Abstract
Frailty is associated with poor outcomes in heart failure (HF). Handgrip strength (HGS) is a simple indicator of Physical frailty. We aimed to assess the prognostic value of HGS in patients under 60 years old with acute decompensated HF with reduced ejection fraction (HFrEF). In this cross-sectional study, we enrolled 125 patients with acute decompensated HFrEF. HGS was measured using a manual dynamometer. The primary outcome was in-hospital mortality. Univariate logistic regression analysis was performed to identify risk factors associated with in-hospital mortality. Receiver operating characteristic (ROC) curve analysis was used to assess the predictive value of HGS for in-hospital mortality. The in-hospital mortality rate was 16%. Survivors had numerically higher, though not statistically significant, median HGS compared to non-survivors (18.8 (IQR: 13.2–25.3) kg vs. 13 (IQR: 11.4–19.5) kg; p = 0.06). HGS showed negative correlation with length of stay (rho = − 0.202, p = 0.024) and NT-proBNP levels (rho = − 0.256, p = 0.004). The area under the ROC curve for overall HGS predicting in-hospital mortality was 0.630 (p = 0.043). Lower left ventricular ejection fraction and higher NT-proBNP levels were significantly associated with increased odds of in-hospital mortality in univariate analysis. Lower handgrip strength was associated with longer hospital stay and higher NT-proBNP levels, and demonstrated a modest ability to predict in-hospital mortality. However, further research is necessary to establish standardized measurement methods and optimal prognostic thresholds before handgrip strength can be widely implemented in the management of this patient population.
Similar content being viewed by others
Introduction
Heart failure (HF) is a significant global health issue, with an estimated 26 million people affected worldwide in 20171. The impact of HF extends beyond physical health, as it places a considerable psychological and economic burden on patients, their families, and healthcare systems. Therefore, there is an ongoing need to enhance risk assessment, prevention, and management strategies to reduce the morbidity, mortality, and healthcare costs associated with this condition2.
Frailty, a complex and multi-dimensional syndrome characterized by decreased resistance to stressors and increased vulnerability to adverse outcomes, is strongly associated with HF. It is estimated to affect almost 50% of patients with HF, with this number rising to 77% in hospitalized patients due to HF3,4,5. It has been widely documented that this condition correlates with poor prognosis, including increased rates of hospitalization, functional decline, and mortality4,6,7. Handgrip strength (HGS) is a simple, inexpensive, and reliable measure of muscle strength that is often used as part of the physical/functional component in frailty assessments8. A recent meta-analysis by Wang et al. has shown that lower HGS is associated with an increased risk of mortality in patients with HF across various age groups. Importantly, they found no significant effect of age on the relationship between HGS and mortality in HF patients9. In HF patients, reduced HGS may reflect skeletal muscle wasting (sarcopenia) and dysfunction, which are common features of the disease and can be evident even in younger HF patients5,9.
While the prevalence and prognostic impact of physical frailty in patients with acute decompensated heart failure (ADHF) has been reported10,11, the specific role of HGS in patients with HFrEF hospitalized due to ADHF has been less extensively studied9. However, notable contributions to this field include the work of Parahiba et al.12, who investigated HGS in ADHF patients, demonstrating its potential as both a predictor of malnutrition and a prognostic marker for short-term mortality. Despite this valuable research, there remains a need for further investigation to fully elucidate the role of HGS in risk stratification and management of patients with HFrEF hospitalized due to ADHF, particularly in diverse populations and clinical settings.
Based on current literature, we hypothesized that lower handgrip strength would correlate with poorer clinical outcomes in acute decompensated HFrEF patients under 60 years old. This study aims to explore the potential prognostic significance of HGS in patients with HFrEF admitted due to ADHF. By comprehensively assessing HGS and its association with surrogates of clinical outcomes in patients younger than 60 years with acute decompensated HFrEF, we aim to contribute to the growing body of evidence supporting the use of frailty assessment tools in HF management and guide future research and clinical practice.
