Abstract
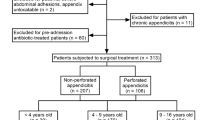
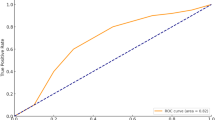
To analyze the clinical characteristics and perforation predictors of appendicitis in infants and toddlers younger than 3 years of age. A retrospective analysis was conducted on the children under 3 years old diagnosed with appendicitis and treated at two centers between March 2018 and May 2024. Based on pathological findings, patients were divided into perforated and non-perforated groups. Further classification was based on the presence or absence of post-appendectomy abscess, resulting in three groups: non-perforated, perforated with post-appendectomy abscess, and perforated without post-appendectomy abscess. Among 72 children with appendicitis, 45 were male (62.5%) and 27 were female (37.5%), with a median age of 31.0 (IQR, 27.0–34.0) months and an average weight of 13.7 ± 2.7 kg. Abdominal ultrasound had a positivity rate of 69.4% (50/72), and 22 patients underwent additional CT scans. All cases were treated with laparoscopic appendectomy, without conversions to open surgery. Perforated appendicitis was diagnosed in 58 cases (80.6%), and non-perforated appendicitis in 14 cases (19.4%). The median symptom duration (48.0 vs. 21.0 h; p < 0.01), CRP levels (70.5 vs. 22.0 mg/L; p < 0.05), and incidence of appendicoliths were significantly higher in the perforated group (p < 0.05). Post-appendectomy abscess was the most common complication, with appendicoliths and prolonged symptom duration being significant risk factors (p < 0.05). The perforated group with post-appendectomy abscess had a significantly longer median hospital stay than the non-perforated group (12.0 vs. 6.0 days; p < 0.01). ROC analysis identified CRP (AUC 0.69, cutoff 34.5 mg/L; p < 0.05) and symptom duration (AUC 0.74, cutoff 35 h; p < 0.01) as predictors of perforation. The high perforation rate of appendicitis in infants and toddlers is associated with prolonged symptoms, elevated CRP, and appendicoliths. Extended symptom duration and appendicoliths increase the risk of post-appendectomy abscesses.
Similar content being viewed by others
Introduction
Acute appendicitis is one of the most common causes of acute abdominal pain in children, with epidemiological data indicating a lifetime risk of approximately 4%1,2. If left untreated, acute appendicitis may progress to perforation, rapidly leading to severe complications such as peritonitis and sepsis. These conditions not only pose a serious threat to the child’s life but also impose significant psychological and financial burdens on the family. Studies have shown that the risk of perforated appendicitis is strongly associated with the child’s age, with younger children being more susceptible to developing perforation3.
In older children, the symptoms and signs of appendicitis are relatively typical, making diagnosis more straightforward. However, as age decreases, particularly in children under the age of 3, clinical presentations often become atypical, leading to significantly higher misdiagnosis rates and an increased risk of progression to perforated appendicitis. This poses a considerable challenge for clinical diagnosis. According to the literature, the misdiagnosis rate for appendicitis in children under 12 years old ranges from 28 to 57%, while in infants and toddlers under 2 years old, it can reach as high as 100%4.
Currently, research on the diagnosis of acute appendicitis in children primarily focuses on laboratory tests. Studies have shown that combining white blood cell (WBC) count and C-reactive protein (CRP) testing can significantly improve diagnostic sensitivity, thereby reducing the likelihood of missed diagnoses5. Additionally, Pentraxin-3, a novel biomarker, has been found to rise rapidly in patients with acute appendicitis and demonstrates superior early diagnostic performance compared to CRP. However, it cannot distinguish between perforated and non-perforated appendicitis6.
Other studies suggest that interleukin-6 and fibrinogen may help predict the severity of acute appendicitis, though their value in diagnosing perforation remains unclear7,8. Research also indicates that serum sodium levels are significantly lower in children with perforated appendicitis compared to those with non-perforated appendicitis. However, hyponatremia serves only as an auxiliary marker and must be interpreted alongside clinical presentations and other laboratory findings9.
Commonly used appendicitis diagnostic scoring systems, such as the Pediatric Appendicitis Risk Calculator, the Pediatric Appendicitis Score, and the Alvarado score, can assist emergency or primary care physicians in the initial evaluation of suspected appendicitis10,11,12. However, the diagnostic accuracy and acceptance of these tools vary significantly, with certain limitations in their application to pediatric populations13.
