Abstract
The Fracture Risk Assessment Tool (FRAX), widely used for predicting the 10-year likelihood of hip fractures, does not incorporate factors like prior falls and sociodemographic characteristics, notably the Social Vulnerability Index (SVI). Recognizing these limitations, we aim to evaluate the predictive accuracy of FRAX by integrating fall frequency, fall energy, and SVI into the model for assessing the risk of fall-induced hip fractures. A retrospective case-control study was conducted, and patients aged ≥ 40 years with a documented diagnosis of a fall-induced hip fracture were age-matched with controls with a history of falls without an associated hip fracture. Basic demographic data, along with information about the number of prior falls and the energy of the current falls, were collected. The FRAX and SVI were calculated accordingly. Logistic regression analysis was employed to identify significant predictors. The performance of the models was evaluated and reported using appropriate metrics. Baseline characteristics of the dataset were presented as medians with interquartile ranges (IQR) or as percentages, where applicable. The significance of the identified variables was quantified using Odds Ratio (OR) along with their 95% Confidence Interval (CI). A p-value threshold of 0.05 was set for statistical significance. A total of 261 patients per group were included with a median age of 74 (IQR 67–80) and 72 (IQR 62–83) years. The FRAX score was significantly associated with the likelihood of experiencing a fall-induced hip fracture, as indicated by an OR of 1.06 (CI: 1.03–1.09). Participants with a one-time history of falls had an OR of 1.58 (CI: 1.02–2.37), compared to 1.84 (CI: 1.09–3.1) for those with multiple falls. The White participants, along with the Housing Type and Transportation domain of the SVI, also demonstrated to play a role (OR = 2.85 (CI: 1.56–5.2) and OR = 0.3 (CI: 0.12–0.8), respectively). This study underscored the significance of factors such as fall frequency, SVI, and race in predicting fall-induced hip fractures. It also highlighted the need for further refinement of the FRAX tool. We recommend that future research should be focused on validating the impact of these sociodemographic and fall characteristics on a broader scale, along with exploring the implications of clinical surrogates related to falls.
Similar content being viewed by others
Introduction
Hip fractures are a debilitating health concern worldwide that is estimated to rise from 1.26 million cases globally in 1990 to 4.5 million cases by 20501,2 An estimated 37.3 million falls occur annually, contributing to over 95% of hip fractures1,3,4 According to the literature, a total of 1.75 million disability-adjusted life years (DALYs) are lost globally, accounting for 0.1% of the worldwide disease burden and 1.4% of the disease burden among women in established market economies5 Therefore, predicting and implementing early intervention strategies is of crucial value to decrease the burden of hip fractures associated with falls.
To accomplish this goal, the Fracture Risk Assessment Tool (FRAX) generated by the World Health Organization (WHO) has been developed to predict the 10-year probability of an adult having a hip fracture6 FRAX utilizes the most important risk factors known for major osteoporotic fractures, including age, sex, weight, height, alcohol use, glucocorticoid use, femoral neck bone mineral density (BMD), history of previous fracture in the patients and their parents, smoking status, and rheumatoid arthritis7 With 6 million yearly calculations done in 173 countries, FRAX has been immensely helpful in predicting fracture risks. However, it is frequently criticized for lacking a detailed and standardized description of each risk factor, including the recency of fracture and glucocorticoid dose8 Furthermore, since falls are one of the most critical factors leading to hip fractures in older adults, a common criticism of FRAX is that it does not factor in fall history8,9.
Since the official launch of FRAX in 2008, concerns have arisen regarding its inability to consider the impact of falls10,11 In 2010, the Task Force acknowledged this concern, stating that “Fracture probability may be underestimated in individuals with a history of frequent falls, but quantification of this risk is not currently possible.” The primary reason for this challenge was the lack of sufficient evidence available at that time. Since then, the body of literature on this topic has expanded, with controversial results suggesting a complex relationship between FRAX and falls and highlighting the need for a more careful approach when integrating the two12,13,14 Furthermore, while much of the research focuses on this aspect, other fall characteristics seem not well investigated. Among these, the mechanics of the falls seem to play a significant role in the risk of hip fractures15 Hayes et al. pointed out that the energy or impact of the fall is found to be a crucial factor when assessing the risk factors for hip fractures16 This suggests that not just the frequency of falls but also their nature and severity might be essential factors in assessing fall-induced hip fracture risk.