Materials and methods
Design and population
This cross-sectional study was conducted between April 2023 and October 2023 at Rajaie Cardiovascular Medical and Research Institute, a tertiary care center for heart failure medicine in Tehran, Iran. The study population included adult patients (18–60 years) who were enrolled with a primary diagnosis of ADHF and a diagnosis of chronic heart failure with reduced ejection fraction (HFrEF; left ventricular ejection fraction [LVEF] ≤ 40%) for at least three months. The primary decision on ADHF diagnosis, confirmed by a heart failure (HF) specialist according to the 2021 European Society of Cardiology (ESC) guidelines, was made by emergency department physicians13. In addition, the management plan was applied and followed by HF specialists considering the ESC guidelines during hospitalization, including the adjustment of diuretics and inotropes (if needed), the initiation or adjustment of medical therapies recommended in the guidelines for HFrEF, including angiotensin receptor/neprilysin inhibitor (or angiotensin-converting enzyme inhibitor if ARNI is not tolerated or contraindicated), a beta blocker, a mineralocorticoid receptor antagonist (MRA), a SGLT2 inhibitor, and a discharge plan.
Exclusion criteria include: (1) patients with acute Denovo heart failure; (2) inability to perform the HGS test with a manual dynamometer due to physical limitations or cognitive impairment; (3) presence of acute conditions, including acute coronary syndrome, acute pulmonary emboli, prosthetic valve malfunction, or cardiogenic shock requiring immediate intervention (mechanical ventilation support, ventricular assist device support, etc.); (4) any uncontrolled chronic condition, excluding heart failure (HF), such as diabetic ketoacidosis, end-stage renal disease (ESRD) requiring hemodialysis, or primary skeletal myopathies, including but not limited to muscular dystrophies, congenital myopathies, metabolic myopathies, and inflammatory myopathies, should be present; (5) The inability to continue the guideline-recommended medical therapies for HFrEF14; and (6) severe malnutrition or cachexia15. After screening patients, study physicians enrolled them for further assessment and data collection if they met eligibility criteria.
The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki and was reviewed and approved by the Ethics Committee of Rajaie Cardiovascular Medical and Research Institute, Tehran, Iran (IR.RHC.REC.1402.034). Written informed consent was obtained from all study participants prior to their enrollment, and all participants voluntarily provided consent for their medical records to be used in this research. In total, 337 patients were screened, and 125 were identified as eligible for further evaluation.
Patient assessment and data collection
After obtaining informed consent, the patient’s assessment was performed within 24 h of hospital admission. Trained physicians (M.B. and A.S.), whose competence in with the instruments was subjectively assessed as satisfactory by an experienced supervisor (S.A.) prior to data collection, performed the HGS assessments. Demographic information (age, sex, and BMI), comorbidities (hypertension, diabetes mellitus, chronic kidney disease, illicit drugs, alcohol, and smoking status), heart failure etiology (ischemic or nonischemic), and other clinical (NYHA class, in-hospital mortality, length of hospital stay) and laboratory data (including NT-Pro-BNP) were obtained from medical records and confirmed during patient assessment. All patients were visited and followed by heart failure experts during their hospital stay. Guideline-directed medical therapies (GDMT) were initiated and adjusted for all patients in the study prior to discharge. The entire study population was monitored for early readmission or all-cause mortality for one month after discharge.
Our primary endpoint was in-hospital mortality, defined as death during the patient’s hospitalization for treatment of acute decompensated heart failure (ADHF). Secondary endpoints included length of hospital stay, defined as the number of days a patient remained hospitalized for treatment of ADHF from the day of admission to the day of discharge, and a composite of all-cause mortality and readmission within 1 month of discharge, which included either mortality or readmission to hospital for heart failure within 30 days of discharge from the first hospitalization for ADHF.
Handgrip strength assessment
HGS was measured using a calibrated Jamar® handheld dynamometer (Sammons Preston, Bolingbrook, IL, USA). Prior to testing, participants received standard instructions, demonstrations and familiarization with the procedures16. Manual dynamometry was performed with both hands. Patients performed the test in a seated position with their hips flexed at 90°, arms hanging beside the trunk and elbows flexed at 90°. They were instructed to squeeze the handles with maximum force. The dominant hand was recorded for each patient, and three maximal contractions were required for each hand, with a 1-minute rest between each trial. The average of the three readings was taken as the final score for each hand17. To compare our results with normal values, we used the handgrip strength data for the Iranian population published by Mohammadian et al.18.
