Abstract
Cell cycle protein E2 (CCNE2) is a member of the Cyclin family, known for driving tumor cell proliferation and invasion. However, the mechanism of its action in head and neck squamous cell carcinoma (HNSCC) remains unclear. The aim of this study is to investigate the relationship between CCNE2 and cisplatin resistance and survival prognosis of head and neck squamous cell carcinoma. We performed transcriptomic sequencing of HNSCC and HNSCC/DDP. Kaplan-Meier analysis and COX regression analysis were used to evaluate the relationship between CCNE2 expression and survival prognosis of HNSCC patients. Multiple potential biological functions of CCNE2 in HNSCC were identified using Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG). Single-sample gene set enrichment analysis (ssGSEA) was used to explore tumor immune infiltration. The potential mechanism of CCNE2 was explored by molecular docking and immunoprecipitation. Cell migration, cell invasion and cell proliferation assays were used to investigate the mechanism of CCNE2 in HNSCC. CCNE2 is up-regulated in HNSCC tissues and cell lines and is associated with poor prognosis. The high expression of CCNE2 in HNSCC is associated with clinical significance. GO and KEGG analysis showed that ccne2 related genes may be involved in the regulation of DNA double-strand break repair and DNA metabolic process. CCNE2 expression was positively correlated with the infiltration levels of helper T cells, Tcm cells and Th2 cells, and negatively correlated with the infiltration levels of DC, neutrophils and pDC. CCNE2 regulates the invasion, migration and proliferation of HNSCC cells by targeting MNAT1. CCNE2 also altered cisplatin resistance in HNSCC/DDP. CCNE2 may be an independent prognostic biomarker of HNSCC through MNAT1, which provides new ideas for cisplatin resistance and therapeutic targets of HNSCC.
Similar content being viewed by others
Introduction
Head and neck squamous cell carcinoma (HNSCC) is a heterogeneous group of tumors arising from the mucosal epithelium of the oral cavity, pharynx and larynx1. Approximately 890,000 new cases are diagnosed every year, resulting in 450,000 deaths, accounting for 4.5% of all cancer diagnoses and deaths worldwide2.The main risk factors include heavy alcohol consumption, smoking and human papilloma virus (HPV) infection3.The current standard treatments for HNSCC involve a combination of surgery, chemotherapy and radiotherapy. Cisplatin-based chemotherapy is considered the mainstay of treatment for patients with advanced HNSCC. Furthermore, current strategies for assessing response to chemotherapy and prognosis are limited and prone to relapse4. Therefore, there is an urgent need to develop a strategy to identify patients who respond to chemotherapy and to improve chemotherapy sensitivity in HNSCC.
The cell cycle protein E2 (CCNE2) gene, located at 8 q22. 1, encodes the CCNE2 in human, which regulates the G1/S transition5. CCNE2 plays a crucial role in process cell biology, promoting DNA replication and activating cyclin-dependent kinase 2 (CDK2), as well as being involved in cell division6.Growing evidence indicates that CCNE2 functions as a proto-oncogene in cancer. For example, Liu’s study found that CCNE2 can promote the development of thyroid cancer7, while Wang’s team found that KIF20A and CCNE2 inhibit non-small cell cancer progression through the PI3K/AKT pathway8.Yang found that downregulation of CCNE2 inhibited cell proliferation, migration and invasion9, and Wander reported a strong association between CCNE2 and acquired drug resistance10. However, the specific roles and underlying mechanisms of CCNE2 in HNSCC development and progression remain unclear.
In addition, Menage a trois 1(MNAT1), cyclin-dependent kinase 7 (CDK7) and Cyclin H together form cyclin-dependent kinase activated kinase (CAK)11.MNAT1 was a switch for CAK activation. Studies have shown that MNAT1 regulates the proliferation, migration and cell cycle of lung cancer cells through the Akt/p21 pathway, and is involved in the development of non-small cell lung cancer12.Qiu found that MNAT1 participated in osteosarcoma development through the PI3K/Akt/mTOR pathway and can affect chemotherapy sensitivity to DDP13.Wang found that has-circ-0001146/miR-26a-5p targets and regulate MNAT1 to control the migration, invasion and apoptosis of osteosarcoma14.However, the regulatory mechanism of MNAT1 in the progression of head and neck cancer remains unexplored.
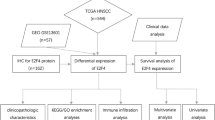
In this study, we screened differentially expressed genes based on RNA-Seq and constructed a cisplatin resistance marker model of head and neck squamous cell carcinoma. We used multiple datasets and experiments with clinical samples to predict and validate CCNE2 as a key factor among the markers. We examined the relationship between CCNE2 expression and survival outcomes in HNSCC patients, and through enrichment and protein-protein interaction (PPI) network analysis, we determined the correlation and biological significance of immune cells infiltrating with CCNE2. Furthermore, we found CCNE2 directly interacts with MNAT1 in HNSCC. Our study proposes a potential link between CCNE2 expression and MNAT1, which may affect HNSCC cisplatin resistance, prognosis, and immunological significance.
