Abstract
Metabolic-dysfunction associated fatty liver disease (MAFLD) is a widespread chronic liver condition that has been steadily increasing among adolescents and young adults in recent years, posing a major global public health concern. This study aims to conduct an in-depth analysis of the Global Burden of Disease (GBD) 2021 data on MAFLD, focusing on prevalence, incidence, and disability-adjusted life years (DALY) for individuals aged 15–39, spanning the period from 1990 to 2021. This research examines data from the GBD study covering 1990 to 2021 to assess the prevalence, incidence, and DALYs associated with of MAFLD in adolescents and young adults aged 15–39. The analysis is broken down by socioeconomic status, geographic regions, and specific countries. Advanced statistical methods, including the estimated annual percentage change (EAPC) and Bayesian age-period-cohort (BAPC) modeling, were used to deliver the most current and thorough epidemiological assessment of MAFLD in this demographic. In 2021, the estimated global cases of non-alcoholic fatty liver disease among adolescents and young adults reached approximately 423 million, representing a 75.31% increase from 1990. The age-standardized prevalence rate (ASPR) was 14,221.32 cases per 100,000 population, and the age-standardized incidence rate (ASIR) was 977.61 cases per 100,000 population in 2021. Between 1990 and 2021, the ASPR, ASIR, age-standardized DALY rate, and age-standardized mortality rate showed a continuous upward trend, with EAPC of 0.84, 0.79, 0.65, and 0.81, respectively. Regions with Middle and Low-middle Socio-Demographic Index (SDI), as well as High-middle SDI, emerged as “hotspots” for MAFLD prevalence, particularly in North Africa, the Middle East, East Asia, and South Asia. Males exhibited higher prevalence rates compared to females, and the rates continued to increase across all adolescents and young adult age groups. By 2050, the ASPR for MAFLD among this population is projected to reach 16,101 cases per 100,000, signaling an alarming trend. Over the last 30 years, the burden of metabolic-dysfunction associated fatty liver disease has significantly increased among adolescents and young adults worldwide. To counter this rising global health concern, it is crucial to develop and implement targeted and effective interventions tailored to socio-economic settings.
Similar content being viewed by others
Introduction
Metabolic-dysfunction associated fatty liver disease is a common chronic liver disorder characterized by the excessive accumulation of fat in the liver, unrelated to significant alcohol intake. Recently, the term Non-Alcoholic Fatty Liver Disease (NAFLD) has been redefined as Metabolic-Dysfunction Associated Fatty Liver Disease (MAFLD) to better reflect its underlying pathophysiological mechanisms and to establish a more inclusive diagnostic criteria1. Since this disease was first coned in 1987, its global prevalence has surged dramatically, now affecting approximately 25% of the adult population worldwide2,3. The increasing incidence of MAFLD among adolescents and young adults, largely driven by the global obesity epidemic, has become a major public health concern4.
Metabolic-dysfunction associated fatty liver disease, particularly its subtype non-alcoholic steatohepatitis (NASH), can progress to advanced liver disease, cirrhosis, and hepatocellular carcinoma (HCC)5. Studies show that approximately 20% of individuals with MAFLD will develop NASH, and of those with NASH, about 30% may further progress to liver fibrosis. Fibrosis involves the gradual hardening and loss of liver function, potentially leading to cirrhosis, which significantly raises the risk of HCC3,6. As a result, MAFLD is projected to become a leading cause of liver-related morbidity, mortality, and transplantation7,8,9. Recent research has revealed that MAFLD extends beyond liver function, emerging as a multisystem disease that impacts multiple organ systems and a variety of regulatory mechanisms. For instance, MAFLD is linked to an increased likelihood of developing cardiovascular disease (CVD), heart issues, and chronic kidney disease (CKD)10. It is also closely linked with metabolic disorders such as obesity, type 2 diabetes mellitus (T2DM), dyslipidemia, and hypertension11.
MAFLD is often considered a “silent” disease, as it typically presents with few or no symptoms. Consequently, its true prevalence is likely significantly underestimated, as limited biochemical and imaging tests is performed in large populations12. The rising prevalence of MAFLD among adolescents and young adults is driven by unhealthy lifestyle factors, including physical inactivity, poor dietary habits, and the consumption of high-fat, high-sugar foods. In this age group, MAFLD often manifests with subtle early symptoms, significant metabolic risk factors, and a prolonged disease course, all contributing to long-term health risks. To gain a deeper understanding of the epidemiology and public health impact of MAFLD in this population, and to examine variations in prevalence and risk factors across regions and demographic groups, a systematic analysis of global disease burden data is necessary.
