Abstract
The HDP prediction model was constructed and validated by using the demographic characteristics, blood routine and biochemical screening indicators in early pregnancy to reduce the incidence of HDP. 16,112 pregnant women admitted to Yuyao People’s Hospital from May 1, 2018 to April 30, 2022 were randomly divided into modeling group (n = 11279) and validation group (n = 4833) according to a ratio of 7:3. Demographic characteristics, blood routine and biochemical screening data of 8–12+ 6 weeks gestation were obtained from Ningbo Health Records system. Univariate analysis and multivariate binary Logistic regression analysis were used to determine the independent risk factors of HDP, and the scoring system was established by using the nomogram. Univariate analysis and multivariate binary Logistic regression analysis showed that Age, BMI, previous medical history, HB, TG, HDL and ALB were independent risk factors for HDP (P < 0.001). In the modeling group, AUC = 0.809, sensitivity = 74.30%, specificity = 73.10%, and in the validation group, AUC = 0.801, sensitivity = 77.60%, specificity = 68.90%. Hosmer-Lemeshow goodness of fit test showed that modeling group: P = 0.195 > 0.05, validation group: P = 0.775 > 0.05. The prediction model of early pregnancy Age, BMI, previous medical history, HB, TG, HDL and ALB can effectively predict the occurrence of HDP.
Similar content being viewed by others
Introduction
Hypertensive disorders complicating pregnancy (HDP) is a disease unique to women during pregnancy. It refers to the sudden occurrence of high blood pressure in pregnant women with no history of hypertension, more than after 20 weeks of gestation. Generally within 12 weeks after delivery, it can return to normal on its own, and is a common cause of maternal and perinatal death1,2.It has been reported3 that the global incidence of HDP is as high as 5–10%. The main clinical symptoms of HDP are hypertension, proteinuria and edema.In severe cases, pregnant women can suffer systemic multi-organ damage or functional failure until death. The disease will not only cause harm to pregnant women such as placental abruption, disseminated intravascular coagulation, cerebral hemorrhage and even death, but also cause harm to the fetus such as intrauterine dysplasia, premature delivery and death, seriously threatening the life and health of the mother and child4,5.The pathogenesis of hypertensive diseases in pregnancy is complex, and the mechanism of occurrence can not be explained by any single factor, but by a combination of maternal, placental, fetal and other factors. At present, we are in an era of personalized, predictable and participatory medical big data, and the occurrence, development or prognosis of diseases can be predicted. ACOG practice bulletin6 points out that early screening of HDP risk factors are extremely important. Early and accurate screening of HDP high-risk groups is of great significance to improve maternal and infant prognosis7,8,9. The clinical prediction model is a quantitative tool for personalized clinical risk assessment, which is built on the support of several logically-calculated variables. In recent years, the construction of HDP prediction model at home and abroad is in the development stage.A retrospective case-control study10 analyzed 62 pregnant women with HDP and confirmed that the HDP risk prediction model established by using maternal impedance electrocardiogram, electrocardiogram Doppler ultrasound and bioimpedance combined with demographic data has high predictive value and clinical significance.Another retrospective case-control study11 analyzed 117 pregnant women with HDP. Seven independent predictors were selected by logistic regression and a prediction model was built based on them. However, the above two studies have not been validated by the model, the number of cases is small, and some predictors are not common clinical examination indicators, so it is difficult to popularize. Therefore, there is no unified prediction method for the prediction model of HDP that can be applied to the clinical practice of real events. Based on this, we need to find a simple and easily available laboratory data to build a predictive model to guide clinical practice, so as to achieve early detection, early diagnosis and early intervention for pregnant women with HDP, and provide data support for improving maternal and infant prognosis.
Materials and methods
Research object: 16,112 pregnant women admitted to Yuyao People’s Hospital from May 1, 2018 to April 30, 2022 were randomly divided into modeling group and validation group according to a ratio of 7:3.Among them, there were 11,279 cases in the modeling group.According to the diagnostic criteria, 936 HDP pregnant women in the modeling group were set as the experimental group, and the other 10,343 pregnant women in the same period were set as non-HDP group. The demographic characteristics including age, birth time, pregnancy time, body mass index (BMI), education level, residence and previous medical history, blood routine and biochemical screening data of pregnant women during the first trimester (8–12+ 6 weeks) were obtained from Ningbo Health Records system. In this study, pregnant women diagnosed with hypertensive disease during pregnancy returned to normal blood pressure at 12 weeks postpartum follow-up, excluding chronic hypertension. This study is a retrospective case-control study, which has been approved by the Ethics Committee of Yuyao People’s Hospital, all methods were performed in accordance with the relevant guidelines and regulations, and all pregnant women participating in this study gave their informed consent.
