Abstract
This study aimed to demonstrate whether plasma galectin-3 could predict the development of postoperative delirium (POD) in patients with acute aortic dissection (AAD). Prospective, observational study. Cardiac surgery intensive care unit. Consecutive patients who were diagnosed with AAD and operated at the Cardiac Medical Center of Fujian Province between December 2020 and December 2022. Patients were classiffed into two groups according to the Confusion Assessment Method for the Intensive Care Unit: POD group and NON-POD group. Each patient’s plasma was tested before emergency surgery. Baseline demographic data and preoperative, intraoperative, and postoperative clinical data were collected. The short-term clinical outcomes were followed up daily. The rate of POD was calculated. The risk factors for POD were analyzed through univariate analysis and multivariate logistic regression. Receiver operating characteristic (ROC) curves were used to assess the ability of plasma galectin-3 to predict POD. A total of 309 study subjects were included in this study, and the rate of POD was 38.8%. Patients with AAD were categorized into the POD and NON-POD cohorts postoperatively based on their CAM-ICU scores. There was no statistically significant difference in the baseline characteristics between the two groups (P > 0.05). However, patients in the POD group had significantly elevated plasma galectin-3 levels (P < 0.001). The ROC curves showed that plasma galectin-3 had a sensitivity of 72.5% and a specificity of 70.9% as a potential biomarker for the diagnosis of POD. The critical value of plasma galectin-3 for diagnosing POD was 9.18 ng/mL. Plasma galectin-3 levels remained an independent predictor of POD after controlling for different variables (P < 0.001). Elevated plasma galectin-3 levels are associated with an increased risk of POD. Plasma galectin-3 may be a prospective biomarker for predicting POD.
Similar content being viewed by others
Introduction
Acute aortic dissection (AAD) is a cardiovascular disease characterized by an acute-onset, rapid progression, and a high mortality rate (up to 85%) due to rupture-related death, which tends to occur within a short time1. AAD requires emergency surgery to prevent rupture, but surgery on the aortic arch involves blood supply to the nervous system. In addition, the surgery needs to be performed under hypothermic conditions, which may further lead to inadequate perfusion of the nervous system. Therefore, AAD increases the risk of postoperative delirium (POD) by 31.8–52.0%2,3. POD is an acute, delirious brain dysfunction characterized by fluctuating levels of attention and consciousness, disorganized thinking, disorientation, and memory impairment4. Previous studies have shown that POD leads to prolonged mechanical ventilation, deterioration of cognitive trajectory, and an increased readmission rate5,6. Furthermore, POD is closely associated with decreased mobility, a prolonged intensive care unit stay, increased costs, and adverse clinical outcomes7. Currently, there is a lack of effective treatment for POD, and the pathogenesis of POD has not been elucidated to date. Nevertheless, there is growing evidence that inflammation is a key early event in the pathophysiological process of POD8. POD may occur immediately after a surgery for AAD, but its symptoms are often delayed9. The delay can be considered a window of prevention and treatment for POD. Assuming that there is a simple and convenient indicator suggesting that POD may develop prior to symptoms appearing, early detection and intervention can greatly reduce the POD-related damage to cognitive function. Therefore, the search for a reliable biomarker for predicting POD is particularly significant for the control and treatment of POD.
Galectin-3, a novel inflammatory biomarker discovered recently, is involved in many pathophysiological processes, including inflammatory response, immunity, and metastasis, and is a key promoter of inflammation associated with cardiovascular diseases10. Galectin-3 has been shown to stimulate the expression of various inflammatory factors and chemokines, attract monocytes and macrophages to accumulate in lesions, and modulate the immune response by acting as a damage-associated molecular pattern or pattern recognition receptor11. García-Revilla et al.12 found that activated glial cells can express galectin-3 during neuroinflammation. It is worth noting that galectin-3 is strongly associated with the inflammation, disease severity, and clinical outcomes of traumatic brain injury and spontaneous cerebral hemorrhage13. Therefore, galectin-3 may reflect the extent of brain damage and the inflammatory state of certain neurological disorders. POD is an acute neuropsychiatric syndrome with increasing evidence showing that it is associated with elevated levels of inflammatory cytokines14. The involvement of galectin-3 in various disease processes has been widely reported. Although galectin-3 has now been documented to be associated with delirium after labor15 and stroke16, those studies were preliminary correlational studies, and further research is needed to determine whether this conclusion can be generalized to other populations. The correlation between galectin-3 and POD in patients with AAD has not been reported to date. This study aimed to explore whether galectin-3 has the potential to be a biomarker for predicting POD in patients with AAD. If the correlation between galectin-3 and POD is confirmed, this will provide a scientific basis and a new idea for the control and treatment of POD.
