Abstract
Jugular venous pulse (JVP) waveform contour is directly linked to right atrial hemodynamics and is a potential tool for diagnosing various cardiovascular diseases. The reference standard, central venous line catheterization, while precise, is restricted to critical care units owing to the necessity for surgical procedures and specialized operator skills. Conventional ultrasound imaging systems can reliably measure jugular venous vessel dynamics but are hindered by low operational frame rates, large form factors, and the requirement for trained operators. In this study, we propose a portable system using single-element ultrasound technology for reliable JVP waveform acquisition and methods for quantifying the JVP contour features. The performance of the system and method was validated against a reference ultrasound imaging system in a preclinical study on 65 asymptomatic volunteers (27 female). Operating at an acquisition rate of 250 Hz, the system reliably captures JVP waveforms with a temporal resolution of 4 ms. The maximum and minimum jugular venous diameter measurements showed a statistically significant and strong correlation with the reference measurements (r = 0.93 and r = 0.86, respectively, p < 0.001). The devised algorithms effectively segmented JVP cycles and analyzed their contour features with a sensitivity and specificity of 92%. These results provide preliminary evidence for the potential use of the developed system for high-fidelity JVP waveform acquisition and pulse contour feature assessment. The ability to accurately evaluate the JVP contour characteristics can provide insights into right atrial hemodynamics, potentially facilitating the early detection and monitoring of vascular anomalies.
Similar content being viewed by others
Introduction
The jugular venous pulse (JVP) waveform provides a direct, non-invasive window into the dynamics of right heart function, offering critical insights into cardiovascular health1,2. The JVP characteristic contour features - a, x, c, x’, v, and y, (illustrated in Fig. 1) are shaped by the right atrial pressure changes that correspond to the cyclic blood volume changes during the cardiac cycle phases. Monitoring these contour features can thus yield remarkable information on cardiovascular disease (CVD) diagnosis and prognosis. Emerging evidence suggests that the assessment of JVP contour features can potentially identify the occurrence of cardiac structural abnormalities, including pericarditis, cardiac tamponade, tricuspid stenosis, tricuspid regurgitation, septal defects, and functional dysfunctions, including atrial fibrillation, pulmonary hypertension, atrioventricular dissociation2,3,4,5.
Despite its potential for heart failure screening, JVP measurements are seldom recorded during clinical examinations. Clinicians estimate jugular venous pressure by visually examining the jugular vein (JV) pulsations in the neck and measuring the vertical distance between the highest point of pulsation and the right atrium4,6. They also monitor distinctive patterns in the JVP, such as Kussmaul’s sign, cannon a wave, dominant v wave, and rapid y descent, which can signal various CVD conditions. However, the accuracy of visual inspection is debatable, and the reliability varies with operator expertise7. The gold standard for recording JVP waveforms is central venous line catheterization8, which involves surgical insertion of a pressure catheter into the internal jugular vein9,10. This procedure is typically performed only in critical care settings, demands medical expertise, and may result in catheter infections, pneumothorax, arrhythmias, and vascular puncture5. Given the complexity of current JVP measurement techniques, there is a critical need for non-invasive, real-time, easy-to-use automated systems to reliably capture and quantify JVP waveform features for the early detection of CVDs.
Although several non-invasive methods, including ultrasonography, photoplethysmography (PPG)11,12 wearable radio frequency sensors13, and optical sensors14 can potentially capture JVP waveforms, they are often limited by various technical challenges. Ultrasonography, the most widely used non-invasive method, offers direct measurement from the jugular vein by tracking its vessel motion patterns15,16,17,18. However, most clinical-grade ultrasound systems are seldom equipped with dedicated image-processing tools for vessel identification and tracking and are often associated with significant expenses. Moreover, they require trained sonographers for accurate measurements and are confined to clinical settings owing to their large form factors. Additionally, these systems typically have limited scan rates (~ 60 Hz), yielding low-resolution JVP waveforms that are inadequate for precise quantification of JVP contour features. Advanced ultra-fast imaging systems using graphical processing units offer milli-second-level resolution19,20 but are limited by substantial computational and hardware requirements21. Existing image-processing tools are primarily designed for arterial measurements and cannot effectively track venous vessel motion due to its multiphasic motion pattern. In addition to the operational limitations of ultrasound imaging systems, legal regulations limit their applicability to hospital settings22. PPG11,12, wearable radio frequency sensors13, and optical sensors14rely on measuring the skin displacements induced by blood volume changes in the JV23,24. For this reason, these measurements are influenced by carotid artery interference, signal distortions, skin surface transfer functions, and dependence on skin-tissue interactions. Additionally, these systems are constrained by their limited resolution, which is critical to measuring the intricate features of the JVP waveform.