In infants and toddlers under the age of 3, the atypical clinical presentation of appendicitis and the high rate of misdiagnosis make it difficult to rely solely on a single laboratory test or scoring tool for diagnosis. Accurate diagnosis requires a comprehensive evaluation of clinical symptoms, laboratory findings, and, when necessary, imaging studies to improve diagnostic accuracy and timeliness. Given the limited research available on appendicitis in this age group, this study aims to analyze the clinical characteristics and diagnostic strategies for appendicitis in infants and toddlers. The goal is to reduce the rate of misdiagnosis and provide pediatric surgeons with more reliable diagnostic and treatment guidance, ultimately improving the prognosis for this special population.
Methods and materials
Study design
This study retrospectively analyzed the clinical data of children under 3 years old diagnosed with appendicitis and treated at Yangzhou Maternal and Child Health Care Hospital and Shanghai Children’s Hospital between March 1, 2018, and May 30, 2024.
Study population
Inclusion Criteria: (1) Children with appendicitis who received diagnosis and treatment at two centers between March 1, 2018, and May 30, 2024; (2) Children under the age of 3; (3) Cases definitively diagnosed as appendicitis preoperatively or intraoperatively.
Exclusion Criteria: (1) Cases with incomplete clinical data or missing key information; (2) Patients who were referred after receiving treatment at other medical institutions and for whom complete medical history and examination results could not be obtained; (3) Cases in which pathological examination did not confirm appendicitis; (4) Patients with severe systemic diseases or immunodeficiencies (e.g., malignant tumors, congenital immunodeficiency disorders).
Data collection
The data collected included the following: (1) demographic information: gender, age, and weight; (2) clinical presentation: symptoms (fever, abdominal pain, vomiting, diarrhea), and physical signs (tenderness, abdominal mass, peritonitis); (3) symptom duration; (4) laboratory findings: WBC count and CRP levels; (5) imaging findings: appendiceal diameter, presence of appendicoliths, and intraperitoneal free fluid as observed via ultrasound or computed tomography (CT) imaging; (6) surgical approach; (7) pathological types of appendicitis; (8) microbiological findings from pus cultures; (9) postoperative complications; (10) length of stay in hospital.
Study groups
Based on the pathological findings of the appendix, the patients were categorized into perforated appendicitis group and non-perforated appendicitis group. Furthermore, based on the presence or absence of post-appendectomy abscess, the patients were divided into three groups: non-perforated group, perforated group without post-appendectomy abscess, and perforated group with post-appendectomy abscess. Differences in demographic characteristics, clinical presentations, laboratory findings, and imaging results were compared across the groups. For clinically significant factors, receiver operating characteristic (ROC) curves were plotted to determine the optimal cutoff values and evaluate their predictive performance.
Statistical analysis
Data were analyzed using SPSS 25.0 (IBM Corp., Armonk, NY). Normally distributed continuous variables are expressed as mean ± standard deviation, and non-normally distributed variables as the median and interquartile range (IQR). Categorical variables are presented as numbers and percentages. Comparisons were made using the t-test, Mann–Whitney U test, chi-squared test, one-way analysis of variance or Kruskal-Wallis H test, as appropriate. ROC curves were constructed to determine optimal cutoff values using the Youden index, and diagnostic performance was assessed. A two-sided p-value < 0.05 was considered statistically significant. Graphs were created using R software (version 4.3.1; R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 72 pediatric patients were included in this study, comprising 45 males (62.5%) and 27 females (37.5%). The median age of the patients was 31.0 (IQR, 27.0–34.0) months, with an average weight of 13.7 ± 2.7 kg. The median duration of symptoms was 48.0 (IQR, 20.5–72.0) hours. All patients underwent abdominal ultrasound, which had a positive detection rate of 69.4% (50/72 cases). Among these, 22 patients underwent additional abdominal CT scans.
Of the 72 patients, 15 were misdiagnosed, resulting in a misdiagnosis rate of 20.8%. The causes of misdiagnosis included conditions such as gastroenteritis, intussusception, and intestinal obstruction, etc. All patients underwent laparoscopic surgery under general anesthesia, during which a systematic and detailed laparoscopic exploration of the abdominal cavity was performed. The appendix was removed using an ultrasonic scalpel and retrieved through the umbilical port. None of the cases required conversion to open surgery.
