Abstract
Autologous and allogeneic bone grafting is currently the clinical gold standard for the treatment of bone defects; however, it is limited by the scarcity of autologous sources and the risk of secondary trauma, as well as the complications of disease transmission and immune rejection associated with allogeneic grafts. The clinical management of bone defects remains a significant challenge. In this study, we prepared a demineralized bone matrix/gelatin methacrylate composite hydrogel loaded with deferoxamine (GelMA/DBM/DFO) using a freeze-drying method and investigated its properties. Assessments using CCK-8, live-dead fluorescence staining, alkaline phosphatase staining, and Alizarin Red staining indicated that the GelMA/DBM/DFO composite hydrogel demonstrated superior biocompatibility and in vitro osteogenic differentiation capacity compared with the GelMA/DBM composite hydrogel. We established a cranial defect model in Sprague–Dawley (SD) rats and examined peripheral blood indices, micro-computed tomography (Micro-CT), hematoxylin and eosin (HE) staining, Masson’s trichrome staining, and immunohistochemical staining for bone morphogenetic protein-2 (BMP-2) and collagen type I (COL-1). Both hydrogels exhibited good biosafety and the GelMA/DBM/DFO hydrogel showed more effective repair of cranial defects in SD rats. This study provides a novel material for bone-defect repair.
Similar content being viewed by others
Introduction
Bone defects, resulting from trauma, infection, bone tumors, and osteoporosis, disrupt the integrity of the skeletal system1,2. While bones possess a certain capacity for self-repair, defects exceeding a critical threshold are challenging to heal and often require surgical intervention3,4. Common clinical treatments for bone defects include autologous, allogeneic, and artificial bone-repair materials5. An ideal bone graft should exhibit good osteogenic potential, biocompatibility, and the ability to promote angiogenesis6,7. Autologous bone is often limited by supply shortages, increased trauma, and infection risks, leading to wider application of allogeneic bone8,9. Allogeneic bone, readily available from living donors or cadavers, is easy to process and store10,11. It has a porous network structure, making it the closest substitute to autologous bone grafts12,13. Freeze drying, irradiation sterilization, and chemical treatment can effectively reduce safety risks14. Moreover, allogeneic bone provides a rich source of bone matrix proteins that promote cell adhesion and proliferation, support bone tissue regeneration, maintain basic bone structure, and supply the bioactive molecules necessary for bone growth15,16,17,18. However, allogeneic bone grafts carry the risks of disease transmission and immune rejection, which may lead to repair failure19,20. Studies comparing the repair effects of autologous bone, allogeneic bone, and biphasal calcium phosphate artificial bone on rat femoral defects have found that allogeneic bone alone has a relatively poor repair capacity. Other studies have indicated that conventional allogeneic bone may fail due to poor vascularization21. Therefore, the use of allogeneic bone requires further improvements10. Demineralized bone matrix (DBM), the most widely used allogeneic bone graft, is composed mainly of collagen and growth factors, such as bone morphogenetic proteins, and exhibits good bioactivity and biocompatibility22,23,24. DBM provides the growth factors required for cell differentiation and promotes cell proliferation24. Currently, DBM is widely used as a scaffold material in bone tissue engineering25. Research using a Sprague–Dawley (SD mouse femoral defect model, in which DBM scaffolds were implanted and their repair was observed, showed that DBM scaffolds promoted bone formation and improved the efficiency of bone-defect repair26. However, pure DBM scaffolds degrade rapidly after implantation, which can lead to the collapse of newly formed bone in the defect area, hindering new bone formation. Therefore, further exploration of the use of DBM is still needed27.
In recent years, the continuous development of bone tissue engineering and other related research on bone defect treatment, hope for bone defect repair has emerged with the use of a class of polymer systems with excellent biocompatibility, the ability to support various bioactive substances, and hydrophilic networks as extracellular matrix simulators. Therefore, they are widely used in tissue engineering research in the biomedical field and are candidate materials for accelerating bone repair28,29. Gelatin methacrylate (GelMA) is a biomaterial used in bone tissue engineering and bone regeneration; it not only has a highly hydrated three-dimensional structure and extracellular matrix analog similar to traditional hydrogels, but can also be polymerized and formed under mild light conditions30. The cured GelMA hydrogel has controllable physical and chemical properties, good biocompatibility and degradation performance, and provides favorable conditions for cell and tissue growth31. Studies have also found that GelMA hydrogels can provide a scaffold structure and a bone microenvironment for bone growth and differentiation, promote the proliferation and differentiation of bone mesenchymal stem cells (BMSCs), and ultimately promote the formation and repair of bone tissue32. However, GelMA hydrogels face challenges in practical applications because of their low mechanical strength and defects33,34. Studies have shown that a new composite prepared by combining DBM and GelMA has good biocompatibility and osteogenic differentiation abilities24. However, other studies have found that the growth and vascularization of surrounding tissues are hindered by the encapsulation of DBM by carriers, resulting in the osteoinductive delay of DBM35. Bone is a highly vascularized tissue; therefore, osteogenesis and angiogenesis coexist in the repair process of bone tissue, and the rapid formation of new blood vessels is conducive to its rapid repair36,37. Difluorooctane (DFO) is an iron-chelating agent that can stabilize hypoxia-inducing factor 1a and accelerate angiogenesis by upregulating hypoxia-inducing factor 1a and its related downstream angiogenic factors38. Studies have shown that the bioactivity of DFO can be effectively maintained by loading it into hydrogels via blending39. This combination enriches the function of the scaffold materials and DFO plays a role in optimizing angiogenesis and promoting bone tissue regeneration.
In this study, a DBM/GelMA composite system loaded with DFO was constructed by combining the treated allogeneic bone with GelMA and DFO for bone defect repair. The bioactive molecules provided by DBM directly stimulated osteogenesis, while GelMA provided a platform for the protection and progressive release of the growth factors, ensuring their effective utilization during bone repair. The addition of DFO further enhanced the angiogenic ability of the material and accelerated cell proliferation and functional activation of osteoblasts in the repair area by promoting the formation of blood vessels. In vitro experiments demonstrated that the composite hydrogel supplemented with DFO promoted the proliferation and osteogenic differentiation of BMSCs. Concurrently, the composite hydrogel effectively promoted the repair of skull defects in rats, with good biosafety. This triple synergistic effect not only accelerated the structural reconstruction of the bone defect area, but may also improve bone tissue integration by enhancing the interaction at the cellular and molecular levels.
Materials and methods
Materials
The following materials were used in the study: scanning electron microscope (Nicolet™ iS20, Thermo, China), Fourier-transform infrared spectrometer (ProX, Phenom, Netherlands), SBC-12 mini sputter coater (SBC-12, Zhongke Scientific Instruments, China), Micro-CT (nanoVoxel-4000, Scanco, Switzerland), fluorescence microscope (Bx53, Olympus, Japan), Universal Testing Machine (MTS, CMT6103, China), gelatin methacrylate (M299511, Aladdin, USA), desferrioxamine (HY-B1625, MCE, China), bone marrow stem cells (BMSCs, PCS-500-012, ATCC, USA), CCK-8 assay kit (CT01A, Saikang Biotech, China), osteogenic culture medium (PT-3002, Lonza, Switzerland), Alizarin Red stain (C0138-100, Biyun Tian, China), hematoxylin stain solution (H104302-1 g, Aladdin, China), and eosin stain solution (E196384, Aladdin, China), Anti-BMP2(GB11252,Servicebio, China), Anti-COL-1(GB11022-3,Servicebio, China), HRP labeled goat anti rabbit IgG (GB23303,Servicebio, China).