In this work, we propose a single-element ultrasound system for the reliable acquisition of high-resolution JVP waveforms coupled with a novel method to extract its contour features (see Methods). The system performance was validated in 65 healthy participants. The present study aimed to (1) explore the feasibility of high-resolution JVP waveform acquisition using the developed single-element ultrasound system, (2) assess the JVP contour features using the developed pulse contour identification algorithm, and (3) investigate the variation in JVP contour features across the study population. To test for accuracy, the JV diameter values and JVP waveforms measured using the proposed system were compared with those recorded using a clinical-grade ultrasound imaging system. The pre-clinical study results and observations are discussed in further sections, demonstrating its potential for the early screening of right atrial anomalies and outlining directions for future research.
Results
The demographic characteristics and baseline measurements of the study population are summarized in Table 1.
Reliability of jugular venous pulse waveform acquisition
The proposed single-element ultrasound system reliably captured JVP waveforms from all the study participants. The system acquires JVP signals at 250 Hz, yielding a temporal resolution of 4 ms. Ultrasound transducer, with a narrow beam at a spatial half-angle of 1.3°, captures high-fidelity RF echo frames when aligned with the longitudinal axis of JV. The RF frames, sampled at 80 MHz, with an amplitude resolution of 10 μm, were further enhanced by up-sampling via cubic spline interpolation. The signal quality (SQ) of the echo, a measure of the sharpness and energy ratio, was used to evaluate the quality of the echo signals (see Methods). Frames with JV wall echoes exhibiting a signal-to-noise ratio (SNR) greater than 20 dB and an SQ score above 20 were selected, while lower-quality frames were excluded to ensure reliable measurements.
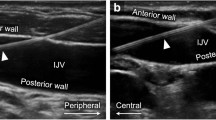
(a) RF echo frame acquired using single-element ultrasound system illustrating the proximal (PW) and distal (DW) JV wall echoes (b) reference JVP Scan highlighting the area selected for diameter estimation. JVP waveforms measured using the (c) proposed system and (d) reference from Participant 1 (Age = 23, Male) (e) proposed system and (f) reference from Participant 6 (Age = 25, Female) (g) proposed and (h) reference from Participant 59 (Age = 34, Female).
A sample of an RF echo frame with an SNR > 20 dB and an SQ > 20 from a particular participant (ID: 16, Age = 25 years, Male, BP = 121/76 mmHg) is represented in Fig. 2(a). The JVP cycles corresponding to the captured JV wall echoes from three volunteers are indicated in Figs. 2(c), (e), and (g). For all the participants, the JVP acquisition could be performed within 3 to 5 min, which included locating the jugular vein, ultrasound transducer probe orientation, and signal recording.
The reference portable imaging system (B-mode) operates at a frame rate of 33 Hz, providing a temporal resolution of 30 ms. The reference cine loop files were processed using commercial tracking software, with the B-scan calibrated at 17.81 pixels/mm. The longitudinal section of the JV from Participant 16 acquired using the reference system is depicted in Fig. 2(b). The respective B-mode JVP waveforms acquired from the three participants are indicated in Figs. 2(d), (f), (h). The acquired reference cine loops had adequate image quality with a frame resolution of 1024 × 768 pixels. Hence, none of the imaging files were discarded from the analysis.
JVP diameter assessment and feature assessment
The developed cycle segmentation algorithm (see Methods) facilitates the selection of high-fidelity, beat-to-beat JVP waveforms while rejecting inadequate cycles with a sensitivity and specificity of 92%. The beat-to-beat cycles obtained after the cycle segmentation phase were monitored to evaluate the JV diameter ranges. The range of minimum (Dmin) and maximum (Dmax) diameters of the JVP cycles measured using the proposed system were 4.37 to 12.87 mm and 5.24 to 14.39 mm, respectively. The JV diameter values measured by the proposed system were comparable to those from the reference system (Dmin: 4.28 to 13.35 mm, Dmax: 5.14 to 14.57 mm). The acquired JVP cycles were periodic and repeatable, with a beat-to-beat coefficient of variation of less than 8%.
The measured JVP waveforms exhibited all characteristic features. The developed pulse contour feature identification algorithm successfully identified these features with an average sensitivity and specificity of 92%. The obtained JVP contour features exhibited minimal cycle-to-cycle variability. The algorithm evaluated the amplitude and time of occurrence of contour features with a mean coefficient of variation of 7.19% for amplitude and 10.24% for timing. Figure 3(a)–(c) shows the automatically labeled pulse contour features of the JVP waveforms acquired from three different participants using the proposed system. Figure 3(d)–(f) illustrates the corresponding JVP waveforms with annotated features captured using the reference imaging system. Due to the limited resolution of the imaging system, not all waveform features were observable. For instance, in Fig. 3(e), the feature point x could not be clearly identified, and in Fig. 3(f), the a’ wave represents a fusion of the a and c waves.
Waveform feature analysis and system performance evaluation
The comparison between the precision of JVP contour feature assessment derived from the proposed and reference techniques in terms of hit rate (percentage of number of cycles with contour features correctly identified to the total number of JVP cycles) is represented in Fig. 3(g). JVP waveforms captured by the proposed system demonstrated enhanced precision in determining the JVP contour features, achieving an average hit rate of 97% compared to 80% for the reference method. This validates the efficacy of the devised algorithm in reliably assessing the JVP waveform features.
