Abstract
To investigate how spinopelvic parameters change when transitioning between standing, sitting, and lateral decubitus (LD) positions, providing insights for optimizing acetabular cup placement in total hip arthroplasty (THA). A retrospective study was performed on 140 patients undergoing primary THA from 2023 to 2024. Lateral spinopelvic radiographs were taken in standing, sitting, and LD positions, measuring SS, PT, pelvic incidence (PI), and ante-inclination (AI). Measurements were performed by two independent reviewers using mediCAD® software, with inter-rater reliability assessed (ICC range: 0.83–0.91). Paired t-tests were used to compare spinopelvic parameters (SPP) values across positions, and associations with demographic factors, spinopelvic mobility, and other clinical variables were analyzed using Chi-square, ANOVA, and Kruskal-Wallis tests. We included 90 men (mean age 44.93 ± 13.28 years) and 50 women (mean age 43.10 ± 12.17 years). Mean BMI was 26.4 ± 3.1 kg/m². SS, PT, and AI showed significant differences across positions (P < 0.001). From standing to LD, SS decreased (<-5°) in 51.4% of patients, remained consistent (-5 to + 5°) in 35.7%, and increased ( > + 5°) in 12.9%. AI decreased in 26.4% of patients, remained consistent in 25.7%, and increased in 47.9%. Changes in AI correlated with SS (P = 0.02) and PT (P = 0.001). No significant associations were found between SPP changes and age, gender, BMI, or spinopelvic mobility. Our study showed that pelvic position and, consequently, acetabular orientation may change in LD, indicating that SPPs in LD cannot be assumed to be the same as in standing. It has implications for surgeons performing THA in LD, as intraoperative pelvic shifts may influence implant positioning and potentially impact postoperative stability and functional outcomes.
Similar content being viewed by others
Introduction
Instability is a common reason for revising arthroplasty, occurring in 1–4% of primary total hip arthroplasties (THAs)1,2. Malpositioning of acetabular cup is a major cause of instability3,4,5. In order to prevent instability, Lewinnek proposed a safe zone for anteversion and inclination angles of the cup component6. However, even within this safe zone, high rates of instability have been reported7,8. To reduce this risk, it has been suggested to adjust the safe zone for spinopelvic parameters (SPPs), such as sacral slope (SS), pelvic tilt (PT), and orientation of the anterior pelvic plane (APP)9.
Recent studies have emphasized the importance of considering dynamic changes in spinopelvic alignment during different positions. For instance, it has been shown that variability in SPPs between standing and sitting positions can significantly impact the functional orientation of the acetabular component1. Moreover, it has been suggested that personalized adjustments to the safe zone based on individual spinopelvic mobility could enhance postoperative stability and reduce dislocation rates10. These findings show that recognizing how these positional changes affect SPPs is increasingly seen as essential for optimizing cup placement and reducing the risk of instability in THA.
Beyond their relevance to THA, SPPs have also been studied in relation to various hip joint disorders. Some studies demonstrated that increased pelvic incidence or pelvic tilt might be associated with the development of hip osteoarthritis11,12. On the other hand, some studies showed no relationship between SPPs and hip osteoarthritis13,14,15. One recent study also reported no significant correlation between hip osteoarthritis or dysplasia, and various SPPs16. These findings further highlight the complexity of spinopelvic alignment and its potential implications for hip biomechanics.
Current routine preoperative spinopelvic measurements rely on standing and sitting lateral spinopelvic radiographs to determine spinopelvic mobility and adjusted safe zones for optimized placement of acetabular component. However, when performing THA in LD position, which is one of the most popular approaches among orthopedic surgeons, the position of pelvis and thus SPPs might change affecting the orientation of acetabular component. To our knowledge, no study has explored the changes in SPPs specifically in the LD position. Given that the acetabular ante-inclination (AI) angle varies with different patient positions17, understanding its behavior in the LD position could be valuable for surgeons performing THA in this orientation. Thus, this study aims to assess the impact of the LD position on pelvic position and SPPs and to compare these findings with SPPs in standing and seated positions.