Postoperative pathological examination confirmed perforated appendicitis in 58 cases (80.6%), including 8 out of 9 infants. The most common pathogen identified in pus cultures was Escherichia coli, observed in 38 cases (Table 1). All patients were successfully discharged postoperatively, and follow-up was conducted for all cases (2 months to 6 years). No patients required readmission during the follow-up period.
The incidence of appendicoliths was significantly higher in the perforated group than in the non-perforated group (p < 0.05). The median symptom duration in the perforated group was 48.0 (IQR, 24.0–72.0) hours, which was significantly longer than that in the non-perforated group (median, 21.0 h, IQR: 10.8–48.0 h; p < 0.01). There was no significant difference in WBC count between the two groups, with a median of 15.0 (IQR, 11.0–18.0) × 10⁹/L in the perforated group and 14.0 (IQR, 12.0–22.0) × 10⁹/L in the non-perforated group. However, the CRP level was significantly higher in the perforated group, with a median of 70.5 (IQR, 19.8–123.3) mg/L, compared to 22.0 (IQR, 8.0–77.0) mg/L in the non-perforated group (p < 0.05). These findings are summarized in Table 2; Fig. 1.
None of the patients experienced adhesive intestinal obstruction or wound infection postoperatively. The most common complication was post-appendectomy abscess, which occurred exclusively in the perforated group (24/58 cases). All cases of abscess were successfully treated with intravenous anti-inflammatory therapy.
Patients were categorized into three groups based on the presence or absence of post-appendectomy abscess formation. The incidence of appendicoliths was significantly higher in the perforated group with post-appendectomy abscess compared to both the non-perforated group and the perforated group without post-appendectomy abscess (p < 0.05) (Table 3). The duration of symptoms in the non-perforated group (median 21.0 h, IQR: 10.8–48.0 h) was significantly shorter than that in the perforated group with post-appendectomy abscess (median 48.0 h, IQR: 35.0–72.0 h; p < 0.01) (Fig. 2A).
The median WBC count and CRP levels were as follows: in the non-perforated group, WBC 14.0 (IQR, 12.0–22.0) × 10⁹/L and CRP 22.0 (IQR, 8.0–77.0) mg/L; in the perforated group without post-appendectomy abscess, WBC 15.0 (IQR, 11.0–18.0)× 10⁹/L and CRP 71.5 (IQR, 12.0–140.5) mg/L; and in the perforated group with post-appendectomy abscess, WBC 14.0 (IQR, 11.0–18.8) × 10⁹/L and CRP 70.5 (IQR, 29.0–112.3) mg/L. No significant differences in WBC count or CRP levels were observed among the three groups (Fig. 2B, 2C). However, the length of stay was significantly longer in the perforated group with post-appendectomy abscess (median: 12.0 days, IQR: 10.3–13.8 days) compared to the non-perforated group (median: 6.0 days, IQR: 5.0–8.0 days; p < 0.01) (Fig. 2D).
The area under the ROC curve (AUC) for CRP in predicting appendiceal perforation was 0.69 (p < 0.05), with an optimal cutoff value of 34.5 mg/L, a sensitivity of 68.97%, and a specificity of 64.29%. The AUC for symptom duration in predicting appendiceal perforation was 0.74 (p < 0.01), with an optimal cutoff value of 35 h, a sensitivity of 67.24%, and a specificity of 71.43% (Fig. 3).
Box Plots of Symptom Duration, White Blood Cell (WBC) Count, and C-reactive Protein (CRP) Level Between Perforated and Non-Perforated Groups. A. The median symptom duration was significantly longer in the perforated group compared to the non-perforated group.B. There was no significant difference in WBC count between the two groups. C. The median CRP level was significantly higher in the perforated group compared to the non-perforated group. Statistical symbols: *: p < 0.05, **: p < 0.01.
Box Plots of Symptom Duration, White Blood Cell (WBC) Count, C-reactive Protein (CRP) Level, and Length of Stay in Hospital in Non-Perforated, Perforated with Post-Appendectomy Abscess, and Perforated without Post-Appendectomy Abscess Groups. A. The symptom duration was significantly shorter in the non-perforated group compared to the perforated with post-appendectomy abscess group. B. There was no significant difference in WBC count among the three groups. C. There was no significant difference in CRP level among the three groups. D. The length of stay in hospital was significantly longer in the perforated with post-appendectomy abscess group compared to the non-perforated group. Statistical symbols: **: p < 0.01.