The relative amplitudes and timing of JVP contour features were assessed to examine their distribution in a healthy cohort. Figure 4(a) represents the box plot illustration of the ratio of the amplitudes of JVP contour features to Dmin (x’) across all participants. The summary of the time location distribution of JVP characteristic features within the cardiac cycle length is presented as boxplots in Fig. 4(b). Consistent dispersion patterns were observed across all distributions.
Comparison of JVP diameter measurement accuracy against reference system
The association between the JVP diameter measurements (Dmax, Dmin) obtained by the proposed system and those from the reference system (longitudinal scan axis) is illustrated in the regression plots in Fig. 5(a) and (b), respectively. The linear regression analysis demonstrated a statistically significant correlation in diameter assessments, Dmax with r = 0.93, p < 0.001, 95% CI [−1.34 to 0.56], and Dmin with r = 0.86, p < 0.001, 95% CI [−2.77 to 0.12]. The agreement between the Dmax and Dmin values measured by the proposed and reference system is illustrated using Bland-Altman analysis, represented in Figs. 5(c) and (d), respectively.
Bland-Altman analysis between the proposed single-element ultrasound system and reference imaging revealed a mean bias of −0.25 mm (SD = 1.14) with Limits of agreement = −2.48 to 2.00 mm for Dmin and − 0.29 mm (SD = 0.81) with Limits of agreement = −1.63 to 1.57 mm for Dmax measurements. BA analysis revealed negligible bias (p > 0.05) and a scattered plot showing no evident trend indicating the absence of systematic progression of errors.
A cross-sectional study (20 participants) was conducted to evaluate the variation in JVP diameter measurements compared to reference imaging measured along both the short and longitudinal axes. Bland-Altman analysis revealed no significant bias between the JV diameters measured using the proposed single-element ultrasound system and reference imaging in both axes. For, short-axis scans, the Dmax showed a mean bias of −0.12 mm (SD: 0.73 mm), and the Dmin showed a mean bias of −0.05 mm (SD:0.66 mm). In the longitudinal axis, Dmax exhibited a mean bias of −0.04 mm (SD: 0.39 mm), while the Dmin demonstrated a mean bias of −0.12 mm (SD: 0.62 mm). These results indicate minimal bias and variability, indicating strong agreement between the proposed system and the reference standard for JVP diameter measurements across both axes, supporting the system’s reliability and accuracy.
JVP waveforms captured using the proposed system yielded a group average correlation of 0.91 with the reference method. The mean beat-to-beat coefficient of variation in Dmin and Dmax assessments were 7.95% and 6.62%, respectively. Figures 6(a)-(c) depicts the example plots of beat-to-beat JV diameter values (Dmax and Dmin) measured from three participants.
Discussion
The multiphasic JVP waveform characterized by three peaks (a, c, v) and three valleys (x, x’, y) reflects the right atrial pressure changes within a cardiac cycle1. These contour features offer valuable clinical information on right atrial hemodynamics and cardiac function2, with established associations to various structural and functional cardiac abnormalities. For example, an absent ‘a wave’ is indicative of atrial fibrillation, whereas an elevated ‘a wave’ signifies increased resistance to right atrial contraction, which is often observed in conditions such as pulmonary hypertension or tricuspid stenosis. Prominent ‘x descents’ are characteristic of cardiac tamponade, and giant ‘v waves’ are typically associated with tricuspid regurgitation2,25. Given its strong diagnostic potential, continuous monitoring of JVP contours could significantly enhance the early detection and management of cardiovascular diseases. However, the reference standard for JVP measurement, central venous catheterization, is confined to critical care settings owing to the measurement complexities10. Existing clinical monitoring technologies limit the utility of JVP contour assessment, primarily due to challenges in non-invasive, high-resolution signal acquisition and the lack of automated algorithms for feature annotation. This underscores the need for advanced, high-fidelity systems capable of real-time JVP contour measurement, which could facilitate early diagnosis and monitoring of cardiac dysfunctions.
This study introduces a single-element ultrasound system for the non-invasive acquisition of high-resolution JVP waveforms coupled with automated methods for mapping JVP contour features. Leveraging the precision of ultrasound technology, our approach minimizes the operational complexity associated with multi-element arrays while providing the resolution necessary to capture the intricate features of the JVP waveform26. The system performance was validated on 65 (healthy) participants aged 21 to 43 years. The system, operating at an acquisition rate of 250 Hz, yields high-fidelity JVP waveforms (time resolution = 4 ms) adequate for precise assessment of JVP contour features. To ensure the fidelity of the JVP waveforms for contour feature assessment, echo frames with a signal quality score below 20 and a signal-to-noise ratio (SNR) of less than 20 dB were automatically excluded from the analysis. JVP waveforms were recorded from all participants and were consistent and periodic, with a beat-to-beat variation of less than 8% (Fig. 6). The acquired JVP waveforms and JV diameter measurements were consistent with ranges reported and corroborated by previous studies15,27.