Inclusion criteria
① Basic clinical data and examination data were complete; ② Patients know the research content and pass the medical ethics visa-free written informed letter.
Exclusion criteria
① Incomplete medical history; ② Cases with clinical outcomes before the data collection of predictive indicators. ③ Cases of essential hypertension.
The inclusion/exclusion criteria flow chart as shown in Fig. 1.
Research content and method
Demographic data collection: Demographic data of the pregnant women were collected, namely Age, body mass index (BMI), birth time, pregnancy time, place of residence (rural, urban), education level (postgraduate or above, university, college or below), and previous medical history.
Blood routine detection: 3 ml of venous blood was collected on fasting and serum indicators including Platelet count(PLT), Hemoglobin(HB), and Hematocrit (HCT) were detected. AG800 automatic platelet aggregator, manufacturer: Shandong Telixin; XN-9000 automatic blood analyzer, manufacturer: SYSMEX, Japan.
Biochemical index detection: 5 ml venous blood was taken on an empty stomach and biochemical index detection was performed, including: Total cholesterol (TC), Triglyceride (TG), High density lipoprotein (HDL), Low density lipoprotein (LDL), glutamic oxaloacetic transaminase (AST), glutamic pyruvic transaminase (ALT), Uric acid acid (UA), Albumin (ALB), Total bilirubin (T-BIL), and Direct bilirubin (D-BIL). Type 008AS automatic biochemical analyzer, manufacturer: Hitachi Diagnostic Products Limited company.
Research method
First, a baseline comparison was made between the data of the modeling group and the validation group to determine the comparability of the two groups of data. Then, a single factor analysis was performed on the data of the modeling group, and the risk factors of HDP were initially screened out. Finally, variables with P < 0.05 in the screened single factor analysis were regarded as independent variables, and binary Logistic regression analysis was performed to determine the independent risk factors of HDP. Receiver operating characteristic (ROC) curve and calibration diagram were used to test the differentiation and consistency of the prediction models of the modeling group and the validation group, so as to determine the value of the prediction and diagnosis of the model.
Statistical method
SPSS 25.0 software and R4.4 software were used for statistical analysis. The counting data were tested by chi-square test on the two groups, expressed by the number of cases (percentage); The continuous data with normal distribution on the two groups were represented by t test, which was expressed by mean ± standard deviation; the non-normal distribution was represented by rank sum test, which was expressed by median (25th ~ 75th percentile) [M (P25 ~ P75)]. After univariate analysis, statistically significant variables were included in multivariate Logistic regression analysis, and the method “Forward: LR” was selected to screen the risk factors affecting hypertensive diseases in pregnancy, and a risk prediction nomogram model was constructed. Unless otherwise noted, P < 0.05 was considered statistically significant. By drawing receiver operating characteristic (ROC) curves, we can calculate the area under the ROC curver(AUC) of the modeling group and validation group.The AUC was used to evaluate the overall differentiation of the model, and the Hosmer-Lemeshow goodness of fit test was used to evaluate the quality of the goodness of fit effect of the model, and the calibration chart was used to test the consistency of the prediction model of the modeling group and the validation group.
Results
Incidence of hypertensive disorders during pregnancy: A total of 16,112 pregnant women were included in this study, including 1352 HDP cases, and the incidence of HDP was 8.39%. Among them, there were 11,279 cases in the modeling group, including 936 HDP cases, and the incidence of HDP in the modeling group was 8.30%. There were 4833 cases in the validation group, including 416 HDP cases, and the incidence of HDP in the validation group was 8.61%. Comparison of baseline data between the modeling group and the validation group as shown in Table 1.
The results of the comparative analysis of the two groups of baseline data showed that: The included 16,112 cases were randomly divided into the modeling group (11279 cases) and the validation group (4833 cases) according to a ratio of 7:3. The included indicators were classified data and Chi-square test was performed on the two groups. The continuous data in the two groups met the normal distribution and the rank sum test was taken if they did not meet the normal distribution. The results showed that there were no significant differences in all indicators between the modeling group and the validation group (P > 0.05). In summary, it could be considered that the baseline data of the two groups were comparable.