Materials and methods
In a retrospective study, we enrolled all patients who underwent primary total hip arthroplasty at our center between 2023 and 2024. The study received approval from the Institutional Review Board of Tehran University of Medical Sciences. The ethical committee board also granted approval for the use of data from our database for research purposes (IR.TUMS.IKHC.REC.1402.011). We confirm that all research was carried out in accordance with the relevant guidelines/ regulations and the Declaration of Helsinki. All patients gave informed consent to take part in the study. We excluded patients with missing or inadequate data/radiographs, revision surgeries, DDH Crowe 3 and 4, and history of previous contralateral THA or spinal surgery from the study. We extracted the patients’ data and radiographs from our institutional database, including gender, age, body mass index (BMI), operative side, and underlying disease.
Radiographic protocol
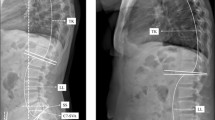
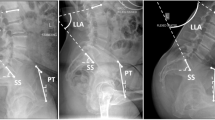
In addition to routine preoperative pelvic and hip radiographs, we took three lateral spinopelvic radiographs for each patient in standing, sitting, and LD positions in our preoperative protocol. For the standing position, the patient stood upright with the side perpendicular to the X-ray detector, arms crossed in front, feet shoulder-width apart, and head in a neutral forward-facing position (Fig. 1). For the sitting position, the patient sat upright on a radiolucent chair with the side perpendicular to the X-ray detector, arms across the chest, feet flat on the floor, hips/knees at 90° angles, and head in a neutral forward-facing position (Fig. 2). For the LD position, the patient lay on their side perpendicular to the X-ray detector, with the operative side above and positioned at 30° of hip and knee flexion, and the lower leg positioned at neutral hip and 45° of knee flexion. The pelvis was fixed so that both anterior superior iliac spines aligned vertically against the table (Fig. 3). In all three positions, the central ray was directed at the level of the iliac crest (L4-L5).
We measured the following SPPs in all three radiographs (Figs. 1, 2 and 3). Sacral slope (SS) was measured by the angle between a line along the S1 superior endplate and a horizontal line. Pelvic Tilt (PT) was measured by the angle between a line from the center of the femoral head to the midpoint of S1 superior endplate and a vertical line. Pelvic Incidence (PI) was measured using the angle between a line perpendicular to the midpoint of S1 superior endplate and a line connecting this point to the center of the femoral head. If the centers of both femoral heads did not overlap, we used the midpoint of the line connecting both femoral head centers. Ante-inclination (AI) was assessed by measuring the angle between a line connecting both ends of the acetabulum and the horizontal line. Two hip fellowship surgeons, under the supervision of the senior author, conducted all the measurements for each patient using the mediCAD® classic 3.5 software, which has been validated with acceptable reliability for preoperative planning of THA18. The mean of the two measurements for each parameter was calculated and used for analysis. Inter-rater reliability was evaluated using the intraclass correlation coefficient (ICC) with a two-way mixed-effects model.
Statistical analysis
We performed data analysis using SPSS v. 26. Continuous variables were reported as mean ± SD. We used the Kolmogorov-Smirnoff test to check for normality. Categorical variables were reported as absolute and relative frequency. We used a paired-sample t-test to compare standing, sitting, and LD values. Pearson’s Chi-square and Fisher’s Exact tests were used to determine the effect of gender, underlying disease, and spinopelvic mobility on changes in SPPs, as well as the impact of changes in different SPPs on each other. One-way ANOVA was used to study the effect of BMI on changes in SPPs. The Kruskal-Wallis test was used to examine the effect of age and PI on changes in SPPs. A significance level of 0.05 was applied in our analysis.
Results
A total of 140 patients were included in this study, consisting of 50 women and 90 men. The mean age was 43.10 ± 12.17 for women and 44.93 ± 13.28 for men. Full demographic data is provided in Table 1.
The interrater reliability (ICC) of angular parameters including SS, PT, PI, and AI were 0.88 (95%CI = 0.79–0.90), 0.86 (95%CI = 0.73–0.96), 0.91 (95%CI = 0.86–0.96), and 0.83 (95%CI = 0.71–0.91) showing good agreement.