The accuracy of the JVP diameter measurements was validated by comparing them against the reference method. As evidenced by the Bland-Altman and regression analyses (Fig. 5), JVP diameter measurements exhibited a strong agreement between the two methods, with statistically insignificant bias (p > 0.05). Also, JVP waveforms recorded using the proposed system were consistent with those measured using the reference system, confirming the accuracy and reliability of the measurements. The developed correlation-based cycle segmentation algorithm ensures accurate selection of JVP cycles, preventing errors that could lead to inaccuracies in contour feature identification. With a sensitivity and specificity of 92%, the algorithm ensured reliable segmentation, which, in turn, enhanced the accuracy of automated JVP feature detection. Additionally, the automated contour feature identification algorithm demonstrated high sensitivity in detecting JVP contour features, with a mean coefficient of variation of less than 11%, ensuring robust and accurate waveform analysis. Furthermore, applying a thicker layer of ultrasound gel between the probe and the skin surface can minimize vein compression by enhancing acoustic coupling and reducing mechanical pressure on the vessel, thereby improving the reliability of JVP acquisition. Implementing a probe hold setup could also improve stabilization and ensure consistent pressure application, reducing operator-induced variability and improving measurement precision.
Comparison of pulse contour features measured by the proposed system with those from the reference method revealed that, while the reference system consistently captured the prominent peaks and valleys across all participants, intricate features, such as the x and v waveforms, were absent in some cases. In contrast, the proposed system reliably detected all contour features. It is important to note that in both systems, not all contour features were consistently observed across all 10 analyzed cycles. For example, in participants 19 and 47, the a and c waves were absent in most cycles, consistent with the reference measurements. The precision of the JVP waveform feature analysis was evaluated using the hit rate analysis (Fig. 3(g)), which indicates the proportion of cycles where all contour features were correctly identified relative to the total number of JVP cycles. JVP measurements were notably more challenging in participants with higher BMI or shorter necks, where visual identification of JV pulsations was difficult. This can be attributed to anatomical factors, such as deeper veins and interference from strong arterial signals.
The JVP waveform and contour features measured in this study were in line with those established in earlier literature involving cardiac catheterization trials, highlighting its potential as a non-invasive alternative. Several studies have explored the utility of imaging ultrasound systems for JVP waveform assessment15,28as they offer direct measurement from the vessel and provide real-time visualization of vessel dynamics. However, these systems demand trained sonographers and operate at lower frame rates, restricting the ability to capture critical JVP waveform features, such as the x, c, and v waves, as observed in prior research and our pilot studies. While high-frame-rate ultrasound systems capable of acquisition rates up to 10k FPS are available, they are compromised in cost, accessibility, computational overhead, and the need for specialized operators19,21. These systems mainly rely on graphics processing unit (GPU) based technology, with few offering real-time processing capabilities. Also, existing tools are primarily focused on arterial dynamics, with no dedicated systems addressing the unique characteristics of venous wall motion. This highlights the need for specialized algorithms capable of capturing the complex multiphasic nature of JVP waveforms and accounting for respiratory artifacts. Emerging advancements in wearable ultrasound technology29 have demonstrated the potential of continuous blood pressure monitoring. While primarily optimized for arterial dynamics, adapting such systems with intelligent algorithms could enable reliable assessment of JVP contour features, enhancing non-invasive continuous measurements.
Recent studies have explored plethysmography, non-contact imaging, RF, and microwave sensors for JVP measurement11,12,13,24,30. The signal quality of surface-based methods like PPG is influenced by skin surface transfer functions, distortions, and the material properties of the skin and underlying tissues. PPG primarily detects the microcirculation of arterial pulsations optically, and hence, the captured signals are a combination of both arterial and venous pulsations. Consequently, extraction of JVP waveforms would require advanced blind source separation techniques. Non-contact imaging-based JVP measurements face similar limitations, including dependence on image sensor specifications and pixel saturation. Since these systems rely on indirect measurements of skin displacement, accurately correlating them with JVP waveforms requires modeling the relationship between JVP pressure and surface deformations, which demands a thorough understanding of the vessel’s characteristics and the properties of the surrounding tissues. Additionally, these systems operate at lower frame rates and are prone to noise, carotid artery interference, and inaccuracies, particularly in individuals with higher BMI or less accessible veins13,31. In contrast to these methods, the proposed system provides direct measurements from the jugular vein, independent of the signal distortions and artifacts inherent in surface-based assessments. The devised system is portable, image-free, and can be implemented in resource-constrained settings with minimal operator intervention.
Limitations
The single-element ultrasound technique reported here to assess the JVP waveform contour features relies on a two-step framework, the first being the acquisition of high-fidelity JV echo frames and the other for post-processing to characterize the JVP contour features. This was to ensure manual monitoring of the quality of the signal by evaluating the signal quality metrics and distension waveform, ensuring reliable measurements. Factors such as carotid artery interference can alter the measurements, and dedicated algorithms to automatedly classify and reject the carotid influence are under development. This pilot validation study was conducted on a small cohort of healthy volunteers with limited age variability, and a clinical ultrasound imaging system was used for reference measurements. Future clinical trials planned on diverse diseased populations are underway to establish the functionality of the proposed system to reliably detect various cardiac dysfunctions. In these studies, we would compare the proposed technique against gold-standard invasive measurements.