Materials and methods
Protocol approvals and patient consent
This clinical study was approved by the ethics review committee of Union Hospital Fujian Medical University, Fujian, China (Ethics Approve No. 2020KY082) and registered in the China Clinical Trials Registration Center (No. ChiCTR2000034856). The protocol in this study conformed to the Declaration of Helsinki. Informed consents were obtained from all the subjects.
Study design and population
This was a prospective, observational study. Consecutive patients who were diagnosed with AAD and underwent surgery at the Cardiac Medical Center of Fujian Province between December 2020 to December 2022 were selected. All patients were diagnosed with AAD through computed tomography (CT), magnetic resonance imaging, or ultrasound; were ≥ 18 years old; and had no history of cognitive impairment, COVID-19, malignancy, previous cardiac surgery, autoimmune disease, chronic liver failure, or chronic renal failure. All patients were anesthetized and operated on by the same anesthesia and treatment groups. The endpoint of this study was the development of delirium within five days postoperatively. The study subjects were divided into the POD group and the NON-POD group based on the results of the CAM for the ICU (CAM-ICU).
Collection of demographic and clinical datas
A questionnaire was designed to collect the participants’ demographic and clinical data, including age, sex, Body mass index (BMI), smoking history, drinking history, and history of cerebral infarction. The initial results of physiological and biochemical indicators measured after admission, including systolic blood pressure, diastolic blood pressure, B type natriuretic peptide (BNP), glycosylated hemoglobin, C-reactive protein (C-rp), leukocytes, neutrophils, monocytes, lymphocytes, erythrocytes, and platelets, were obtained from medical records. Clinical data, including the duration of surgery, duration of aortic cross-clamping, duration of mechanical ventilation, and total length of hospital stay, were also assessed. The baseline characteristics of the patients were recorded by professionals for statistical analysis.
Blood test
After admission, about 5 ml of peripheral blood was collected with the patient’s consent before emergency surgery, and the blood samples were stored in a refrigerator at 4 °C. The blood samples were centrifuged at 15,000 rpm for 20 min at 4 °C within 2 h of collection, and the upper plasma layer was collected and frozen at − 80 °C. According to previous studies and the instruction manual, the concentration of plasma galectin-3 was measured using an enzyme-linked immunosorbent assay17.
Assessment for POD
The CAM recommended by the fourth edition of The Diagnostic and Statistical Manual of Mental Disorders published in the United States was adopted, and the CAM-ICU score was used as a diagnostic tool18. From postoperative admission to the ICU until day 5, an assessment for POD was performed daily by a trained researcher at 8:00 a.m., 4:00 p.m., and 8:00 p.m. For patients who had any clinical evidence of POD outside the above assessment time points, an additional assessment was performed by the intensive care physicians. All the researchers and clinical staff were trained to conduct the assessment for POD. There was a designated researcher blinded to CAM-ICU determinations who completed a structured chart review for evidence of delirium. The assessment for POD using the CAM-ICU was divided into two steps. First, a patient’s state of consciousness was assessed using the Richmond Agitation-Sedation Scale (RASS), which is a 10-point scale with 1 to 4 indicating varying degrees of anxiety and agitation, 0 indicating a state of calmness, and − 1 to − 5 indicating varying degrees of sedation (− 5 for no conscious response and − 1 for drowsiness). The assessment for delirium was discontinued if a patient was deeply sedated or had no conscious response (RASS score of − 5 to − 4). The second step, which was the assessment for delirium, was performed if the RASS score was ≥ − 3. The CAM-ICU scale was used to assess for delirium, and the diagnostic criteria included four items: 1) sudden changes in or a fluctuating mental state; 2) scattered attention; 3) disordered thinking; and 4) an altered level of consciousness. POD was diagnosed when criteria 1 + 2 + 3 or 1 + 2 + 4 were met.