Regarding spinopelvic mobility, 11 patients (7.9%) were classified as stiff, 47 (33.6%) as mobile, and 82 (58.6%) as hypermobile. Table 2 displays the mean values of SPPs, including SS, PT, PI, and AI, and their changes from standing to sitting and standing to LD position. Except for PI, which is an anatomic parameter, all other parameters showed a significant change both from standing to sitting (P < 0.001) and from standing to LD position (P < 0.001).
Three patterns of change in SPPs were observed from standing to LD position: decreasing (<-5°), consistent (-5 to + 5°), and increasing ( > + 5) (Fig. 4). Specifically, changes in SS were decreasing (<-5°) in 51.4% of cases, consistent (-5° to + 5°) in 35.7% of cases, and increasing ( > + 5°) in 12.9% of cases. Changes in PT were decreasing (<-5°) in 13.6% of cases, consistent (-5° to + 5°) in 39.3% of cases, and increasing ( > + 5°) in 47.1% of cases. As expected, there was a significant inverse association between changes in SS and PT from standing to LD position (χ2(4, 140) = 133.59, P < 0.001, Cramer’s V = 0.69).
In terms of changes in AI from standing to LD position, 26.4% of cases showed a decrease (<-5°), 25.7% showed consistency (-5° to + 5°), and 47.9% showed an increase ( > + 5°). Changes in AI also showed a significant moderate association with changes in SS (Fischer’s Exact P = 0.02, Cramer’s V = 0.2) and PT (Fischer’s Exact P = 0.001, Cramer’s V = 0.2). As seen in Fig. 5 and 65.2% of patients with an increasing PT ( > + 5°) also had an increasing AI ( > + 5°), 36.4% with a consistent PT (-5° to + 5°) also had a consistent AI, and 52.6% with a decreasing PT (<-5°) also had a decreasing AI.
No association was found between changes in SS from standing to LD position and gender (Chi-square, χ2(2, 140) = 1.106 P = 0.575), age (Kruskal-Wallis, χ²(2, 140) = 4.23, P = 0.120), BMI (ANOVA, F (2,147) = 0.469, P = 0.627), underlying disease (Fischer’s Exact, P = 0.366), operative side (Chi-square, χ2(2, 140) = 1.925, P = 0.382), spinopelvic mobility (Fischer’s Exact, P = 0.393), and PI (Kruskal-Wallis, χ²(2, 140) = 2.15, P = 0.340).
Discussion
Spinopelvic parameters (SPPs) play a crucial role in THA outcomes by influencing acetabular orientation and implant positioning, thereby affecting the risk of complications such as dislocation and impingement19. Recent studies emphasize the importance of accounting for dynamic spinopelvic alignment changes across positions, suggesting that individualized safe zone adjustments based on spinopelvic mobility may improve stability and reduce dislocation rates10.
Although many orthopedic surgeons perform THA in the lateral decubitus (LD) position, to the best of our knowledge, no study has specifically examined changes in pelvic position and SPPs in this position. Given that acetabular ante-inclination (AI) varies with patient positioning17, understanding its dynamics in the LD position could aid implant placement. A back-propagation neural network (BPNN) model has predicted sitting SPPs from standing radiographs, providing insights for THA planning20. However, no study has investigated how SPPs change when transitioning from standing to LD position. This study is the first to address this gap by assessing the influence of the LD position on SPPs and comparing these findings with SPPs in standing and sitting positions.
A recent study validated a patient-specific approach for positioning the acetabular component in THA by considering spinopelvic biomechanics. Comparing this approach to qualitative hip-spine classification targets revealed the superiority of patient-specific safe zones, providing more precise and tailored guidance for acetabular positioning. This study underscores the importance of incorporating individual SPPs in THA planning to improve surgical outcomes and reduce the risk of instability21. Additionally, some studies have shown that 40-70% of components fall outside the safe zone22,23,24,25,26. This is particularly important considering the reported high rates of instability within the safe zone27. The presence of a cup positioned within a suitable orientation range has been linked to a decreased likelihood of dislocation, although the danger is not entirely eradicated28. While a cup positioned within an appropriate range reduces the risk of dislocation, other variables related to the patient, surgery, and implant also impact the stability of THA. Therefore, careful surgical planning is crucial in addressing this complex matter29. Our results support the idea that a personalized approach, considering the dynamic changes in SPPs, may reduce the risk of postoperative dislocation and highlight the dynamic nature of spinopelvic alignment and its potential implications for THA.