Preparation of composite hydrogels
The rat tibiae were prepared by rinsing with high-pressure water to remove excess bone marrow; degreased with PBS solution at room temperature for 24 h; then immersed in PBS buffer containing 0.25% W/V trypsin at 37 °C for 24 h, followed by washing with PBS buffer for 1 h; treated with PBS buffer containing 10 mM Tris and 0.1% SDS at room temperature for 24 h; transferred to EDTA at 37 °C for 1 h; rinsed multiple times with PBS buffer before freeze-drying to remove excess enzyme solution. The demineralized tibiae were then ground in a cryogenic grinder at a frequency of 10 cycles per second for 15 min to obtain fine bone powder; the fine bone powder was filtered through a 40-µm mesh to obtain the DBM. Dissolve 20 g of GelMA in 100 ml of ultrapure water containing 0.5% lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP, a kind of Photoinitiator) at 40 °C to obtain a GelMA sol. Add the prepared DBM to the GelMA sol and mix using a vortex mixer. Pour the mixture into a cylindrical polytetrafluoroethylene mold with a diameter of 5 mm and a height of 1 mm, and cure under ultraviolet light for 2 min to prepare the GelMA/DBM composite hydrogel. Dissolve DFO in ultrapure water and add it to the mixture of GelMA and DBM, with a final DFO concentration of 1µM. Pour the mixture into the mold to prepare the GelMA/DBM/DFO composite hydrogel.
Scanning electron microscopy (SEM)
To investigate the surface morphological characteristics of the two types of hydrogels, the surface morphology was characterized using a scanning electron microscope (Nicolet™ iS20, Thermo, China). The prepared GelMA/DBM and GelMA/DBM/DFO composite hydrogels were freeze-dried and sputter-coated with gold using an SBC-12 mini sputter coater. The surface morphologies of the materials were observed at an acceleration voltage of 5 kV.
Fourier-transform infrared spectroscopy (FTIR)
The potassium bromide (KBr) pellet method was used for analysis. Dried KBr crystals were mixed with the sample in an agate mortar, ground into a fine powder, uniformly mixed, and pressed into pellets. The sample spectrum was obtained using a FTIR (ProX, Phenom) with a spectral range of 400–4000 cm-1, and the data were plotted.
Swelling and degradation properties of hydrogels
Swelling property test
The samples were immersed in a 37 °C PBS and placed in a 37 °C environment. At predetermined time points (3, 5, 7, 24, and 48 h), the samples were removed, and the surface liquid was blotted dry and weighed. The weight was recorded as Wt and the initial weight after freeze-drying was recorded as Wd. The swelling rate of the hydrogel was calculated using the following formula:
Degradation test
The initial masses of the freeze-dried samples were weighed and recorded as W0. The samples were then immersed in a PBS at 37 °C and retrieved at specific time points (1, 2, 3, and 4 weeks). After freeze-drying, the samples were weighed again, and the weight was recorded as Wt. The degradation rate of the hydrogel was calculated using the following formula:
Mechanical properties of hydrogel
Select GelMA/DBM and GelMA/DBM/DFO samples (diameter: 5 mm, height: 1 mm). Use a Universal Testing Machine (MTSCMT6103, China) to conduct compression and tensile experiments on it, with a compression speed of 0.5 mm/min, repeated 3 times, and a tensile speed of 10 mm/min, repeated 3 times. Draw the stress-strain curve of the composite hydrogel.
In vitro cell experiments
Thawing and passage of BMSCs
Vials containing BMSCs were removed from liquid nitrogen and placed in a 37 °C water bath to facilitate thawing. After gentle agitation, the contents were transferred to a 15 ml centrifuge tube and centrifuged at 1000 rpm for 5 min. The supernatant was discarded and 1 ml of culture medium was added to resuspend the cells. The cell suspension was then transferred to a new culture dish, and 10 ml of culture medium was added. The dish was gently agitated and placed in a CO2 incubator for culturing. When the cell density reached approximately 80 ~ 90%, the cells were ready for first passage.
CCK-8 cell proliferation assay
BMSCs were digested with trypsin, suspended in the culture medium to form a cell solution, and seeded at a density of 1 × 10^5 cells/cm2. After 1, 2, and 3 days of culture, the supernatant was aspirated, and 200 µl of CCK-8 incubation solution was added to each well. The cells were incubated for 2 h at 37 °C in a 5% CO2 environment. Absorbance was measured at 450 nm using a microplate reader to analyze cell proliferation on the hydrogels.
Live/dead cell fluorescence staining
The two composite hydrogels were fixed in a 24-well plate. Third-generation BMSCs in the proliferation phase were digested with trypsin, suspended in culture medium to form a cell solution, and seeded on the surface of the composite hydrogels (5 × 10^3 cells/50 µl). The cells were cultured for 7 days, and the medium was changed every 3 days. Live/dead cells were stained using acridine orange/ethidium bromide. Fluorescence images were obtained using a fluorescence microscope and cell viability was observed.
Alkaline phosphatase staining for osteogenic differentiation ability of hydrogels
Third-generation BMSCs in the proliferation phase were digested with trypsin, suspended in the culture medium to form a cell solution, and seeded on the composite hydrogels at a density of 1 × 10^5 cells/cm2. The cells and hydrogels were cultured in an osteogenic medium. Alkaline phosphatase staining was used to assess the alkaline phosphatase content of the cells on the composite hydrogels on the 7th day of co-culture: The co-culture scaffolds were washed with PBS three times for 10 min; fixed with 4% paraformaldehyde solution for 30 min, then rinsed with PBS; stained with BCIP/NBT dye in a 37 °C water bath for 30 min; and rinsed with distilled water three times for 5 min before observation under a light microscope.
Alizarin red staining for osteogenic differentiation ability of hydrogels
Third-generation BMSCs in the proliferation phase were digested with trypsin, suspended in the culture medium to form a cell solution, and seeded on the composite hydrogels at a density of 1 × 10^5 cells/cm2. The cells and hydrogels were cultured in an osteogenic medium. Alizarin Red staining was used to assess calcium deposition on the composite hydrogels on day 14 of co-culture. The hydrogels were washed with PBS three times for 10 min, fixed with 4% paraformaldehyde solution for 30 min, rinsed with PBS two to three times after removing the fixative, stained with alizarin red dye at room temperature for 30 min, rinsed again with PBS before staining, rinsed with distilled water three times for 5 min, and air-dried before observation under a light microscope.
In vivo animal experiments
A total of 27 male Sprague-Dawley (SD) rats, aged over 8 weeks and weighing 280–410 g, were obtained from Beijing HFK Bio and used in this study.All experimental animals were kept under the same housing conditions. The rats were randomly divided into three groups: control group (n = 9), with only a cranial defect model prepared on one side; GelMA/DBM group (n = 9), with a cranial defect model prepared on one side and GelMA/DBM hydrogel implanted at the defect site; and GelMA/DBM/DFO group (n = 9), with a cranial defect model prepared on one side and GelMA/DBM/DFO hydrogel implanted at the defect site. The animals were sacrificed 4, 8, and 12 weeks postoperatively.
