Abstract
The most important risk factor in ischaemic stroke patients is hypertension (HT). Blood pressure regulation has an important role in hypertensive acute ischaemic stroke patients (AIS). In this study, we planned to compare the efficacy of nicardipine and esmolol infusion on blood pressure control and clinical outcome in hypertensive AIS patients. The study is a retrospective, cross-sectional study. It includes hypertensive AIS patients admitted to the emergency department. Target blood pressure, time to reach target blood pressure, discharge modified Rankin Scale (mRS), intracranial haemorrhage according to The European Cooperative Acute Stroke Study (ECASS II) and 30-day mortality of patients who were started Nicardipine or Esmolol within the indication were determined and mortality and morbidity of the two groups were compared. The study included 82 acute ischaemic stroke patients who were hypertensive at presentation. The mean age of the patients was 72 years (39–93). No difference was observed between the Nicardipine (n = 40) and Esmolol (n = 42) groups in terms of sociodemographic data, vital functions and clinical status (National Institutes of Health Stroke Scale - NIHSS) at admission. The target blood pressure levels were reached faster and more effectively in the Nicardipine group than in the Esmolol group (p < 0.001). No difference was observed between the two groups in terms of mRS, ECASS II scores and 30-day mortality. Nicardipine is more effective than Esmolol in blood pressure control in AIS patients who are candidates for invasive procedures such as thrombolysis and thrombectomy. The fact that there is no difference in mortality and morbidity between the two drugs suggests that Esmolol can also be used in selected patients.
Similar content being viewed by others
Introduction
Although the prevalence and mortality rate of stroke have decreased in recent years due to improved diagnostic and therapeutic methods, stroke remains one of the main causes of death and disability in adults1. Stroke is a clinical syndrome that causes sudden, focal or global impairment of the central nervous system due to vascular causes. Ischemic stroke is responsible for 70–85% of all stroke cases. Stroke is the second leading cause of death in the world after ischemic heart disease. More than 13 million new stroke cases are observed every year2,3.
Hemodynamic disturbances are common in acute stroke and management of blood pressure, particularly the acute hypertensive response that accompanies most stroke presentations, is often seen as a target for early intervention. Current resources available to guide emergency physicians on the optimal approach to high blood pressure in acute stroke are limited but evolving4.
The consensus is that blood pressure should only be lowered if the systolic pressure exceeds 220 mm Hg or the diastolic pressure exceeds 120 mm Hg. However, systolic blood pressure (SBP) greater than 185 mm Hg or diastolic blood pressure (DBP) greater than 110 mm Hg is a contraindication to the use of thrombolytics. Therefore, treatment of high blood pressure in acute ischemic stroke may vary depending on whether the patient is a candidate for invasive treatment such as thrombolytics or thrombectomy5.
There is currently no consensus on the best agents for lowering blood pressure in ischemic stroke. However, some principles should be considered in their selection. First, short-acting, titratable antihypertensives are most appropriate in the emergency department setting. Second, rapidly acting agents that maintain stable cerebral blood flow are preferred. Many agents have been clinically studied for blood pressure regulation in acute ischemic stroke. In the light of these studies, fast-acting, rapid reversal agents are recommended. Oral agents are not recommended due to the associated risk of aspiration and slow onset of effects. Recommended treatments include labetalol, nicardipine, clevidipine and sodium nitroprusside6. Since esmolol is a short and fast-acting beta1 selective blocker, it is one of the agents that can be used IV (intravenously) in patients with acute ischemic stroke when indicated.
In our emergency department, the two drug groups that meet these characteristics and are frequently used are beta antogonists (Esmolol) and calcium channel blockers (Nicardipine). Esmolol is the shortest-acting cardioselective beta 1 adrenergic receptor blocker. It is administered as a continuous infusion titrated after a loading dose (Loading: 0.25–0.5 mg/kg IVP 1 min, Infusion: 0.05–0.3 mg/kg/minute IV). Nicardipine is a second generation dihydropyridine calcium antagonist that selectively inhibits vascular smooth muscle contraction. There is no loading dose and it is administered as a continuous infusion by titration (5 mg/h IV infusion, increasing by 2.5 mg/h every 5–10 min). Although the duration of action of both drug groups is short, their mechanisms of action are different.