Materials and methods
Cell culture
TU212 (iCell Bioscience Inc, China), AMC-HN-8(BeNa Culture Collection, China), and HBE135-E6E7 (iCell Bioscience Inc, China) cells were maintained in Dulbecco’s Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 100 U/mL penicillin, and 100 mg/mL streptomycin. TU686 (iCell Bioscience Inc, China) cells were cultured in Roswell Park Memorial Institute (RPMI) 1640 medium. Growth was maintained at 37 ℃ and 5% CO2, and the medium was changed regularly to maintain optimal growth conditions. The cell lines were checked for mycoplasma using the BeyoDirect™ Mycoplasma qPCR Detection reagent, and the results showed that none of the cells were mycoplasma free.
Construction of cisplatin-resistant strains
Cisplatin concentrations were exposed to HNSCC cells starting at low concentrations. After each exposure, the cells were allowed to restore in the conventional medium, until they show the normal growth and achieve expected levels of resistance (5 µg/mL cisplatin). The cisplatin-resistant cells were named HNSCC/DDP. This was followed by conventional cultured cells.
Cell viability assay
Cells from different groups were seeded separately in 96-well plates. Primary and cisplatin-resistant cell lines were treated with progressively increasing concentrations of cisplatin after 24 h. Cell proliferation assay was performed using 10% CCK8 medium to compare cell viability to verify cisplatin resistance.
Transcriptomic experiment
HNSCC cell lines and HNSCC/DDP cell lines were collected and transferred to EP tubes containing TRIZOL. Samples were then flash frozen in liquid nitrogen for 30 min. RNA sequencing services were provided by GENE DENOVO(China).
Database source and processing
We extracted Gene Expression and clinical data of HNSCC patients from multiple databases, including The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO) and UALCAN databases. RNA-seq data is used to analyze CCNE2 and MNAT1 expression level. All data were standardized after download, including removal of low-quality samples and batch effect correction. Data processing and analysis were performed using relevant packages in the R language, such as DESeq2 for differential expression analysis and edgeR for standardized processing.
Patient and clinical samples
From September 2022 to August 2023, a total of 26 pairs of laryngeal cancer tissues and para-cancer tissues were collected from LSCC patients who underwent partial or total laryngectomy in the Second Hospital of Harbin Medical University (Harbin, China). All patients were initially diagnosed with laryngeal squamous cell carcinoma and underwent total or partial laryngectomy with or without neck dissection. No preoperative chemotherapy or radiotherapy was performed. All samples were pathologically confirmed and stored in a − 80 ℃ freezer until further processing. This study was approved by the Ethics Committee of Harbin Medical University (YJSKY2022-057).
Cell transfection
Lipo8000™ transfection reagent (Beyotime, China)4 µl mixed with 2.5 µg of plasmid and 100pmol stained small interfering RNA were added to 125 µl Opti-MEM medium, mixed gently, incubated for 20 min and added to 6-well plates. Transfected cells were cultured for 48 h at 37 ℃ in a 5% CO2 environment for subsequent experiments. The siRNA sequences are listed in table S1 in the Supplementary material.
Immunohistochemistry
Collected tissue samples were fixed in 4% paraformaldehyde, dehydrated and embedded in paraffin, cut into 4 μm thick sections, and dried at 37 ℃ before deparaffinized before antigen repair. The proteins were blocked with goat serum and purified with primary antibody (CCNE2, 1:200; SC-28351, SANTA; MNAT1, 1:200; SC-131442, SANTA) were incubated overnight at 4 ℃ and with biotinylated secondary antibody (goat anti-mouse) for 1 h at 20℃. Finally, color was developed with DAB, counterstained with hematoxylin, dehydrated and sealed.
Quantitative real-time PCR
Authentic time-quantitative polymerase chain reaction (RT-qPCR) total RNA was extracted from tissues and cells using TRIzol (Invitrogen, USA) and reverse transcribed using the PrimeScript RT kit (Roche, Switzerland). Then, using FastStart Universal SYBR green Master (Roche, Switzerland), with GAPDH as internal controls, RT - qPCR repeated three times. The relative expression of targets was calculated using the 2-ΔΔCt method. Primers used for RT-qPCR are listed in table S2.
Transwell invasion
Cells were suspended in 200 µL of FBS-free medium and seeded in an upper chamber precoated with 50 µL Matrigel Matrix (BD Biosciences). The chambers were then placed into 24-well plates, of which 700 µL medium containing 20% FBS/hole. After 24 h of incubation, the cells were fixed with 4% paraformaldehyde and the chambers were stained with 0.1% crystal violet.
Co-immunoprecipitation (Co-IP) assays
Cells were lysed on ice for 30 min, and supernatants were collected by centrifugation of lysates at 14,000 ×g at 4 ℃ to estimate protein concentration. Co-immunoprecipitation was performed using protein A + G magnetic beads, which were resuspended with MNAT1 antibody and incubated for 1 h at 24 ℃. The supernatant was discarded by centrifugation, the protein sample was added, and the mixture was incubated overnight at 4 ℃ on an oscillator. Finally, the precipitate was washed and boiled with SDS for 5 min at 95 ℃. Supernatant by western blot analysis.