Construction of animal model
All experimental protocols of this study have been approved by the Medical Ethics Committee of Zunyi Medical University(ZMU21-2412-014), and all methods were carried out in accordance with relevant guidelines and regulations (the anesthesia method used in this study was abdominal injection of pentobarbital sodium); This research adopts the method of euthanasia for physical interruption of brain activity, in line with the “AVMA Guidelines for the Euthanasia of Animals: 2020 Edition”. In this study, 27 male rats were used to prepare a unilateral rat skull defect model. The GelMA/DBM/DFO and GelMA/DBM groups were implanted with composite hydrogels, which were cylinders with a diameter of 5 mm and a height of 1 mm. They were sterilized with ethylene oxide before implantation. SD rats were fasted for 8 h and prevented from drinking for 4 h before surgery, and the patient was anesthetized by intraperitoneal injection of 40 ml/kg with 3% pentobarbital sodium. SD rats were skinned and fixed on the operating table after anesthesia took effect. The surgical area was disinfected with 1% iodophor and covered with towel; a scalpel was used to cut the subcutaneous tissue and periosteal layer by layer through the median line at the top of the skull, and the subperiosteal tissue was gently removed by the handle of the surgical knife to fully expose the target location. A circular full-layer bone defect with a diameter of 5 mm and a depth of 1 mm was drilled vertically at a low speed with a hollow trephine head on the left side of the sagittal suture of the skull. At the beginning, an additional external force was added, and when close to the skull drilling, the additional external force was stopped, and the skull was disrupted by the natural gravity of the drill (the drill was tilted 20 to 30° from the vertical direction of forward, back, left, and right, respectively). After skull looseness was tested with ophthalmic tweezers, the skull was removed along the defect edge, after which the defect area was rinsed with 0.9% normal saline. The composite hydrogel was implanted in the GelMA/DBM and GelMA/DBM/DFO groups, and the defect model was prepared in the control group without the composite hydrogel (Fig. 1). After the composite hydrogel was implanted, the iodophor was used for disinfection; absorbable sutures were disinfected layer-by-layer, and penicillin was injected into the muscle (800,000 U/day). The rats were returned to their original feeding environment and fed in a single cage. Penicillin was injected for 3 consecutive days after the operation (800,000 U/day).
Sampling
Blood was drawn and specimens were collected
At 4, 8 and 12 weeks after surgery, 3 SD rats were randomly selected for blood test. Skull, liver and kidney samples were collected from SD rats in each group.SD rats were sacrificed by spinal dislocation. After skin preparation, the skull bone defect was exposed along the original incision, the repair degree of skull bone defect was observed, and the skull was sawed off with a vise. The skull, liver and kidney specimens were stored in 4% paraformaldehyde solution.
Decalcification, embedding and slicing
The skulls of rats fixed in 4% paraformaldehyde solution were washed by running water.15 times the volume of decalcification fluid was added into the skull of rats. Change the decalcification solution twice a week for 3 weeks. When the needle can easily penetrate the bone, it proves that the decalcification effect is good. After decalcification, it was alkalized with 5% sodium sulfate solution and rinsed with running water. The skull was dehydrated in the ethanol concentration gradient (70%, 80%, 90%, 95%, 100%) for 4 h each time. The sample was immersed in xylene solution for 1.5 h until it was obviously transparent. In the oven at 56℃, 50% and 100% paraffin wax were treated for 1 h, and finally paraffin wax embedding was carried out. Use a microtome to slice (5 μm).At the 4th, 8th and 12th week, the skull, liver and kidney of SD rats were taken, fixed in 4% paraformaldehyde solution, and then embedded in paraffin wax. After embedding, the skull, liver and kidney were sliced by microtome (5 μm).
Micro-CT imaging test
For sample pretreatment, the skull defect samples taken at 4, 8, and 12 weeks after surgery were fixed with 70–75% alcohol for more than 48 h. To scan the samples, the were removed, wrapped in cotton soaked with alcohol, placed in an EP tube with appropriate capacity, and fixed in a fixator along the long axis. Micro-CT scanning parameters were adjusted (voltage 70 KV, power 7 W, 4-frame superposition, angle gain 0.72°, exposure time 100 ms, sample rotation 360°), and the samples were scanned. 3D data were reconstructed after scanning was completed. Imaging results and quantitative indicators were obtained and the samples were analyzed.
Histological evaluation
Slices of HE dyed paraffinized samples and the oven was preheated for 40 min. For dewaxing, the slide was put into xylene (I) and xylene (II) for 10 min respectively, then into gradient alcohol (100, 95, 80, and 70%) for 2 min to elute xylene, and finally washed in distilled water for 3 mi.; The samples were dyed with hematoxylin for 1 min and rinsed with tap water to wash away the excess dye solution. Hydrochloric acid ethanol was differentiated into 20 s, the samples were rinsed with tap water again, and then 1% ammonia aqueous solution was added for 1 min. After treatment with the eosin dye for 10 s, the samples were rinsed with tap water. The slides were dehydrated by gradient alcohol (75%, 85%, and 95%) for 2 min each, then anhydrous ethanol for 5 min, and finally xylene for 5 min. Next, the slides were removed, dried, and sealed with a, neutral gum. The nucleus was dark blue under the light microscope, and the envelope and fibrous tissue were red. These steps were repeated many times.
To perform immunohistochemical paraffin section dewaxing to water, the slides were placed in xylene (I) and xylene (II) for 10 min each, then in gradient alcohol (100, 95, 80, and 70%) for 2 min to elute xylene, and finally washed in distilled water for 3 min. For antigen repair, the slices were immersed into sodium citrate buffer (10 mM, PH6.0), boiled in a pressure cooker, held for 15 min, then deflated and cooled slowly.
To block endogenous peroxidase, the slices were placed in 3% hydrogen peroxide solution, incubated at room temperature away from light for 25 min, then placed in PBS (pH7.4) and washed three times on a decolorizing shaking table for 5 min. For serum closure, the tissues were uniformly covered with 3% BSA drops in the tissue chemistry circle and closed at room temperature for 30 min. The sealing solution was gently shaken off, diluted primary antibodies were dropped on the slices (1:400), and the slices were placed flat in a wet box at 4℃ for overnight incubation. The slide was placed in PBS (pH7.4) and washed by shaking on the decolorizing table 3 times for 5 min each. After the slices were slightly dried, the tissue was covered with secondary antibody (HRP label) of the corresponding species of the primary antibody in the circle and incubated at room temperature for 50 min. For DAB color development, the slides were placed in PBS and washed by shaking on a decolorizing table 3 times for 5 min each. After the sections had dried slightly, the newly prepared DAB color development solution was added to the circle. The color development time was monitored under a microscope. To restain the nucleus, hematoxylin was used for approximately 3 min, the samples were rinsed with tap water, hematoxylin differentiation solution was added for a few seconds, the samples were rinsed with tap water; finally, hematoxylin blue return solution was added, and the samples were rinsed with running water. The slices were placed into gradient alcohol (75% and 85%) for 5 min each, removed, baked dry, and sealed with gum.
Statistical analysis
All experiments were repeated at least thrice. Data were processed using SPSS 29.0 (IBM SPSS Statistics Professional Software) and presented as mean ± standard deviation (mean ± SD). Intergroup comparisons were performed using a one-way ANOVA and independent sample t-tests. Graphs were plotted using GraphPad Prism and Origin software. Statistical significance was set at P < 0.05.
Results
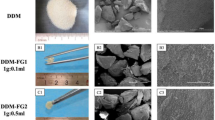
Scanning electron microscopy (SEM) images of composite hydrogels
SEM observations showed that both types of composite hydrogels, with the addition of DBM and DFO, possessed a three-dimensional interwoven network structure. Under various magnifications, numerous uneven and irregular concave-convex structures were observed, indicating a rough surface (Fig. 2).
Fourier-transform infrared (FTIR) spectroscopy analysis of composite hydrogels
FTIR spectroscopy identified a characteristic absorption peak near 1014 cm-1 in the spectrum of pure DBM, likely due to the asymmetric stretching vibration of the PO43- groups. This peak was also visible in the GelMA/DBM spectrum, confirming successful preparation of the GelMA/DBM composite hydrogel. Furthermore, after the addition of DFO, two characteristic absorption peaks appeared at 2933 and 2856 cm−1, which may be attributed to the asymmetric and symmetric stretching vibrations of the CH2 groups in DFO, indicating the successful incorporation of DFO into the GelMA/DBM composite, resulting in the GelMA/DBM/DFO hydrogel (Fig. 3).
Swelling properties of composite hydrogels
The swelling properties of the hydrogels were determined by weighing. As time progressed, both the GelMA/DBM and GelMA/DBM/DFO composite hydrogels gradually swelled in the aqueous solution. At all-time points, the swelling rate of the GelMA/DBM composite hydrogel in the aqueous solution was significantly higher than that of the GelMA/DBM/DFO composite hydrogel (Fig. 4, P < 0.01).