Receiver Operating Characteristic (ROC) Curves for Symptom Duration and C-reactive Protein (CRP) Levels. The area under the ROC curve (AUC) for symptom duration was 0.74 (p < 0.01), with an optimal cutoff value of 35 h, a sensitivity of 67.24%, and a specificity of 71.43%. The AUC for CRP was 0.69 (p < 0.05), with an optimal cutoff value of 34.5 mg/L, a sensitivity of 68.97%, and a specificity of 64.29%.
Discussion
Previous studies have shown that infants and toddlers account for only 2.3–5.4% of all pediatric appendicitis cases14,15. Due to the atypical and nonspecific symptoms of appendicitis in this age group, misdiagnosis or missed diagnosis is common, often resulting in delayed treatment. Furthermore, the perforation rate in appendicitis cases among infants and toddlers is significantly higher. Bonadio et al. reviewed risk factors associated with appendicitis in 180 preschool children and identified 53 cases in children under 3 years old, with a perforation rate as high as 82.8%16. Similarly, Pogorelić et al. studied the clinical characteristics and treatment outcomes of appendicitis in children under 5 years old, identifying 26 cases of appendicitis in infants and toddlers, 21 of which were perforated, accounting for 80.8%17. In the present study, a total of 72 cases of appendicitis in infants and toddlers were included, among which 58 cases were perforated appendicitis (80.6%). This perforation rate is consistent with the data reported in the aforementioned studies16,17.
The high perforation rate in infants and toddlers may be attributed to several factors. First, their anatomical structures are not yet fully developed, lacking a well-formed omental barrier to contain inflammation within the abdominal cavity. This makes appendicitis more likely to progress rapidly to perforation and peritonitis. Second, infants and toddlers, particularly infants (9/72 cases), have not yet developed fluent language skills and are unable to accurately describe symptoms associated with appendicitis, which may lead to delays in diagnosis and treatment. In addition, the atypical nature of clinical symptoms significantly increases the difficulty of diagnosis. This may be partly attributed to the inability of pediatric patients to clearly describe the specific location of abdominal pain, resulting in clinical presentations that are often nonspecific, such as fever or vomiting. Moreover, abdominal pain in pediatric patients of this age group is a common manifestation of numerous conditions, such as constipation, gastroenteritis, intussusception, and intestinal colic, which further complicates the process of differential diagnosis. Finally, factors such as the age, educational level, and attentiveness of caregivers to early signs of discomfort in infants may also play a critical role in the occurrence of appendiceal perforation. In this study, 8 out of 9 cases of appendicitis in infants involved perforation, with a perforation rate approaching 90%. The only non-perforated case was a 7-month-old male infant. We speculate that this may be attributed to the caregivers’ heightened sensitivity to early signs of discomfort in the infant, allowing timely diagnosis and treatment during the early stages of the disease, successfully preventing appendiceal perforation.
Studies have shown that appendiceal perforation may be associated with various risk factors such as age, duration of symptoms, elevated WBC, elevated CRP, and the presence of appendicoliths18,19,20,21. However, most of these studies have focused on the entire pediatric age group or preschool-aged children, with relatively few studies specifically investigating risk factors for appendicitis in infants and toddlers. The results of this study indicate that appendiceal perforation in infants and toddlers is closely associated with symptom duration, elevated CRP levels, and the presence of appendicoliths.