Analysis of tumor immune infiltration
From TCGA database (https://portal.gdc.cancer.gov) to download and organize TCGA - HNSCC project STAR process of RNAseq data and extract the TPM format of the data and clinical data. Remove normal + Remove no clinical information Filter out useless data. Single-sample gene enrichment analysis (ssGSEA) algorithm based on R package-GSVA15 and TIMER database were used to calculate the relationship between the corresponding CCNE2 and immune cell infiltration by using the markers of immune cells provided by Immunity article.
GO and KEGG enrichment analysis
Enrichment analysis of the selected DEGs was performed using the enrich GO function and enrich KEGG function of Cluster Profiler package (table S3). The significant (p < 0.05) pathways were selected for enrichment, and the ggplot2 package was used to plot the GO bar chart and bubble chart. The Pathview package was used to visualize the significant KEGG pathways and show the distribution of genes in each path16.
Protein interaction network and module analysis
The selected DEGs were input into the STRING database (https://string-db.org/). Set the minimum confidence is 0.4, extraction of PPI network data. Cytoscape software was used to import PPI network data for network visualization and analysis (table S4).
Molecular docking
Using AlphaFold 3 prediction of protein and protein interactions. Pymol v2.3.4 was used to analyze the predicted structure, and the amino acid pairs that could interact with each other to form hydrogen bonds were obtained. The predicted polymer structure was analyzed using PRODIGY, and the binding energy formed between proteins was obtained to be -10 kcal/mol.
Multiple immunofluorescence
Paraffin sections were dehydrated after baking and blocked with repair antigen and serum. The primary antibody (CCNE2, 1:200; SC-28351, SANTA; MNAT1, 1:200; SC-131442, SANTA) were blocked overnight at 4℃ and then incubated with the corresponding secondary antibody at room temperature for 30 min. Photographs were taken after 5 min of Hoechst staining.
Cell migration assay
Cells were spread into 6-well plates 24 h in advance for knockdown and overexpression of the corresponding genes. Cells were allowed to grow for 48 h before being photographed by scratching with the tip of a gun. Twenty-four hours after the addition of serum-free medium, photographs were taken and counted.
Electron microscopy experiments
Cells were fixed with 5% glutaraldehyde, washed with orthophosphoric acid, and fixed in trichrome tetroxide. After dehydration with ethanol and acetone, the plates were fixed in SPUSE resin, and the sections were stained and photographed.
EdU experiments
Knockdown and overexpression of the corresponding genes were performed after cells were seeded in 96-well plates overnight. After 48 h, 1:500 EdU100Μl/ well was added and incubated for 2 h. Fixed, rinsed, and Click reaction solution was used in the dark for 15 min at room temperature. Images were taken after rinsing and staining with Hoechst for 5 min.
Statistic analysis
Statistical analyses and plots were performed with the use of the R package, version 4.2.1. CCNE2 and MNAT1 expression in unpaired and paired samples were analyzed using the Wilcoxon rank-sum test and Wilcoxon signed-rank test, respectively. ROC analysis was performed using the pROC (1.18.0) and ggplot2[3.3.6] packages, respectively. The expression levels of CCNE2 and MNAT1 were analyzed by querying GEO, TIMER and UALCAN databases. Using KM method, we compared the TCGA CCNE2 high expression and CCNE2 low expression, MNAT1 high expression and MNAT1 lower expression differences of patients. Cox regression analysis was used to analyze the correlation between CCNE2 and MNAT1 expression and clinical characteristics. A p value of less than 0.05 was considered to indicate significance.
Results
CCNE2 expression in cisplatin-resistant cell lines and HNSCC
Stable cisplatin-resistant head and neck squamous cell carcinoma cells were established after 8 months of cisplatin induction (Fig. 1A). As shown in table S5, we found 610 differentially expressed genes between HNSCC and HNSCC/DDP by transcriptome sequencing (log₂ Fold Change > 1 or log₂ Fold Change < -1, p < 0.05). Our query to the DDR (DNA Damage Response) gene list had 69 genes (http://www.gsea-msigdb.org/gsea/msigdb/cards/WP_DNA_DAMAGE_RESPONSE.html). We can get 10 genes by taking their intersection, which are: CDKN1A, GADD45A, ABL1, BBC3, MRE11, MYC, GADD45B, PML, CYCS, CCNE2 (Fig. 1B, C and table S6). In transcriptome sequencing of HNSCC and HNSCC/DDP, we identified three low and seven high expression DDR genes. The expression levels of these 10 genes in different malignant tumors were evaluated by analyzing the TCGA database. Data from TCGA showed that high CCNE2 expression in HNSCC (Fig. 1D). Further analysis of GEO datasets GSE142083 and GSE127165 confirmed that high CCNE2 expression in HNSCC (Fig. 1E, F). To validate this finding, we performed RT-qPCR on 26 pairs of HNSCC and adjacent tissues, which showed that CCNE2 was significantly over-expressed in HNSCC (Fig. 1G). RT-qPCR of human bronchial epithelial cells ( HBE135-E6E7) and HNSCC cells (TU686, TU212, AMC-HN-8) also confirmed high expression CCNE2 in HNSCC cell lines (Fig. 1H). Kaplan-Meier survival curve analysis demonstrated that high CCNE2 expression was significantly associated with poor prognosis in HNSCC patients (Fig. 1I). To evaluate the potential of CCNE2 as a diagnostic marker for HNSCC, we constructed a receiver operating characteristic (ROC) curve, showing an area under the curve (AUC) of 0.818, indicating significant diagnostic value (Fig. 1J).