Degradation properties of composite hydrogels
The degradation properties of the hydrogels were assessed by weighing. The degradation rates of both the hydrogels increased over time. At week 4, the degradation rate of the GelMA/DBM composite hydrogel was higher than that of the GelMA/DBM/DFO composite hydrogel; however, the difference was not statistically significant (Fig. 5, P > 0.05).
Mechanical properties of hydrogel
The mechanical properties of the two composite hydrogels were tested using a universal material testing machine. The results revealed that the GelMA/DBM/DFO group exhibited superior compressive strength compared to the GelMA/DBM group, with the maximum compressive strength of the GelMA/DBM/DFO group reaching 3.61 MPa, while that of the GelMA/DBM group was 2.52 MPa (Fig. 6A). In terms of tensile properties, the GelMA/DBM/DFO group demonstrated a fracture elongation of 34.08%, whereas the GelMA/DBM group showed a fracture elongation of 18.96% (Fig. 6B).
Cell proliferation assay of composite hydrogels
BMSCs were cultured on the surface of the scaffolds, and their proliferation was observed on days 1, 2, and 3. The results indicated an upward trend in cell proliferation in all the groups during the culture period (Fig. 7). On day 1, both the GelMA/DBM and GelMA/DBM/DFO composite hydrogel groups promoted the proliferation of BMSCs with statistically significant differences (P < 0.05). On day 2, the cell proliferation rate in both the GelMA/DBM and GelMA/DBM/DFO groups increased compared to that on day 1, with statistically significant differences (P < 0.05). On day 3, both composite hydrogel groups significantly promoted the proliferation of BMSCs, with statistically significant differences (P < 0.01).
Live/dead cell fluorescence staining of composite hydrogels
Live/dead cell fluorescence staining was performed to assess the numbers of viable and dead cells within the GelMA/DBM and GelMA/DBM/DFO composite hydrogels. The GelMA/DBM/DFO group exhibited a higher number of viable cells and a lower number of dead cells than the GelMA/DBM group (Fig. 8).
Osteogenic differentiation capability of composite hydrogels
The osteogenic potential of the hydrogels was evaluated by culturing BMSCs on the surface and assessing early-stage osteogenic differentiation with alkaline phosphatase (ALP) staining on day 7, and late-stage osteogenic differentiation with Alizarin Red staining on day 14. The results showed that the GelMA/DBM/DFO group had a higher ALP staining intensity on day 7 than the GelMA/DBM group. On day 14, the GelMA/DBM/DFO hydrogel group demonstrated a higher level of calcium deposition than the GelMA/DBM group (Figs. 9 and 10).
Gross observation of rat calvarial defect model
The rats recovered smoothly after surgery, with minimal activity on the day of surgery and no food or water intake. On the first postoperative day, the rats were minimally active, with normal defecation and urination, good incision apposition, continued antibiotic injection, and incision disinfection. By the second postoperative day, their activity returned to normal, with regular diet and water intake, normal defecation and urination, no evident abnormalities at the surgical site, and continued antibiotic injection and incision disinfection. On the third postoperative day, all SD rats had normal activity, diet, and water intake, with no abnormalities at the surgical site, and continued antibiotic injection and incision disinfection. One week postoperatively, all the rats had healed incisions with no bleeding, discharge, swelling, or other complications.
Biocompatibility of composite hydrogels
Blood test results
Peripheral blood indices of the SD rats in the blank control group, GelMA/DBM group, and GelMA/DBM/DFO group at weeks 4, 8, and 12 post-surgery showed no significant differences in white blood cell (WBC), red blood cell (RBC), hemoglobin (HB), platelet (PLT), alanine aminotransferase (ALT), aspartate aminotransferase (AST), urea (Urea), and creatinine (Cr) levels (Table 1, P > 0.05).
Liver and kidney tissue hematoxylin and eosin (HE) staining
To assess the toxicity of the composite hydrogels in vivo, the liver and kidney tissues were harvested from SD rats at weeks 4, 8, and 12 postoperatively and sectioned. HE staining showed normal morphology in liver cells, central veins, and hepatic sinusoids, as well as in renal glomeruli and renal tubules, with no evidence of inflammatory cell infiltration, indicating no significant toxicity from the two types of composite hydrogels (Figs. 11 and 12).
Osteogenic capacity of composite hydrogels
Micro-CT
Micro-CT was performed on the calvarial defect area of SD rats at 4, 8, and 12 weeks postoperatively. At week 4, new bone formation was observed in all the groups, with the GelMA/DBM/DFO group exhibiting a larger area of new bone formation than the GelMA/DBM and blank control groups. The GelMA/DBM group showed some new bone formation, but a smaller area, whereas the control group showed only a small amount of new bone formation. At week 8, the GelMA/DBM/DFO group showed an increased area of new bone formation, which was still larger than those of the GelMA/DBM and control groups. The GelMA/DBM group showed a slight increase in the new bone tissue, whereas the control group had a larger bone defect area. At week 12, the bone defect area in the GelMA/DBM/DFO group was almost completely filled with new bone, with a larger filling area compared to that in the GelMA/DBM and control groups. The GelMA/DBM group also showed new bone formation with partial filling of the bone-defect area, whereas the control group still had a larger bone-defect area (Fig. 13). The bone volume fraction (BV/TV), a direct indicator of bone quantity changes, was measured to quantitatively analyze the effect of the GelMA/DBM/DFO hydrogel on the repair of calvarial defects in SD rats. The results showed that the BV/TV values of the GelMA/DBM/DFO group at weeks 4, 8, and 12 post-surgery were all significantly greater than those of the GelMA/DBM and control groups (Fig. 14, P < 0.05).
Histological examination with HE and masson’s staining
To assess the effects of the composite hydrogels on the repair of calvarial defects in SD rats, calvarial tissues were harvested 4, 8, and 12 weeks postoperatively and sectioned. HE staining revealed that at week 4, the GelMA/DBM/DFO group had noticeable formation of new trabecular bone, with a greater amount of trabeculae compared to the GelMA/DBM and control groups. The GelMA/DBM group showed a small amount of new trabecular bone, whereas the control group showed hardly any new trabecular bone. At week 8, the amount of new trabecular bones in the GelMA/DBM/DFO group was higher than those in the GelMA/DBM and control groups. The GelMA/DBM group showed a slight increase in the amount of new trabecular bones, whereas the control group had fewer bones. At week 12, the bone defect area in the GelMA/DBM/DFO group was filled with a large amount of new trabecular bone, and the bone defect area was filled with bone trabeculae. The GelMA/DBM group also showed an increased distribution of new trabecular bone, whereas the control group had only a small amount of bone trabeculae (Fig. 15). Masson’s staining showed that at week 4, the GelMA/DBM/DFO group had a noticeable formation of blue collagen and red muscle fiber tissue compared to the GelMA/DBM group, with the control group having the least amount of these tissues. At week 8, the collagen and muscle fiber tissues in the GelMA/DBM/DFO group increased and were greater than those in the GelMA/DBM and control groups. The GelMA/DBM group showed a slight increase in collagen and muscle fiber tissue, whereas the control group still had less collagen and muscle fiber tissue. At week 12, the bone defect area in the GelMA/DBM/DFO group was filled with dark blue mature bone collagen, followed by the GelMA/DBM group and the blank control group having the least (Fig. 16).