Given the multifactorial nature of hip fractures, efforts have been made to point out the relevant demographic and other non-medical risk factors in hip fractures17,18,19,20 Some factors, including age and sex, are already addressed in the FRAX, while others, like race, ethnicity, and socioeconomic factors, are not. The Social Vulnerability Index (SVI), developed by the Centers for Disease Control and Prevention (CDC), is intended to measure the vulnerability of communities to environmental hazards, disease outbreaks, and other public health emergencies21 It encompasses various subscales, including Socioeconomic Status, Household Characteristics, Racial and Ethnic Minority Status, Housing Type and Transportation. When used in medicine, it enables capturing the pre-existing social inadequacies that make individuals or communities disproportionately vulnerable to a particular medical condition or disease22 By understanding these correlations, healthcare providers and policymakers can develop more targeted interventions and resource allocations to reduce the risk of fall-induced injuries in the most vulnerable populations.
In this study, we hypothesized that fall frequency and energy, along with the SVI, are of predictive value in fall-induced hip fractures. Moreover, in order to have a more comprehensive and accurate assessment of hip fracture risk, we aim to develop a modified version of the FRAX that incorporates additional variables found to be significant risk factors for fall-induced hip fractures in our study.
Results
A total of 261 patients per group were included, and their demographic data are depicted in Table 1. Race, BMI, FRAX, Racial and Ethnic Minority Status, Housing type and Transportation showed significant differences between the hip fracture and no fracture groups.
The outcome of the logistic regression test on various factors that showed significant differences between the fracture and no-fracture groups, as well as fall characteristics, including energy and number of falls, are shown in Table 2. White participants also showed a higher rate of fall-induced fracture (OR = 2.85; CI:1.56–5.20), although there was an imbalance in sample composition, with White participants making up 86% of the sample and participants from other racial backgrounds comprising 13%. Housing Type and Transportation were shown to decrease the chance of experiencing the injury significantly (OR = 0.30, CI:0.12–0.80).
The FRAX tool and the prediction model developed in this study (modified FRAX) were evaluated using the data of the cases and the control group. The performances of the FRAX tool, as well as the modified FRAX, are shown in Table 3. Moreover, the relevant AUCs for each model are illustrated in Figs. 1 and 2. The final prediction model was developed using the coefficients of the best model and deployed on the following web address https://fixus.mgh.harvard.edu/fall/.
Discussions
Almost half of the elderly population experience a fall, and up to 10% have reported a skeletal injury3 A strong association between the propensity to fall and future fracture is mentioned in various studies. These studies showed a greater risk in individuals with a history of multiple falls23,24 However, the history and frequency of falls have not been included in current prediction models such as the FRAX tool. Falls and hip fractures share many similar risk factors, including increasing age, smoking, alcohol consumption, and frailty; thus, hypothesizing that FRAX and any other prediction model that could predict fractures could also be modified to predict the risk of fall-induced fractures would be reasonable12,25 Including patient-specific characteristics such as race, country of origin, medications, and medical conditions affecting bone quality were considered in several studies to improve the accuracy, validity, and reliability of the FRAX tool12 In this study, we investigated the added predictive value of fall characteristics, basic demographics, SVI, and its domains to the FRAX score for the prediction of fall-induced hip fractures. Our results showed that the number of falls, race, Housing type and Transportation subscale of the SVI play a considerable role in predicting the risk of fall-induced hip fractures.
In the nuanced realm of assessing fracture risk, the relationship between fall frequency and the FRAX score emerges as a complex and evolving topic12 In 2015, Harvey et al. conducted a study in a 1,836 male population comparing the predictive value of FRAX and fall frequency for future falls24 They suggested a twist by concluding that the FRAX score is capable of predicting future falls (Hazard Ratio = 1.64; CI:1.36–1.97). This finding implied that since falls and fractures share a lot of risk factors, FRAX has an inherent mention of falls. However, this perspective was challenged by subsequent research from the same team in a large-scale study with 7,857 male patients14 Here, they discovered that a patient’s fall frequency indeed has its independent predictive value for future osteoporotic fractures, regardless of their FRAX score. This key insight brought to light the value of including fall history in assessing fracture risk, suggesting that the FRAX score’s effectiveness could be enhanced by integrating this factor.