Single-factor analysis results of two groups of data in the modeling group as shown in Table 2.
The results of single factor analysis of demographic data, blood routine indexes and biochemical indexes in the modeling group showed that: Chi-square test was performed on the classified data of the two groups with or without hypertensive disease in pregnancy in the modeling group. T-test was taken for continuous data consistent with normal distribution, and rank sum test was taken for data inconsistent with normal distribution. The results showed that previous medical history, Age, BMI, HB, HCT, TC, TG, HDL, LDL and ALB were the factors that affected hypertensive diseases during pregnancy (P < 0.05), and there was no statistical difference in other indicators (P > 0.05).
Assignment of some independent variables of HDP multi-factor Logistic regression in the modeling group as shown in Table 3.
HDP multi-factor Logistic regression analysis results in the modeling group as shown in Table 4.
The results of multi-factor Logistic regression analysis showed that: In the modeling group, with or without pregnancy-induced hypertension as the dependent variable and P < 0.05 as the independent variable in the univariate analysis, binary Logistic regression analysis was carried out, and the method was selected as “Forward: LR “, the results showed that the previous medical history(OR = 3.760, 95%CI: 3.105–4.553, P < 0.001), Age(OR = 1.087, 95%CI: 1.072–1.103, P < 0.001), BMI (OR = 1.151, 95%CI: 1.128–1.175, P < 0.001), HB (OR = 1.052, 95%CI: 1.045–1.059, P < 0.001), TG (OR = 1.633, 95%CI: 1.489–1.791, P < 0.001), HDL(OR = 0.615, 95%CI: 0.523–0.723, P < 0.001)and ALB (OR = 0.887, 95%CI: 0.867–0.907, P < 0.001) were independent risk factors for hypertensive diseases during pregnancy.
Presentation of HDP prediction model
According to the above multivariate Logistic regression analysis, 7 variables were selected, and R language was used to construct a nomogram to assess the risk of HDP. The score value of each variable corresponds to the score of the top scoring axis, and then the score of 7 variables is added together to obtain the total score. The total score corresponds to the value on the bottom axis, which is the occurrence risk probability of HDP as shown in Fig. 2.
The evaluation of the prediction model
The ROC curve analysis showed that the prediction model of both the modeling group and the validation group was valuable in predicting and diagnosing the risk of hypertensive pregnancy (P < 0.05). In the modeling group, AUC = 0.809, sensitivity = 74.30%, specificity = 73.10%. In the validation group, AUC = 0.801, sensitivity = 77.60%,specificity = 68.90%. It shows that the prediction model has a good degree of differentiation as shown in Fig. 3A and B.
The Hosmer-Lemeshow goodness of fit test was used to evaluate the quality of the goodness of fit effect of the model. The Hosmer-Lemeshow goodness of fit test showed that the modeling group:χ2 = 11.112, P = 0.195 > 0.05, and the validation group: χ2 = 4.832, P = 0.775 > 0.05, indicating that the calibration degree of the two prediction models was good, and the existing information was fully used to fit the models. The calibration chart is an intuitive representation of the test result. Through the calibration curve, we can see the accuracy of the model prediction as shown in Fig. 4A and B.
Discussion
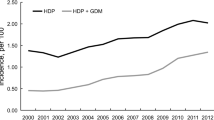
HDP is a group of diseases mainly characterized by abnormal increase of blood pressure during pregnancy.According to statistics12,13,14, the incidence of HDP at home and abroad is increasing year by year. The latest WHO data shows that the global incidence of HDP was about 116.4 per 100,000 women of childbearing age in 2019, seriously endangering the health and safety of mothers and children.In addition, studies have proved that HDP is closely related to the occurrence of short-term and long-term cardiovascular diseases in pregnant women15,16.Previous studies have shown that if pregnant women with HDP are not treated in time, the incidence of adverse pregnancy outcomes is significantly increased17, so early identification and prevention in clinical practice is crucial.At present, there have been many reports on HDP prediction models at home and abroad18,19, but the risk factors contained in these models are not uniform, and the relevant indicators can not be obtained by routine inspection, so it is difficult to routinely apply in primary hospitals, especially in resource-poor areas.Most maternal and perinatal deaths are reported to occur in low and middle income countries20.Some studies have pointed out21 that the physical function impairment caused by HDP has a significant performance in the early pregnancy and presents a state of continuous progression. Based on this, finding a simple and easily available laboratory data to build an early prediction model is extremely important to improve maternal and infant outcomes.