Although past research has investigated MAFLD epidemiology at global and regional levels13,14,15,16, including some focused on adolescents17, there is still a lack of comprehensive epidemiological analyses specifically targeting the adolescent population. Additionally, in the post-pandemic era, the long-term health effects of COVID-19 are becoming increasingly significant, with MAFLD emerging as one such concern18. Our analysis utilizes the latest data from the 2021 Global Burden of Disease (GBD) database to comprehensively examine the possible effects of the COVID-19 pandemic on MAFLD rates—an area that prior studies, based on pre-2020 data, could not fully address. Using GBD 2021 data, our study seeks to offer the latest and most comprehensive epidemiological insights into MAFLD among adolescents and young adults. We applied advanced statistical techniques, such as EAPC and BAPC projections, to assess trends over time, explore population characteristics and variations, evaluate associated risk factors, and make future predictions. By integrating this data, we gained insights into how global health crises impact MAFLD prevalence in young populations, thereby providing essential information for developing effective prevention and intervention strategies to mitigate MAFLD’s effect on global health.
Methods
Data acquisition and sources
In this study, data on MAFLD among youths and young adults were sourced from the Global Burden of Disease (GBD) 2021 dataset, which provides a comprehensive assessment of health loss for 371 diseases across 204 countries and territories, encompassing metrics such as prevalence, disease severity, and mortality19. Specifically, data on Total burden related to MAFLD were extracted, including prevalence, incidence, and disability-adjusted life years (DALYs). Our research targets youths and young adults, with the age range of 15–39 years chosen as the population for analysis. The data were accessed and downloaded via the Global Health Data Exchange (GHDx) platform (http://ghdx.healthdata.org/gbd-results-tool). GHDx is the world’s most comprehensive catalog of surveys, censuses, vital statistics, and other health-related data. For gathering the data utilized in the models, the GBD conducts thorough reviews, takes advantage of spontaneous searches, and integrates information supplied by national collaborators and the WHO. Data seeking is iterative and ongoing in process in order to identify new sources20. Moreover, SDI data were used to evaluate the influence of socioeconomic factors on disease burden. Countries and territories were grouped into five SDI strata in the GBD 2021, ranging from low to high development.
Disease definition
To address issues with the former nonalcoholic fatty liver disease (NAFLD) term, APASL was the first society to endorse the MAFLD definition21. The definition of MAFLD requires (1) evidence of hepatic steatosis (HS), confirmed through imaging or histology, and (2) the absence of secondary causes of hepatic fat accumulation, such as significant alcohol consumption, long-term use of steatogenic medications, or monogenic hereditary disorders6. In the ICD-9 classification, MAFLD does not have a distinct code and is generally categorized under 571.8 (Other specified chronic liver disease). However, in ICD-10, MAFLD is coded under K75.8 (Other specified inflammatory liver diseases) and K76.0 (Fatty liver, not elsewhere classified). The GBD categorizes causative factors into four tiers, starting from the most general (Level 1) and narrowing down to the most specific ((Level 1).The total burden related to MAFLD is categorized under the most detailed cause level.
Statistical analysis
We carried out a descriptive study to examine metabolic-dysfunction associated fatty liver disease variations by gender, age brackets (spanning 5-year intervals: 15–19, 20–24, 25–29, 30–34, and 35–39 years), and the Sociodemographic Index(SDI), which was divided into five categories. To examine the global distribution and regional variations in the burden of MAFLD, we created global maps and performed regional comparative analyses. Age-standardized rates(ASR) were calculated using the world standard population defined for the GBD study. All GBD estimates for disease burden are presented with 95% uncertainty intervals (UIs), which represent the range within which the true value of a parameter is expected to fall with 95% probability. These UIs not only capture variability in parameter estimation but also address uncertainties stemming from data collection, model selection, and other factors related to the estimation process22.
To analyze long-term trends in the ASR of MAFLD prevalence, incidence, and disability-adjusted life years (DALYs), we also applied the Estimated Annual Percentage Change (EAPC) method. The EAPC is a widely used metric for quantifying temporal trends in disease burden across various populations. It is derived from fitting a linear regression model to the natural logarithm of ASR over time. The model is expressed as:
where t represents the calendar year, \(\alpha\) is the intercept representing the baseline ASR at the starting year, and \(\beta\) is the slope coefficient indicating the annual change in log-transformed ASR. The EAPC was then calculated using the following formula:
reflecting the estimated annual percentage change in ASR over the study period23. We evaluated long-term trends using the EAPC and its 95% confidence interval (CI), where a positive EAPC indicates an increasing trend in ASR, while a negative EAPC signifies a decreasing trend.
The choice of EAPC is based on its robustness in providing a straightforward interpretation of temporal trends and its compatibility with the GBD framework. EAPC has been extensively applied in previous studies assessing time trends in various diseases24,25. Its simplicity in interpretation and compatibility with ASR-based disease burden estimation make it a preferred method for longitudinal analysis.