Our study builds upon this existing body of knowledge, indicating the improved performance of the FRAX score when prior falls are included in the model. While Harvey et al. focused explicitly on male participants, in the present study, we did not observe any changes when the model was adjusted for sex26 In a study by Kanis et al. involving 21,116 male and female participants, a progressive increase in Hazard Ratios was observed with the rising number of falls27 When these ratios were adjusted for age, sex, and FRAX variables, a slight decrease was noted. However, the present study focused specifically on patients with hip fractures caused by falls, providing distinct insights relevant to that population. Moreover, in our study, mainly involving elderly participants, we did not find the energy of falls to be a significant predictor within the FRAX model28,29 Notably, we observed a low incidence of high-energy falls among both the cases and controls, aligning with existing literature that low-energy falls are more common in older adults30,31 Including fall energy in the FRAX model may not significantly affect fracture risk assessment in older adults, but its impact on younger populations warrants further investigation across various age groups.
In predicting fall-induced hip fractures, the significance of incorporating patient sociodemographic characteristics is increasingly recognized. Previous studies have underscored the impact of factors such as race, geographic location, age, economic conditions, and housing on the incidence and management of hip fractures. For instance, disparities in hip fracture rates and outcomes have been observed across different racial and ethnic groups,32 while geographic variations highlight the influence of environmental and healthcare access differences33 This understanding has led to the adaptation of the FRAX in various countries, with each version tailored to reflect the specific characteristics and needs of the local population. Our findings showed that being White was associated with a notably higher risk of fall-induced injuries. This aligns with findings by Ellis et al., who reported that White individuals experienced approximately double the rate of fall-induced hip fractures compared to Black or Hispanic individuals and triple the rate observed in Asian or Pacific Islander individuals34 It is imperative, however, to reflect on the demographic makeup of our study cohort, predominantly composed of White participants, which underscores the need for caution in extrapolating our findings to broader populations35,36,37.
Whether the broader sociodemographic factors captured by the SVI are of added value in fall-induced injuries is a topic that is not directly addressed in the literature. In this study, we found a significant inverse role for the SVI’s Housing Type and Transportation domain, meaning the less vulnerable individuals had a higher chance of sustaining a fall-induced hip fracture. This counterintuitive result warrants a deeper investigation into the dynamics of the Housing Type and Transportation domain, which includes the number of units in a building, the presence of mobile homes, the number of occupants per room, the presence of a vehicle in a household, and group living arrangements38 One possible explanation could be that a higher number of occupants, typically associated with a higher vulnerability score, might paradoxically confer a protective effect against falls through heightened physical engagement39 Bernhart et al. showed that older adults residing in households with two or more individuals were twice as likely to adhere to aerobic guidelines for physical activity compared to those living in single-adult households40 Similarly, Meghani et al. concluded that residing with family plays a crucial role in assisting older adults to stay active and manage their personal responsibilities effectively41 While other socioeconomic factors seem to have a remarkable effect on hip fractures and falls separately, in this study, we did not find a role for other domains of the SVI in fall-induced hip fractures. In contrast, using the Housing-based Index of Socioeconomic Status (HOUSES), Ryu et al. concluded that a higher socioeconomic status reduces the likelihood of falls42 It is important to note, however, that their study included individuals across all age groups. Similarly, a study conducted in the UK highlighted the impact of material deprivation on the incidence of hip fractures among young adults, with a relative risk (RR = 1.64; CI:1.57–1.72) in poorer electoral wards43 However, they reported no association in individuals aged 85 and over (RR = 0.94, CI:0.87–1.01), suggesting the decreased effect of socioeconomic factors on the elderly, which is consistent with the outcomes of our study.