In this study, the early prediction model of HDP was constructed based on the demographic characteristics, blood routine and biochemical indicators of early pregnancy. The data used in the model were all routine test items during childbirth, which were easy to obtain. The AUC of this research model is 0.809, which is higher than the prediction model constructed by Ji Jiansheng22.A total of 16,112 pregnant women were included in this study, including 1352 cases of HDP, and the incidence of HDP was 8.39%. They were randomly divided into modeling group and validation group according to a ratio of 7:3. Statistical data showed that there was no significant difference in all indicators between the modeling group and the validation group (P > 0.05), so it could be considered that the baseline data of the two groups was comparable. After univariate analysis and multivariate Logistic regression analysis, it was confirmed that Age, BMI, previous medical history, HB, TG, HDL and ALB were independent risk factors for HDP (P < 0.001). Finally, based on the above 7 variables selected by multivariate Logistic regression analysis, R language was used to construct a nomogram for evaluating the risk of HDP, and the model was visualized and easy to understand.In order to validate the reliability of the model, an internal validation method was used in this study. The validation results showed that the AUC of the validation group was 0.801, the sensitivity was 77.60%, and the specificity was 68.90%, indicating that the prediction model had good differentiation.In addition, Hosmer-Lemeshow goodness of fit test showed that the modeling group: χ2 = 11.112, P = 0.195 > 0.05, and the validation group:χ2 = 4.832, P = 0.775 > 0.05. Combined with the intuitive performance of the calibration chart, the prediction model had good consistency and high accuracy.
Demographic data are readily available in clinical practice. The results of this study are consistent with the relevant studies of Ji Jiansheng22. The survey of the demographic information of pregnant women in the early pregnancy can effectively predict the risk of HDP.HDP can occur in women of all ages during the reproductive period, but many real-world statistics show that advanced pregnancy is an important risk factor for HDP. The ACOG Practice Bulletin in 201923 adjusted the age of risk factors from > 40 years to ≥ 35 years, and pointed out that advanced age (age ≥ 35 years old) is an independent high risk factor for hypertensive diseases in pregnancy24.A multicenter cohort study confirmed25 that a significantly increased risk of pregnancy induced hypertension in older women compared to women of childbearing age (OR = 3.11, 95%CI: 1.79–5.38, P < 0.001).A retrospective case-control study26 pointet out that maternal age ≥ 40 years old was an independent risk factor for hypertensive disease in pregnancy (AOR 1.5; 95%CI:1.3–1.7,P < 0.001).Studies have pointed out27 that with the increase of age, the physiological functions of the body, including the uterus, decrease and the elasticity of blood vessels decrease, which leads to the decrease of the adaptability of the body and the impairment of the endothelial function of blood vessels, resulting in hemodynamic changes and the eventual increase of blood pressure. In addition, The insulin sensitivity of elderly pregnant women is weakened, which affects the function of islet beta cells, easily leads to lipid metabolism disorder, aggravates metabolic syndrome, and eventually leads to increased blood pressure in pregnant women. This study also showed that the older the age, the higher the risk of HDP (OR = 1.087, 95%CI: 1.072–1.103). At present, the delay of childbearing age is a universal problem in the world, so how to predict and prevent the occurrence of HDP in elderly pregnant women is a challenge and difficult problem faced by obstetricians.
In this study, BMI was found to be positively correlated with the occurrence of HDP (OR = 1.151, 95%CI: 1.128–1.175, P < 0.001).A multicenter cohort study28 showed that Overweight and obese women respectively had a 1.92-fold(aRR = 1.92, 95% CI: 1.73–2.14, P < 0.001) and 5.06-fold (aRR = 5.06, 95%CI: 4.43–5.78, P < 0.001) increased risk of developing preeclampsia compared with women with normal body mass indexand, and the faster the rate of weight gain during pregnancy, the higher the incidence of preeclampsia. Higher preconception BMI and gestational weight gain are not only independent risk factors for the increased incidence of preeclampsia, but also have a superposition effect.Another multicenter retrospective study29 was the first to explore the association between intergestational annual BMI change and HDP in subsequent pregnancies, and found that increased annual BMI was an independent risk factor for HDP in subsequent pregnancies (aOR = 2.30; 95% CI: 1.76–3.01), and suggested that an increase in BMI of ≥ 1.0 kg/m² per year was associated with HDP in subsequent pregnancies in women with no history of HDP.The specific pathogenesis between BMI and HDP remains unclear. Currently, it is believed that obesity may increase the level of oxidative stress, cause dyslipidemia, hyperinsulinemia and insulin resistance, induce the increase of inflammatory factors in systemic blood circulation, accelerate the damage of vascular endothelial cells, and thus lead to HDP30.