There are no studies in the literature comparing these two drugs in hypertensive acute ischemic stroke patients. In this study, we aimed to retrospectively investigate the effects of these two drugs on prognosis in ischemic stroke patients who were started for hypertension control within the indication.
Materials and methods
Type and ethical aspects of the research
Our study is a retrospective study in which hypertensive patients diagnosed with acute ischemic stroke admitted to the emergency department of the University of Health Sciences Sisli Hamidiye Etfal Training and Research Hospital were examined. The approval of the University of Health Sciences Şişli Hamidiye Etfal Training and Research Hospital Health Practice and Research Center Clinical Research Ethics Committee dated 24/10/2023 and decision number 4137 was obtained.
Research sample and population
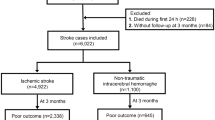
This study includes hypertensive acute ischemic stroke patients admitted to the emergency department of Health Sciences University Şişli Hamidiye Etfal Training and Research Hospital between January 01, 2020 and October 01, 2023. It includes the group of patients who received esmolol or nicardipine treatment protocols for blood pressure control, followed by thrombectomy and thrombolytic (IV alteplase) treatment, and whose follow-up treatment was complete in the data recording system. 448 hypertensive AIS patients were evaluated for eligibility. The study included 82 patients receiving only Nicardipine (n = 40) or only Esmolol (n = 42) for blood pressure regulation (Fig. 1). This number was obtained randomly after exclusion criteria and no bias was applied. Only these drug infusions were given in the treatment of malignant hypertension before-after invasive procedures.
Drugs used and dosage
Hypertensive emergencies require immediate reduction of blood pressure with intravenous (i.v.) drug therapy. Two of the antihypertensive agents recommended by the Turkish Neurology Association in the Acute Ischemic Stroke Diagnosis and Treatment Guidelines, as well as in other countries, are Esmolol and Nicardipine. Esmolol (0.5-1 mg/kg as i.v. bolus; 50–300 mcg/kg/min as i.v. infusion) can be started if patients do not have pathologies such as second or third-degree AV block, systolic heart failure, asthma, bradycardia7,8. Nicardipine infusion (5 mg/h IV infusion, increasing by 2.5 mg/h every 5–10 min) is indicated in hypertensive (SBP > 185 mm Hg or DBP > 110 mm Hg) acute ischaemic stroke patients with indication for thrombolytic therapy. Contraindicated in liver failure7,8,9.
In hypertensive acute stroke patients, antihypertensive agents are initiated to achieve a 15% reduction in blood pressure within one hour. The target blood pressure for treatment with antihypertensive agents in patients who are candidates for invasive treatment in our emergency department is SBP < 185 mm Hg DBP < 105 mm Hg. When the pressure drops below these values, invasive treatments are initiated and deeper blood pressure drops (SBP < 140 mm/hg) are prevented because cerebral perfusion will be impaired. Antihypertensive agents are titrated according to pressure changes and stopped if necessary8,9.
Data collection
Patient Information Management System (PANATES) of Health Sciences University, Şişli Hamidiye Etfal Training and Research Hospital was used for data collection. Demographic characteristics of the patients such as age and gender, complaints at emergency room admission, duration of emergency room admission after the onset of symptoms, vital parameters such as systolic blood pressure, diastolic blood pressure, pulse rate, respiratory rate, oxygen saturation, history of previous or known chronic diseases, time taken for thrombolytics after blood pressure regulation, and follow-up treatment processes after hospitalization were accessed from the electronic files of the patients. The National Institutes of Health Stroke Scale (NIHSS) was used to measure stroke severity at admission10. The classification in the Second European-Australasian Acute Stroke Study (ECASS II) was used to define intracranial hemorrhagic transformation by Cranial CT at 24 h after thrombolytic and thrombectomy11. The modified Rankin Scale (mRS) was used to classify the mortality-morbidity of patients after treatment12.