Calculation of sample size
The Leslie Kish formula was used to calculate the sample size as follows:
According to Lin’s findings, the prevalence of delirium after surgery for ADD was set at 31.8%3; the margin of error was controlled at δ = л × 0.2, which resulted in δ = 0.0636; and the ɑ was set at 0.05. The sample size was increased by 25% to consider factors such as dropout. Therefore, the final calculated sample size was 208*(1 + 0.25) = 260 cases.
Statistical analysis
Patients were divided into POD group and NON-POD group according to whether delirium occurred after operation. SPSS26.0 statistical software was used for data processing and analysising. Qualitative parameters were expressed as numbers and percentage N (%). Chi-square test or Fisher exact test was selected as the difference test method between groups. Continuous variables consistent with normal distribution were represented by Mean ± SD, while non-normal distribution data were represented by median and quartile. Independent sample T test and Mann–Whitney U test were used for difference test. According to the quartile of galectin-3 levels, the number of POD was grouped and calculated. LASSO regression analysis was used to screen the characteristic factors. Multivariate logistic regression analysis of the relationship between plasma Galectin-3 level and POD. The sensitivity and specificity of plasma Galectin-3 levels in POD diagnosis were evaluated by receiver operating characteristic (ROC) curve analysis, and the maximumYouden index was calculated as the critical value. p < 0.05 indicated signiffcance.
Results
Clinical characteristics
From December 2020 to December 2022, 363 patients with AAD were included, and 309 patients were finally included, as shown in Fig. 1. We documented demographic and clinical characteristics. According to the scores of RASS and CAM-ICU, the AAD patients were divided into POD group (120 cases) and Non-POD group (189 cases), and the incidence of POD was 38.8%.
Table 1 shows the demographic and clinical characteristics of the POD group and the NON-POD group. There were no statistically significant difference in the baseline characteristics between the two groups (P > 0.05). There were statistically significant differences in Galectin-3, BNP, procalcitonin, CPB, surgery duration, analgesics and sedatives, hypoxemia, APACHEII, mechanical ventilation duration, ICU stay and hospitalization days, P < 0.05.
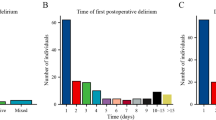
Relationship plasma galectin-3 levels and POD with AAD patients
In Fig. 2A, the violin chart showed that there were significant differences in plasma Galectin-3 levels between the POD group and the non-POD group, p < 0.01. According to the quartile of plasma galectin-3 levels, the prevalence of POD is shown in Fig. 2B. The results showed a linear relationship between the prevalence of POD and the quartile of baseline plasma galectin-3 levels in AAD patients: the prevalence of POD increased with the increase of plasma galectin-3 levels (p < 0.001).
Relationship plasma galectin-3 level and POD. (A) The violin chart showed that plasma galectin-3 levels were compared between NON-POD group and POD group. The white dots show the median and the difference was tested by Mann–Whitney U test, p < 0.01. (B) Incidence of POD in subgroups divided by galectin-3 level quartiles. Q1, ≤ 4.24 ng/ml; Q2, 4.24–8.17 ng/ml; Q3, 8.17–15.23 ng/ml; Q4, ≥ 15.23 ng/ml.
Lasso regression screens characteristic variables
The LASSO regression model effectively reduces the influence of irrelevant features. In this study, we integrated all general demographic and clinical data collected before, during, and after the operation into the LASSO regression model for feature selection. Each path in the model illustrated the changing trend of the coefficients under different regularization intensities (Fig. 3A). By shrinking the coefficients to prevent over fitting, the path map demonstrated how these coefficients adjust with increasing penalty severity (Fig. 3B). Our analysis revealed that the LASSO regression model performed optimally when the standard error λ of the minimum distance was set at 0.058, resulting in a model that retained six variable features: BNP, Galectin-3, APACHE II, analgesics and sedatives, surgery duration, and hypoxemia.
Feature selection was performed using the Minimum Absolute shrink and selection operator (LASSO) binary logistic regression model. (A) The adjustment parameter (λ) in the LASSO model is selected by minimum criteria using 10 × cross-validation. The relationship between the area under the subject operating characteristic (AUC) curve and log (λ) is plotted. Draw a vertical dotted line at the best value using 1 standard error of the minimum standard and the minimum standard (1-SE standard). According to tenfold cross-validation, the standard error of the minimum distance λ is 0.058. (B) Lasso coefficient profile for each texture feature. Generate coefficient profiles from logarithmic (λ) sequences. A vertical line is drawn at the selected value using × 10 cross validation, where the best λ yields 6 filter variables.