Our findings indicate that the modified FRAX model yielded modest improvements in predictive performance over the conventional FRAX tool, specifically within a population characterized by frequent falls. Although the incremental gain was limited, this outcome highlights an important limitation in the traditional FRAX’s ability to fully capture fracture risk associated with recurrent falls and socioeconomic factors. These results underscore the need for continued refinement of existing risk assessment models, advocating for future studies that incorporate additional clinical, demographic, and socioeconomic predictors to enhance fracture prediction accuracy in diverse patient cohorts. However, the study has a few limitations to be considered. First, although previous studies have shown different results with specific elderly age groups, in this study, because of a relatively small sample size, we could not conduct a group-wise analysis by age. Second, the energy of falls was measured based on a height criterion, and since oftentimes the height was not explicitly mentioned in clinicians’ notes, we relied on the interpretation of the clinical notes made by expert observers. However, if the expert observers were not confident about the interpretation of the fall energy, we would not include that factor for the patient in assessing our prediction models. Additionally, this study did not undergo external validation due to constraints such as limited data availability and resources, and we acknowledge that external validation is essential for assessing the generalizability of our findings.
Conclusion
This study highlights the importance of considering patients’ history, frequency of prior falls, and SVI in assessing the risk of fall-induced hip fractures. Furthermore, our findings demonstrate notable limitations in the conventional FRAX model’s ability to accurately predict fracture risk among patients prone to falls, emphasizing the necessity for refinement. Future research should prioritize age-specific analyses, integrate social determinants and socioeconomic indicators like the SVI and Area Deprivation Index, and account for detailed fall characteristics.
Materials and methods
Study design and population
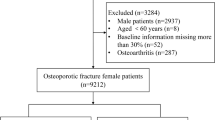
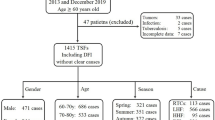
We conducted a retrospective case-control study through a tertiary institution located in Boston, Massachusetts. The study protocol was approved by the institutional review board (IRB) of the Mass General Brigham. Given the study’s retrospective design, informed consent was waived by the IRB (Mass General Brigham IRB # 2023P000741, May 3rd, 2023). Data were queried from the institution’s data repository, the Research Patient Data Registry (RPDR), for the period 2010 to 2023. Relevant ICD-9, ICD-10, and CPT codes, along with string searches for clinician notes, were used for the data query. The initial results were screened, and participants aged ≥ 40 years with a confirmed diagnosis of fall-induced hip fracture were included as cases, and those who experienced falls without a resultant hip injury as controls. A total of 2,132 patients with a history of falls who were assessed for hip fractures were screened. Cases (patients with hip fracture) and controls (without hip fracture) were age-matched for the final analysis. The study excluded individuals who had a repair, revision, or reconstruction surgery due to a previous hip fracture, who did not have a mention of the mechanism of falls on their charts, or who experienced falls resulting from violent encounters and animal attacks, significant external forces such as car or motor vehicle accidents, high-impact sports like skiing, and those with fractures caused by underlying pathological conditions to avoid the influence of confounding injuries44 We also excluded patients who did not have enough information on their charts for the calculation of the FRAX score or for the assessment of their falling injury. The study methods adhered to the principles of the Declaration of Helsinki.
Outcomes and variables
Baseline information of the participants including age, gender, height, weight, body mass index (BMI), race, previous fracture, parent with a fractured hip, smoking status, glucocorticoid use, history of rheumatoid arthritis, secondary osteoporosis, and alcohol consumption. Because most participants were White, racial identity was categorized into two groups: White participants and participants from other racial groups (including American Indian or Alaska Native, Asian, Black or African American, and Native Hawaiian or Other Pacific Islander). The smoking status was determined at the time of the falling incidence. Glucocorticoids had to be used before or at the time of the fall45 To qualify for osteoporosis secondary to a medical condition, the patient had to have one of the following diseases: Type 1 and 2 diabetes, chronic liver disease, inflammatory bowel disease, hypogonadism, celiac disease, premature menopause, cystic fibrosis, renal disease, chronic pancreatitis, sickle cell disease, or hyperthyroidism, clinical visit dates, and notes were collected through the initial query. A thorough search of patients’ electronic health records was done to collect information about the number of previous falls that occurred any time before the most recent incident. This included searching for a mention of a fall on all the documented notes, imaging reports, and encounter reasons. The energy of falls was extracted from clinicians’ notes. Low-energy falls were defined as falling from < 1 m and high-energy as > 1 m46 Because most of the time, the falling incidence was described without an explicit mention of the height, it needed to be inferred from the notes by an expert reviewer. As a result, two orthopaedic clinical researchers labeled the patients due to the extracted description of the fall; in case of a disagreement, the opinion of a third experienced observer would help in making the final decision. FRAX scores were calculated using the online calculation tool (Fracture Risk Assessment Tool)45 The overall SVI and its subcategories, including Socioeconomic Status, Household Characteristics, Racial and Ethnic Minority Status, and Housing Type and Transportation were estimated using the participant’s zip code and CDC’s ATSDR calculation tool (Agency for Toxic Substances and Disease Registry).