Although pelvic incidence (PI) is a fixed anatomical parameter, it has been shown that the sacral slope, pelvic tilt, and ante-inclination (AI) are closely related parameters that change with body position. PI is a fixed anatomical parameter equal to the sum of sacral slope and pelvic tilt (PI = SS + PT). Changes in SS and PT occur in opposite directions to maintain sagittal balance30. In a standing position, the normal sacral slope is 40°±10° and when pelvis tilts anteriorly, the sacral slope increases. Moreover, when transitioning from standing to sitting, the pelvis tilts posteriorly by about 20° and it results in a decrease in sacral slope to 20°±9° and an increase in acetabular ante-inclination, combining both anteversion and inclination, from 35°±10° to 52°±11°31. It is worth noting that, each degree of posterior pelvic tilt leads to a 0.7° increase in acetabular ante-inclination30. In addition, a normal ΔSS, the change in sacral slope from standing to sitting, is 10°-30°, with an average of 20°(ΔSS) and it reflects spinopelvic mobility30. Our study showed an inverse relationship between changes in SS and PT when transitioning from standing to LD position. It confirms the interdependence of these parameters and suggests that positional alterations significantly impact one another.
We also found a significant moderate association between changes in AI and changes in SS and PT when transitioning from standing to the lateral decubitus (LD) position. As shown in Fig. 5, nearly two-thirds (65.2%) of patients who experienced an increase of > + 5° in PT during this transition also exhibited a > + 5° increase in AI. This finding is consistent with the study by Lazennec et al., which demonstrated that functional acetabular anteversion increases with rising PT32. However, their study examined this change from a standing to a sitting position. Our results suggest that AI, a critical parameter for cup positioning in total hip arthroplasty (THA), is influenced by positional changes in SS and PT. Consequently, alterations in pelvic tilt in the lateral position can affect acetabular AI and the orientation of the acetabular cup. In other words, the AI measured in the standing lateral spinopelvic view does not necessarily remain constant in the LD position.
Several studies highlight the effect of age and sex on spinopelvic parameters. As individuals progress in age, there is a significant reduction in lumbar lordosis and an increase in pelvic tilt, potentially impacting overall stability spinal alignment33,34. Tuan Hao Tan et al., in a systematic review and meta-analysis showed that younger and female patients exhibit marked disparities in LL, SS and PT, thus suggesting the presence of age and sex variations, which should be taken into account during planning of spinal realignment surgeries35. Interestingly, our study did not find significant associations between changes in SPPs and factors such as gender, age, BMI, underlying disease, operative side, spinopelvic mobility, and PI. This suggests that the observed changes in SPPs are primarily driven by positional alterations rather than patient-specific demographic or clinical characteristics.
Our study had some limitations. First, although we made every effort to standardize patient positioning during lateral spinopelvic radiography, controlling pelvic rotation remained challenging, particularly in the lateral decubitus position. To minimize potential measurement bias, an orthopedic surgeon supervised patient positioning and reviewed the radiographs to ensure accuracy. Second, we obtained lateral spinopelvic X-rays in a straight-seated position. According to a study by Ohyama et al., sacral slope differs significantly between straight and relaxed-seated positions36, which may have influenced our results. Third, We did not assess SPPs after THA, although studies have shown that they can change after the operation and overtime37. Furthermore, we did not follow the patients to assess the success of the procedure and the percentage of dislocation. The lack of postoperative follow-up prevented us from comparing the concordance of cup position with preoperative measurements in standing and lateral decubitus position.
Conclusion
Our study showed that pelvic position and, consequently, acetabular orientation may change in the LD position, indicating that SPPs in LD cannot be assumed to be the same as in standing. This finding has implications for surgeons performing THA in this position, as intraoperative pelvic shifts may influence implant positioning and potentially impact postoperative stability and functional outcomes. Future research should focus on longitudinal studies to further elucidate the impact of these dynamic changes on THA outcomes and explore the potential benefits of a personalized approach to cup positioning based on dynamic SPPs.
Data availability
The datasets used and analysed during the current study will be available from the corresponding author on reasonable request.