Statistical analysis
Continuous variables were expressed as medians (interquartile range, IQR). Categorical variables were expressed as numbers (percentages). The Shapiro-Wilk test assessed the normality of the data distribution for all continuous variables.
Due to the non-normal distribution of the data, non-parametric tests were used for the analyses. The Mann-Whitney U test was used to compare continuous variables between two groups, such as HGS (total, dominant hand, and non-dominant hand) between survivors and non-survivors and between readmitted/deceased within one month and not readmitted/deceased within one month.
Spearman’s rank correlation coefficient (Spearman’s rho) was calculated to assess the relationship between continuous variables, such as total HGS and NT-proBNP levels, and total HGS and the length of hospital stay.
Logistic regression analyses were performed to identify risk factors associated with in-hospital mortality. For the univariate analysis, we selected variables based on their clinical relevance to heart failure outcomes and previous literature. These included demographic factors (age, sex), heart failure characteristics (disease duration, etiology, left ventricular ejection fraction), comorbidities (diabetes mellitus, hypertension, chronic kidney disease), lifestyle factors (smoking), laboratory parameters (hemoglobin, BUN, creatinine, eGFR, NT-proBNP), and our primary variable of interest, handgrip strength (overall, dominant hand, and non-dominant hand). We also constructed three multivariate logistic regression models. For these models, we included variables that showed statistical significance in the univariate analysis or demonstrated a significant correlation/association with in-hospital mortality in other statistical tests. To avoid multicollinearity, we created separate models for overall handgrip strength, dominant hand strength, and non-dominant hand strength (Models 1, 2, and 3, respectively).
Receiver operating characteristic (ROC) curve analysis was performed to assess the predictive value of total HGS, HGS of the dominant hand, and HGS of the non-dominant hand for in-hospital mortality. The area under the curve (AUC) was calculated, and the optimal cutoff value was determined by maximizing the Youden index (sensitivity + specificity minus 1).
A two-sided p-value of < 0.05 was considered statistically significant. Analyses were performed using IBM SPSS Statistics for Windows, version 27.0 (IBM Corp., Armonk, NY). In addition, data visualization was performed using MedCalc® Statistical Software Version 22 (MedCalc Software Ltd., Ostend, Belgium).
Results
Baseline characteristics
The study included 125 patients with ADHF with reduced ejection fraction (HFrEF). The median age of the participants was 53 years (IQR: 45–57), with the majority (41.6%) in the 55–60 age group, and 32% (n = 40) of the participants being female. The median BMI was 26.6 kg/m2 (IQR: 22.6–32.3). Ischemic etiology was present in 52.8% (n = 66) of patients, and the median disease duration was 24 months (IQR: 3–90). Comorbidities included hypertension (40.8%, n = 51), diabetes mellitus (26.4%, n = 33), and chronic kidney disease (23.2%, n = 29). The median left ventricular ejection fraction (LVEF) was 15% (IQR: 10–30), and the median level of N-terminal pro-B-type natriuretic peptide (NT-proBNP) was 6500 pg/ml (IQR: 3789–12367). In addition, 54.4% and 40% of the study population fell into NYHA functional classes III and IV, respectively. All patients received tolerable doses of GDMT at the time of discharge. Table 1 summarizes the details of demographic and laboratory data.
The median total hand grip strength (HGS) was 18.2 kg (IQR: 12.2–25.1), with the HGS of the dominant hand being 19.2 kg (IQR: 13.7–26) and the HGS of the non-dominant hand being 16.2 kg (IQR: 11–23) (Table 1). Looking at the normal values of HGS in different age and sex subgroups of the Iranian population18, the HGS values were below the lower limit of the norm in 81.2% of men and 50% of women.