In this study, previous medical history was the strongest predictor of HDP (OR = 3.760, 95%CI: 3.105–4.553, P < 0.001).A multicenter study31 found that preexisting medical history was an important predictor of hypertensive disease during pregnancy, the HDP rate of pregnant women with a history of hypertensive disease during pregnancy was 5 times higher than that of women without a history of hypertensive disease during pregnancy (AOR = 5.25,95%CI: 1.39–19.86), the rate of HDP in pregnant women with a history of kidney disease was 3.25 times higher than that without a history of kidney disease (AOR = 3.32, 95% CI: 1.04–10.58), and the rate of HDP in pregnant women with a history of asthma was 38 times higher than that without a history of asthma (AOR = 37.95, 95% CI: 1.41–1021).An US cohort study32 pointed out that pregnant women with a history of thyroid disease were susceptible to HDP, hypothyroidism was significantly associated with preeclampsia (OR = 1.47, 99%CI: 1.20–1.81) and superimposed preeclampsia (OR = 2.25, 99%CI: 1.53–3.29), hyperthyroidism was significantly correlated with preeclampsia (OR = 1.78, 99%CI = 1.08–2.94) and superimposed preeclampsia(OR = 3.64, 99%CI: 1.82–7.29) .
Hemoglobin is the core test item in blood routine.Current relevant studies33 believe that anemia during pregnancy can lead to adverse pregnancy outcomes, such as hypertensive diseases during pregnancy.This study confirmed that high hemoglobin level was positively correlated with the occurrence of HDP (OR = 1.052, 95%CI: 1.045–1.059, P < 0.001).A multicenters retrospective study34 found that hemoglobin levels in early pregnancy were significantly positively associated with preeclampsia, and pregnant women with hemoglobin levels ≥ 130 g/L had a significantly increased risk of preeclampsia (OR = 1.303, 95%CI: 1.006–1.689, P < 0.001), this association was particularly significant when hemoglobin levels exceeded 150 g/L (OR = 2.375, 95%CI: 1.203–4.688, P < 0.001).A prospective cohort study35 confirmed that the risk of pregnancy-induced hypertensive disease in pregnant women with high hemoglobin concentration (HB ≥ 132 g/L) in early pregnancy was 1.462 times that of the normal control group (110 g/L ≤ HB < 132 g/L) (OR = 2.462, 95%CI: 0.995–6.090, P = 0.045).These results are basically consistent with the results of this study.The mechanism between high hemoglobin level and HDP has not been fully clarified. Currently, it is believed that high Hb concentration leads to increased blood viscosity in pregnant women, thereby reducing placental microvascular blood flow, resulting in placental hypophoria and decreased oxygenation, and ultimately placental ischemia and hypoxia, resulting in HDP34.Relevant evidence also shows that high hemoglobin level reflects iron overload to a certain extent. Iron is a strong pro-oxidant, and iron overload will increase oxidative stress of beta cells, lead to insulin resistance, accelerate the expression of inflammatory factors in pregnant women’s blood circulation, and thus cause vascular endothelial cell damage and cause HDP36.In addition, it has been proved that37 hemoglobin plays a direct role in the regulation of nitric oxide (NO), which is an effective vasodilator and can cause the expansion of vascular smooth muscle cells, while free Hb can bind to NO, thus leading to vascular contraction, and then placental ischemia and hypoxia, inducing HDP.