Immunohistochemical staining of calvarial tissues
Further understanding of the formation of bone morphogenetic protein 2 (BMP-2) and type I collagen (Col-I) in the bone defect area was obtained by immunohistochemical staining to study the osteogenic activity of the implanted materials. The results of calvarial immunohistochemical staining showed that at week 4, areas with positive expression of BMP-2 and Col-I were visible around the bone defect; the GelMA/DBM/DFO group had higher BMP-2 and Col-I positive expression than the GelMA/DBM group and the control group. The GelMA/DBM group exhibited a small number of distributed positive expression areas, whereas the control group exhibited few positive expression areas. At week 8, the positive expression of BMP-2 and Col-I in each group increased, with the GelMA/DBM/DFO group showing a stronger positive expression than the other two groups. The GelMA/DBM group showed an increase in positive expression, whereas the control group showed the lowest positive expression. At week 12, the GelMA/DBM/DFO group had the highest BMP-2- and Col-I-positive expression, followed by the GelMA/DBM group, and the control group had the lowest expression (Figs. 17 and 18).
Discussion
The increasing number of patients with bone defects caused by trauma, infection, and tumors has made the repair of bone defects, particularly large-segment defects, a clinical challenge. Currently, common treatments for bone defects have varying degrees of disadvantages; hence, exploring new artificial bone repair materials is an urgent issue to be addressed40. DBM is the most widely used allograft and is composed of bone-conductive collagen, residual calcium, and non-collagenous proteins with osteoinductive properties that promote bone tissue repair24,27. However, the demineralized particles of DBM are prone to rapid dispersion after demining, making its osteoinductive capacity unpredictable and limiting its use as a bone repair material41. GelMA has excellent biocompatibility, high porosity, high water content, and biodegradability, and is widely used in the biomedicine42,43. GelMA is a photosensitive material that can quickly cross-link under blue and ultraviolet light, forming a three-dimensional structure with a certain strength44. Studies have found that GelMA can achieve good and controllable mechanical properties through photopolymerization, meeting the requirements of bone defect repair scaffolds39. However, owing to their rapid substance exchange rate, pure GelMA hydrogels cannot meet the physiological needs of the body, thus limiting their application in bone tissue repair45,46. DFO, an iron chelator, was recently found to promote osteogenesis. It activates the hypoxia-inducible factor-1α signaling pathway and participates in bone tissue formation and angiogenesis39,47. In previous studies, DFO was often loaded onto the surface of the scaffold, making it difficult to achieve long-term stability; thus, its role in repairing large-segment bone defects is limited and requires further optimization48. Some studies have combined these substances to construct new composite materials that promote bone-defect repair. Ramis et al. found that GelMA composites loaded with DBM had good biocompatibility, in vitro osteogenic differentiation ability, and in vivo bone defect repair ability24. Chen et al. constructed electrospun GelMA fibers loaded with DFO and found that this composite material promoted the proliferation of BMSCs and effectively repaired femoral defects in mice49. The biocompatibility and bone-repair capacity of GelMA/DBM and GelMA/DFO composite materials have been confirmed; however, the performance of a combination of these materials has not yet been explored. Therefore, in this study, GelMA/DBM/DFO composite hydrogels were prepared by loading DFO onto GelMA/DBM to explore their chemical properties, biocompatibility, osteogenic differentiation ability, and ability to promote the repair of rat calvarial defects.
In this study, the GelMA/DBM and GelMA/DBM/DFO composite hydrogels were prepared by co-mixing and freeze-drying. The prepared composite hydrogels exhibited a three-dimensional mesh structure, and the surfaces of both types had uneven and rough concave-convex structures (Fig. 2). The 3D network structure of the GelMA/DBM composite was mainly composed of GelMA, and the addition of DFO, which may be uniformly dispersed within the GelMA/DBM composite, did not significantly affect its structure50,51. Rough bone repair materials with surface irregularities are more conducive to osteoblast growth and vascularization, thereby facilitating bone tissue healing52,53. FTIR spectroscopy revealed characteristic absorption peaks at 1014 cm-1, 2933 cm-1, and 2856 cm-1 in the GelMA/DBM and GelMA/DBM/DFO spectra, likely due to the asymmetric stretching vibration of PO43- in DBM and the asymmetric and symmetric stretching vibrations of CH2 in DFO54, confirming the successful preparation of the composite hydrogels (Fig. 3).
A lower swelling rate can reduce the potential damage to the surrounding tissues by providing a more stable support environment for the bone-defect area55. Additionally, a lower swelling rate can enhance the mechanical properties of the material and better mimic the physical characteristics of bone56. In this study, the swelling and degradation properties of the GelMA/DBM and GelMA/DBM/DFO composite hydrogels were evaluated using the weighing method. The swelling experiment showed that both composite hydrogels gradually swelled in aqueous solution, but the GelMA/DBM/DFO composite hydrogel had a lower swelling rate than the GelMA/DBM composite hydrogel, indicating that the former could reduce damage to the surrounding tissues and potentially have better mechanical properties (Fig. 4). The degradation behavior plays a crucial role in tissue regeneration and controlled drug release rates. Bone repair materials with appropriate degradation rates can match the growth rate of the bone tissue47,57. The degradation experiments showed that both composite hydrogels gradually degraded over time. At four weeks, the degradation rate of the GelMA/DBM/DFO group was lower than that of the GelMA/DBM group, indicating that the former could better match the growth rate of the bone tissue (Fig. 5). The reason for the lower swelling rate of the GelMA/DBM/DFO group compared to that of the GelMA/DBM group may be the addition of DFO, which occupies the space within the composite material, reduces porosity, hinders the binding of water molecules to the composite material, and ultimately results in a lower swelling rate of the GelMA/DBM/DFO composite hydrogel compared to the GelMA/DBM composite hydrogel58,59. Additionally, the lower swelling rate of the GelMA/DBM/DFO composite hydrogel affected the speed and quantity of water molecules penetrating the polymer network, leading to a slower degradation rate than that of the GelMA/DBM composite hydrogel58. Another possible reason is that the absence of DFO wrapping in the GelMA/DBM composite hydrogel allowed the DBM to come into direct contact with the aqueous solution, thereby increasing the absorption of the organic phase and accelerating the degradation rate of the GelMA/DBM composite hydrogel60.
The mechanical properties of biological tissues refer to their response to deformation, including compressive and tensile properties61. In this study, compression tests revealed that the GelMA/DBM/DFO group exhibited superior maximum compressive strength compared to the GelMA/DBM group. In terms of tensile properties, the GelMA/DBM/DFO group also outperformed the GelMA/DBM group (Fig. 6). These results demonstrate that the GelMA/DBM/DFO group possesses better mechanical properties than the GelMA/DBM group. The composite hydrogel prepared in this study may be suitable for non-load-bearing bone defects61.
Biocompatibility considers the interaction between the host and material. Good biocompatibility indicates that the material has low toxicity to the host and is safe. The biocompatibility of materials can be evaluated through a series of in vitro and in vivo experiments62,63. In this study first co-cultured BMSCs with the composite hydrogels, and a CCK-8 assay was used to test the cell proliferation capacity of the hydrogels. The cell proliferation capacity of the GelMA/DBM/DFO group on days 1, 2, and 3 was higher than that of the GelMA/DBM group, indicating that the former can better promote BMSC proliferation. The reason may be that the addition of DFO activates the hypoxia-inducible factor-1α signaling pathway, stimulates angiogenesis in bone tissue, simulates the function of the extraosseous vascular network, and thus promotes cell proliferation and differentiation64. The number of cells on the GelMA/DBM and GelMA/DBM/DFO hydrogels was determined using live/dead cell fluorescence staining. The GelMA/DBM/DFO group had a higher number of viable cells than the GelMA/DBM group, which was consistent with the results of the CCK-8 assay. Furthermore, this study also tested the biocompatibility of each group of hydrogels in vivo by HE staining of peripheral blood, liver, and kidney tissues in SD rats. No evident abnormalities in the peripheral blood tests of the control, GelMA/DBM, and GelMA/DBM/DFO groups were observed; the liver and kidney tissue showed that the liver cells, central veins, hepatic sinusoids, renal glomeruli, and renal tubules of each group of SD rats had normal morphology, with no evident inflammatory cell infiltration, indicating that the two types of composite hydrogels had no toxicity. The reasons for no evident toxic reactions in response to the two types of composite hydrogels may be as follows: first, GelMA itself has good biocompatibility and non-toxicity, which can promote cell proliferation and migration; second, previous studies have found that using GelMA as a carrier for DBM in the treatment of bone defects showed no cytotoxic reactions; finally, some studies have used low doses of DFO to promote fracture healing and found that at low doses (25µM), DFO can promote cell proliferation without toxic reactions24,65,66. Combining the results of CCK-8, live/dead cell fluorescence staining, SD rat peripheral blood tests, and liver and kidney tissue HE staining, it was demonstrated that the GelMA/DBM/DFO composite hydrogel promoted the proliferation of BMSCs better, had low toxicity, and exhibited good biocompatibility (Figs. 7, 8, 11 and 12).