Analysis of factors associated with overall HGS revealed several significant relationships (Tables S1 and S2). Age showed a weak negative correlation with HGS (r = -0.184, p = 0.040), while NT-proBNP levels demonstrated a stronger negative correlation (r = -0.256, p = 0.004). The scatterplot (Fig. 1) shows the relationship between HGS and NT-proBNP levels in the study population. The 95% confidence interval for the Spearman’s rho correlation coefficient ranged from − 0.417 to -0.079, further confirming the significant inverse relationship between these two variables. Gender was significantly associated with HGS, with males having higher median HGS (21.3 kg, IQR: 13.5–27.7) compared to females (13.4 kg, IQR: 8.9–17.6) (p < 0.001). Smoking status was also associated with HGS, with non-smokers showing higher median HGS (25 kg, IQR: 17.2–28.5) compared to smokers (16.1 kg, IQR: 11.6–23) (p = 0.002). Patients without chronic kidney disease had higher median HGS (19.1 kg, IQR: 13-25.4) compared to those with the condition (14.1 kg, IQR: 10.7–19.7) (p = 0.028).
Other factors, including BMI, LVEF, disease duration, eGFR, heart failure etiology, NYHA class, hypertension, and diabetes mellitus, did not show significant associations with overall HGS.
Association between HGS and patient outcomes
The median duration of hospitalization was nine days (IQR: 6–16). A significant, albeit weak, negative correlation was observed between HGS and length of stay (Spearman’s rho = -0.202, P = 0.024). The in-hospital mortality rate was 16% (n = 20). Patients who survived had a numerically higher, but not statistically significant, median HGS of 18.8 kg (IQR: 13.2–25.3) than those who did not survive (13 kg, IQR: 11.4–19.5; P = 0.066). Of the patients who survived hospitalization (n = 105), 33.3% (n = 35) were readmitted or died within one month. However, there was no significant difference in HGS between patients who were readmitted or died within one month and those who were not (P = 0.758) (Table 2).
Risk factors for in-hospital mortality
Univariate logistic regression was performed to identify risk factors associated with in-hospital mortality (Table 3). On analysis, two variables were found to be significantly associated with in-hospital mortality, including LVEF (OR = 0.935, 95% CI: 0.881–0.993, P = 0.029) and NT-proBNP levels (OR = 1.467, 95% CI: 1.167–1.817, P = 0.014). Although not statistically significant, diabetes mellitus (P = 0.087) and chronic kidney disease (P = 0.058), as well as hand grip strength (P = 0.06) (total, dominant, and non-dominant hand), showed a trend towards association with in-hospital mortality in this univariate analysis. Multivariate logistic regression models were also constructed (Models 1, 2, and 3 in Table 3), which included variables such as gender, age, chronic kidney disease, smoking status, LVEF, NT-proBNP, and various measures of HGS. However, in these adjusted models, none of the variables retained statistical significance.
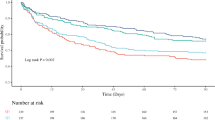
Predictive value of handgrip strength for in-hospital mortality: a ROC curve analysis
Figure 2 presents the ROC curves for predicting in-hospital mortality using HGS measurements and NT-proBNP levels. As shown in panel A, the AUC for overall HGS was 0.630 (95% CI: 0.539–0.714, p = 0.043), indicating a statistically significant, albeit modest, discriminatory ability to predict in-hospital mortality. However, it also indicates a potential for false positives if HGS were to be used as a prognostic tool. Similarly, the AUC for HGS of the non-dominant hand was 0.634 (95% CI 0.543–0.718, p = 0.039), and the AUC for HGS of the dominant hand was 0.624 (95% CI 0.533–0.709, p = 0.054) (Panels B and C). These results suggest that HGS, particularly when measured in total or in the non-dominant hand, has a comparable predictive value for in-hospital mortality in this patient population.
Overall HGS and HGS for the dominant and non-dominant hands had optimal cutoff values of 14.4 kg (sensitivity: 60%, specificity: 67.62%), 20.33 kg (sensitivity: 80%, specificity: 50.46%), and 14.7 kg (sensitivity: 66%, specificity: 63.81%), respectively. The Youden index was highest for HGS of the dominant hand (0.3048), followed by HGS of the non-dominant hand (0.2881) and HGS total (0.2762). However, the optimal cutoff value for HGS of the dominant hand (≤ 20.33) had a lower specificity (50.46%) than the other two variables.