Blood lipids are the general term of lipids contained in blood. Abnormal metabolism of blood lipids in pregnant women can induce maternal inflammation, oxidative stress and vascular endothelial dysfunction, thus leading to HDP30.In this study, it was found that triglyceride was positively correlated with HDP (OR = 1.633, 95%CI: 1.489–1.791, P < 0.001), while high-density lipoprotein was negatively correlated with HDP (OR = 0.615, 95%CI: 0.523–0.723, P < 0.001).A prospective study38 found that the increase of maternal triglyceride was more significant in the preeclampsia group (P < 0.05), and the increase of fetal triglyceride in the preeclampsia group was more significant than that in the normal pregnancy group, which also provided a theoretical basis for exploring the role of this indicator in the long-term cardiovascular risk of the mother and offspring.An analysis of 41 cohort studies39 showed that triglycerides were significantly higher in women with preeclampsia and eclampsia than in women with normal pregnancy (MD = 7.7 mg/dL, 95%CI:3.6–11.7), while high-density lipoprotein levels were significantly lower than those in the normal pregnancy group (MD=-2.15 mg/dL, 95% CI: 3.46–0.85).These results are basically consistent with the results of this study. The specific mechanism of dyslipidemia and HDP remains unclear.At present, it is believed that when pregnant women suffer from lipid metabolism disorder, triglycerides will further increase, which will cause the reduction of prostacyclin synthesis in vascular endothelial cells and trigger vasospasm. The decrease of HDL level can inhibit the accumulation of anti-lipid, lead to the increase of lipid peroxide, and seriously damage vascular endothelial cells. In addition, abnormal lipid levels can reduce nitric oxide synthesis, lead to vasoconstriction and diastole disorders, and trigger systemic arteriolar spasm, all of which provide conditions for the occurrence and development of HDP40.
In this study, ALB was an independent risk factor for hypertensive disorders during pregnancy and was negatively associated with HDP(OR = 0.887, 95%CI: 0.867–0.907, P < 0.001). A prospective study41 dynamically tracked the ALB during pregnancy, the results showed that the extent of ALB decline in the preeclampsia group can early forewarn preeclampsia(AUC = 0.742)and can also early forewarn severe preeclampsia(AUC = 0.756).There was a significant negative correlation between ALB level and the incidence of preeclampsia complications (r=-0.19, P < 0.01).A recent prospective study42 showed that the serum albumin level of preeclampsia pregnant women was significantly lower than that of the control group (F = 102.3, P < 0.001), and the incidence of adverse pregnancy outcomes was higher.Relevant studies41,43 have pointed out that serum albumin can remove free radicals in the body, inhibit the production of free radicals by multinucleated cells, and have anti-oxidative stress effects. In the subclinical stage of HDP, serum albumin has undergone a series of changes, and the abnormal level may be the first clinical manifestation before the clinical symptoms of HDP pregnant women, and it is also one of the indicators of laboratory changes in the subclinical stage.
In summary, the prediction model constructed by Age, BMI, previous medical history, HB, TG, HDL and ALB of pregnant women in early pregnancy can effectively monitor and manage high-risk pregnancy groups, better guide clinical work, and provide strong evidence for early detection, diagnosis and treatment of hypertensive diseases in pregnancy, so as to reduce adverse pregnancy outcomes and improve maternal and infant prognosis.
Innovation of research
Based on the current situation, combined with the actual clinical needs, this study analyzed and constructed the HDP prediction model and nomogram based on the risk factors of HDP in pregnant women, and carried out internal validation at the same time. Its innovation lies in using the research objects of the observation group to construct the model and the research objects of the validation group to carry out internal validation. The clinical application value and feasibility of the prediction model and the nomogram were evaluated comprehensively. In addition, the indicators used in this study are all routine clinical prenatal examination items, which are easy to obtain and do not increase additional costs, so it has strong promotion.
Limitations of the study
(1) As this study is a retrospective analysis, information bias is inevitable.
(2) Although the sample size is large, the study object is only limited to Yuyao People’s Hospital, which is a single-center study with limited regional limits. The application feasibility of the model still needs to be confirmed by large-sample and multi-center studies.
For the above problems, large sample and multi-center clinical studies can be conducted in the future, and HDP types can be studied in groups if necessary. Moreover, long-term health effects of HDP need to be followed up for a long time. In the future, the correlation between HDP and the long-term health of mother and child can be further studied to provide new ideas for clinical diagnosis and treatment.
Data availability
The data that support the findings ofthis study are available from thecorresponding author upon reasonable request.
References
Agrawal, A. & Wenger, N. K. Hypertension during pregnancy. Curr. Hypertens. Rep.. 22, 64–65 (2020).
Alipour, J., Payandeh, A. & Karimi, A. Prevalence of maternalmortality causes based on ICD-MM: a systematic reviewand meta-analysis. BMC Pregnancy Childbirth. 23, 821 (2023).