Conclusion
A non-invasive, portable, and affordable system was developed to reliably measure the pulse contour features of the jugular venous pulse. The JVP diameter measurements obtained from this system were validated through comparison with a reference imaging ultrasound method in a pre-clinical in vivo study involving sixty-five participants aged 21 to 43 years. A strong statistically significant correlation was observed in the diameter values measured using the proposed and reference devices. The JVP waveform captured using the proposed and reference methods were morphologically similar and were on par with the earlier reported studies. The developed automated cycle segmentation and pulse contour identification algorithms evaluate the contour features reliably and eliminate the cumbersome task of manual annotation. The proposed system can measure high-quality jugular venous pulses non-invasively, proving its potential for early detection and prediction of cardiovascular anomalies.
Methods
Participants
The JVP waveforms were collected from sixty-five healthy participants from South India, all without a known history of CVDs. This study was performed in alignment with the protocols sanctioned by the Institutional Ethics Committee of IIT Madras (Approval Number: IEC/2021-01/JJ/07) and adhered to the ethical guidelines of the revised Helsinki Declaration of 2013. Informed written consent was obtained from all participants before the study. The participant selection and measurement protocols followed the ARTERY Society measurement guidelines for non-invasive hemodynamic systems. Participants aged above eighteen years were recruited for the study, with exclusion criteria including heart failure, pregnancy, venous dysfunctions, psychiatric illness, and history of carcinoma. Demographic information, clinical history, and lifestyle habits (alcohol, smoking, diet restrictions) were documented, and anthropometric measurements (height, weight, BMI) were recorded.
Participants were instructed to rest in the supine position for 5 min, as the venous pulsations are prominent in the supine compared to the sitting posture12. The operator ensured that the participant’s neck muscles are relaxed, maintaining the head in a neutral supine position and avoiding hyperextension32,33. Brachial blood pressure and heart rate measurements were recorded using the pressure cuff placed on the participant’s left arm. The right internal jugular vein was selected as the measurement site due to its proximity to the right atrium. The location of JV was visually identified by examining the neck pulsations, and the transducer probe was positioned with minimal hold-on pressure. Participants were instructed to avoid movements to prevent posture-induced variability. For JVP diameter assessments, the supine position was preferred as the increased central venous pressure and reduced gravitational effects in this posture facilitate venous filling, resulting in a near-circular cross-sectional shape32,33,34. This enhances imaging quality and allows for more precise and reliable diameter measurements. Participants were initially positioned supine with a slight inclination, and the head angle was adjusted between 0° and 30° to optimize signal quality based on JV wall echo metrics. The signal quality served as a real-time feedback metric, ensuring consistent and robust measurements. Optimal positioning was further confirmed using reference imaging scans, where the angulation was adjusted to achieve a near-circular JV cross-section. The elevation angle was fine-tuned, either positive or negative, by the operator to ensure the JV cross-section appeared nearly circular.
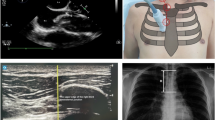
Effect of probe hold-on pressure on the jugular vein morphology (a-c) longitudinal and (d-f) short-axis ultrasound scans showing a distended JV under minimal hold-on pressure (a, d), partial compression with increased pressure (b, e) and complete collapse of JV under excessive pressure (c, f). Corresponding RF frames acquired using the proposed system illustrate variations in signal quality, with distinct vessel wall echoes at (g) minimal pressure, (h) altered signal quality under increased pressure, and (i) merged JV walls upon collapse.
Once distinct wall echoes with sufficient signal quality were observed, the vessel wall motion pattern was monitored, and the probe was reoriented, if necessary to obtain the strong wall echoes of sufficient signal quality. JVP waveforms were recorded for 30 consecutive cardiac cycles. Care was taken to ensure minimal contact pressure with the skin to prevent the flattening of the JV. The low frame rate distension waveform, coupled with the wall motion pattern and SQ metrics, offers real-time visual guidance to the operator, thereby ensuring the quality of recorded frames. Figure 7 illustrates the effect of hold-on pressure on JV morphology, demonstrating the variations in vessel diameter across longitudinal and short-axis ultrasound scans along with corresponding RF frames. With increasing hold-on pressure, the SQ progressively deteriorates, reflecting partial vein compression, and upon collapse, the opposing vein walls coalesce. To ensure measurement reliability, echo frames with an SQ score > 20 were selected for further processing to evaluate the JVP waveform, diameter, and pulse contour characteristics.