We further employed the Bayesian Age-Period-Cohort (BAPC) model to improve trend estimation reliability and capture nonlinear trends. BAPC offers a flexible framework for incorporating age, period, and cohort effects, enhancing precision through shrinkage estimation and providing probabilistic predictions of future trends. This approach is especially beneficial for handling sparse data and making long-term projections compared to conventional regression methods. Recent studies have demonstrated the advantages of BAPC in providing more stable and reliable future projections, including its applications in estimating cancer burden from particulate matter pollution and forecasting infectious disease trends26,27.
All statistical computations and visual representations were carried out using R Studio software (version 4.2.1), employing the BAPC (version 0.0.36), INLA (version 24.05.011), and ggplot2 (version 3.4.2) packages. In each analysis, a two-tailed p-value under 0.05 was deemed indicative of statistical significance.
Risk factors
The risk factor analysis conducted in GBD 2021 utilized a methodology grounded in the comparative risk assessment framework, which is based on a causal network of hierarchically structured, potentially interactive, and modifiable risk factors. For each risk-outcome pair, the relative risk (RR) as a function of exposure, the summary exposure value (SEV), and the theoretical minimum risk exposure level (TMREL) were calculated. These estimates were used to derive the population attributable fraction (PAF), representing the proportional reduction in health risk if exposure were reduced to the TMREL. The attributable burden for each specific risk factor was determined by multiplying the PAF by the disease burden, measured in DALYs28. We selected behavioral and metabolic risk factors closely associated with MAFLD for analysis. In the GBD study, behavioral risk factors include smoking, alcohol consumption, unhealthy diet, physical inactivity, drug use, unsafe sexual practices, and poor breastfeeding habits. While metabolic risk factors included high fasting plasma glucose, high low-density lipoprotein (LDL) cholesterol, high systolic blood pressure, high body mass index but low bone mineral density and impaired kidney function29.We aim to explore the potential associations between these factors and MAFLD.
Prediction
To predict the future burden of MAFLD disease, the future disease burden from 2021 to 2050 was predicted by using the BAPC model integrated nested Laplace approximations. The BAPC model, implemented using the ‘INLA’ and ‘BAPC’ packages in R, allowed us to forecast the incidence and prevalence of the disease through 2050. This model considers the effects of age, period, and cohort, providing a comprehensive approach to understanding future trends in disease burden20,30.
Results
Global level
We noted a marked rise in the burden of MAFLD among global youth and young adults, particularly in the 15–39 age group, from 1990 to 2021 (Table 1, Supplementary Tables S1, S2). By 2021, the estimated prevalence worldwide reached 423,059,626.9 cases (95% UI: 366,558,184.4–494,288,314.5), representing a 75.31% increase from 241,327,584.6 cases (95% UI:208,552,726.3–281,185,672.3) in 1990. Correspondingly, the age-standardized prevalence rate (ASPR) increased to 11,010.48 cases per 100,000 population(95% UI: 9,515.14–12,828.99) in 1990 to 14,221.32 cases per 100,000 population (95% UI: 12,322.00–16,615.70) in 2021. Meanwhile, the number of incident cases surged from 17,053,028.78 in 1990 to 29,082,232.37 in 2021, an increase of 70.54%. The age-standardized incidence rate (ASIR) escalated from 778.04 cases per 100,000 population (95% UI: 670.53–901.83) in 1990 to 977.61 cases per 100,000 population (95% UI: 839.97–1,125.92) in 2021. In 2021, the number of Disability-Adjusted Life Years (DALY) reached 377,553.18 (95% UI: 246,023.87–548,563.02), indicating a significant upward trend compared to 225,363.89 (95% UI: 153,054.61–328,277.70) in 1990.
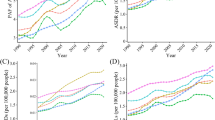
From 1990 to 2021, ASPR, ASIR, and age-standardized DALY rate of MAFLD among global youth and young adults showed a steady increase (Fig. 1). The EAPC for ASPR, ASIR and age-standardized DALY rate were 0.84 (95% CI: 0.78–0.91), 0.79 (95% CI: 0.74–0.84), and 0.65 (95% CI: 0.55–0.75), respectively (Tables 1, Tables S1, S2). Males consistently exhibited higher prevalence rates compared to females (Fig. 1). Nevertheless, both genders experienced a dramatic increase in ASPR, ASIR, and age-standardized DALY rates from 1990 to 2021, underscoring the escalating impact of MAFLD on global youth and young adults, affecting young populations across different genders and regions profoundly.
Temporal trend of age-standardised prevalence rate, age-standardised incidence rate and age-standardised disability adjusted life years (DALY) for the burden of MAFLD, globally and by sociodemographic index (five categories; countries with a high, high-middle, middle, low-middle, or low sociodemographic index) from 1990 to 2021.