Statistical analysis
Mean, standard deviation, median, percentile (25–75) minimum, maximum, frequency and ratio values were used in descriptive statistics of the data. The distribution of variables was measured with the Kolmogorov Simirnov test. Independent sample t test, mann-whitney u test were used to analyze quantitative independent data. Chi-square test was used in the analysis of qualitative independent data and Fisher’s exact test was used when chi-square test conditions were not met. p < 0.05 was considered statistically significant. SPSS 28.0 program was used in the analysis.
Findings
The study included 82 ischemic stroke patients who were hypertensive (systolic BP > 184 mm Hg, diastolic BP > 110 mm Hg) at presentation. The mean age of the patients was 72 years (39–93). The number of men and women was equal (n = 41). All patients received thrombolytics and thrombectomy. Patients were divided into two groups as nicardipine (n = 40) and esmolol (n = 42) treatment groups for blood pressure regulation before lytic and thrombectomy procedures. There was no difference in sociodemographic data between the two groups. The history of HT was higher in the nicardipine group compared to the esmolol group and there was a statistical difference (Table 1).
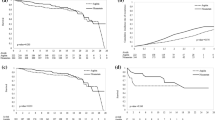
We evaluated the two groups in terms of vital functions and clinical status at the time of emergency admission. In the Nicardipine group, the last systolic and diastolic blood pressures measured before thrombolytic therapy and the time taken for blood pressure regulation were lower and statistically significant than Esmolol group (p < 0.001) (Fig. 2). Pulse rate was higher in the Esmolol group compared to the other group, and the time between symptom onset and presentation to the emergency department was longer. Although the mortality rate was higher in the group started on nicardipine, there was no statistical difference (Table 2). Among patients on medication for hypertension, blood pressure control was achieved faster in the Nicardipine group (n = 37) than in the Esmolol group (n = 30) (p < 0.001) (not shown on the table).
We compared the groups in terms of hematologic parameters. Hgb and Hct levels were higher in the group receiving esmolol. MPV, HCO3, BE, Urea, Glucose and Triglyceride levels were higher and statistically significant in the group receiving Nicardipine (Table 3).
There was no statistical difference between the two groups in terms of intracranial haemorrhage 24 h after the procedure. Bleeding after thrombectomy and thrombolysis was observed in 14 patients in the group receiving nicardipine and in 12 patients in the group receiving esmolol (Table 4).
Discussion
We found no difference in mortality and morbidity in the two drug groups we used as infusion for blood pressure regulation in hypertensive acute ischemic patients. We found that Nicardipine showed faster efficacy in blood pressure regulation than Esmolol. There was no difference in clinical outcome between the groups treated with Nicardipine or Esmolol in blood pressure control of hypertensive acute ischaemic stroke patients.
Hypertension is one of the most important risk factors in acute ischemic stroke patients and is one of the most frequently detected metabolic disorders in this patient group presenting to the emergency department. Although controversy continues about blood pressure management in acute stroke patients, impaired brain perfusion due to sudden drop in blood pressure in ischemic stroke patients may worsen the ischemic condition. However, there is a consensus on blood pressure control before invasive procedures such as thrombectemy and thrombolytics13. In our study, we found that there was a greater decrease in blood pressure in the Nicardipine group compared to the Esmolol group. In the patient group receiving Nicardipine infusion, the mean systolic blood pressure was found to be 157 mmhg, which is above the normohypotensive values that may cause impaired brain perfusion.
Time is very important especially in the treatment of patients who are thrombolytic candidates, because failure to control blood pressure smoothly and rapidly may eliminate the opportunity for thrombectomy or thrombolytic administration14. We noted faster blood pressure control in the group in which we started Nicardipine infusion as a superiority of Nicardipine over Esmolol. One of the most important contraindications for thrombolytics is a duration of more than 4.5 h between the onset of symptoms and initiation of treatment. This period is 6 h in thrombectomy candidates and may extend up to 24 h in some patients15. The time between the onset of symptoms and presentation to the emergency department may decrease the time required to start thrombolytic treatment. In this limited time, Nicardipine infusion should be started to rapidly regulate blood pressure in patients presenting with high blood pressure that is contraindicated for thrombolytic therapy.