For reference measurements, a linear array ultrasound probe (L15HD, Clarius, Vancouver, Canada) was used to scan the JV motion along the longitudinal axis for 30 s. The acquired reference cine loop files were recorded in video graphic format (.avi file) and were processed offline with the Carotid Studio software (Cardiovascular suite, Quipu, Italy). The software enables automated tracking of JV wall motion over a 15-second window, with manual adjustments to ensure precise vessel boundary detection. The imaging axis was calibrated by converting pixel distances to millimeters, facilitating accurate JV diameter measurements. The tracking software provides manual control to ensure the tracking of good-quality frames. The reference JVP waveform and diameter ranges were computed and saved in a standard format.
Jugular venous pulse acquisition and Pre-processing
The measurement system utilizes a single-element ultrasound transducer (5 mm diameter) operating at an excitation frequency of 10 MHz. This custom-designed narrow-band transducer features a spatial half angle of less than 1.3° and operates in pulse-echo mode, generating a focused beam with a pulse repetition frequency of 250 Hz. The narrow half-angle beam width coupled with the poor-off axis sensitivity of the designed ultrasound transducer optimizes maximum sensitivity along the transducer’s central axis. This design ensures JVP measurements along the true diameter of the jugular vein, assuming a nearly circular cross-section. The ultrasound transducer (diameter: 5 mm) is enclosed within a custom-designed probe featuring a square head (length: 12.70 mm) and an ergonomic contoured body (97.5 mm × 29.57 mm) to enhance usability and operational stability. The ARM Cortex-M4 microcontroller (32-bit, LPC4370 FET256, NXP Semiconductors) controls the excitation of ultrasound pulses. While operating in receiver mode, the transducer captures the RF frames from the JV walls, which are conditioned using the analog front-end circuitry. These RF frames are digitized at a sampling frequency of 80 MHz. The system interfaces with the laptop via a USB 2.0 port, and a highspeed USB cable facilitates the transfer of digitized frames to the host system, which are stored as raw data files.
(a) Representation of the proposed single-element ultrasound system for JVP waveform feature extraction and the transducer probe design. (b) Schematic of Hardware and (c) Software architecture. (d) Illustration of the various steps of the devised automated cycle segmentation and pulse contour feature identification algorithms.
Software algorithms for JVP acquisition and waveform contour identification were developed in the LabVIEW platform (LabVIEW 2020, 32-bit, National Instruments Co., USA). The RF echo frames are conditioned by a 3rd-order Butterworth filter (frequency range: 1 to 10 MHz). When the probe is correctly positioned on the JV, each frame consists of static echoes from non-moving tissues, a transducer saturation zone, and a pair of negatively correlated venous wall echoes. The pair of moving echoes represent the proximal and distal vessel walls if their motion is negatively correlated over successive frames. The captured wall echoes offer information about the JV vessel’s wall dynamics. The shift in echo locations in subsequent frames corresponds to the expansion and contraction of the jugular vein during the cardiac cycle. The JV proximal and distal wall locations, identified from these moving echoes, are gated by placing cursor windows to define the JV region of interest (ROI). The acquisition software allows manual gating, enabling the operator to select the vessel wall echoes in real-time. A cross-correlation-based algorithm is implemented to track the frame-to-frame shifts in proximal and distal wall echo locations. These shifts are cumulatively added to update the vessel wall location, ensuring continuous wall motion tracking. The locations of the animated cursors are continuously updated, corresponding to the wall locations. A low-frame rate JV distension waveform is generated from the wall locations and is displayed in real-time.
The quality of captured signals is monitored by measuring the signal quality score, a metric to evaluate the strength and sharpness of the JV wall echoes. The SQ is calculated by estimating the ratio of vessel wall to lumen amplitude and energy values, and it is indicated on a cumulative scale from 0 to 100, with each JV wall echo contributing a score of 50. A low SQ score (SQ < 20 for each echo) provides real-time feedback, prompting the operator to re-orient the single-element ultrasound transducer for improved signal acquisition. The system software leverages the SQ score to guide the operator toward achieving high-quality acquisitions, with an SQ threshold greater than 20 for both proximal and distal wall echoes considered sufficient for reliable diameter measurements. Frames, with echoes meeting the threshold quality, are subsequently processed for reliable JVP measurements. Therefore, the low frame rate distension waveform, coupled with the wall motion pattern and SQ metrics, offers real-time visual guidance to the operator, ensuring reliable acquisition of high-fidelity JVP waveforms. Applying a squared Hilbert transform to the selected jugular vein (JV) region of interest (ROI) allows for the identification of the proximal and distal wall locations, which are subsequently used to calculate the JV lumen diameter. This diameter is calculated using an L-fit algorithm that measures the distance between the trailing edge of the proximal wall echo and the leading edge of the distal wall echo. Figure 8 (a) shows a representation of the proposed measurement system, with Fig. 8 (b) and (c) detailing the hardware and software architectures, respectively.