An ideal bone-repair material should have not only good biocompatibility but also strong osteogenic differentiation capabilities67. ALP is an early differentiation marker of osteoblasts, and its activity is closely related to osteogenic differentiation capacity68,69. To test the early osteogenic performance of the GelMA/DBM/DFO hydrogel, this study co-cultured BMSCs with the composite hydrogel and ALP staining on day 7 showed that the GelMA/DBM/DFO group had a higher ALP content than the GelMA/DBM group. Calcium is the main component of the extracellular bone matrix and calcium deposition is a late differentiation marker of osteoblasts70,71. To test the late osteogenic performance of the GelMA/DBM/DFO hydrogel, BMSCs were co-cultured with the composite hydrogel, and Alizarin Red staining was used to analyze calcium deposition on day 14. The GelMA/DBM/DFO group had more calcium deposition than the GelMA/DBM group, demonstrating that the GelMA/DBM/DFO composite hydrogel had a stronger in vitro osteogenic differentiation capacity for BMSCs than the GelMA/DBM composite hydrogel (Figs. 9 and 10).
To explore the in vivo osteogenic performance of the two composite hydrogels, a calvarial defect model was prepared for validation. Large animals such as dogs, pigs, and sheep have similar healing mechanisms to humans; however, owing to their high costs and other disadvantages, they are not as widely used as rodents in practical applications72,73. Mice are inexpensive and reproduce quickly; however, their small size is not conducive for surgery74,75. In contrast, rats are not only cost-effective, but also have a body size that facilitates surgery, making them the experimental animals of choice for the calvarial defect model in this study to explore the in vivo osteogenic performance of the two types of composite hydrogels.
Micro-CT is a non-destructive 3D imaging technique that clearly shows the internal microstructure of bone tissue and is suitable for the detection of small-animal bone tissue. It is widely used in the bone-related fields76. The bone volume fraction, which refers to the ratio of bone tissue volume to tissue volume, directly reflects changes in bone quantity and is a quantitative indicator in micro-CT77. Micro-CT was used to observe the morphology and quantitatively analyze the repair of calvarial defects in SD rats. Compared with the GelMA/DBM and control groups, the GelMA/DBM/DFO group had more evident new bone proliferation in the bone defect area, and the bone defect area was significantly reduced. At week 12, some bone defect areas in the GelMA/DBM/DFO group were almost completely filled with new bone, and the bone volume fraction of the GelMA/DBM/DFO group at weeks 4, 8, and 12 post-surgery was greater than those of the GelMA/DBM and control groups (Figs. 14 and 15). HE staining is the most basic and widely used histological technique that can distinguish bone tissue structure and cells in the bone marrow cavity78,79. Therefore, this study further observed the repair of calvarial defects through HE staining of calvarial tissue and found that at weeks 4, 8, and 12 post-surgery, the bone defect edges in the GelMA/DBM/DFO group had a more gradual formation of new trabecular bone, with a greater amount of new trabecular bone. Masson’s staining showed that at weeks 4, 8, and 12 post-surgeries, the GelMA/DBM/DFO group gradually formed more dark-blue mature bone collagen than the GelMA/DBM and control groups (Fig. 16). In addition, we analyzed the expression of osteogenic differentiation factors in the two materials using immunohistochemical staining. BMP-2 is a growth factor that regulates bone tissue development, induces the proliferation and osteogenic differentiation of stem cells, and promotes new bone80. Col-I plays a crucial role in the formation and maturation of the cell matrix, and is widely distributed in bone tissues81. The results showed that at weeks 4, 8, and 12 post-surgery, the positive expression areas of the bone markers BMP-2 and Col-I around the new bone matrix in each group were visible, and the GelMA/DBM/DFO group showed higher expression levels than the GelMA/DBM and control groups at each time point (Figs. 17 and 18).
Due to the fact that DFO can promote bone tissue repair and accelerate angiogenesis by upregulating hypoxia inducible factor-1 α and related downstream factors, this may be the reason why the GelMA/DBM/DFO group exhibits better bone repair ability than the GelMA/DBM group38. Previous studies using a rabbit ulna model revealed that grafts incorporating DFO demonstrated significantly enhanced neovascularization compared to those without DFO82.Another study evaluated the angiogenic effects of DFO by loading it onto porous titanium alloys and co-culturing with HUVEC cells, the results demonstrated that the DFO-loaded group exhibited a higher number of blood vessels compared to the non-loaded group83. Additionally, research by Yan et al. also indicated that DFO can promote the repair of bone defect tissues84. These in vivo experimental results indicate that the GelMA/DBM/DFO composite hydrogel can better promote the repair of calvarial defects in SD rats than the GelMA/DBM composite hydrogel. This study only explored the repair capacity of the GelMA/DBM/DFO composite hydrogel for non-load-bearing bone defects, providing a preliminary experimental basis for new materials in bone defect repair; however, further research is still needed for the repair of load-bearing bones and large-segment bone defects.
In response to the need for new materials for bone repair, we successfully prepared a composite hydrogel material system consisting of rat allograft DBM/GelMA loaded with DFO. The DBM/GelMA composite hydrogel loaded with DFO significantly promoted the proliferation and osteogenic differentiation of BMSCs and promoted the reconstruction and repair of bone at the site of rat skull defects. This composite hydrogel showed significant advantages in bone repair and regeneration, and this study provides a new material option for bone defect repair.
Data availability
All data generated or analyzed during this study are include in this published article.All data generated or analyzed during this study are include in this published article.
References
Teixeira, M. A., Amorim, M. & Felgueiras, H. P. Poly(vinyl alcohol)-based nanofibrous electrospun scaffolds for tissue engineering applications. Polym. (Basel)12 (1). (2019).
Zhao, D. et al. Poly(lactic-co-glycolic acid)-based composite bone-substitute materials. Bioact Mater.6 (2), 346–360 (2021).
Chen, R. et al. Mesenchymal stem cell-immune cell interaction and related modulations for bone tissue engineering. Stem Cells Int.2022 7153584 (2022).
Altundag, O., Oteyaka, M. O. & Celebi-Saltik, B. Co- and triaxial electrospinning for stem cell-based bone regeneration. Curr. Stem Cell. Res. Ther.19 (6), 865–878 (2024).
Jiang, T. et al. Research progress on nanomaterials for tissue engineering in oral diseases. J. Funct. Biomater.14 (8). (2023).
Wang, J. C. et al. Development of aospine bone (bone osteobiologics and evidence) classification. Glob. Spine J.10 (7), 871–874 (2020).
Virk, M. S. & Lieberman, J. R. Biologic adjuvants for fracture healing. Arthritis Res. Ther.14 (6), 225 (2012).
Zhou, L. et al. Healing of bone defects by induced pluripotent stem cell-derived bone marrow mesenchymal stem cells seeded on hydroxyapatite-zirconia. Ann. Transl. Med.9 (23), 1723 (2021).
Solakoglu, O. et al. A 3-year prospective randomized clinical trial of alveolar bone crest response and clinical parameters through 1, 2, and 3 years of clinical function of implants placed 4 months after alveolar ridge preservation using two different allogeneic bone-grafting materials. Int. J. Implant Dent.8 (1), 5 (2022).