CCNE2 was up-regulated in HNSCC. (A) The IC50 of TU212, AMC-HN-8, TU686, AMC-HN-8/DDP, TU212/DDP and TU686/DDP cells were detected. (B) Intersection of DDR genes and HNSCC + HNSCC/DDP transcriptome sequencing. (C)Volcano plot of differentially expressed genes. (D) TCGA database analysis of CCNE2 expression in HNSCC tissues. (E,F) GEO database analysis of CCNE2 expression in HNSCC tissues. (G) RT-qPCR determination of CCNE2 mRNA expression levels in HNSCC and normal tissues (n = 26). (H) CCNE2 expression level of RT - qPCR in TU686 TU212, AMC - HN − 8 and HBE135-E6E7 cell lines. (I) Survival curves between CCNE2 high and CCNE2 low patients with HNSCC. (J) ROC curve was established to investigate the value of CCNE2 in identifying HNSCC tissues. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
Relationship between CCNE2 expression and clinical features
Using the UALCAN database for subgroup analysis of various pathological features, we found that CCNE2 transcript levels were significantly increased in HNSCC patients (Fig. 2A). Subgroup analysis by TP53 mutation status, cancer stages, race, age, tumor grade, nodal metastasis status, HPV status showed that CCNE2 expression was significantly higher in HNSCC patients than in the normal group (p < 0.05; Table S7, Fig. 2B–H). Logistic regression analysis showed that CCNE2 expression in HNSCC was significantly correlated with histological grade (OR of G3 and G4 vs. G1 and G2 = 1.704, p = 0.012), while no significant associations were found with age, M stage, T stage, N stage, smoking, alcohol consumption, lymph node metastasis, or sex (Table S8). Further validation using TCGA data (Table S9) confirmed the association of high CCNE2 expression with neck lymph node dissection (p = 0.02) and clinic pathological features (p = 0.01).
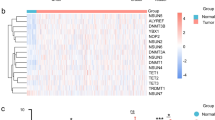
CCNE2 patient subgroups enrichment gene transcription and correlation analysis. (A) CCNE2 box plot in normal and HNSCC tissues. (B) CCNE2 box plot of normal individuals and TP53 mutation status. (C) CCNE2 box plots of normal individuals and individual cancer stages. (D) CCNE2 box pattern plots of normal individuals and patients of different races. (E) CCNE2 box plots for each age group of normal individuals and patient age. (F) CCNE2 box plot of normal individuals and tumor grade. (G) CCNE2 box plot of normal individuals and different lymph node metastasis status. (H) of normal individuals and HPV CCNE2 box figure. (I) Intersection of CCNE2-related genes, HNSCC-HNSCC DDP resistance differential genes and DDR genes. (J) Heat map of expression of genes associated with CCNE2 in normal patients and HNSCC. (K) PPI network enrichment analysis network diagram constructed based on STRING dataset. (L) Top 8 genes in PPI network. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
PPI network analysis
As shown in Table S10, we divided CCNE2 expression in head and neck squamous cell carcinoma into high and low expression groups based on DESeq2 process for differential analysis, and obtained 5529 differentially expressed genes. At the same time, we found that DNA damage repair genes (DDR Genes)17 contained 276 genes. DDR Genes were intersected with CCNE2 related genes and HNSCC-HNSCC/DDP differential genes to obtain 38 genes (Fig. 2I). The heatmap shows the expression of 38 genes in healthy and HNSCC patients (Fig. 2J). The PPI network of co-expressed genes eligible for STRING was assembled and visualized using Cytoscape, and the interactions among the 38 DEGs in the HNSCC group were analyzed. The Linkedomics functional module was used to perform GO and KEGG pathway co-expression analysis of 38 genes in HNSCC mRNA sequencing data from 548 patients from TCGA. A total of 219 interactions were identified among the 38 proteins (Fig. 2K; Table S11). Finally, we screened the top eight hub genes: CCNE2, MNAT1, RRM1, FEN1, TTK, PCNA, RFC3, and CHEK1 (Fig. 2L).
GO and KEGG enrichment analysis
We performed enrichment analysis using GO and KEGG databases to explore the biological functions of CCNE2-related differential genes (DEGs) in HNSCC (Fig. 3A, B). GO analysis showed that these DEGs were related to biological processes (BP), cellular components (CC), and molecular functions (MF). DEGs were enriched in multiple biological pathways, including double-strand break repair, regulation of DNA metabolic processes, DNA repair, chromosomal region, chromosome, telomeric region, replication fork, and catalytic activity. KEGG analysis showed enrichment in the Fanconi anemia pathway, base excision repair, and mismatch repair. These findings indicate that high CCNE2 expression is closely associated with various biological processes, such as DNA repair and cell cycle regulation. Previous studies have shown that patients undergoing chemotherapy exhibit high levels of persistent DNA damage, supporting the potential role of CCNE2 as a biomarker for HNSCC and its importance as a target for chemotherapy18,19.
