akbari, H. Prevalence of overweight and obesity among Iranian school children in different ethnicities. Iran. J. Pediatr. 21(4), 514 (2011).
Kranjac, A. W. & Wagmiller, R. L. Association between age and obesity over time. Pediatrics https://doi.org/10.1542/peds.2015-2096 (2016).
Hales, C. M., Fryar, C. D., Carroll, M. D., Freedman, D. S. & Ogden, C. L. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA 319(16), 1723–1725 (2018).
Katzmarzyk, P. T. et al. Relationship between lifestyle behaviors and obesity in children ages 9–11: Results from a 12-country study. Obesity 23(8), 1696–1702 (2015).
Golan, M. Parents as agents of change in childhood obesity–from research to practice. Int. J. Pediatr. Obes. 1(2), 66–76 (2006).
Oktaviani, S., Mizutani, M., Nishide, R. & Tanimura, S. Factors associated with overweight/obesity of children aged 6–12 years in Indonesia. BMC Pediatr. 23(1), 484 (2023).
Küçükali, E., Ince, O., Aydin, A. & Günay, T. Identification of significant risk factors for obesity among children aged five to nine years: A cross-sectional analysis. J. Pediatr. Res. 11(2), 88–94 (2024).
Shah, B., Cost, K. T., Fuller, A., Birken, C. S. & Anderson, L. N. Sex and gender differences in childhood obesity: Contributing to the research agenda. BMJ Nutr. Prevent. Health 3(2), 387 (2020).
Symington, E. A., Gericke, G. J., Nel, J. H. & Labadarios, D. The relationship between stunting and overweight among children from South Africa: Secondary analysis of the national food consumption survey-Fortification baseline I. S. Afr. Med. J. 106(1), 65–69 (2016).
Bohn, C. et al. Having siblings promotes a more healthy weight status—whereas only children are at greater risk for higher BMI in later childhood. PLoS ONE 17(7), e0271676 (2022).
Kelishadi, R. et al. Is single-child family associated with cardio-metabolic risk factors: The CASPIAN-V study. BMC Cardiovasc. Disord. 18, 1–8 (2018).
Ochiai, H. et al. Number of siblings, birth order, and childhood overweight: A population-based cross-sectional study in Japan. BMC Public Health 12, 1–7 (2012).
Park, S. H. & Cormier, E. Influence of siblings on child health behaviors and obesity: A systematic review. J. Child Fam. Stud. 27, 2069–2081 (2018).
Pachucki, M. C., Lovenheim, M. F. & Harding, M. Within-family obesity associations: Evaluation of parent, child, and sibling relationships. Am. J. Prev. Med. 47(4), 382–391 (2014).
Premkumar, S. & Ramanan, P. V. Rural childhood obesity–an emerging health concern. Indian J. Endocrinol. Metab. 23(3), 289–292 (2019).
Arslan, H. N., Dundar, C. & Terzi, O. Prevalence of overweight and obesity among school children and parents: A cross-sectional study. Rural Remote Health 21(4), 1–9 (2021).
Crouch, E., Abshire, D. A., Wirth, M. D., Hung, P. & Benavidez, G. A. Peer reviewed: Rural-urban differences in overweight and obesity, physical activity, and food security among children and adolescents. Prevent. Chronic Dis. https://doi.org/10.5888/pcd20.230136 (2023).
Dong, Y. et al. Geographical variation and urban-rural disparity of overweight and obesity in Chinese school-aged children between 2010 and 2014: Two successive national cross-sectional surveys. BMJ Open 9(4), e025559 (2019).
Craig, L. C., McNeill, G., Macdiarmid, J. I., Masson, L. F. & Holmes, B. A. Dietary patterns of school-age children in Scotland: Association with socio-economic indicators, physical activity and obesity. Br. J. Nutr. 103(3), 319–334 (2010).
Gamboa-Gamboa, T., Fantin, R., Cordoba, J., Caravaca, I. & Gómez-Duarte, I. Relationship between childhood obesity and socio-economic status among primary school children in Costa Rica. Public Health Nutr. 24(12), 3825–3833 (2021).
Gupta, N., Goel, K., Shah, P. & Misra, A. Childhood obesity in developing countries: epidemiology, determinants, and prevention. Endocr. Rev. 33(1), 48–70 (2012).