Zou, W. et al. A comparative study of autogenous, allograft and artificial bone substitutes on bone regeneration and immunotoxicity in rat femur defect model. Regen Biomater.8 (1), rbaa40 (2021).
Lim, K. T. et al. Human teeth-derived bioceramics for improved bone regeneration. Nanomaterials (Basel)10 (12) (2020).
Kovac, Z. et al. Regeneration of horizontal bone defect in edentulous maxilla using the allogenic bone-plate shell technique and a composite bone graft-a case report. Med. (Kaunas)59 (3). (2023).
Cao, Y. T. et al. Enucleation combined with guided bone regeneration in small and medium-sized odontogenic jaw cysts. World J. Clin. Cases10 (9), 2764–2772 (2022).
Tang, G. et al. Recent trends in the development of bone regenerative biomaterials. Front. Cell. Dev. Biol.9, 665813 (2021).
Huang, J. et al. Covalent immobilization of VEGF on allogeneic bone through polydopamine coating to improve bone regeneration. Front. Bioeng. Biotechnol.10, 1003677 (2022).
Fillingham, Y. & Jacobs, J. Bone grafts and their substitutes. Bone Joint J.98-B (1), 6–9 (2016).
Krasny, K. et al. Allogeneic bone block volume preservation in ridge augmentation for implants. Int. J. Periodont. Restor. Dent.38 (3), 355–360 (2018).
Li, D. M. et al. Application of a new anatomic hook-rod-pedicle screw system in young patients with lumbar spondylolysis: A pilot study. World J. Clin. Cases10 (17), 5680–5689 (2022).
Kumar, A. et al. Manufacturing functional hydrogels for inducing angiogenic-osteogenic coupled progressions in hard tissue repairs: prospects and challenges. Biomater. Sci.10 (19), 5472–5497 (2022).
Cao, Z. M. et al. Efficacy comparison of vascularized Iliac crest bone flap and Ilizarov bone transport in the treatment of traumatic bone defects of the tibia combined with large soft tissue defects. J. Orthop. Surg. Res.18 (1), 349 (2023).
Kuroda, R. et al. Clinical impact of Circulating CD34-positive cells on bone regeneration and healing. Tissue Eng. Part. B Rev.20 (3), 190–199 (2014).
Gatam, A. R., Gatam, L. & Lumban, T. S. Comparison of clinical and radiological outcomes of lumbar interbody fusion using a combination of hydroxyapatite and demineralized bone matrix and autografts for lumbar degenerative spondylolisthesis. Asian Spine J.11 (5), 706–714 (2017).
Yang, L. et al. Relative influence on cell behaviors of osteoblasts seeded onto demineralized bone matrix with diverse particle size. Cell. Tissue Bank.24 (2), 369–385 (2023).
Ramis, J. M. et al. Improved physical and osteoinductive properties of demineralized bone matrix by gelatin methacryloyl formulation. J. Tissue Eng. Regen Med.14 (3), 475–485 (2020).
Hassibi, H. et al. Allogenic bone graft enriched by periosteal stem cell and growth factors for osteogenesis in critical size bone defect in rabbit model: histopathological and radiological evaluation. Iran. J. Pathol.15 (3), 205–216 (2020).
Jiang, X. et al. Osteogenic efficiency in vivo of scaffolding material of prefabricated vascularization. Exp. Ther. Med.17 (1), 398–402 (2019).
Hogan, K. J. et al. Development of photoreactive demineralized bone matrix 3D printing colloidal inks for bone tissue engineering. Regen Biomater.10, rbad90 (2023).
Wei, Y. et al. Preparation of PVA fluorescent gel and luminescence of europium sensitized by terbium (III). Polym. (Basel)12 (4). (2020).
Jeon, O. et al. Stem cell-laden hydrogel Bioink for generation of high resolution and fidelity engineered tissues with complex geometries. Bioact Mater.15, 185–193 (2022).
Peng, W. et al. Recent progress of collagen, Chitosan, alginate and other hydrogels in skin repair and wound dressing applications. Int. J. Biol. Macromol.208, 400–408 (2022).
Xu, W. et al. Controlled release of Silibinin in GelMA hydrogels inhibits inflammation by inducing M2-type macrophage polarization and promotes vascularization in vitro. RSC Adv.12 (21), 13192–13202 (2022).
Li, J. et al. Biomimetic methacrylated gelatin hydrogel loaded with bone marrow mesenchymal stem cells for bone tissue regeneration. Front. Bioeng. Biotechnol.9, 770049 (2021).
Wei, H. et al. 3D printing of MOF-reinforced methacrylated gelatin scaffolds for bone regeneration. J. Biomater. Sci. Polym. Ed.35 (4), 443–462 (2024).
Qin, B. et al. Antisense YycF and BMP-2 co-delivery gelatin methacryloyl and carboxymethyl Chitosan hydrogel composite for infective bone defects regeneration. Int. J. Biol. Macromol.253 (Pt 5), 127233 (2023).
Ma, L. & Tian, M. [Feasibility of an injectable and in situ gelling gelatin hydrogel for demineralized bone matrix powder delivery]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi31 (3), 300–305 (2017).
Alarcin, E. et al. Injectable shear-thinning hydrogels for delivering osteogenic and angiogenic cells and growth factors. Biomater. Sci.6 (6), 1604–1615 (2018).
Yin, J. et al. Nb(2)C MXene-functionalized scaffolds enables osteosarcoma phototherapy and angiogenesis/osteogenesis of bone defects. Nanomicro Lett.13 (1), 30 (2021).
Zhang, Y. et al. 3D hypoxia-mimicking and anti-synechia hydrogel enabling promoted neovascularization for renal injury repair and regeneration. Mater. Today Bio21, 100694 (2023).
Li, Z. et al. 3D bioprinted gelatin/gellan gum-based scaffold with double-crosslinking network for vascularized bone regeneration. Carbohydr. Polym.290, 119469 (2022).
Wehrle, E. et al. Spatio-temporal characterization of fracture healing patterns and assessment of biomaterials by time-lapsed in vivo micro-computed tomography. Sci. Rep.11 (1), 8660 (2021).
Chen, C. et al. Self-assembled nanocomposite hydrogels as carriers for demineralized bone matrix particles and enhanced bone repair. Adv. Healthc. Mater.13 (10), e2303592 (2024).
Lin, Y. et al. Osteosarocma progression in biomimetic matrix with different stiffness: insights from a three-dimensional printed gelatin methacrylamide hydrogel. Int. J. Biol. Macromol.252, 126391 (2023).
Novais, G. B. et al. Development of a new formulation based on in situ photopolymerized polymer for the treatment of spinal cord injury. Polym. (Basel)13 (24) (2021).
Ren-Jie, X. et al. A biphasic calcium phosphate/acylated methacrylate gelatin composite hydrogel promotes osteogenesis and bone repair. Connect. Tissue Res.64 (5), 445–456 (2023).
Guan, X. et al. Development of hydrogels for regenerative engineering. Biotechnol. J.12 (5). (2017).
Buie, T., McCune, J. & Cosgriff-Hernandez, E. Gelatin matrices for growth factor sequestration. Trends Biotechnol.38 (5), 546–557 (2020).
Zhang, J. et al. Osteoimmunity-regulating biomimetically hierarchical scaffold for augmented bone regeneration. Adv. Mater.34 (36), e2202044 (2022).
Zhang, S. et al. A nonlinear relationship between the triglycerides to high-density lipoprotein cholesterol ratio and stroke risk: an analysis based on data from the China health and retirement longitudinal study. Diabetol. Metab. Syndr.16 (1), 96 (2024).
Chen, W. et al. Electrospun fibers improving cellular respiration via mitochondrial protection. Small17 (46), e2104012 (2021).