SDI regional level
In 2021, the middle SDI and low-middle SDI regions became the “epicenters” of MAFLD burden among youth and young adults, with the largest total case counts. The prevalence and incidence rates in the middle SDI region were 15,515.52 per 100,000 population(95% UI: 13,400.00–18,085.40) and 1,073.67 per 100,000 population(95% UI: 921.65–1,237.27), respectively, while in the low-middle SDI region, the rates were 14,168.98 per 100,000 population (95% UI: 12,265.64–16,434.92) and 1,010.21 per 100,000 population (95% UI: 873.01–1,168.87), placing both regions at the forefront in comparisons among SDI categories (Tables 1 and S1). Additionally, the age-standardized DALY rate in the high-middle SDI region reached the highest level in 2021, at 14.87 per 100,000 population(95% UI: 9.23–22.89), and the ASPR in this region was also high, at 15,505.82 per 100,000 population (95% UI: 13,356.38–18,155.99). From 1990 to 2021, the trend of MAFLD among youth in both global and SDI regions exhibited a gradual increase (Fig. 1). The EAPC for ASPR and ASIR were highest in high SDI regions, reaching 1.320 (95% CI: 1.256–1.384) and 1.12 (95% CI: 1.05–1.20), respectively. The largest increase in age-standardized DALY rates occurred in the high-middle SDI region, with a corresponding EAPC of 2.12 (95% CI: 1.67–2.58).
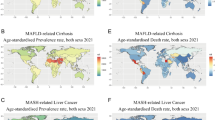
GBD regional level
In 2021, North Africa and the Middle East became the focal point of MAFLD prevalence among adolescents and young adults, with an ASPR of 27,269.21 cases per 100,000 population (95% UI: 23,656.38–31,525.15) and an ASIR of 1,836.44 cases per 100,000 population (95% UI: 1,587.68–2,091.66), significantly surpassing other GBD regions globally. The projected number of cases peaked in South Asia, reaching approximately 100,017,482.1 cases (95% UI: 86,161,773.9–116,387,957.3), while Oceania reported the lowest number of cases at 678,037.07 (95% UI: 584,073.01–792,144.65). In the high-income Asia Pacific region, both the ASPR and ASIR were the lowest, at 9,199.95 cases per 100,000 population (95% UI: 7,893.75–10,728.84) and 543.98 cases per 100,000 population (95% UI: 468.98–627.94), respectively (Table 1 and Supplementary Tables S1).
In the 21 regions analyzed, the prevalence and incidence of MAFLD increased over time across all regions (Fig. 2A and B). Notably, the prevalence rate in North Africa and the Middle East experienced the steepest rise, boasting an estimated annual percentage change (EAPC) of 1.200 (95% CI: 1.144–1.256). Following closely was East Asia, with an EAPC of 1.010 (95% CI: 0.748–1.273). Furthermore, East Asia experienced the most severe increase in incidence, reaching an EAPC of 0.849 (95% CI: 0.598–1.101). The fluctuations in DALY rates varied significantly across regions over time, with Eastern Europe witnessing a rapid surge, yielding an EAPC of 6.859 (95% CI: 5.575–8.158). Central Asia ranked second in this regard, with an EAPC of 2.206 (95% CI: 1.790–2.624). In contrast, several high or upper-middle SDI regions, including Western Europe, High-income Asia Pacific, and East Asia, observed a decline in age-standardized DALY rates over time (Fig. 2; Tables 1 and Supplementary Tables S1, S2).
The change trends and correlation analyses of prevalence rate and SDI from 1990 to 2021. (A) The change trends and correlation of ASPR and SDI from 1990 to 2021 in 21 regions. (B) The change trends and correlation of ASIR and SDI from 1990 to 2021 in 21 regions. (C) The change trends and correlation of age-standardized DALY rate and SDI from 1990 to 2021 in 21 regions. (D) Correlation between age-standardized prevalence rate and SDI in 204 countries in 2021. (E) Correlation between age-standardized incidence rate and SDI in 204 countries in 2021. (F) Correlation between age-standardized DALYs rate and SDI in 204 countries in 2021.
Countries level
In 2021, among the 204 countries analyzed, Qatar had the highest age-standardized prevalence rate (ASPR) for MAFLD, with 37,750.8 cases per 100,000 population(95% UI: 32,195.4–44,266.1). Kuwait and the United Arab Emirates closely trailed, securing the second and third positions, respectively. In stark contrast, Japan had the lowest ASPR at 8,120.7 cases per 100,000 population (95% UI: 7,010.1–9,476.1). Egypt emerged as the country with the highest age-standardized incidence rate (ASIR), recording 2,330.4 cases per 100,000 population(95% UI: 2,041.7–2,653.3). Regarding DALY, Turkmenistan reported the highest age-standardized DALY rate in 2021, reaching 113.4 cases per 100,000 population(95% UI: 61.0–193.7) (Fig. 3, Supplementary Figs. S1, S2).