Unger, T. et al. International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 75,1334–1357(2020). (2020).
Jiang, L. et al. A global view ofhypertensive disorders and diabetes mellitus duringpregnancy. Nat. Rev. Endocrinol. 18, 760–775 (2022).
Agrawal, S., Cerdeira, A. S. & Redman, C. Meta-Analysis and systematic review to assess the role of soluble FMS-Like tyrosine Kinase-1 and placenta growth factor ratio in prediction of preeclampsia: the SaPPPhirE study. Hypertension. 71, 306–316 (2018).
ACOG Practice Bulletin No. 202 Summary: gestational hypertension and preeclampsia. Obstet. Gynecol. 133, 1 (2019).
Lu, Y., Chen, R., Cai, J., Huang, Z. & Yuan, H. The management of hypertension in women planning for pregnancy. Br. Med. Bull. 128, 75–84 (2018).
Gestational Hypertension and Preeclampsia. ACOG practice bulletin summary, number 222. Obstet. Gynecol. 135, 1492–1495 (2020).
Leavitt, K. & Običan, S. Treatment and prevention of hypertensive disorders during pregnancy. Clin. Perinatol. 46, 173–185 (2019).
Vonck, S. et al. Development of a biophysical screening model for gestational hypertensive diseases. Biomed. Sci. 26, 38–39 (2019).
Hou, Y., Yun, L., Zhang, L., Lin, J. & &Xu, R. A risk factor-based predictive model for new-onset hypertension during pregnancy in Chinese Han women. BMC Cardiovasc. Disord. 20, 155 (2020).
Tuo, Y. et al. Global, regional, and National burden of thalassemia, 1990–2021: a systematic analysis for the global burden of disease study 2021. EClinicalMedicine 72, 102619 (2024).
Jiang, L. et al. A global view ofhypertensive disorders and diabetes mellitus duringpregnancys. Nat. Rev. Endocrinol. 18, 760–775 (2022).
Alipour, J. & Payandeh, A. Prevalence of maternalmortality causes based on ICD-MM: a systematic reviewand meta-analysis.BMC.Pregnancy. Childbirth. 23, 821 (2023).
Theilen, L. H. Pre-eclampsia and cardiovascular risk: comparingapples with apples. BJOG.125,1655 (2018).
Siargkas, A. et al. Impact of velamentous cord insertion on perinatal outcomes:asystematic review and meta-analysis.Am.J.Obstet.Gynecol. MFM5, 100812 (2023).
Reddy, M. et al. Challenging the definition of hypertension in pregnancy: a retrospective cohort study. Am. J. Obstet. Gynecol. 222, 606e1–606e21 (2020).
Saleh, L. et al. Prediction of preeclampsia-related complications in women with suspected or confirmed pre-eclampsia: development and internal validation of clinical prediction model.ultrasound. Obstet. Gynecol. 58, 698–704 (2021).
Ukah, U. V. et al. Placental growth factor for the prognosis of women with preeclampsia (fullPIERS model extension):context matters.BMC.Pregnancy.Childbirth.20, 668 (2020).
Heestermans, T. et al. Prognostic models for adverse pregnancy outcomes in low-income and middle-income countries: a systematic review.bmj. Glob Health 4, e001759–e001760 (2019).
Metoki, H. et al. Hypertensive disorders of pregnancy:definitio, managenlent and out-of-office blood pressure measurement. Hypertensres. 45,1298–1309 (2022).
Ji, J. S., Chen, M. F., Zhou, M. L. & Chen, D. Q. Construction and verification of prediction model of hypertensive disorders of pregnancy based on demographic and clinical characteristics. Maternal Child. Health Care China. 36, 4878–4884 (2021).
ACOG Practice Bulletin NO. 202 Gestalional Hypertension and Preeclampsia.Obstet Gynecol.133,1(2019).
Wang, D. W. et al. Clinical characteristics of138 hospitalized patients with 2019 novel Coronavirus-Infected pneumonia in Wuhan. China JAMA 323,1061–1062 (2020).
Fitzpatrick, K. E., Tuffnell, D., Kurinczuk, J. J. & Knight, M. Pregnancy at very advanced maternal age: a UK population-based cohort study. BJOG 124, 1097–1106 (2017).