Ji, L. et al. 2-N, 6-O sulfated Chitosan evokes periosteal stem cells for bone regeneration. Bioact Mater.34, 282–297 (2024).
Kurian, A. G. et al. Multifunctional GelMA platforms with nanomaterials for advanced tissue therapeutics. Bioact Mater.8, 267–295 (2022).
Falguera, U. M. et al. A narrative review of cell-based approaches for cranial bone regeneration. Pharmaceutics14 (1). (2022).
Rokaya, D. et al. Polymeric materials and films in dentistry: an overview. J. Adv. Res.14, 25–34 (2018).
Wu, M. et al. Smart-responsive multifunctional therapeutic system for improved regenerative microenvironment and accelerated bone regeneration via mild photothermal therapy. Adv. Sci.11 (2), e2304641 (2024).
Nkhwa, S. et al. Combinatorial design of calcium meta phosphate poly(vinyl alcohol) bone-like biocomposites. J. Mater. Sci. Mater. Med.29 (8), 128 (2018).
Thang, N. H., Chien, T. B. & Cuong, D. X. Polymer-based hydrogels applied in drug delivery: an overview. Gels9 (7) (2023).
Zhou, Y. et al. Microstructure and corrosion behavior of iron based biocomposites prepared by laser additive manufacturing. Micromachines (Basel)13 (5) (2022).
Louf, J. F. et al. Under pressure: hydrogel swelling in a granular medium. Sci. Adv.7 (7). (2021).
Florian, P. E. et al. Salecan-clay based polymer nanocomposites for chemotherapeutic drug delivery systems; characterization and in vitro biocompatibility studies. Mater. (Basel) 13 (23). (2020).
Wang, X. H., Jia, S. J. & Hao, D. J. Advances in the modification of injectable calcium-phosphate-based bone cements for clinical application. Chin. Med. J. (Engl.)133 (21), 2610–2612 (2020).
Zhu, Y. et al. Bioprinted PDLSCs with high-concentration GelMA hydrogels exhibit enhanced osteogenic differentiation in vitro and promote bone regeneration in vivo. Clin. Oral Investig.27 (9), 5153–5170 (2023).
Jurak, M. et al. What affects the biocompatibility of polymers? Adv. Colloid Interface Sci.294, 102451 (2021).
Rahman, M., Dutta, N. K. & Roy, C. N. Magnesium alloys with tunable interfaces as bone implant materials. Front. Bioeng. Biotechnol.8, 564 (2020).
Zhao, X. et al. Electrospun biomimetic periosteum capable of controlled release of multiple agents for programmed promoting bone regeneration. Adv. Healthc. Mater.13 (12), e2303134 (2024).
Zhang, X. et al. A bioactive gelatin-methacrylate incorporating magnesium phosphate cement for bone regeneration. Biomedicines12 (1). (2024).
Donneys, A. et al. Localized deferoxamine injection augments vascularity and improves bony union in pathologic fracture healing after radiotherapy. Bone52 (1), 318–325 (2013).
Zhao, Z. H. et al. Sustained release of naringin from silk-fibroin-nanohydroxyapatite scaffold for the enhancement of bone regeneration. Mater. Today Bio13, 100206 (2022).
Makris, K., Mousa, C. & Cavalier, E. Alkaline phosphatases: biochemistry, functions, and measurement. Calcif Tissue Int.112 (2), 233–242 (2023).
Lao, W. et al. Regulatory effects and mechanism of action of green tea polyphenols on osteogenesis and adipogenesis in human adipose tissue-derived stem cells. Curr. Issues Mol. Biol.44 (12), 6046–6058 (2022).
Xu, W. et al. Biodegradable calcium carbonate/mesoporous silica/poly(lactic-glycolic acid) microspheres scaffolds with osteogenesis ability for bone regeneration. RSC Adv.11 (9), 5055–5064 (2021).
Park, K. R. et al. TMARg, a novel anthraquinone isolated from rubia cordifolia Nakai, increases osteogenesis and mineralization through BMP2 and beta-catenin signaling. Int. J. Mol. Sci.21 (15). (2020).
Mauro, A. G. et al. The role of NLRP3 inflammasome in pericarditis: potential for therapeutic approaches. JACC Basic Transl Sci.6 (2), 137–150 (2021).
Vivas, D. et al. Derivation of multipotent mesenchymal stromal cells from ovine bone marrow. Curr. Protoc. Stem Cell. Biol.44, 2B–9B (2018).
Liu, Y. et al. Animal models of complex regional pain syndrome type I. J. Pain Res.14, 3711–3721 (2021).
Lebaschi, A. H. et al. Biomechanical, histologic, and molecular evaluation of tendon healing in a new murine model of rotator cuff repair. Arthroscopy34 (4), 1173–1183 (2018).
Akhter, M. P. & Recker, R. R. High resolution imaging in bone tissue research-review. Bone143, 115620 (2021).
Liu, Y. et al. Influence of Chinese herbal formula on bone characteristics of Cobb broiler chickens. Genes (Basel)13 (10). (2022).
Chen, H. et al. Clinical diagnosis of gastric cancer by high-sensitivity THz fiber-based fast-scanning near-field imaging. Cancers (Basel)14 (16). (2022).
Chen, B. et al. Elimination of senescent cells by senolytics facilitates bony endplate microvessel formation and mitigates disc degeneration in aged mice. Front. Cell. Dev. Biol.10, 853688 (2022).
Li, Y. et al. Physical and chemical properties, biosafety evaluation, and effects of nano natural deer bone meal on bone marrow mesenchymal stem cells. Front. Bioeng. Biotechnol.10, 891765 (2022).
Sun, Y. et al. Plasma spray vs. electrochemical deposition: toward a better osteogenic effect of hydroxyapatite coatings on 3D-printed titanium scaffolds. Front. Bioeng. Biotechnol.9, 705774 (2021).
Drager, J. et al. Hypoxia biomimicry to enhance monetite bone defect repair. Tissue Eng. Part A23 (23–24), 1372–1381 (2017).
Xu, Q. et al. Enhancing osteogenesis and angiogenesis functions for Ti-24Nb-4Zr-8Sn scaffolds with methacrylated gelatin and deferoxamine. Front. Bioeng. Biotechnol.12, 1372636 (2024).
Yan, Y. et al. Vascularized 3D printed scaffolds for promoting bone regeneration. Biomaterials 190–191 (2019).
Acknowledgements
This research was financially supported by The Program for Science and Technology Project of Guizhou Province. Qiankehe Platform Talents (No. [2021] 5613) and The Key Program for Science and Technology Project of Guizhou Province (No. ZK [2021] 007) and The Grants from the National Natural Science Foundation of China (82160577) and Guangdong Province Science and Technology Plan Project (2020B1111560001). Hundred Talents Program of Guangdong Academy of Sciences (2020GDASYL-20200102005). GDAS’ Project of Science and Technology Development (2022GDASZH-2022010110).
Author information
Authors and Affiliations
Contributions
Honghan Wu: Writing—original draft, Software, Methodology, Investigation. Jun Huang: Resources, Methodology, Formal analysis. Hengpeng Wu: Validation, Methodology. Weikang Xu: Visualization, Data curation. Qian Zhong: Visualization, Software.Jiaxiang Song: Funding acquisition.Xitao Linghu: Validation, Conceptualization. Botao Gao: review & editing. Qingde Wa: Writing—review & editing, Supervision, Conceptualization.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Statement of ethics
All experimental protocols of this study have been approved by the Medical Ethics Committee of Zunyi Medical University, and all methods were carried out in accordance with ARRIVE guidelines and regulations (the anesthesia method used in this study was abdominal injection of pentobarbital sodium).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, H., Huang, J., Wu, H. et al. Enhancement of in vitro and in vivo bone repair performance of decalcified bone/gelma by desferrioxamine. Sci Rep 15, 14092 (2025). https://doi.org/10.1038/s41598-025-99101-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-99101-w