Jugular venous pulse waveform analysis
The acquired JVP distension waveform depicts the dynamic motion of the vessel walls with respect to the minimum diameter (Dmin) position. We developed an automated cycle segmentation algorithm to evaluate the diameter and beat-to-beat pulse contour features. This correlation-based cycle segmentation algorithm automatically selects and segments individual cycles from the measured JVP signals. It implements a windowed correlation approach, where the window length is determined using FFT information, and the reference cycle is generated by averaging the first five good JVP cycles. For cycle segmentation, the correlation between the reference JVP cycle and captured JVP waveforms are monitored. Both reference cycle and captured waveforms are normalized in the range − 1 to 1 range to eliminate the errors due to motion artifacts. A correlation coefficient threshold of 0.9 is selected to detect the JVP cycles, ensuring precise segmentation. Furthermore, the maximum (Dmax) and minimum (Dmin) diameter locations and their amplitudes are monitored, and JV distension is calculated as their difference. From the host of acquired beat-to-beat JVP cycles, a minimum of 10 JVP cycles are selected, corresponding to the highest correlation coefficient and cycle quality for JVP contour feature assessment.
To classify the morphology of the JVP waveform in relation to cardiac abnormalities, it is crucial to assess the amplitude, location, and ratio between the key JVP waveform features. Our approach to JVP contour assessment relies on the inbuilt LabVIEW peak-valley detection algorithm, which fits individual JVP cycles into sequential groups of data points, and each fit is compared against the threshold value. The number of data points in a fit, and the threshold parameters are standardized through several iterations on multiple cycles and based on the literature data on the ideal JVP cycle. The algorithm detects waveform characteristics by identifying peak and valley locations, allowing us to compute amplitude ratios and time intervals to assess morphological variations. Beat-to-beat values of JVP characteristic features for the selected JVP cycles are computed and recorded. The schematic of the primary blocks of the designed automated cycle segmentation and pulse contour identification algorithm is illustrated in Fig. 8 (d).
Statistical analysis
All the measurement variables are represented as mean ± standard deviation. The agreement between the proposed system and the reference approach was investigated through the Bland-Altman (BA) representations indicated by the bias and confidence interval (Bias ± 1.96 Standard Deviation). Logistic regression analysis was performed to compare the JV diameter values obtained using the proposed and reference techniques. The correlation between two variables was reported using Pearson’s correlation coefficient (r), and their statistical significance is represented using the p-value. Paired student t-test for means was used to deduct the significance of measurement differences, where the significance level α = 0.05 was chosen for these null-hypothesis tests. The accuracy of the developed automated cycle segmentation and contour feature identification algorithms were quantified in terms of sensitivity and hit rate analysis. The sensitivity of these algorithms was evaluated by calculating the proportion of true positives (correctly identified contour features) against all instances where the feature was present. This approach helped assess the system’s accuracy in detecting JVP features and segmenting the cycles. All the statistical analyses were performed using the GraphPad Prism software (version 9, GraphPad Prism, San Diego USA).
Data availability
The paper contains all pertinent data and analyses. While the datasets produced during the study are not publicly available, they can be obtained from the corresponding author upon reasonable request.
Change history
11 June 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41598-025-05436-9
References
Lewis, T. Remarks on early signs of cardiac failure of the congestive type. Br. Med. J. 849–852 (1930).
Ranganathan, N. & Sivaciyan, V. Jugular venous pulse descent patterns: recognition and clinical relevance. CJC Open. 5, 200–207 (2023).
Mackenzie, J. The venous and liver pulse and the arhythmic contraction of the cardiac cavities. J. Pathol. Bacteriol. 2, 1894, pp. 84–154, 273–345.
Applefeld, M. M. The Jugular Venous Pressure and Pulse Contour. In Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Butterworths; Boston: (1990).
Ranganathan, V. S. N. & Saksena, F. B. The Art and Science of Cardiac Physical Examination. Totowa, New Jersey, USA: Humana Press Inc., vol. 30, pp. 141–210, (2006).
Conn, R. D. & O’keefe. Simplified Evaluation of the Jugular Venous Pressure: Significance of Inspiratory Collapse of Jugular Veins. Mo Med. 2012 Mar-Apr;109(2):150-2.
Brennan, J. M. et al. A comparison by medicine residents of physical examination versus Hand-Carried ultrasound for Estimation of right atrial pressure. Am. J. Cardiol. 99, 1614–1616 (2007).
Smith, R. N. & Nolan, J. P. Central venous catheters. BMJ (Online) vol. 347 (2013).
Magder, S. Central venous pressure monitoring. Curr. Opin. Crit. Care. 12, 219–227 (2006).
Mcgee, D. C. & Gould, M. K. Preventing Complications of Central Venous Catheterization. n engl j med vol. 12 www.nejm.org (2003).
Amelard, R. et al. Non-contact hemodynamic imaging reveals the jugular venous pulse waveform. Sci. Rep. 7, (2017).
García-López, I. & Rodriguez-Villegas, E. Extracting the jugular venous pulse from anterior neck contact photoplethysmography. Sci. Rep. 10, (2020).
Conroy, T. B., Zhou, J. & Kan, E. C. Jugular venous pulse waveform extraction from a wearable radio frequency sensor. IEEE Sens. J. 23, 10140–10148 (2023).