References
Haynes, J. A. et al. Contemporary surgical indications and referral trends in revision total hip arthroplasty: A 10-Year review. J. Arthroplasty. 31(3), 622 (2016).
Jamshidi, M. M. M., Moharrami, A. & Mortazavi, S. M. J. How to avoid instability after total hip arthroplasty, narrative review. Iran. J. Orthop. Surg. 18(4), 163 (2020).
Hermansen, L. L., Viberg, B., Hansen, L. & Overgaard, S. True cumulative incidence of and risk factors for hip dislocation within 2 years after primary total hip arthroplasty due to osteoarthritis: A nationwide population-based study from the Danish hip arthroplasty register. J. Bone Joint Surg. Am. 103(4), 295 (2021).
Leichtle, U. G., Leichtle, C. I., Taslaci, F., Reize, P. & Wünschel, M. Dislocation after total hip arthroplasty: risk factors and treatment options. Acta Orthop. Traumatol. Turc. 47(2), 96 (2013).
Masonis, J. L. & Bourne, R. B. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin. Orthop. Relat. Res. 405, 46 (2002).
Lewinnek, G. E., Lewis, J. L., Tarr, R., Compere, C. L. & Zimmerman, J. R. Dislocations after total hip-replacement arthroplasties. J. Bone Joint Surg. Am. 60(2), 217 (1978).
Christensen, C. P., Karthikeyan, T. & Jacobs, C. A. Greater prevalence of wound complications requiring reoperation with direct anterior approach total hip arthroplasty. J. Arthroplasty. 29(9), 1839 (2014).
Ilchmann, T., Zimmerli, W., Bolliger, L., Graber, P. & Clauss, M. Risk of infection in primary, elective total hip arthroplasty with direct anterior approach or lateral transgluteal approach: a prospective cohort study of 1104 hips. BMC Musculoskelet. Disord. 17(1), 471 (2016).
Sharma, A. K. & Vigdorchik, J. M. The hip-spine relationship in total hip arthroplasty: how to execute the plan. J. Arthroplasty 36(7s), S111 (2021).
Stefl, M. et al. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J. 99(1_Supple_A), 37 (2017).
Yoshimoto, H. et al. Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine 30(14), 1650 (2005).
Sariali, E., Lazennec, J. Y., Khiami, F., Gorin, M. & Catonne, Y. Modification of pelvic orientation after total hip replacement in primary osteoarthritis. Hip Int. 19(3), 257 (2009).
Bendaya, S. et al. Healthy vs. osteoarthritic hips: a comparison of hip, pelvis and femoral parameters and relationships using the EOS® system. Clin. Biomech. Elsevier Ltd. 30(2), 195 (2015).
Gebhart, J., Weinberg, D., Bohl, M. & Liu, R. Relationship between pelvic incidence and osteoarthritis of the hip. Bone Joint Res. 5(2), 66 (2016).
Raphael, I. J. et al. Pelvic incidence in patients with hip osteoarthritis. Archives Bone Joint Surg. 4(2), 132 (2016).
Soydan, Z., Bayramoglu, E., Altas, O. & Şen, C. Revealing the effect of spinopelvic alignment on hip disorders. Clin. Med. Insights: Arthritis Musculoskelet. Disord. 16, 11795441231191790 (2023).
Elbuluk, A. M., Wright-Chisem, J. I., Vigdorchik, J. M. & Nunley, R. M. Applying the hip-spine relationship: what x-rays and measurements are important? J. Arthroplasty. 36(7s), S94 (2021).
Bouché, P-A. et al. Validation of mediCAD® software for fully digital preoperative planning of total hip arthroplasty: a retrospective study. Orthop. Traumatol. Surg. Res. 110(6), 103941 (2024).
Grammatopoulos, G., Innmann, M., Phan, P., Bodner, R. & Meermans, G. Spinopelvic challenges in primary total hip arthroplasty. EFORT Open. Reviews. 8(5), 298 (2023).
Zhao, M. et al. An artificial neural network model based on standing lateral radiographs for predicting sitting pelvic tilt in healthy adults. Front. Surg. 9, 977505 (2022).