CCNE2 enrichment analysis and CCNE2 biological function center gene expression and heat map. (A,B) Bubble plot and chord diagram based on GO/KEGG analysis of CCNE2-related genes. (C–I) Scatter plot of the relationship between CCNE2 and seven related hub genes. (J) Heatmap of co-expression of screened genes and CCNE2 genes in HNSCC patients. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
Roles of CCNE2 and DNA loss repair factors in HNSCC
The repair of DNA damage affects the development and recurrence of HNSCC20. We intersected CCNE2 expression with DNA damage repair factors reported in the literature, identifying 7 genes: MNAT1, RRM1, FEN1, TTK, PCNA, RFC3, and CHEK1. CCNE2 expression was strongly correlated with the expression of these genes involved in DNA damage repair in HNSCC (Fig. 3C–I). Analyzing the differences in DNA damage repair genes between the high and low CCNE2 expression groups in HNSCC patients revealed that the expression levels of all genes were upregulated in the high CCNE2 expression group (Fig. 3J, Table S12). This demonstrates a clear relationship between DNA damage repair and CCNE2 expression levels in HNSCC.
Relationship between CCNE2 expression and immune cell infiltration
Using the ssGSEA method, we verified the close relationship between CCNE2 and immune cells (Fig. 4A). The results showed that CCNE2 expression a positively correlated with Th2 cells, T helper cells, and Tcm cells (p < 0.001), and negatively correlated with pDC, DC, and neutrophils (p < 0.001) (Fig. 4B–G). The TIMER database was used to examine the association between CCNE2 expression in HNSCC tissues and immune cell infiltration levels, showing that CCNE2 was associated with B cells, CD8-positive T cells, CD4-positive T cells, and dendritic cell infiltration (Fig. 4H). The infiltration of T helper cells, Tcm, Tem, and Th2 cells increased in the high CCNE2 expression group (p < 0.05), while the infiltration of DC, iDC, mast cells, neutrophils, NK CD56dim cells, and pDC decreased (p < 0.05) (Fig. 4I). These results confirm that increased CCNE2 expression in HNSCC is closely related to immune cell infiltration, suggesting a significant role for CCNE2 in the immune microenvironment of HNSCC.
Relationship between CCNE2 expression and microenvironment of immune infiltrating cells in HNSCC. (A) Forest plots depicting the relationship between CCNE2 expression level and the relative abundance of 24 immune cells. (B–G) scatterplot, shows the high and low CCNE2 expression between groups of T helper cells, Th 2 cells, Tcm cells, pDC, DC, the degree of differentiation of Neutrophils. (H) CCNE2 expression was correlated with the degree of immune cell infiltration by SCNA. (I) Scatter plot showing the correlation between the 24 immune cells and CCNE2 expression levels. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
MNAT1 is upregulated in HNSCC
Previous studies have identified 7 DNA damage repair genes closely related to CCNE2. MNAT1 gene was evaluated using the TCGA database, showing increased expression in various cancers, including HNSCC (Fig. 5A). MNAT1 upregulation in HNSCC was also confirmed in GEO datasets GSE127165 and GSE142083 (Fig. 5B, C). Data from TCGA showed that high MNAT1 expression in HNSCC (Fig. 5D). RT-qPCR analysis verified that MNAT1 was significantly upregulated in HNSCC cell lines compared to human bronchial epithelial cells ( HBE135-E6E7) (Fig. 5E). Kaplan-Meier survival curve analysis showed that increased MNAT1 expression levels were significantly associated with poor prognosis in HNSCC patients (Fig. 5F). ROC curve analysis showed an AUC of 0.866, indicating significant diagnostic value for MNAT1 in HNSCC (Fig. 5G).
The expression level of MNAT1 in HNSCC was validated in TCGA and GEO databases and in vitro experiments. (A) Comparison of MNAT1 expression levels in different cancer tissues and normal tissues. (B,C) CEO database analysis of MNAT1 expression in HNSCC tissues. (D) TCGA database analysis of MNAT1 expression in HNSCC tissues. (E) MNAT1 expression level of RT - qPCR in TU686, TU212, AMC - HN − 8 and HBE135-E6E7 cell lines. (F) Survival curves between patients with high MNAT1 and those with low MNAT11 in HNSCC patients. (G) ROC curve was established to investigate the value of CCNE2 in identifying HNSCC tissues. * p < 0.05 * * p < 0.01 * * * p < 0.001 ****p < 0.0001.
CCNE2 and MNAT1 jointly affect the progression of HNSCC
PRODIGY analysis predicted the multimer structure and binding energy between CCNE2 and MNAT1, with a binding energy of -10 kcal/mol, suggesting a possible molecular interaction (Fig. 6A). Immune co-precipitation confirmed a potential direct interaction between MNAT1 and CCNE2 (Fig. 6B). Immunofluorescence staining showed that HNSCC tissues with high CCNE2 expression also had high MNAT1 expression and vice versa (Fig. 6C).