This study found that the duration of symptoms was significantly longer in the perforated group than in the non-perforated group, and even longer in the perforated group with post-appendectomy abscess compared to the non-perforated group (p < 0.01). This finding suggests that the longer the duration of symptoms, the higher the risk of appendiceal perforation in infants and toddlers, and the greater the likelihood of post-appendectomy abscess formation. In this study, the incidence of post-appendectomy abscess formation was as high as 33.3% (24/72 cases). This not only prolonged the length of stay in hospital and increased the complexity of treatment and patient suffering but also imposed a greater economic burden on families and society. Therefore, early detection and timely management of appendicitis in infants and toddlers are critically important. To achieve this, efforts should be made to strengthen prevention and health education. On one hand, educational outreach targeting parents of pediatric outpatients should be conducted to raise awareness of the atypical presentation of appendicitis in infants and toddlers, as well as the severe consequences of delayed treatment. On the other hand, during clinical practice, prompt diagnosis and early surgical intervention should be emphasized. Although theoretically, early surgery helps prevent disease progression, previous studies have shown that prolonged time from admission to surgery is not an independent risk factor for perforated appendicitis22,23. Therefore, enhancing caregivers’ sensitivity to early signs of the disease may be even more critical. This study also found that infants and toddlers with a symptom duration exceeding 35 h were more likely to develop perforated appendicitis. This finding further underscores the importance of early recognition, diagnosis, and treatment, providing strong clinical guidance for practice. It also highlights a potential direction for interventions aimed at reducing the complication rate of appendicitis in infants and toddlers.
Evidence from the literature indicates that WBC and CRP, as combined biomarkers, demonstrate clinical utility in the diagnosis of appendicitis and in differentiating perforated from non-perforated cases. However, using either marker alone is insufficient for accurate prediction24,25. Interestingly, our findings differ slightly from previous reports. In this study, there was no significant difference in WBC levels between the perforated and non-perforated groups, whereas CRP levels showed a statistically significant difference. This suggests that CRP may have value in predicting whether appendicitis in infants and toddlers has progressed to perforation. However, CRP levels did not show a significant difference in predicting the occurrence of post-appendectomy abscesses. This indicates that while CRP may be a useful marker for predicting perforation, its role in assessing the risk of post-appendectomy abscess formation is limited. Our findings further demonstrate that when CRP levels exceed 34.5 mg/L, the likelihood of appendiceal perforation in infants and toddlers increases. Nevertheless, compared to symptom duration, the predictive efficacy of CRP remains limited. Therefore, a combined assessment of symptom duration and CRP levels may be a more effective strategy to improve the early identification and intervention for perforated appendicitis in this age group.
In this study, the positive rate of appendicoliths in the perforated group was 75.9%, significantly higher than the 42.9% observed in the non-perforated group. Additionally, patients with appendicoliths were more likely to develop post-appendectomy abscesses. Previous studies have reported that pediatric appendicitis with appendicoliths is often associated with persistent abdominal pain and more severe clinical symptoms, and children with appendicoliths are at a higher risk of perforation compared to those without appendicoliths19,26. CT imaging studies of appendicitis have shown that mechanical obstruction of the appendiceal lumen caused by appendicoliths is a key factor in the development of perforation. Obstruction by appendicoliths increases intraluminal pressure, leading to inflammation, edema of the appendiceal wall, and eventual erosion and perforation27,28. This mechanism elucidates why children with appendicitis associated with appendicoliths have an increased risk of perforation, underscoring the clinical importance of identifying appendicoliths in practice.
Abdominal ultrasound and CT have both demonstrated sensitivities and specificities exceeding 90% for diagnosing appendicitis29,30,31,32. However, these studies primarily focused on older children, while the diagnosis of appendicitis in infants and toddlers presents additional diagnostic challenges. False-negative results may be attributed to several factors, including poor cooperation due to crying or restlessness during the examination, tissue edema within the abdominal cavity, and atypical appendiceal positioning (e.g., retrocecal appendix), all of which make precise localization of the appendix more difficult. In this study, the positive detection rate of abdominal ultrasound was 69.4%, with 22 patients subsequently undergoing abdominal CT. Gonzalez et al. reported that ultrasound has lower sensitivity for detecting perforated appendicitis and appendicoliths, which may lead to missed diagnoses. Furthermore, ultrasound is highly operator-dependent, with accuracy varying significantly between hospitals and individual operators33. Thus, in cases where diagnosing appendicitis is challenging, abdominal CT serves as an important supplementary tool for improving diagnostic accuracy.
In summary, the atypical clinical presentation of appendicitis in infants and toddlers, combined with poor cooperation during physical examinations and uncertainties in imaging studies, poses significant challenges for pediatric surgeons. These challenges are further compounded when the pediatric surgeon lacks extensive clinical experience, potentially leading to underestimation or misdiagnosis of the condition, resulting in delayed diagnosis and treatment. Such delays not only prolong the course of the disease but may also indirectly increase the risk of appendiceal perforation, further exacerbating the patient’s condition. Therefore, improving the capacity for early diagnosis and comprehensive assessment of appendicitis in infants and toddlers is particularly critical.