Logistic regression analysis for the association of galectin-3 with POD
To avoid collinearity and overfitting, we combined single-factor analysis (P ≤ 0.2) with LASSO analysis. Feature factors were selected based on previous studies and expert opinions to facilitate subsequent multifactor analysis. The results of the logical analysis are shown in Table 2. In Model 1, after adjusting for age, gender and BMI, low plasma Galectin-3 levels (≤ 9.18 ng/mL) were used as the reference. High plasma Galectin-3 levels (> 9.18 ng/mL) were found to be a risk factor for postoperative delirium (POD) (OR = 5.764, 95% CI = 3.503–9.658, P = 0.001). In Model 2, after further adjusting for APACHE-II and BNP, the high Galectin-3 levels continued to be a risk factor for POD (OR = 5.480, 95% CI = 3.288–9.311, P < 0.001). In Model 3, after adjusting for confounding factors, the high Galectin-3 levels remained a significant risk factor for POD (OR = 3.914, 95% CI = 2.264–6.851, P < 0.001). Additionally, we conducted a further analysis of the variance inflation factor (VIF) for each variable, as shown in Supplementary Table 1, to ensure that none of the variables exhibited problematic collinearity. Correlation tests were also performed to explore potential associations between the variables, as presented in Supplementary Table 2. Based on these results, we confirm that Galectin-3 remains a distinct and relevant predictor in the model, with no significant collinearity that would undermine the robustness of the model.
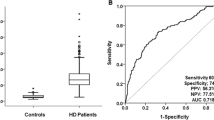
ROC analysis of plasma galectin-3 in the POD with AAD patients
The results of ROC analysis showed that Galectin-3 had the highest predictive value in Fig. 4. The area under the curve (AUC) of serum galectin-3 in AAD patients was 0.737 (95% CI: 0.690–0.794), while the diagnostic sensitivity was 72.5%, and the specificity was 70.9%. In ROC analysis, we found that the cut-off value for Galectin-3 diagnosis of POD was 9.18 ng/mL. In addition, Fig. 4 presents the ROC curves for other variables included in the multivariate regression model. The AUC for analgesics and sedatives in AAD patients was 0.685 (95% CI: 0.625–0.746), with a diagnostic sensitivity of 75.8% and specificity of 61.4%. The AUC for surgery duration was 0.610 (95% CI: 0.546–0.674), with a sensitivity of 65.8% and specificity of 53.4%. The AUC for hypoxemia was 0.639 (95% CI: 0.575–0.704), with a sensitivity of 72.5% and specificity of 70.9%. The AUC for APACHE-II was 0.588 (95% CI: 0.523–0.653), with a sensitivity of 70.8% and specificity of 44.4%. Finally, the AUC for BNP was 0.572 (95% CI: 0.506–0.639), with a sensitivity of 60.8% and specificity of 53.4%.
Discussion
In this study, we observed that the rate of POD in patients with AAD was 38.8%, which is consistent with that reported previously3. In addition, we compared the difference in plasma galectin-3 levels between AAD patients with and without POD, which revealed that plasma galectin-3 levels in the patients with POD were significantly higher. We also found that the incidence of POD increased with increasing galectin-3 levels, suggesting that the plasma galectin-3 level is associated with the incidence of POD. To assess the accuracy of the galectin-3 level in the diagnosis of POD, we performed a receiver operating characteristic curve analysis, which revealed that the plasma galectin-3 level had a high sensitivity and specificity for the diagnosis of POD. Various models were introduced to further determine the relationship between POD and galectin-3 levels. We found that the galectin-3 level can be used as an independent predictor for POD.