The interaction between CCNE2 and MNAT1 and its effect on HNSCC were verified in vitro. (A) Predicted interaction between MNAT1 protein and CCNE2 protein, mnat1 protein in yellow, Blue is ccne2 protein. (B) Co-IP of MNAT1 with CCNE2 in AMC-HN-8. (C) CCNE2 expression in high/low MNAT1 expressing LSCC tissues was analysed using mIHC assays. 200×. (D) The knockdown efficiency of CCNE2 was determined by RT-qPCR. (E) Transmission electron microscopy was used to observe the changes of mitochondria in HNSCC. (F)RT-qPCR was used to detect the efficiency of MNAT1 overexpression. (G–I)The effects of CCNE2-KD and MNAT1-OE on the migration of HNSCC cells were detected by wound healing assay.*p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
To further investigate the effect of CCNE2 on the behavior of HNSCC cells, we transfected CCNE2 knockdown (CCNE2-KD) into HNSCC cells. RT-qPCR results showed that the mRNA expression of CCNE2 was significantly decreased after knockdown (Fig. 6D). To further clarify the role of CCNE2 in suppressing mitochondria in HNSCC, we found that CCNE2 knockdown cells exhibited reduced mitochondrial volume and increased mitochondrial membrane density under projection electron microscopy (Fig. 6E).
To further investigate the effect of MNAT1 on the behavior of HNSCC cells, HNSCC cells were transfected with MNAT1 overexpression (MNAT1-OE). RT-qPCR results showed that the mRNA expression of NMAT1 was significantly increased after overexpression (Fig. 6F). Cell migration assay showed that CCNE2 knockdown attenuated cell migration ability compared with the control group, and this phenomenon was ameliorated by simultaneous overexpression of MNAT1 (Fig. 6G–I). Next, we will separately treat HNSCCS for 48 h and examine the changes in cell viability by EdU in each group. We found that knockdown of CCNE2 suppressed cell proliferation rate of HNSCC, while overexpression of MNAT1 ameliorated this inhibitory effect (Fig. 7A, B).
CCNE2 regulates HNSCC proliferation, invasion and cisplatin resistance through MNAT1. (A,B) EdU assay was used to detect the proliferation of HNSCC after CCNE2-OE and MNAT1-KD. (C,D) The cisplatin-resistance of HNSCC/DDP after CCNE2-OE and MNAT1-KD was detected by immunofluorescence assay. (E,F) Transwell assay was used to detect the effects of CCNE2-OE and MNAT1-KD on HNSCC invasion. (G) Immunohistochemical analysis further validated the up-regulation of CCNE2 and MNAT1 in HNSCC tissues. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
Cisplatin can cause DNA damage, and γ-H2AX has been widely used as a sensitive marker of DNA damage. We performed immunofluorescence experiments after adding 5 µg/ ml cisplatin to the corresponding cell lines. We found that CCNE2 knockdown cells had increased DNA damage compared to controls, and that elevated MNAT1 ameliorated this phenomenon (Fig. 7C, D). Cell invasion assays revealed that CCNE2 knockdown reduced HNSCC invasiveness, while MNAT1 overexpression mitigated this effect (Fig. 7E, F). Finally, we performed IHC on the patient’s adjacent non-cancer tissues and head and neck squamous cell carcinoma tissues. We observed that both CCNE2 and MNAT1 were expressed higher in HNSCC tissues than in controls (Fig. 7G). Through clinical sample analysis and corresponding in vitro experiments, we explored that CCNE2 plays a key role in HNSCC progression and cisplatin resistance by targeting MNAT1 and exhibits synergistic effects.
Discussion
The treatment of head and neck squamous cell carcinoma includes surgery, radiotherapy, chemotherapy and other comprehensive treatment. Chemotherapy is one of the most effective treatments for advanced tumors, but increasing drug resistance is a major cause of cancer recurrence and treatment failure. Therefore, the discovery of novel therapeutic targets to overcome chemotherapy resistance is essential to establish an effective treatment for HNSCC patients. Cisplatin, one of the most potent and widely used chemotherapeutic agents for the treatment of solid tumors, is involved in DNA damage by forming covalent adducts with DNA. HNSCC is prone to relapse and metastasis after cisplatin resistance. In this study, transcriptome sequencing was performed on HNSCC and HNSCC/DDP, and the results showed that CCNE2 was low expressed in them. The role of CCNE2 in cisplatin resistance and metastasis and invasion of head and neck squamous cell carcinoma is not fully understood. Here, we present relevant evidence indicating that CCNE2 can target MNAT1 to modulate the development process of HNSCC in terms of cell growth, invasion, metastasis and cisplatin resistance, and coordinate the pathological processes related to DNA damage. First, CCNE2 alters the immune response of HNSCC. Second, CCNE2 enhanced the invasion, proliferation, migration and other abilities of HNSCC. Third, CCNE2 is closely related to DNA damage in HNSCC.
CCNE2 plays a crucial role in cell cycle regulation, mediating the transition from G1 to S phase by interacting with CDK21. We observed high expression of CCNE2 in HNSCC cell lines and tissue samples. The overexpression of CCNE2 was closely associated with the clinic pathological characteristics of HNSCC patients. ROC curve analysis demonstrated that CCNE2 serves as a promising diagnostic biomarker to distinguish HNSCC from normal tissues. In addition, Kaplan-Meier survival curve analysis showed that high CCNE2 expression correlates with poor prognosis in HNSCC patients. Although the exact mechanism of the effect of CCNE2 up-regulation on tumors requires further mechanistic study, the up-regulated CCNE2 has a significant effect on HNSCC.