This study focuses on the specific population of children under the age of three with appendicitis, a group for which relevant research remains scarce, thus demonstrating a certain degree of novelty. However, the study has several limitations: (1) Limited sample size: This study retrospectively analyzed a relatively small number of cases, which may introduce some degree of bias into the statistical results. For instance, the AUC values of CRP and symptom duration demonstrated moderate predictive efficacy. Future studies with larger sample sizes are needed to provide more robust and in-depth findings. (2) Potential influence of surgical expertise: The level of clinical experience of the operating surgeon might have contributed to the incidence of postoperative complications. This study was unable to exclude the impact of this factor. Future research should employ more robust study designs to address and control for such confounding variables. (3) Lack of comparison with other age groups: This study primarily concentrated on appendicitis in infants and toddlers, without incorporating comparative analyses with older pediatric age groups. Future studies should explore the similarities and differences in appendicitis across different age groups to provide a more comprehensive understanding of the disease.
Conclusion
Appendicitis in infants and toddlers is associated with a markedly high risk of perforation, closely linked to symptom duration, elevated CRP levels, and the presence of appendicoliths. Patients presenting with prolonged symptom duration and appendicoliths are at increased risk of developing post-appendectomy abscesses. Due to the atypical clinical presentation of appendicitis in this age group, misdiagnosis is frequent. Pediatric surgeons should maintain a high index of suspicion to facilitate early diagnosis and prompt intervention.
Data availability
The datasets used and analyzed during this study are available from the corresponding author on reasonable request.
Change history
21 June 2025
The original online version of this Article was revised: In the original version of this Article, the address of affiliation 2 was erroneously added as affiliation 3. The incorrect affiliation has been deleted.
References
Shannon, L. C., et al., Postoperative antibiotics, outcomes, and resource use in children with gangrenous appendicitis. JAMA Surg., 159(5). (2024).
Grith Laerkholm, H. et al. Changes in incidence and management of acute appendicitis in Children-A Population-Based study in the period 2000–2015. Eur. J. Pediatr. Surg., 31(4). (2020).
Sujoy, N. et al. Laparoscopic versus open appendicectomy for complicated appendicitis in children: A systematic review and meta-analysis. J. Pediatr. Surg., 57(3). (2021).
Yasmine, L. et al. Influence of age on clinical presentation, diagnosis delay and outcome in pre-school children with acute appendicitis. BMC Pediatr., 20(1). (2020).
David, F. C. et al. Diagnostic accuracy of blood tests of inflammation in paediatric appendicitis: a systematic review and meta-analysis. BMJ Open., 12(11). (2022).
Sachit, A. et al. Utility of Pentraxin-3 as a biomarker for diagnosis of acute appendicitis: a systematic review and meta-analysis. Pediatr. Surg. Int., 38(8). (2022).
Javier, A. M. et al. Discriminatory capacity of serum interleukin-6 between complicated and uncomplicated acute appendicitis in children: a prospective validation study. World J. Pediatr., 18(12). (2022).
Zhenfei, W. et al. Fibrinogen as a marker of overall and complicated acute appendicitis: A systematic review and Meta-Analysis. J. Surg. Res., 280(0). (2022).
Weihua, Z. et al. Hyponatremia as a predictor of complicated appendicitis in children: A systematic review and meta-analysis. Asian J. Surg., 45(10). (2022).
Dale, M. C., et al., Validation of the pediatric appendicitis risk calculator (pARC) in a community emergency department setting. Ann. Emerg. Med., 74(4). (2019).
Madan, S. Pediatric appendicitis score. J. Pediatr. Surg., 37(6). (2002).
Siyuan, B. et al. The value of the Alvarado score for the diagnosis of acute appendicitis in children: A systematic review and Meta-Analysis. J. Pediatr. Surg., 58(10). (2023).
Zenon, P. et al. Prospective validation of Alvarado score and pediatric appendicitis score for the diagnosis of acute appendicitis in children. Pediatr. Emerg. Care, 31(3). (2015).
Javed, A. et al. Appendicitis in children less than 3 years of age: a 28-year review. Pediatr. Surg. Int., 19(12). (2004).