NT-proBNP demonstrated the highest predictive ability with an AUC of 0.718 (p < 0.001), as shown in panel D. Panel E provides a visual comparison of the ROC curves for NT-proBNP and all HGS measurements. While NT-proBNP appears to have slightly better predictive performance, the curves for the HGS measurements closely follow each other, indicating similar predictive abilities among the different HGS measures. Additionally, pairwise comparisons of the ROC curves revealed no statistically significant differences between the AUCs of NT-proBNP and any of the HGS measurements, or among the different HGS measurements themselves (Table S3); suggesting that the predictive performance of HGS measurements for in-hospital mortality is not significantly different from that of NT-proBNP, a well-established biomarker in heart failure.
Discussion
The importance of frailty and sarcopenia in adult patients with HF younger than 60 years has been emphasized in recent studies from our institute5,19. In our current study, we investigated the prognostic value of HGS, a key component of physical frailty assessment, in patients with acutely decompensated HFrEF with a mean age of 53 years. In our study, a trend was observed for the association between HGS and in-hospital mortality (P = 0.06). Additionally, the length of hospital stay was significantly longer in patients with lower HGS scores. Chung et al., Parahiba et al., Tanaka et al., Wang et al., and Singh et al. demonstrated that lower HGS was associated with an increased risk of death in patients with heart failure9,12,20,21,22. Furthermore, we found no significant difference in HGS between patients who were readmitted or died within one month and those who were not (p = 0.896). This is in contrast to Joyce et al., who found that poor HGS was associated with a higher risk of readmission or emergency department visit within 6 months in hospitalized patients with heart failure23.
Singh et al. also found in a prospective study of 210 chronic HF patients that HGS alone had good predictive accuracy for mortality (area under the curve: 0.75, p < 0.001), with a cutoff value of 16.95 kg having a sensitivity of 72% and specificity of 63%21. Our study determined that the most effective threshold for overall HGS to predict in-hospital mortality was 14.4 kg. This threshold had a sensitivity of 0.6 and a specificity of 0.67. Although this threshold value can help identify patients at high risk, its moderate specificity indicates that it may also result in a significant number of false positives, potentially exaggerating the risk of death in certain patients.
The suggested prognostic value of HGS in young HF patients is thought to be due to its ability to detect the systemic effects of HF on skeletal muscle function and the general state of frailty, independent of the aging process9,24. Reduced muscle strength, as measured by HGS, may result from the complex interplay of factors in HF, including decreased cardiac output, chronic inflammation, metabolic dysfunction, and neurohormonal activation24. In addition, poor HGS could be a sign of an advanced stage of heart failure and be helpful in distinguishing those patients who require more comprehensive heart failure care and treatment25.
There are several possible reasons for our relatively different study results. First, it is important to note that our study was conducted at a tertiary referral center for heart failure. Therefore, our study population may represent a more advanced and severe stage of heart failure compared to the general heart failure population. The HGS levels, which were below the lower limit of normal in approximately 70% of our study population, a relatively high in-hospital mortality rate (16%), a significant early readmission rate despite attempts to achieve GDMT, and a negative correlation between NT-ProBNP levels and HGS emphasize the severity of the disease in our patient population.
Although several studies have provided convincing evidence for the prognostic value of HGS in HF patients, several limitations should be considered. First, the cutoff values for the definition of low HGS varied across studies, ranging from 16.95 kg to 25.5 kg12,21. This heterogeneity may reflect differences in patient population, measurement methods, and study design, but it also underscores the need for standardized definitions of frailty and low HGS in HF patients. Second, most studies were conducted in single centers or specific populations (e.g., elderly, acutely decompensated HF), which may limit the generalizability of results to the broader HF population. Third, the retrospective nature of some studies may introduce potential biases, such as selection and information bias, which could compromise the validity of the results.
Therefore, the generalizability of our results to other heart failure populations treated under different conditions may be limited. The high mortality and readmission rates observed in our studies underscore the complexity and severity of heart failure cases treated at our tertiary referral center. Future studies conducted in various clinical settings and patient populations are needed to validate our results and gain a deeper understanding of the prognostic value of handgrip strength and other factors across the spectrum of heart failure severity and treatment strategies.