In addition to arterial thrombosis, many secondary metabolic disorders can be seen in acute ischemic stroke. Hypertension, hypotension, hyperglycemia, hypoxia are some of the common abnormal clinical conditions. In addition to being one of the most important risk factors of ischemic stroke, HT may also have an impact on the functional outcomes of patients. Ischemic stroke is a consequence of a variety of pathological conditions arising from systemic cardiovascular disease or primary cerebrovascular disease, the vast majority of which are thought to be related to hypertension. Therefore, the majority of AIS is a consequence of chronic hypertension (HT)15. In our study, hypertension was found to be the most common risk factor in accordance with the literature. In addition, a history of chronic hypertension was recorded more frequently in the group started on nicardipine, but other risk factors did not differ between the groups. We found that blood pressure regulation was faster in this group compared to the Esmolol group. However, it remains unclear whether different blood pressure management strategies are necessary in acute ischemic stroke patients with a history of hypertension before stroke onset15.
In a study conducted for the control of hypertension occurring after craniotomy, Nicardipine and Esmolol were compared and it was found that Niacardipine was more effective in blood pressure control16. In other studies, conducted outside acute ischemic stroke, Nicardipine was found to be more effective than Esmolol in blood pressure control17,18. In our study, we found that Nicardipine was faster and more effective than Esmolol in blood pressure control in acute ischemic stroke patients.
Nicardipine is a second class dihydropyridine (DHP) group calcium channel blocker. It has high specificity for L-type calcium channels (LTCCs). It shows activity through the ɑ1 subunit found in vascular smooth muscle cells and cardiomyocytes19. Esmolol is a selective Beta-1 receptor blocker. Beta-1 receptors are primarily found in cardiac nodal tissue, cardiac myocytes, other cardiac conduction pathway tissues and kidneys. Esmolol shows its effect by selectively binding to beta-1 receptor sites and inhibiting the effects of epinephrine and norepinephrine on these sites20,21. The fact that Nicardipine is faster and more effective than Esmolol in blood pressure control may be related with its multiple effects.
Although Nicardipine was more effective than Esmolol in blood pressure control in ischemic stroke patients, we found no difference between the two groups in terms of intracranial bleeding after invasive procedures, length of stay, discharge mRS and mortality. In hypertensive ischemic stroke patients, current guidelines suggest that patients eligible for intravenous thrombolysis should have their blood pressure carefully lowered to systolic blood pressure < 185 mmHg and diastolic blood pressure < 110 mmHg before initiation of IVT and controlled to < 180/105 mmHg within the first 24 h after treatment. It is emphasized that blood pressure reduction should be careful and individualized, as an exaggerated drop in blood pressure can lead to complications such as stroke progression or acute kidney injury. To date, no blood pressure reduction strategy has been shown to be superior6,22. The fact that there was no difference between the two groups we compared in terms of sociodemographic, vital parameters and clinical status at presentation standardized the two groups. The fact that Nicardipine did not differ from Esmolol in terms of clinical outcome between the two groups is evidence that Esmolol is also a preferable antihypertensive agent in patients with acute ischemic stroke. We think that this situation is due to the pre-infusion loading dose in the treatment protocol.
A review article by Bath et al. indicated that the use of beta-blockers for blood pressure regulation in patients with AIS may be harmful. They based this conclusion on the BEST (β-Blocker Stroke Trial) study, which suggested that reduced cardiac output may impair cerebral perfusion. The drugs tested in this study were atenolol and propranolol. The half-life of these drugs (6–7 h) is much longer than the half-life of Esmolol, which was limited to minutes, used in our study23. In our study, blood pressure reduction was slower in the group receiving Esmolol than in the group receiving Nicardipine, but the outcomes in the two groups were similar. Esmolol’s rapid onset of action, rapid clearance from the kidneys, and a half-life measured in minutes when stopped (9 min) differentiate it positively from long-acting beta-blocker drugs and explain successful results similar to Nicardipine. In the same review, Bath et al. cited the results of the ATACH-2 (Antihypertensive Treatment of Acute Cerebral Hemorrhage-2) study and stated that intravenous calcium channel blockers (nicardipine or nimodipine) may be neuroprotective in patients with ischemic stroke and intracerebral hemorrhage, but are neutral in terms of clinical outcome23. In our study that included only AIS patients, we found that the blood pressure of patients receiving nicardipine infusion was regulated faster, and there was no difference in terms of clinical outcome compared to the group receiving esmolol.