Global GBD and temporal trends of MAFLD prevalence in 204 countries or territories. (A) The ASR per 100,000 people in 2021. (B) EAPC for MAFLD prevalence. *Maps were generated using R (version 4.3.3; https://www.r-project.org/) and the ‘rnaturalearth’ package (version 1.0.1; https://github.com/ropensci/rnaturalearth), based on vector data from Natural Earth (https://www.naturalearthdata.com/).
From 1990 to 2021, the global prevalence of MAFLD among the youth and young adult population aged 15–39 revealed significant disparities between countries (Fig. 2D). The prevalence of MAFLD in Iran (Islamic Republic of) demonstrated the most pronounced increase during this period (EAPC: 1.720; 95% CI: 1.120–2.323). In contrast, Timor-Leste exhibited the most significant decline from 1990 to 2021 (EAPC: – 0.150; 95% CI: – 0.229 to – 0.072). Regarding the incidence of MAFLD, Equatorial Guinea exhibited the steepest increase from 1990 to 2021, with an EAPC of 1.608 (95% CI: 1.517–1.699), while Japan saw the steepest drop in the incidence of MAFLD (EAPC: − 0.010; 95% CI: − 0.143 to 0.124). In contrast, the Russian Federation reported the most pronounced rise in age-standardized DALY rates (EAPC: 7.668; 95% CI: 6.282 to 9.073). Furthermore, we measured the relative changes between 1990 and 2021 across the global and various countries using percentage change (PC) (Supplementary Fig. S3), finding that the leading countries align closely with the results of the EAPC.
Age and sex patterns
In 2021, the global prevalence of MAFLD showed clear patterns related to age and gender (Fig. 4). Among individuals aged 15 to 39, the number of cases in males consistently surpassed that in females, with prevalence increasing with age and peaking in the 35–39 age group. Notably, the incidence of MAFLD exhibited a downward trend with increasing age, with the highest peak occurring in the youngest group, 15–19 years, where males consistently outnumbered females, showing a greater gender disparity as age decreased. In terms of DALY and mortality, both indicators exhibited rapid increases with advancing age. In the younger age groups (15–19 and 20–24 years), females slightly surpassed males, but as age increased, the disease burden borne by males became significantly greater than that of females, with this disparity widening further with age. Compared to the situation in 1990, the distribution of the disease by gender and age has not changed significantly, but the number of cases has exhibited a spiral increase. Additionally, country-level age- and sex-specific incidence rates of MAFLD in 1990 and 2021 are provided in Supplementary Tables S6, highlighting variations across 204 nations.
Attributable risk factors
The increasingly severe burden of MAFLD has prompted us to investigate the disease’s risk factors. High fasting blood glucose and tobacco use have been identified as the primary behavioral and metabolic risk factors associated with MAFLD, with the percentages of DALY and mortality represented as outcomes of the disease (Fig. 5). From 1990 to 2021, the proportion of DALY and mortality attributed to high fasting blood glucose significantly increased globally and across various regions, particularly in low-middle and high SDI areas. In contrast, the impact of tobacco remained relatively stable overall. While there was an increase in low SDI and middle-low SDI regions, the growth trend was more gradual, and high SDI regions exhibited stability or a slight decrease.
Risk attribution factors for MAFLD. (A) Trends in the Proportion of MAFLD DALYs attributable to Tobacco and High Fasting Plasma Glucose, Globally and in 5 SDI Regions, from 1990 to 2021. (B) Proportion of MAFLD DALY attributable to tobacco and high fasting plasma glucose for 21 GBD regions, 2021. (C) Trends in the Proportion of MAFLD Deaths attributable to Tobacco and High Fasting Plasma Glucose, Globally and in 5 SDI Regions, from 1990 to 2021. (D) Proportion of MAFLD Deaths attributable to tobacco and high fasting plasma glucose for 21 GBD regions, 2021.
The analysis of results across 21 GBD regions indicates significant regional variations in the impacts of high fasting blood glucose and tobacco on MAFLD (Fig. 5B and D). In terms of high fasting blood glucose, the region with the highest DALY percentage in 2021 was Southern Sub-Saharan Africa [0.23 (0.02, 0.5)], followed by East Asia [0.20 (0.02, 0.45)] and Western Sub-Saharan Africa [0.15 (0.01, 0.35)]. These three regions also exhibited the highest proportions of total mortality in 2021. Regarding tobacco use, its influence on MAFLD was particularly pronounced in Southern Sub-Saharan Africa, East Asia, and Southeast Asia, with DALY percentages of 0.26 (0.08, 0.5), 0.26 (0.08, 0.49), and 0.15 (0.05, 0.31), respectively. In 2021, Southern Sub-Saharan Africa and East Asia bore the brunt of the impact from smoking and elevated fasting blood sugar levels.