It has been reported that CCNE2 plays an oncogenic role in different tumors through the PI3K/AKT pathway8. To elucidate the potential biological functions and regulatory pathways of CCNE2, we analyzed the genes encoding CCNE2-related proteins and co-expressed genes in HNSCC tissues. Analysis of TCGA mRNA sequencing data identified differentially expressed genes associated with ccne2. GO and KEGG enrichment analysis showed that these DEGs were involved in a variety of biological processes and signaling pathways. These include double-strand break repair, regulation of DNA metabolic processes, DNA repair, chromosomal region organization, chromosome maintenance, telomeric region dynamics, replication fork activity, catalytic function to DNA, impaired DNA binding, ATP-dependent DNA activity, Fanconi anemia pathway, base excision repair, and mismatch repair. These results suggest that CCNE2 may regulate cellular immune function and DNA damage repair processes through these pathways, thereby contributing to HNSCC progression. This is closely related to the role of the downstream gene MNAT1 of CCNE2 in cells. MNAT1 participates in the development of osteosarcoma through the PI3K/Akt/mTOR pathway and can affect the chemosensitivity to DDP13. Cytoscape software was used to construct the PPI network, and the core gene cluster was found to include CCNE2, MNAT1, RRM1, FEN1, TTK, PCNA, RFC3, and CHEK1. These key genes may play a key role in the pathogenesis and progression of HNSCC. Understanding the role of tumor-infiltrating inflammatory cells (TIICs) in the development and progression of is essential for developing novel therapies and prognostic tools22. TIICs significantly influence HNSCC prognosis by contributing to the tumor’s immunosuppressive environment and facilitating immune escape. HNSCC is characterized by intricate interactions between epithelial cells, blood vessels, lymphatic vessels, cytokines, chemokines, and infiltrating immune cells. Ting et al. developed a model predicting survival outcomes in HNSCC patients undergoing radiotherapy based on TIIC data within the tumor microenvironment23. TIICs promote a complex network of cell-cell interactions that enhance the immunosuppressive. T helper cells, essential for orchestrating immune response, play pivotal roles in infection, chronic inflammatory, autoimmune diseases, and carcinogenesis24. The pDCs, which produce type I interferon, modulate immune responses25.Our results showed that CCNE2 expression positively correlates with Th2 cells, T helper cells, and Tcm cells, but negatively correlates with pDC, DC, and neutrophils. TIMER database analysis indicated that CCNE2 expression is associated with levels of B cell, CD8-positive T cell, CD4-positive T cell, and dendritic cell infiltration. These findings suggest that CCNE2 plays an integral role in regulating immune cell infiltration in HNSCC. In addition, we found by transmission electron microscopy that reduction of mitochondrial volume and increase of mitochondrial membrane density occurred in HNSCC cells after CCNE2 knockdown.
To bridge these immunological observations with functional mechanisms, we delved into the results of transcriptome sequencing of HNSCC and HNSCC/DDP tissues. We found that MNAT1 expression was consistent with CCNE2 expression. We validated the high expression of MNAT1 in HNSCC cell lines and tissue samples. PRODIGY prediction suggested a direct interaction between CCNE2 and MNAT1. We demonstrated that CCNE2 and MNAT1 have correlated expression levels. For the regulatory relationship between CCNE2 and MNAT1, rescue experiments were performed. We found that overexpression of MNAT1 ameliorated CCNE2-induced invasion, migration and proliferation of HNSCC cells. Overexpression of MNAT1 rescued CCNE2-mediated DNA damage in HNSCC/DDP cells. CCNE2 is found to regulate the expression of MNAT1, which in turn influences the DNA damage response pathways involved in cisplatin resistance in HNSCC. This interaction is significant as it suggests that targeting MNAT1 could enhance the efficacy of cisplatin treatment by overcoming resistance mechanisms associated with CCNE2.In conclusion, the results obtained suggest that CCNE2 plays a role in HNSCC progression and resistance to cisplatin by targeting MNAT1.
Conclusions
Our study shows for the first time that CCNE2 promotes tumor invasion, proliferation and migration through the MNAT1 gene and is closely associated with cisplatin resistance, poor survival and immune infiltration in HNSCC. These findings provide new potential targets for the diagnosis and treatment of HNSCC.
Data availability
Data availability statementThe data that support the findings of this study are available on request from the corresponding author, Linli Tian, upon reasonable request.
References
Goel, B. et al. Therapeutic approaches for the treatment of head and neck squamous cell carcinoma-An update on clinical trials. Transl Oncol. 21, 101426 (2022).
Barsouk, A. et al. Risk factors, and prevention of head and neck squamous cell carcinoma. Med. Sci. (Basel) ; 11(2). (2023).
Haddad, R. I. et al. Nivolumab plus ipilimumab versus EXTREME regimen as First-Line treatment for recurrent/metastatic squamous cell carcinoma of the head and neck: the final results of checkmate 651. J. Clin. Oncol. 41 (12), 2166–2180 (2023).
Yu, C. et al. Current status and perspective of tumor immunotherapy for head and neck squamous cell carcinoma. Front. Cell. Dev. Biol. 10, 941750 (2022).