This study has several strengths, including the focus on a specific patient population (acutely decompensated HFrEF in patients younger than 60 years old) and the comprehensive assessment of HGS and its relationship to various clinical outcomes. However, despite the valuable insight provided by the present study, it has some limitations. First, it is crucial to acknowledge that our study primarily assesses muscle strength via HGS measurement and does not constitute a comprehensive frailty evaluation. While HGS is a valuable component of physical function assessment, it does not capture the full spectrum of muscle function or the multidimensional nature of frailty. Therefore, our findings should be interpreted in the context of muscle strength rather than overall frailty. Second, the relatively small sample size may have limited the power to detect significant associations between HGS and mortality in the univariate analysis. As a single-center study conducted at a tertiary referral center for heart failure, our results may not be generalizable to all ADHF patients or to those treated in different clinical settings. Third, the severity of heart failure in our cohort, as evidenced by the high in-hospital mortality rate (16%) and significant early readmission rate, may differ from that seen in other centers or in the general heart failure population. Fourth, our study did not collect detailed data on specific treatments beyond GDMT or non-pharmacological interventions. Finally, the cross-sectional nature of our study limits our ability to assess changes in HGS over time and their relationship to long-term outcomes.
Despite these limitations, the consistent results of several studies with different designs, populations and statistical methods provide strong evidence for the association between reduced HGS and increased mortality risk in HF patients. The simplicity, low cost and ease of use of HGS measurement make it an attractive tool for risk stratification in clinical practice, especially in resource-limited settings. In addition, incorporating HGS into existing risk prediction models can improve their accuracy and help identify high-risk patients who may benefit from targeted interventions such as exercise training, nutritional support and medication optimization.
Conclusion
The assessment of HGS in patients with HF, especially those with ADHF and reduced EF aged less than 60 years, offers some potential prognostic insights that could aid clinical decision-making. The simplicity and relatively low cost of the test may suggest wider applicability. However, it is important to point out that further research is needed to clarify the measurement methods and determine optimal prognostic thresholds.
Data availability
All data gathered and analyzed during this study are included in this published article. In addition, the dataset used is available from the corresponding author upon reasonable request.
Abbreviations
- ADHF:
-
Acute decompensated heart failure
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- BNP:
-
B-type natriuretic peptide
- BUN:
-
Blood urea nitrogen
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- ED:
-
Emergency department
- eGFR:
-
Estimated glomerular filtration rate
- ESC:
-
European Society of Cardiology
- HF:
-
Heart failure
- HFrEF:
-
Heart failure with reduced ejection fraction
- HGS:
-
Handgrip strength
- IQR:
-
Interquartile range
- LVEF:
-
Left ventricular ejection fraction
- NT-proBNP:
-
N-terminal pro-B-type natriuretic peptide
- OR:
-
Odds ratio
- ROC:
-
Receiver operating characteristic
References
Savarese, G. & Lund, L. H. Global public health burden of heart failure. Card Fail. Rev. 3(1), 7–11 (2017).
Pratley, R. et al. Chap. 1: The burden of heart failure. Am. J. Med. 137(2S), S3–S8 (2024).
Denfeld, Q. E. et al. The prevalence of frailty in heart failure: A systematic review and meta-analysis. Int. J. Cardiol. 236, 283–289 (2017).
Valdiviesso, R. et al. Frailty phenotype in heart failure: A condition that transcends age. Revista Portuguesa de Cardiologia: Orgao Oficial da Sociedade Portuguesa de Cardiologia = Portuguese. J. Cardiology: Official J. Portuguese Soc. Cardiol. (23), S0870-2551 00044 (2023).
Hajahmadi, M. et al. Muscle wasting in young patients with dilated cardiomyopathy. J. Cachexia Sarcopenia Muscle 8(4), 542–548 (2017).
Talha, K. M. et al. Frailty and heart failure: State-of-the-art review. J. Cachexia Sarcopenia Muscle 14(5), 1959–1972 (2023).
Abdolmaleki, M., Ohadi, L. & Maleki, S. Dilated cardiomyopathy in patients with hypoparathyroidism: A narrative review. Health Sci. Rep. 7(1), e1796 (2024).
Chainani, V. et al. Objective measures of the frailty syndrome (hand grip strength and gait speed) and cardiovascular mortality: A systematic review. Int. J. Cardiol. 215, 487–493 (2016).
Wang, Y. et al. Handgrip strength and the prognosis of patients with heart failure: A meta-analysis. Clin. Cardiol. 46(10), 1173–1184 (2023).