Corrigan, L., O’farrell, A., Moran, P. & Daly D. Hypertension in pregnancy: prevalence, risk factors and outcomes for women birthing in Ireland.Pregnancy. Hypertens. 24,1–6 (2021).
Gestational Hypertension and Preeclampsia:ACOG Practice Bullentin, Number.222 Obstet Gynecol. 135,e237-e260 (2020).
Gong, X. et al. Risk of preeclampsia by gestational weight gain in women with varied prepregnancy BMI:a retrospective cohort study. Front. Endoernol(Lausanne). 13, 1–9 (2022).
Tano, S. et al. Annual body mass index gain and risk of hypertensive disorders of pregnancy in a subsequent pregnancy. Sci. Rep. 11, 22519 (2021).
Zaki, M. et al. Evaluation of DNA damage profle in obese women and its associaton to risk ofmetabolic syndrome, polyeystic ovary syndrome and recurrent prseclampsia.genes. Dis 5, 367–373 (2018).
Gudeta, T. A. Pregnancy induced hypertension and associated factors among women attending delivery service at Mizan-Tepi university teaching hospital, Tepi general hospital and Gebretsadik Shawo hospital, Southwest, Ethiopia. Ethiop. J. Health Sci. 29, 831–840 (2019).
Männistö, T. et al. Thyroid diseases and adverse pregnancy outcomes in a contemporary US cohort. J. Clin. Endocrinol. Metab. 98, 2725–2733 (2013).
Daru, J. et al. Risk of maternal mortality in women with severe anaemia during pregnancy and post partum: a multilevel analysis. Lancet Glob Health. 6, e548–e554 (2018).
Wang, C. et al. Hemoglobin levels during the first trimester of pregnancy are associated with the risk of gestational diabetes mellitus, pre-eclampsia and preterm birth in Chinese women: a retrospective study. BMC Pregnancy Childbirth 18,263-264 (2018).
Aghamohammadi, A., Zafari, M. & &Tofighi, M. High maternal hemoglobin concentration in first trimester as risk factor for pregnancy induced hypertension. Casp. J. Intern. Med. 2, 194–197 (2011).
Liu, Q. et al. Role of iron deficiency and overload in the pathogenesis of diabetes and diabetic complications. Curr. Med. Chem. 16, 113–129 (2009).
Treuer, A. V. & Gonzalez, D. R. Nitric oxide synthases,S-nitrosylation and cardiovascular health: from molecular mechanisms to therapeutic opportunities (review). Mol. Med. Rep. 11, 1555–1565 (2015).
Alahakoon, T. I., Medbury, H. J., Williams, H. & Lee, V. W. Lipid profiling in maternal and fetal circulations in preeclampsia and fetal growth restriction-a prospective case control observational study. BMC Pregnancy Childbirth 20, 61–62 (2020).
Alonso-Ventura, V. et al. Effects of preeclampsia and eclampsia on maternal metabolic and biochemical outcomes in later life: a systematic review and meta-analysis. Metabolism 102, 154012 (2020).
Chen, W., Guo, Y., Yao, X. & Zhao, D. Correlation of blood lipid and serum inflammatory factor levels with hypertensive disorder complicating pregnancy. Front. Surg. 9, 917458 (2022).
Shi, J. M., Yang, Z., Li, F. Q. & Wang, G. J. Preliminary study of human serum albumin level in early warning onset of preeclampsia. Chin. J. Obstet. Gynecol. 55, 29–30 (2020).
Ye, S. & Jiang, Y. Correlation of 24-h urinary protein excretion, serum indicators, and placental growth factor in patients with preeclampsia and their adverse outcome. Altern. Ther. Health Med. 3, AT8329 (2024).
Di Muzio, E. et al. Imatinib binding tohuman serum albumin modulates Heme association andreactivity. Arch. Biochem. Biophys. 560, 100–112 (2014).
Funding
Fund program:Zhejiang Medical and Health Science and Technology Project (2021KY1073)
Author information
Authors and Affiliations
Contributions
CYY designed the study, acquired, analyzed and interpreted data, wrote the manuscript. MJT acquired, analyzed and interpreted data, revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethics approval and consent to participate
The ethics committee of Yuyao People’s Hospital approved the study, and all patients gave written informed consent for participating in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, Y., Ma, J. The construction and validation of a prediction model of hypertensive disease in pregnancy. Sci Rep 15, 13406 (2025). https://doi.org/10.1038/s41598-025-98416-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-98416-y