In our small sample size study, we can say that the patient group in which we used Nicardipine was superior to the group in which we used Esmolol in controlling hypertensive AIS patients rapidly and effectively. In addition, the final blood pressure levels lowered for thrombolytic initiation in the group in which we used Nicardipine were determined to be above the values warned for brain perfusion disorder in the literature.
Limitations
The single center, retrospective and small number of patients are some of the important limitations of our study. Primarily the retrospective design and relatively low sample size may have introduced selection bias, and limit the generalizability of the findings. Apart from these, only the time until the target blood pressure was achieved and the target blood pressures of both drug groups were compared. Patients with a history of hypertension were excluded if they were taking antihypertensive agents before presentation to the emergency department. Since the times in the follow-up charts for target blood pressure could not be standardized, only the times when they were controlled could be included in the study.
Conclusion
We would like to state that there was no difference between the two drugs in terms of clinical outcomes in acute ischemic stroke patients. Esmolol is an agent that can be used for blood pressure control in hypertensive acute ischemic stroke patients admitted to the emergency department. In patients who are candidates for invasive procedures such as thrombolytics and thrombectomy, starting Nicardipine may provide an advantage over Esmolol, considering the time limitations. However, it should be kept in mind that Nicardipine may worsen ischemia by impairing cerebral perfusion due to its greater blood pressure lowering effect and by reducing pneumbra nutrition. Since Nicardipine has different side effects such as reflex tachycardia and Esmolol has different side effects such as bradycardia, it is useful to individualize hypertension treatment in stroke patients. The findings need to be supported by randomized controlled, large-scale studies.
Data availability
The datasets used and/or analyzed during the current study are available for sharing by the corresponding author upon request.
References
Global Burden of Disease Collaborators. Global, regional, and National burden of stroke, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 18, 439–458. https://doi.org/10.1016/S1474-4422(19)30034-1 (2019).
Bill, F. & Foundation, M. G. Global, regional, and National burden of stroke, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 18, 439–458. https://doi.org/10.1016/S1474-4422(19)30034-1 (2016).
Feigin, V. L., Norrving, B. & Mensah, G. A. Global burden of stroke. Circ. Res. 120, 439–448. https://doi.org/10.1161/CIRCRESAHA.116.308413 (2017).
Stead, L. G. et al. The impact of blood pressure hemodynamics in acute ischemic stroke: a prospective cohort study. Int. J. Emerg. Med. 5, 1–4. https://doi.org/10.1186/1865-1380-5-3 (2012).
Kirkman, M. A., Citerio, G. & Smith, M. The intensive care management of acute ischemic stroke: an overview. Intensiv. Care Med. 40, 640–653. https://doi.org/10.1007/s00134-014-3266-z (2014).
Powers, W. J. et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American heart association/american stroke association. Stroke 50 (12), e344–e418. https://doi.org/10.1161/STR.0000000000000211 (2019).
Martins, S. C. O. et al. Guidelines for acute ischemic stroke treatment: part II: stroke treatment. Arq. Neuropsiquiatr. 70, 885–893. https://doi.org/10.1590/s0004-282x2012001100012 (2012).
Williams, B. et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European society of cardiology (ESC) and the European society of hypertension (ESH). Eur. Heart J. 39 (33), 3021–3104. https://doi.org/10.1093/eurheartj/ehy339 (2018).
Unger, T. et al. 2020 International society of hypertension global hypertension practice guidelines. Hypertension 75 (6), 1334–1357. https://doi.org/10.1161/HYPERTENSIONAHA.120.15026 (2020).
Brott, T. et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke 20 (7), 864–870. https://doi.org/10.1161/01.STR.20.7.864 (1989).