A large amount of data has shown that the high morbidity and mortality rates of POD are important health problems for human beings18. Individuals who are susceptible to having an elevated inflammatory response when exposed to a source of acute stress, such as surgery or infection, are at an increased risk of developing delirium19. AAD is a cardiovascular disease with an acute onset, rapid progression, and a high mortality rate. POD remains one of the most common and serious complications despite the fact that modified triple-branched stent graft implantation has greatly reduced the durations of operation, cardiopulmonary bypass, and aortic cross-clamping by eliminating anastomosis of the branches of the aortic arch20. The mechanism of POD remains unknown, but increasing evidence suggests that inflammation may be involved in this process21. Our findings led to a consistent conclusion, and our multivariate analysis showed that the inflammatory factor galectin-3 was significantly higher in the POD group than in the non-POD group. It is evident that inflammation play a crucial role in the pathogenesis of POD. However, our study found that WBC, platelet, and C-rp were not significantly associated with POD, which is consistent with the findings of previous studies3,7,22. This discrepancy may be due to the differing mechanisms of action of various inflammatory factors across different disease processes. AAD was a serious cardiovascular condition characterized by the tearing of the inner lining of the aorta, leading to the formation of a dissection within the aortic wall. Evidence suggests that Galectin-3 can be considered an inflammatory biomarker of vascular injury in the early stages of development23. Therefore, Galectin-3 may be more sensitive than traditional inflammatory markers (e.g., WBC, platelets, C-rp) in the context of vascular injury diseases.
Studies have reported that systemic inflammatory mediators cross the blood–brain barrier, activating brain microglia and inducing neuroinflammation. Previous studies have also shown that neuroinflammation tends to increase with age and that age is a predictor of the development of POD24. Interestingly, in our study, there was no statistical difference between the two groups of study subjects. This may be explained by the fact that advanced age is a risk factor for the development of AAD.
Galectin-3 has been reported to be involved in various pathophysiological processes, including apoptosis, adhesion, angiogenesis, cell migration, cell proliferation, and cell differentiation, but its main function is to induce inflammation and fibrosis25. Galectin-3 is a central regulator of key processes in acute and chronic inflammatory environments26. Galectin-3 can cross-link with glycosylated membrane receptors by binding to the glycan portion of receptors through its carboxyl-terminal domain. This can trigger multiple signaling cascades, leading to the activation of inflammatory cells. A sustained inflammatory response has been recognized as a key factor in promoting the progression of POD27,28.
Galectin-3 has recently been shown to be involved in various neurological disorders. T. Cengiz identified galectin-3 as a potential non-invasive biomarker for determining advanced Parkinson’s disease29. In recent years, galectin-3 has emerged as a new biomarker for stroke and cerebrovascular disease. Wang revealed that after a patient with cognitive impairment had an acute ischemic stroke, the high galectin-3 levels aggravated the neuroinflammation, which was closely associated with a poor prognosis30. Galectin-3 may be a prognostic biomarker for hemorrhagic stroke. Nishikawa et al.31 showed that in subarachnoid hemorrhage, an elevated plasma galectin-3 level was associated with delayed cerebral ischemia after subarachnoid hemorrhage but had no such association with vasospasm, suggesting that galectin-3 may be a new prospective therapeutic or research target for brain injury after subarachnoid hemorrhage. However, the relationship between galectin-3 and POD remains unknown. To date, the findings of Zhu et al.15 demonstrated that elevated maternal galectin-3 levels are associated with serum S100B, C-reactive protein, and the Acute Physiology and Chronic Health Evaluation II (APACHE-II) score. Galectin-3 may be involved in the inflammatory process of brain injury, which is related to maternal delirium, and may have the potential to be a biomarker for predicting maternal delirium. The APACHE-II score can assess the severity of a disease and its prognosis. The results of this study showed that there was a statistically significant difference in the APACHE-II score between the POD and non-POD groups, which is consistent with the findings of Zhu et al.15. However, Zhu Y’s study population comprised postpartum women in the ICU, which is a population that not only often suffers from complications like acute pancreatitis, acute heart failure, urolithiasis, infections, hemorrhage, and other illnesses but also suffers from a rapid decline in estrogen and progesterone levels coupled with maternal separation anxiety32. Therefore, further exploration is required to determine whether the conclusion can be extended to other populations. The relationship between galectin-3 and delirium also requires further in-depth studies. A study conducted by Klimiec-Moskal et al.16 further discovered that the galectin-3 level was associated with post-stroke delirium, but the study was only a preliminary study, and no conclusion was drawn as to whether galectin-3 could be used as a predictor. The current findings suggest the possibility that galectin-3 is involved in cognitive impairment. Our study will further deepen our understanding of the involvement of galectin-3 in the field of cognitive impairment. Consequently, we believe this study will provide valuable insights into research on POD related to AAD. Strategies targeting Galectin-3 may also be employed to help prevent POD. These strategies could include early screening and risk assessment, as well as the development of personalized care plans. Additionally, further clinical trials will be conducted to verify the effectiveness of Galectin-3 as a biomarker for the prevention of postoperative delirium and to identify the most effective interventions.