Yu-Tang, C., Jan-You, L. & Yu-Sheng, H. Appendicitis in children younger than 3 years of age: an 18-year experience. Kaohsiung J. Med. Sci., 22(9). (2006).
William, B. et al. Appendicitis in preschool aged children: regression analysis of factors associated with perforation outcome. J. Pediatr. Surg., 50(9). (2015).
Zenon, P. et al. Acute appendicitis in children younger than five years of age: diagnostic challenge for pediatric surgeons. Surg. Infect. (Larchmt), 21(3). (2019).
Samiksha, B. et al. Appendicitis in children less than 5 years old: influence of age on presentation and outcome. Am. J. Surg., 204(6). (2012).
Diya, I., Marc, A. C. & Walter, C. J, Appendiceal fecalith is associated with early perforation in pediatric patients. J. Pediatr. Surg., 43(5). (2008).
Veerle, A. B. v.d.B., et al., Diagnosing perforated appendicitis in pediatric patients: a new model. J. Pediatr. Surg., 51(3). (2015).
Mirelle, E. E. B., et al., Discriminating between simple and perforated appendicitis. J. Surg. Res., 176(1). (2011).
Xuan-Binh, D. P., et al., Factors predictive of complicated appendicitis in children. J. Surg. Res., 206(1). (2016).
Stephanie, K. S., et al., Time to appendectomy and risk of complicated appendicitis and adverse outcomes in children. JAMA Pediatr. 171(8).
Giorgio, S., Vittorina, G. & Piergiorgio, G. Inflammatory markers for acute appendicitis in children: are they helpful? J. Pediatr. Surg., 42(5). (2007).
Marcelo, A. B., et al., Predictive value of white blood cell count and C-reactive protein in children with appendicitis. J. Pediatr. Surg., 42(7). (2007).
Hee Mang, Y. et al. Pediatric appendicitis with appendicolith often presents with prolonged abdominal pain and a high risk of perforation. World J. Pediatr., 14(2). (2018).
Naoko Iwahashi, K. & Hiroshi, K. Retained appendicolith in an inflamed appendix. Emerg. Radiol., 16(2). (2008).
Mitsutomi, I. et al. Significance of size and location of appendicoliths as exacerbating factor of acute appendicitis. Emerg. Radiol., 20(2). (2012).
Thomas, P. C., et al., Benchmarking the value of ultrasound for acute appendicitis in children. J. Pediatr. Surg., 51(12). (2016).
Kiera, R. et al. Diagnostic ultrasound for acute appendicitis: the gold standard. J. Pediatr. Surg., 59(2). (2023).
Andrea, S. D., et al., US or CT for diagnosis of appendicitis in children and adults?? A Meta-Analysis. Radiology, 241(1). (2006).
Kevin, A. E., et al., Acute appendicitis: A Meta-Analysis of the diagnostic accuracy of US, CT, and MRI as Second-Line imaging tests after an initial US. Radiology, 288(3). (2018).
Dani, O. G., et al., Can ultrasound reliably identify complicated appendicitis in children? J. Surg. Res., 229(0). (2018).
Acknowledgements
We extend our gratitude to Wenbin Jiang from Shanghai Children’s Hospital for his contributions to the statistical analysis, manuscript preparation, and submission of this article.
Author information
Authors and Affiliations
Contributions
D.L., Z.Z., and J.W. designed the study. Z.Z., J.W., J.Z., G.W., W.P.,Y.Y, and Y.Z. collected and analyzed the data. F.C. provided guidance on data interpretation. D.L. wrote the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
We declare that there are no conflicts of interest related to this manuscript.
Ethical approval
This study was conducted in accordance with the relevant guidelines and the Declaration of Helsinki. It is a retrospective study of clinical data and it has been approved by the Ethics Review Committee of both Yangzhou Maternal and Child Health Care Hospital Affiliated to Yangzhou University and Shanghai Children’s Hospital (Approval No: 2024024 and 2018R055). Because of the retrospective nature of this study, the informed consent for inclusion was waived by the ethics committee of Yangzhou Maternal and Child Health Care Hospital and Shanghai Children’s Hospital.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, D., Zhang, Z., Wan, J. et al. Clinical features and perforation predictors of appendicitis in infants and toddlers under 3: A retrospective two-center study. Sci Rep 15, 14338 (2025). https://doi.org/10.1038/s41598-025-99293-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-99293-1