Ramkumar, P. N. et al. Patient-specific safe zones for acetabular component positioning in total hip arthroplasty: mathematically accounting for spinopelvic biomechanics. J. Arthroplast. 38(9), 1779 (2023).
Bosker, B., Verheyen, C., Horstmann, W. & Tulp, N. Poor accuracy of freehand cup positioning during total hip arthroplasty. Arch. Orthop. Trauma Surg. 127, 375 (2007).
Callanan, M. C. et al. The John Charnley award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin. Orthop. Relat. Research®. 469(2), 319 (2011).
Hassan, D. M., Johnston, G. H., Dust, W. N., Watson, G. & Dolovich, A. T. Accuracy of intraoperative assessment of acetabular prosthesis placement. J. Arthroplast. 13(1), 80 (1998).
Reize, P., Geiger, E. V., Suckel, A., Rudert, M. & Wülker, N. Influence of surgical experience on accuracy of acetabular cup positioning in total hip arthroplasty. Am. J. Orthop. (Belle Mead NJ). 37(7), 360 (2008).
Grammatopoulos, G. et al. 2018 Frank Stinchfield award: spinopelvic hypermobility is associated with an inferior outcome after THA: examining the effect of spinal arthrodesis. Clin. Orthop. Relat. Research®. 477(2), 310 (2019).
Esposito, C. I. et al. Total hip arthroplasty patients with fixed spinopelvic alignment are at higher risk of hip dislocation. J. Arthroplast. 33(5), 1449 (2018).
Grammatopoulos, G. et al. The effect of orientation of the acetabular component on outcome following total hip arthroplasty with small diameter hard-on-soft bearings. Bone Joint J. 97(2), 164 (2015).
Meermans, G., Grammatopoulos, G., Innmann, M. & Beverland, D. Cup placement in primary total hip arthroplasty: how to get it right without navigation or robotics. EFORT Open. Rev. 7(6), 365 (2022).
Jamshidi, M. M. M., Moharrami, A., Sharifpour, S., Mafi, A. R. & Mortazavi, S. J. The role of spinopelvic parameters in total hip arthroplasty: a current concept review. J. Orthop. Spine Trauma. 40, (2022).
Batra, S., Khare, T., Kabra, A. P. & Malhotra, R. Hip-spine relationship in total hip arthroplasty–Simplifying the concepts. J. Clin. Orthop. Trauma. 29, 101877 (2022).
Lazennec, J-Y. et al. Hip spine relationships: application to total hip arthroplasty. Hip Int. 17(5_suppl), 91 (2007).
Prost, S. et al. Do age-related variations of sagittal alignment rely on spinopelvic organization? An observational study of 1540 subjects. Global Spine J. 13(8), 2144 (2023).
Asai, Y. et al. Sagittal spino-pelvic alignment in adults: the Wakayama spine study. PloS One. 12(6), e0178697 (2017).
Tan, T. H., Tan, J-H. & Hey, H. W. D. Changes in spinopelvic parameters between standing and sitting postures: a systematic review and meta-analysis. Clin. Spine Surg. 37(3), 97 (2024).
Ohyama, Y. et al. Measurement of spinopelvic sagittal alignment in the relaxed seated position rather than in the straight seated position is suitable for assessing spinopelvic mobility in patients before total hip arthroplasty. Sicot J. 9, 2 (2023).
Sultan, A. A. et al. The impact of spino-pelvic alignment on total hip arthroplasty outcomes: a critical analysis of current evidence. J. Arthroplast. 33(5), 1606 (2018).
Acknowledgements
We are grateful to Mrs. Zahra Pajouhandeh and Mrs. Zahra Chaboki, research specialists at our center, whose assistance contributed to the successful completion of this project.
Author information
Authors and Affiliations
Contributions
M.R. wrote the original draft and performed data analysis. A.M. collected data and conducted radiographic measurements. A.A. revised the manuscript and conducted radiographic measurements. M.H. assisted with data collection. S.M.J.M. conceived the original idea and developed the methodology. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Razzaghof, M., Moharrami, A., Abbaszadeh, A. et al. Spinopelvic parameters in the lateral decubitus are different from standing and sitting positions. Sci Rep 15, 14685 (2025). https://doi.org/10.1038/s41598-025-98819-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-98819-x