There are several limitations to this study. First, the study was a single-center observational study, and a larger sample size and multicenter trial are needed to determine the predictive value of galectin-3 for POD occurrence in patients with AAD. Second, due to the acute and critical nature of AAD, preoperative cognitive baseline assessment was not performed, which could have provided additional insight into POD prediction. Finally, Galectin-3 has potential predictive value for POD, but the strength of Galectin-3 alone is not enough, a more comprehensive approach, incorporating both preoperative biomarkers and intraoperative factors, is necessary for improved POD prediction.
Conclusion
This study mainly found that Galectin-3 may be a prospective biomarker for predicting POD with AAD. Correlation analysis showed that POD incidence in AAD patients gradually increased with the increase of plasma galectin-3 level. Logistic regression results showed that plasma galectin-3 level may be an predictor of postoperative AAD. If the link between plasma galectin-3 levels and POD is further confirmed, it may have important value for ultra-early intervention of POD.
Data availability
The original contributions presented in the study are included in the article material, further inquiries can be directed to the corresponding author.
References
Mangum, K. D. & Farber, M. A. Genetic and epigenetic regulation of abdominal aortic aneurysms. Clin. Genet. 97(6), 815–826 (2020).
Shi, Q. et al. Risk factors for postoperative delirium in type a aortic dissection patients: A retrospective study. Med. Sci. Monit. 25, 3692–3699 (2019).
Lin, J.-L. et al. A nomogram model for assessing predictors and prognosis of postoperative delirium in patients receiving acute type A aortic dissection surgery. BMC Cardiovasc. Disord. 23(1), 72 (2023).
Swarbrick, C. J. & Partridge, J. S. L. Evidence-based strategies to reduce the incidence of postoperative delirium: A narrative review. Anaesthesia 77(Suppl), 1 (2022).
Lee, D. H. et al. Postoperative delirium in patients receiving hip bipolar hemiarthroplasty for displaced femoral neck fractures: The risk factors and further clinical outcomes. J. Arthroplasty 38(4), 737–742 (2023).
Jin, Z., Hu, J. & Ma, D. Postoperative delirium: Perioperative assessment, risk reduction, and management. Br. J. Anaesth. 125(4), 492–504 (2020).
Lin, Y.-J. et al. Association between glucose variability and postoperative delirium in acute aortic dissection patients: An observational study. J. Cardiothorac. Surg. 16(1), 82 (2021).
Neerland, B. E. et al. Associations between delirium and preoperative cerebrospinal fluid C-reactive protein, interleukin-6, and interleukin-6 receptor in individuals with acute hip fracture. J. Am. Geriatr. Soc. 64(7), 1456–1463 (2016).
Wang, S. et al. Systematic review and meta-analysis of the risk factors for postoperative delirium in patients with acute type A aortic dissection. J. Thorac. Dis. 15(2), 668–678 (2023).
Wang, Z. et al. Melatonin inhibits atherosclerosis progression via galectin-3 downregulation to enhance autophagy and inhibit inflammation. J. Pineal Res. 74(3), e12855 (2023).
Sayed, A. et al. Galectin-3: A novel marker for the prediction of stroke incidence and clinical prognosis. Mediat. Inflamm. 2022, 2924773 (2022).
García-Revilla, J. et al. Galectin-3, a rising star in modulating microglia activation under conditions of neurodegeneration. Cell Death Dis. 13(7), 628 (2022).
Yan, X.-J. et al. Role of galectin-3 in plasma as a predictive biomarker of outcome after acute intracerebral hemorrhage. J. Neurol. Sci. 368, 121–127 (2016).
Taylor, J. et al. Postoperative delirium and changes in the blood-brain barrier, neuroinflammation, and cerebrospinal fluid lactate: A prospective cohort study. Br. J. Anaesth. 129(2), 219–230 (2022).
Zhu, Y. et al. Serum galectin-3 levels and delirium among postpartum intensive care unit women. Brain Behav. 7(8), e00773 (2017).
Klimiec-Moskal, E. et al. Elevated plasma levels of galectin-3 binding protein are associated with post-stroke delirium—A pilot study. J. Neuroimmunol. 356, 577579 (2021).