Fagundes, R. & Teixeira, L. K. Cyclin E/CDK2: DNA replication, replication stress and genomic instability. Front. Cell. Dev. Biol. 9, 774845 (2021).
Wu, Y. et al. Metformin targets a YAP1-TEAD4 complex via AMPKα to regulate CCNE1/2 in bladder cancer cells. J. Exp. Clin. Cancer Res. 38 (1), 376 (2019).
Liu, C. Z. et al. Clinical significance of CCNE2 protein and mRNA expression in thyroid cancer tissues. Adv. Med. Sci. 65 (2), 442–456 (2020).
Wang, Q., Wu, H., Wu, Q. & Zhong, S. Berberine targets KIF20A and CCNE2 to inhibit the progression of nonsmall cell lung cancer via the PI3K/AKT pathway. Drug Dev. Res. 84 (5), 907–921 (2023).
Yang, J. et al. Antibiotic Tigecycline inhibits cell proliferation, migration and invasion via down-regulating CCNE2 in pancreatic ductal adenocarcinoma. J. Cell. Mol. Med. 24 (7), 4245–4260 (2020).
Wander, S. A. et al. The genomic landscape of intrinsic and acquired resistance to Cyclin-Dependent kinase 4/6 inhibitors in patients with hormone Receptor-Positive metastatic breast Cancer. Cancer Discov. 10 (8), 1174–1193 (2020).
Yang, Z., Sharma, K. & de Lange, T. TRF1 uses a noncanonical function of TFIIH to promote telomere replication. Genes Dev. 36 (17–18), 956–969 (2022).
Chen, Y., Guan, J. X. & Shen, H. [MNAT1 expression in non-small cell lung cancer and its biological cellular impact]. Zhonghua Bing Li Xue Za Zhi. 48 (8), 626–632 (2019).
Qiu, C. et al. MNAT1 promotes proliferation and the chemo-resistance of osteosarcoma cell to cisplatin through regulating PI3K/Akt/mTOR pathway. BMC Cancer. 20 (1), 1187 (2020).
Wang, J. et al. The regulatory effect of has-circ-0001146/miR-26a-5p/MNAT1 network on the proliferation and invasion of osteosarcoma. Biosci. Rep. ; 40(6). (2020).
Yoshihara, K. et al. Inferring tumour purity and stromal and immune cell admixture from expression data. Nat. Commun. 4, 2612 (2013).
Yu, G., Wang, L. G., Han, Y. & He, Q. Y. ClusterProfiler: an R package for comparing biological themes among gene clusters. Omics 16 (5), 284–287 (2012).
Knijnenburg, T. A. et al. Genomic and molecular landscape of DNA damage repair deficiency across the Cancer genome atlas. Cell. Rep. 23 (1), 239–54e6 (2018).
van den Boogaard, W. M. C., Komninos, D. S. J. & Vermeij, W. P. Chemotherapy Side-Effects: not all DNA damage is equal. Cancers (Basel) ; 14(3). (2022).
Liu, J. et al. miR-302d targeting of CDKN1A regulates DNA damage and steroid hormone secretion in bovine cumulus cells. Genes (Basel) ; 14(12). (2023).
Psyrri, A. et al. The DNA damage response network in the treatment of head and neck squamous cell carcinoma. ESMO Open. 6 (2), 100075 (2021).
Liu, M. et al. Compound K is a potential clinical anticancer agent in prostate cancer by arresting cell cycle. Phytomedicine 109, 154584 (2023).
Vonderheide, R. H., Domchek, S. M. & Clark, A. S. Immunotherapy for breast cancer: what are we missing?? Clin. Cancer Res. 23 (11), 2640–2646 (2017).
Xu, T. et al. Developing and validating the model of tumor-infiltrating immune cell to predict survival in patients receiving radiation therapy for head and neck squamous cell carcinoma. Transl Cancer Res. 13 (1), 394–412 (2024).
Gagliani, N. & Huber, S. Basic aspects of T helper cell differentiation. Methods Mol. Biol. 1514, 19–30 (2017).
Lee, Y. J., Kim, Y., Park, S. H. & Jo, J. C. Plasmacytoid dendritic cell neoplasms. Blood Res. 58 (S1), 90–95 (2023).
Acknowledgements
We would like to express our heartfelt thanks to Tao Yang, Zhijie Li, Yu Zhang and Dong Wang for their valuable contributions to technical assistance.
Author information
Authors and Affiliations
Contributions
Ran An, Linli Tian and Ming Liu designed the project. Ran An and Xiaolin Xu performed the experiments. Yue Wang, Jiayi Ding and Boyu Li processed the data. Ran An and Fan Yang wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Statements relating to ethics and integrity policies
This study was approved by the ethics committee of Harbin Medical University (approval No. YJSKY2022-057). We certify that the study was performed in accordance with the 1964 declaration of HELSINKI and later amendments.
Patient consent statement
Written informed consent was obtained from all the participants prior to the enrollment of this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
An, R., Xu, X., Wang, Y. et al. CCNE2 promotes cisplatin resistance and affects prognosis of head and neck squamous cell carcinoma by targeting MNAT1. Sci Rep 15, 14011 (2025). https://doi.org/10.1038/s41598-025-98989-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-98989-8