Future burden of MAFLD
Figure 6 illustrates the projected future trends in MAFLD prevalence, incidence, DALY, and mortality rates for males and females globally. The data indicate that the burden of MAFLD among young populations is expected to rise steadily in the coming years. By 2050, the global age-standardized prevalence rate (ASPR) of MAFLD is anticipated to reach 16,101 cases per 100,000 population (95% UI: 11,640–20,562). Males are projected to have a higher prevalence than females, with an estimated 17,046 cases per 100,000 population (95% UI: 12,120–21,971). The age-standardized incidence rate (ASIR) is also expected to show continuous growth, reaching 1,170 cases per 100,000 population globally by 2050 (95% UI: 754–1,585), with males significantly exceeding females. Furthermore, by 2050, the ASR for global MAFLD is projected to reach 13.4 cases per 100,000 population (95% UI: 8.1–18.8), showing a slight decline for males (12.3 cases per 100,000; 95% UI: 6.9–17.8) while females exhibit an upward trend (13.7 cases per 100,000; 95% UI: 8.3–19.2).
According to projected population changes, by 2030, an estimated 458 million individuals (95% UI: 440–476) globally will be affected by MAFLD, increasing to 521 million (95% UI: 371–666) by 2050. This represents an approximate increase of 13.8% in total cases compared to 2030. From 2030 to 2050, the expected number of cases in males is projected to rise from 249 million (95% UI: 238–261) to 284 million (95% UI: 202–366), while the expected number of cases in females will increase from 209 million (95% UI: 200–218) to 240 million (95% UI: 173–306). Notably, the projected trends exhibit significant regional disparities; for instance, regions such as Andean Latin America, East Asia, South Asia, Tropical Latin America, and Southern Latin America are expected to see marked increases, whereas growth in regions such as High-income Asia Pacific, Central Europe, and Eastern Europe may be more modest or stabilize (Table 2). Furthermore, our analysis extends to country-level projections across 204 nations, providing a more detailed perspective on the future burden of MAFLD at the national level. These projections reveal substantial heterogeneity in MAFLD burden, with certain countries experiencing more pronounced increases, while others exhibit relatively stable trends (Supplementary Tables S7).
Discussion
Principal findings
Metabolic-Dysfunction Associated Fatty Liver Disease (MAFLD) is a significant and growing public health concern, with a marked increase in prevalence among adolescents from 1990 to 2021, according to the 2021 Global Burden of Disease (GBD) data. The burden is particularly high in countries with medium, upper-middle, and lower-middle socio-demographic indices (SDI), with males being more susceptible than females. Tobacco use and elevated fasting blood glucose are identified as significant risk factors. Bayesian Age-Period-Cohort predictions suggest a continued rise in MAFLD cases through 2050, highlighting the need for global intervention2,28.
Trends in MAFLD development parallel to obesity progression
MAFLD development is closely linked to obesity, with an estimated prevalence of 30% to 37% among obese individuals. Abdominal obesity and increased visceral adipose tissue (VAT) are particularly associated with MAFLD, while subcutaneous adipose tissue (SAT) is correlated with MAFLD regression31. Weight loss has been shown to improve MAFLD outcomes, emphasizing the importance of effective weight management32,33,34.
Regional differences in the burden of MAFLD
The burden of MAFLD varies across SDI categories, with the highest prevalence in middle SDI regions, followed by high-middle and low-middle SDI regions. North Africa, the Middle East, and East Asia are identified as hotspots for MAFLD prevalence, likely due to rising obesity rates and lifestyle changes13,35. Urbanization and dietary shifts towards high-calorie, high-sugar, and high-fat foods contribute to the increasing prevalence of MAFLD in these regions36,37,39.
Interethnic differences and genetic predisposition
Genetic variants near the TM6SF2, PNPLA3, NCAN, and PPP1R3B genes contribute to MAFLD susceptibility, with the PNPLA3 I148M variant being most prevalent among Hispanic populations (49%) and least common among African Americans (17%)40,41,42. Lean MAFLD cases in Asia are associated with the PNPLA3 rs738409 GG allele, highlighting the role of genetics in disease expression43,44,45.
Health system and policy implications
Countries with middle and low-middle SDI levels lag in universal health coverage for non-communicable diseases, necessitating targeted policies and resource allocation for disease prevention and management46,47. High SDI regions, despite lower prevalence, show significant annual increases in MAFLD cases, underscoring the need for robust health education and policy measures46.
Sex and age disparities in the burden of MAFLD
Males aged 15–39 are more likely to develop MAFLD than females, with tobacco use identified as a significant risk factor48. The highest prevalence is observed in the 35–39 age group, but an alarming trend of increased incidence is seen in younger cohorts (under 30 years), highlighting the need for focused interventions in this age group49.