Umehara, T. et al. Frailty in elderly patients with acute heart failure increases readmission. Heart Lung 57, 102–109 (2023).
Pandey, A. et al. Frailty among older decompensated heart failure patients: Prevalence, association with patient-centered outcomes, and efficient detection methods. JACC: Heart Fail. 7(12), 1079–1088 (2019).
Parahiba, S. M. et al. Handgrip strength in patients with acute decompensated heart failure: Accuracy as a predictor of malnutrition and prognostic value. Nutrition 91, 111352 (2021).
McDonagh, T. A. et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 42(36), 3599–3726 (2021).
Malgie, J. et al. Guideline-directed medical therapy for HFrEF: Sequencing strategies and barriers for life-saving drug therapy. Heart Fail. Rev. 28(5), 1221–1234 (2023).
Rahman, A. et al. Malnutrition and cachexia in heart failure. JPEN J. Parenter. Enter. Nutr. 40(4), 475–486 (2016).
Bobos, P. et al. Measurement properties of the hand grip strength assessment: A systematic review with meta-analysis. Arch. Phys. Med. Rehabil. 101(3), 553–565 (2020).
Roberts, H. C. et al. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 40(4), 423–429 (2011).
Mohammadian, M. et al. Normative data of grip and pinch strengths in healthy adults of Iranian population. Iran. J. Public. Health. 43(8), 1113–1122 (2014).
Khajali, Z. et al. Sarcopenia in young adults with congenital heart disease. JCSM Rapid Commun. 5(1), 77–85 (2021).
Chung, C. J. et al. Reduced handgrip strength as a marker of frailty predicts clinical outcomes in patients with heart failure undergoing ventricular assist device placement. J. Card. Fail. 20(5), 310–315 (2014).
Singh, G. et al. A simple effective method for frailty in heart failure with impact on clinical outcomes in North Indian population. J. Saudi Heart Assoc. 33(3), 213–220 (2021).
Tanaka, S. et al. Incremental value of objective frailty assessment to predict mortality in elderly patients hospitalized for heart failure. J. Card Fail. 24(11), 723–732 (2018).
Joyce, E. et al. Prospective assessment of combined handgrip strength and Mini-Cog identifies hospitalized heart failure patients at increased post-hospitalization risk. ESC Heart Fail. 5(5), 948–952 (2018).
Philippou, A. et al. Heart failure-induced skeletal muscle wasting. Curr. Heart Fail. Rep. 17(5), 299–308 (2020).
Hsi, B., Province, V. & Tang, W. H. W. Frailty in the advanced heart failure patient: A challenging, neglected, yet potentially modifiable risk factor. Curr. Treat. Options Cardiovasc. Med. 25(8), 261–271 (2023).
Funding
This research received no specific grant or financial support from funding agencies, commercial sources, or not-for-profit organizations.
Author information
Authors and Affiliations
Contributions
E.K.: Conceptualization; Methodology; Data curation; Formal analysis; Writing—original draft. S.A.: Conceptualization; Methodology; Data curation; Writing—review & editing. M.B.: Investigation; Methodology. A.S.: Investigation; Methodology. F.C.: Investigation; Methodology, Visualization. S.J.: Writing—review & editing; Formal analysis. EH: Writing—review & editing. R.O.: Supervision; Investigation; Methodology. S.T.: Supervision; Investigation; Methodology. M.M.: Supervision; Investigation; Methodology. Z.A.F.J.: Investigation; Methodology. M.B.: Investigation; Methodology. M.M.: Investigation; Methodology. S.M.: Data curation; Formal analysis. N.N.: Conceptualization; Supervision; Methodology; Writing—review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki and was reviewed and approved by the Ethics Committee of Rajaie Cardiovascular Medical and Research Center, Tehran, Iran (IR.RHC.REC.1402.034). In addition, written, signed, and dated informed consent was obtained from all study participants before enrollment. All participants voluntarily consented to have their medical records used in this research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kohansal, E., Adimi, S., Baghi, M. et al. Exploring the potential of handgrip strength as a prognostic marker in acute decompensated heart failure with reduced ejection fraction: a cross-sectional study. Sci Rep 15, 14076 (2025). https://doi.org/10.1038/s41598-025-99140-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-99140-3