Li, J. & Hooker, N. H. Childhood obesity and schools: evidence from the national survey of children’s health. J. Sch. Health 80(2), 96–103 (2010).
Soheilipour, F., Pishgahroudsari, M. & Pazouki, A. Overweight and obesity prevalence in iranian children aged 8–12 years; a study in Tehran. J. Compr. Pediatr. https://doi.org/10.5812/compreped-120827 (2022).
Roblin, L. Childhood obesity: food, nutrient, and eating-habit trends and influences. Appl. Physiol. Nutr. Metab. 32(4), 635–645 (2007).
Kumar, S. & Kelly, A. S. Review of childhood obesity: from epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin. Proc. 92, 251–265 (2017).
Whitaker, R. C., Wright, J. A., Pepe, M. S., Seidel, K. D. & Dietz, W. H. Predicting obesity in young adulthood from childhood and parental obesity. N. Engl. J. Med. 337(13), 869–873 (1997).
Faghih, S. et al. Assessment of obesity, unhealthy food habits, and nutritional knowledge of primary school children. Int. J. School Health 2(2), 1–5 (2015).
Rodrigues, D., Machado-Rodrigues, A. M. & Padez, C. Parental misperception of their child’s weight status and how weight underestimation is associated with childhood obesity. Am. J. Hum. Biol. 32(5), e23393 (2020).
Ramos Salas, X. et al. Parental perceptions of children’s weight status in 22 countries: The WHO European childhood obesity surveillance initiative: COSI 2015/2017. Obes Facts. 14(6), 658–674 (2021).
Ruiter, E. L. M. et al. Parents’ underestimation of their child’s weight status Moderating factors and change over time: A cross-sectional study. PLoS ONE 15(1), e0227761 (2020).
Kim, J. & Lim, H. Nutritional management in childhood obesity. J. Obes. Metab. Syndr. 28(4), 225 (2019).
Chatham, R. E. & Mixer, S. J. Cultural influences on childhood obesity in ethnic minorities: a qualitative systematic review. J. Transcult. Nurs. 31(1), 87–99 (2020).
Fang, D., Thomsen, M. R., Nayga, R. M. & Goudie, A. Association of neighborhood geographic spatial factors with rates of childhood obesity. JAMA Netw. Open 1(4), e180954 (2018).
Acknowledgements
We would like to cordially thanks to all children’s parents who participated in this study. We also have a special thanks to Fars Governorate, deputy of Research and Technology and deputy of Health Affairs; especially Mrs. Maharat at Shiraz university of medical sciences. Moreover, Education department of Fars province and all health-care teachers of schools who supported us in conducting this large study are appreciated.
Funding
This study was funded by SUMS and working group of research and technology council of Fars Governorate with grant no: 28492.
Author information
Authors and Affiliations
Contributions
B.H., L.E., K.B.L., P.K., L.A., R.K. contributed in the conceptualization of research’s idea. B.H., F.R., E.Z., F.B., N.H., F.S., Z.H. contributed in proposal writing and data collection. B.H., A.D., F.Y., Y.M. contributed in manuscript drafting and data analysis. B.H., A.D., N.A. contributed in statistical analysis, modelling and mapping. A.G., M.A.Z., S.K.H., F.G. were technical assistants and supervised all administrative steps of this study. All authors participated in internal peer review and writing the final version of manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The ethics committee of Shiraz University of Medical Sciences (SUMS) approved the study’s protocol and encoded it as IR.SUMS.REC.1402.049. Also, we were committed to and observed the 1964 Helsinki Declaration protocol in this study. Children’ parents were informed about the objective of this study and informed consent was obtained from each of them. Furthermore, all participants were made aware that their participation in the study was voluntary and that they could withdraw at any point. Additionally, they were given the assurance that their information would be kept confidential and participation in this study is free of charge. In case of children with overweight/obesity, they were referred to specialists to solve their problem.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Honarvar, B., Erfannia, L., Rafiee, F. et al. Overweight and obesity and its determinants in primary school students: a population-based study from Iran. Sci Rep 15, 21010 (2025). https://doi.org/10.1038/s41598-025-98352-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-98352-x