Limitations of the study
Our analysis, based on the 2021 GBD data, focused on adolescents and young adults, potentially underestimating the overall impact of MAFLD. Regional data quality varied, and only two risk factors were considered, limiting the comprehensive understanding of MAFLD’s multifactorial nature.
Conclusion
MAFLD is an escalating global health concern, particularly in middle SDI countries and regions like North Africa, the Middle East, and East Asia. Targeted interventions, improved public health measures, and enhanced data accuracy are essential to address this growing issue effectively.
Data availability
The datasets generated during the current study are available in the Global Health Data Exchange query tool (https://vizhub.healthdata.org/gbd-results).
References
Eslam, M. et al. The Asian Pacific association for the study of the liver clinical practice guidelines for the diagnosis and management of metabolic dysfunction-associated fatty liver disease. Hepatol. Int. 2025, 56 (2025).
Le, M. H. et al. 2019 global NAFLD prevalence: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 20(12), 2809–17.e28 (2022).
Younossi, Z. M. et al. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64(1), 73–84 (2016).
Li, J. et al. Meta-analysis: global prevalence, trend and forecasting of non-alcoholic fatty liver disease in children and adolescents, 2000–2021. Aliment Pharmacol. Ther. 56(3), 396–406 (2022).
Anstee, Q. M., Targher, G. & Day, C. P. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat. Rev. Gastroenterol. Hepatol. 10(6), 330–344 (2013).
Chalasani, N. et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology 67(1), 328–357 (2018).
Estes, C. et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J. Hepatol. 69(4), 896–904 (2018).
Estes, C., Razavi, H., Loomba, R., Younossi, Z. & Sanyal, A. J. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology 67(1), 123–133 (2018).
Younossi, Z. M. et al. Nonalcoholic steatohepatitis is the most rapidly increasing indication for liver transplantation in the United States. Clin. Gastroenterol. Hepatol. 19(3), 580–9.e5 (2021).
Byrne, C. D. & Targher, G. NAFLD: a multisystem disease. J. Hepatol. 62(1 Suppl), S47-64 (2015).
Cotter, T. G. & Rinella, M. Nonalcoholic fatty liver disease 2020: the state of the disease. Gastroenterology 158(7), 1851–1864 (2020).
Long, L. & Zhou, X. Defining severe NAFLD based on ICD codes in large cohorts: balancing feasibility and limitations. J. Hepatol. 79(6), e232–e233 (2023).
Chen, H. et al. The global, regional, and national burden and trends of NAFLD in 204 countries and territories: an analysis from global burden of disease 2019. JMIR Public Health Surveill. 8(12), e34809 (2022).
Golabi, P. et al. Burden of non-alcoholic fatty liver disease in Asia, the Middle East and North Africa: data from Global Burden of Disease 2009–2019. J. Hepatol. 75(4), 795–809 (2021).
Liu, Z. P. et al. Global burden of cirrhosis and other chronic liver diseases due to nonalcoholic fatty liver disease, 1990–2019. World J. Hepatol. 15(11), 1210–1225 (2023).
Paik, J. M. et al. The burden of nonalcoholic fatty liver disease (NAFLD) is rapidly growing in every region of the world from 1990 to 2019. Hepatol. Commun. 7, 10 (2023).
Paik, J. M. et al. Global burden of NAFLD and chronic liver disease among adolescents and young adults. Hepatology 75(5), 1204–1217 (2022).
Ma, Y. et al. Risks of digestive diseases in long COVID: evidence from a population-based cohort study. BMC Med. 22(1), 14 (2024).
Steinmetz, J. D. et al. Global, regional, and national burden of disorders affecting the nervous system, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 23(4), 344–381 (2024).
Chen, Y. et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 402(10397), 203–234 (2023).
Eslam, M., Sanyal, A. J. & George, J. Toward more accurate nomenclature for fatty liver diseases. Gastroenterology 157(3), 590–593 (2019).
Naghavi, M. et al. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403(10440), 2100–2132 (2024).
Chen, Z. F. et al. Global, regional, and national burden and trends of migraine among youths and young adults aged 15–39 years from 1990 to 2021: findings from the global burden of disease study 2021. J. Headache Pain. 25(1), 131 (2024).
Murray, C. J. et al. Five insights from the Global Burden of Disease Study 2019. Lancet 396(10258), 1135–1159 (2020).
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
Chen, J. et al. Global, regional, and national burden of cancers attributable to particulate matter pollution from 1990 to 2019 and projection to 2050: Worsening or improving?. J. Hazard Mater. 477, 135319 (2024).
Huang, D. et al. Global temporal trends and projections of acute hepatitis E incidence among women of childbearing age: age-period-cohort analysis 2021. J. Infect. 89(4), 106250 (2024).
Brauer, M. et al. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403(10440), 2162–2203 (2024).
Stanaway, J. D. et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159), 1923–1994 (2018).