Amelard, R. et al. Optical hemodynamic imaging of jugular venous dynamics during altered central venous pressure. IEEE Trans. Biomed. Eng. 68, 2582–2591 (2021).
Zamboni, P. et al. Central venous pressure Estimation from ultrasound assessment of the jugular venous pulse. PLoS One 15, (2020).
Jaffe, A., Goryachev, I., Sodini, C. & Anthony, B. W. Central venous pressure Estimation with force-coupled ultrasound of the internal jugular vein. Sci. Rep. 13, (2023).
George, N. R. et al. Jugular Venous Diameter Measurement Using A-Mode Ultrasound: A Feasibility Study. IEEE Int. Symp. Med. Meas. Appl. MeMeA 2023 - Conf. Proc. 1–6 (2022).
George, N. R. et al. A pilot observational cohort study to investigate the effect of Valsalva maneuver on internal jugular venous diameter. Proc. Ann. Int. Conf. IEEE Med. Biol. Soc. (2023).
Bercoff, J. Ultrafast Ultrasound Imaging. www.intechopen.com
Luo, J., Li, R. X. & Konofagou, E. E. Pulse wave imaging of the human carotid artery: an in vivo feasibility study. IEEE Trans. Ultrason. Ferroelectr. Freq. Control. 59, 174–181 (2012).
Cikes, M., Tong, L. & Sutherland, G. R. & D’hooge, J. Ultrafast Cardiac Ultrasound Imaging Technical Principles, Applications, and Clinical Benefits. J Am Coll Cardiol Img. (8) 812–823 (2014).
Bhaktwani, A. The PC-PNDT act in a nutshell. Indian J. Radiol. Imaging. 22, 133–134 (2012).
Proto, A., Conti, D., Menegatti, E., Taibi, A. & Gadda, G. Plethysmography System to Monitor the Jugular Venous Pulse: A Feasibility Study. Diagnostics 11, (2021).
Lam, P. et al. Non-contact quantification of jugular venous pulse waveforms from skin displacements. Sci. Rep. 8, (2018).
Chua Chiaco, J. M. S., Parikh, N. I. & Fergusson, D. J. The Jugular Venous Pressure Revisited. Cleveland Clinic Journal of Medicine vol. 80 638–644 Preprint at (2013). https://doi.org/10.3949/ccjm.80a.13039
Wagner, D. R. et al. Comparison of A-mode and B-mode ultrasound for measurement of subcutaneous fat. Ultrasound Med. Biol. 46, 944–951 (2020).
Menegatti, E. et al. Human internal jugular valve M-mode ultrasound characterization. Curr. Neurovasc Res. 11, 149–155 (2014).
Pellicori, P. et al. Prognostic significance of Ultrasound-Assessed jugular vein distensibility in heart failure. Heart 101, 1149–1158 (2015).
Wang, C. et al. Monitoring of the central blood pressure waveform via a conformal ultrasonic device. Nat. Biomed. Eng. 2, 687–695 (2018).
George, N. R. et al. Wearable Accelerometer System for Jugular Venous Pulse Quantification: A Pilot Study. 2024 IEEE Int. Symp. Med. Meas. Appl. MeMeA (2024).
Suzuki, S., Hoshiga, M., Kotani, K. & Asao, T. Assessment of Non-Contact measurement using a microwave sensor to jugular venous pulse monitoring. J. Biomed. Sci. Eng. 14, 94–102 (2021).
Moço, A., Hamelmann, P., Stuijk, S. & De Haan, G. The Importance of Posture and Skin-Site Selection on Remote Measurements of Neck Pulsations: An Ultrasonographic Study. (2018).
McGee, S. R. Physical examination of venous pressure: a critical review. Am. Heart J. 136 (Issue1), 10–18 (1998).
Devine, P. J., Sullenberger, L. E., Bellin, D. A. & Atwood, J. E. Jugular venous pulse: window into the right heart. South. Med. J. 100 (10), 1022–1027 (2007).
Acknowledgements
The authors wish to acknowledge the researchers of ACT lab -IIT Madras and the staff and engineers of HTIC-IIT Madras, Chennai, India, who provided technical support for the study.
Author information
Authors and Affiliations
Contributions
N.R.G contributed towards conceptualization, methodology, software, study design, data collection, formal analysis, investigation, validation, visualization, and manuscript preparation. R.M. contributed to methodology, review, and editing. K.V.R contributed towards software, supervision and formal analysis. P.M.N. contributed to project administration, conceptualization, resources, review, and editing. M.S. contributed towards funding acquisition, project, and resource administration. J.J. contributed to conceptualization, methodology, project administration, review, and editing. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in the name of Mohanasankar Sivaprakasam, which was incorrectly given as Mohanasankar Sivapraksam.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
George, N.R., Nabeel, P.M., Raj, K.V. et al. Single-element ultrasound system for high-resolution jugular venous pulse contour detection. Sci Rep 15, 13902 (2025). https://doi.org/10.1038/s41598-025-98943-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-98943-8