Larrue, V., von Kummer, R., Müller, A. & Bluhmki, E. Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with Recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian acute stroke study (ECASS II). Stroke 32 (2), 438–441. https://doi.org/10.1161/01.STR.32.2.438 (2001).
Banks, J. L. & Marotta, C. A. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke 38 (3), 1091–1096. https://doi.org/10.1161/01.STR.0000258355.23810.c6 (2007).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American college of cardiology/american heart association task force on clinical practice guidelines. Hypertension 71 (6), e13–e115. https://doi.org/10.1161/hyp.0000000000000066 (2018).
Miller, J., Kinni, H., Lewandowski, C., Nowak, R. & Levy, P. Management of hypertension in stroke. Ann. Emerg. Med. 64 (3), 248–255. https://doi.org/10.1016/j.annemergmed.2014.03.004 (2014).
Gąsecki, D., Kwarciany, M., Kowalczyk, K., Narkiewicz, K. & Karaszewski, B. Blood pressure management in acute ischemic stroke. Curr. Hypertens. Rep. 23, 1–11. https://doi.org/10.1007/s11906-020-01120-7 (2021). https://link.springer.com/article/
Bebawy, J. F. et al. Nicardipine is superior to Esmolol for the management of postcraniotomy emergence hypertension: a randomized open-label study. Anesth. Analg. 120 (1), 186–192. https://doi.org/10.1213/ANE.0000000000000473 (2015).
Park, S. H. et al. Nicardipine is more effective than Esmolol at preventing blood pressure increases during emergence from total intravenous anesthesia. Korean J. Anesthesiol. 57 (5), 597–603. https://doi.org/10.4097/kjae.2009.57.5.597 (2009).
Kovac, A. L. & Masiongale, A. Comparison of Nicardipine versus Esmolol in attenuating the hemodynamic responses to anesthesia emergence and extubation. J. Cardiothorac. Vasc. Anesth. 21 (1), 45–50. https://doi.org/10.1053/j.jvca.2006.08.005 (2007).
Striessnig, J., Ortner, N. J. & Pinggera, A. Pharmacology of L-type calcium channels: novel drugs for old targets? Curr. Mol. Pharmacol. 8 (2), 110–122. https://doi.org/10.2174/1874467208666150507105845 (2015).
Warne, T. et al. Structure of a beta1-adrenergic G-protein-coupled receptor. Nature 454 (7203), 486–491. https://doi.org/10.1038/nature07101 (2008).
Rosenbaum, D. M., Rasmussen, S. G. & Kobilka, B. K. The structure and function of G-protein-coupled receptors. Nature 459 (7245), 356–363 (2009).
Ahmed, N. et al. Consensus statements and recommendations from the ESO-Karolinska stroke update conference, Stockholm 11–13 November 2018. Eur. Stroke J. 4 (4), 307–317. https://doi.org/10.1177/2396987319863606 (2018).
Bath, P. M., Appleton, J. P., Krishnan, K. & Sprigg, N. Blood pressure in acute stroke: to treat or not to treat: that is still the question. That Is Still Question Stroke. 49, 1784–1790. https://doi.org/10.1161/strokeaha.118.021254 (2018).
Acknowledgements
The authors would like to thank Dr Derya Öztürk for the support of this research.
Author information
Authors and Affiliations
Contributions
MA, CS—provided the main framework, identified, and organized primary materials, and collaborated in writing the manuscript. KU, KZ—identified appropriate references and collaborated on the writing of the manuscript. AE, KM —reviewed and contributed to drafting sections of the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was performed after the approval of institutional ethics committee (University of Health Sciences Şişli Hamidiye Etfal Training and Research Hospital Health Application and Research Center Clinical Research Ethics Committee, date: 24/10/2023, no: 4137) in accordance with the Declaration of Helsinki. Patients or their legal representatives were informed about the study and a consent form was obtained.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Melekoğlu, A., Kahveci, U., Köksal, Z. et al. Comparison of Esmolol and Nicardipine treatment in hypertensive acute ıschemic stroke patients. Sci Rep 15, 14376 (2025). https://doi.org/10.1038/s41598-025-98699-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-98699-1