Li, J., Jia, H., Liu, Z. & Xu, K. Global, regional and national trends in the burden of low bone mineral density from 1990 to 2030: a Bayesian age-period-cohort modeling study. Bone 189, 117253 (2024).
Younossi, Z. et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 15(1), 11–20 (2018).
Farrell, G. C. The liver and the waistline: fifty years of growth. J. Gastroenterol. Hepatol. 24(Suppl 3), S105–S118 (2009).
Gao, X. et al. Impact of the COVID-19 pandemic on liver disease-related mortality rates in the United States. J. Hepatol. 78(1), 16–27 (2023).
Kim, D. et al. Changing trends in etiology-based annual mortality from chronic liver disease, from 2007 through 2016. Gastroenterology 155(4), 1154–63.e3 (2018).
Cai, J., Zhang, X. J. & Li, H. Progress and challenges in the prevention and control of nonalcoholic fatty liver disease. Med. Res. Rev. 39(1), 328–348 (2019).
El-Serag, H. B., Tran, T. & Everhart, J. E. Diabetes increases the risk of chronic liver disease and hepatocellular carcinoma. Gastroenterology 126(2), 460–468 (2004).
Tanase, D. M. et al. The Intricate Relationship between Type 2 Diabetes Mellitus (T2DM), Insulin Resistance (IR), and Nonalcoholic Fatty Liver Disease (NAFLD). J. Diabetes Res. 2020, 3920196 (2020).
Barquera, S. et al. Energy intake from beverages is increasing among Mexican adolescents and adults. J. Nutr. 138(12), 2454–2461 (2008).
Wang, L. et al. Trends in consumption of ultraprocessed foods among US youths aged 2–19 years, 1999–2018. JAMA 326(6), 519–530 (2021).
Fahed, A. C., El-Hage-Sleiman, A. K., Farhat, T. I. & Nemer, G. M. Diet, genetics, and disease: a focus on the middle East and north Africa region. J. Nutr. Metab. 2012, 109037 (2012).
Fan, J. G., Kim, S. U. & Wong, V. W. New trends on obesity and NAFLD in Asia. J. Hepatol. 67(4), 862–873 (2017).
Guerrero, R., Vega, G. L., Grundy, S. M. & Browning, J. D. Ethnic differences in hepatic steatosis: an insulin resistance paradox?. Hepatology 49(3), 791–801 (2009).
Brouwers, M. C., van Greevenbroek, M. M. & Cantor, R. M. Heritability of nonalcoholic fatty liver disease. Gastroenterology 137(4), 1536 (2009).
Chen, L. Z. et al. PNPLA3 I148M variant in nonalcoholic fatty liver disease: demographic and ethnic characteristics and the role of the variant in nonalcoholic fatty liver fibrosis. World J. Gastroenterol. 21(3), 794–802 (2015).
Sookoian, S. & Pirola, C. J. Meta-analysis of the influence of I148M variant of patatin-like phospholipase domain containing 3 gene (PNPLA3) on the susceptibility and histological severity of nonalcoholic fatty liver disease. Hepatology 53(6), 1883–1894 (2011).
Chan, W. K. et al. Clinical features and treatment of nonalcoholic fatty liver disease across the Asia Pacific region-the GO ASIA initiative. Aliment Pharmacol. Ther. 47(6), 816–825 (2018).
Lozano, R. et al. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258), 1250–1284 (2020).
Hu, X. et al. Prevalence and factors associated with nonalcoholic fatty liver disease in Shanghai work-units. BMC Gastroenterol. 12, 123 (2012).
Caballería, L. et al. Prevalence and factors associated with the presence of nonalcoholic fatty liver disease in an adult population in Spain. Eur. J. Gastroenterol. Hepatol. 22(1), 24–32 (2010).
Funding
This study was supported by the Key Project of Science and Technology Program of Jiangxi Provincial Department of Education (No. GJJ210130), the Technology Program of Jiangxi Provincial Health Commission (No. 202410021), the Humanities and Social Sciences Program of Jiangxi Province Colleges and universities (No.GL162033), and the Medical Ideological and Political Program of The First Affiliated Hospital of Nanchang University (No. NDYFY_SZ2023029).
Author information
Authors and Affiliations
Contributions
RSY and HLY conceptualized and designed the research; RSY and HLY collected and analyzed the data; HLY wrote and revised the manuscript; FGQ and LYA critically revised the manuscript for important intellectual content. RSY, HLY, SJ, YZS, SWP, ZFK, FC, XJ, DGH, LYA and FGQ jointly supervised the study. All authors actively contributed to the writing of the manuscript and approved the final submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ruan, S., Huang, L., Song, J. et al. Global burden trends and forecasts for MAFLD in adolescents and young adults from 1990 to 2021. Sci Rep 15, 13534 (2025). https://doi.org/10.1038/s41598-025-98489-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-98489-9