Chen, Y. et al. Galectin 3 enhances platelet aggregation and thrombosis via Dectin-1 activation: A translational study. Eur. Heart J. 43(37), 3556–3574 (2022).
Hamadnalla, H. et al. Optimal interval and duration of CAM-ICU assessments for delirium detection after cardiac surgery. J. Clin. Anesth. 71, 110233 (2021).
Lv, X.-C. et al. Plasma interleukin-6 is a potential predictive biomarker for postoperative delirium among acute type a aortic dissection patients treated with open surgical repair. J. Cardiothorac. Surg. 16(1), 146 (2021).
Chen, L.-W. et al. Ascending aorta and hemiarch replacement combined with modified triple-branched stent graft implantation for repair of acute debakey type I aortic dissection. Ann. Thorac. Surg. 103(2), 595–601 (2017).
Alam, A. et al. Surgery, neuroinflammation and cognitive impairment. EBioMedicine 37, 547–556 (2018).
Lin, Y. et al. Risk factors for postoperative delirium in patients with triple-branched stent graft implantation. J. Cardiothorac. Surg. 15(1), 171 (2020).
Atalar, M. N. et al. Assessment of serum galectin-3, methylated arginine and Hs-CRP levels in type 2 diabetes and prediabetes. Life Sci. 231, 116577 (2019).
Li, T. et al. Effect of regional vs general anesthesia on incidence of postoperative delirium in older patients undergoing hip fracture surgery: The RAGA randomized trial. JAMA 327(1), 50–58 (2022).
Sygitowicz, G., Maciejak-Jastrzębska, A. & Sitkiewicz, D. The diagnostic and therapeutic potential of galectin-3 in cardiovascular diseases. Biomolecules 12(1), 66 (2021).
Yip, P. K. et al. Galectin-3 released in response to traumatic brain injury acts as an alarmin orchestrating brain immune response and promoting neurodegeneration. Sci. Rep. 7, 41689 (2017).
Liu, X. et al. Single-cell RNA sequencing identifies an Il1rn+/Trem1+ macrophage subpopulation as a cellular target for mitigating the progression of thoracic aortic aneurysm and dissection. Cell Discov. 8(1), 11 (2022).
Cui, H. et al. Untargeted metabolomics identifies succinate as a biomarker and therapeutic target in aortic aneurysm and dissection. Eur. Heart J. 42(42), 4373–4385 (2021).
Cengiz, T. et al. The roles of galectin-3 and galectin-4 in the idiopatic Parkinson disease and its progression. Clin. Neurol. Neurosurg. 184, 105373 (2019).
Wang, Q. et al. Serum galectin-3 as a potential predictive biomarker is associated with poststroke cognitive impairment. Oxid. Med. Cell Longev. 2021, 5827812 (2021).
Nishikawa, H. & Suzuki, H. Possible role of inflammation and galectin-3 in brain injury after subarachnoid hemorrhage. Brain Sci. 8(2), 66 (2018).
Oliveira-Neto, A. F. et al. Prediction of severe maternal outcome among pregnant and puerperal women in obstetric ICU. Crit. Care Med. 47(2), e136–e143 (2019).
Acknowledgements
The authors appreciate all subjects who participated in this study. We would also like to thank Fujian Medical University Union Hospital for supporting the data collection of this study.
Funding
This work was supported by the Joint Funds for the innovation of science and Technology, Fujian province, China (Grant Number 2021Y0023); the Union Hospital, Fujian Medical University, Fuzhou, China (Grant Number 2022YYZDXK01); and the Key Laboratory of Cardio-Thoracic Surgery (Fujian Medical University), Fujian Province University Construction Project (No. 2019-67).
Author information
Authors and Affiliations
Contributions
C.L. and L.Y. designed the study and submitted the manuscript.J.F., C.M. and P.Y. prepared the first draft of the manuscript and made the literature review. J.F. and C.M. were contributed equally to this study and shared the first authorship. L.S. and W.Z. maded substantial changes in the manuscript. P.Q. andL.S. collected and analyzed datas together. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jiang, F., Cai, M., Peng, Y. et al. A correlational study of plasma galectin-3 as a potential predictive marker of postoperative delirium in patients with acute aortic dissection. Sci Rep 15, 16022 (2025). https://doi.org/10.1038/s41598-025-98858-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-98858-4