Statistical analysis
Data were analyzed utilizing Statistical Package for the Social Sciences (SPSS Version 28.0, 2021). Descriptive statistics were used to summarize the baseline characteristics of the participants in both groups. The normality of the continuous data was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests. T-test, or Mann-Whitney U test, was used to compare normally and non-normally distributed data, respectively. Data were shown as median (Interquartile range; IQR), odds ratio (OR), 95% confidence interval (CI), and percentage (%). A p-value of 0.05 was considered as significant. A binary logistic regression was performed with a stepwise approach to decide on the most relevant predictors based on the level of significance. The performance of the FRAX score, as well as our prediction models, were assessed according to their performance metrics, including the Area Under the Receiver Operating Characteristics Curve (AUC), sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and Youden’s J. The variables from the model with the best performance were chosen to develop the prediction formula. The following formula was used:
Where “P” is the predicted probability of the outcome; “e” is the base of the natural logarithm (approximately equal to 2.71828); “β0" is the intercept; “β1,β2,…” are the coefficients for the predictor variables; “x1,x2,…” are the predictor variables.
Data availability
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
References
Veronese, N. & Maggi, S. Epidemiology and social costs of hip fracture. Injury 49 (8), 1458–1460. https://doi.org/10.1016/j.injury.2018.04.015 (2018).
Gullberg, B., Johnell, O. & Kanis, J. A. World-wide projections for hip fracture. Osteoporos. Int. 7 (5), 407–413. https://doi.org/10.1007/PL00004148 (1997).
Masud, T., Binkley, N., Boonen, S. & Hannan, M. T. Official positions for FRAX® clinical regarding falls and frailty: can falls and frailty be used in FRAX®? From joint official positions development conference of the international society for clinical densitometry and international osteoporosis foundation on FRAX®. J. Clin. Densitometry. 14 (3), 194–204 (2011).
Dytfeld, J. & Michalak, M. Type 2 diabetes and risk of low-energy fractures in postmenopausal women: meta-analysis of observational studies. Aging Clin. Exp. Res. 29 (2), 301–309. https://doi.org/10.1007/s40520-016-0562-1 (2017).
Johnell, O. & Kanis, J. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos. Int. 15, 897–902 (2004).
Kanis, J. A. Assessment of Osteoporosis at the Primary Health-Care Level. Technical Report, World Health Organization Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield (2007).
Kanis, J. A., Johansson, H., Harvey, N. C. & McCloskey, E. V. A brief history of FRAX. Arch. Osteoporos. 13 (1), 118. https://doi.org/10.1007/s11657-018-0510-0 (2018).
El Miedany, Y. FRAX: re-adjust or re-think. Arch. Osteoporos. 15 (1), 150. https://doi.org/10.1007/s11657-020-00827-z (2020).
Task Force of the FRAX Initiative et al. Interpretation and use of FRAX in clinical practice. Osteoporos. Int. 22 (9), 2395–2411. https://doi.org/10.1007/s00198-011-1713-z (2011).
Schwartz, A. V., Nevitt, M. C., Brown, B. W. Jr & Kelsey, J. L. Increased falling as a risk factor for fracture among older women: the study of osteoporotic fractures. Am. J. Epidemiol. 161 (2), 180–185. https://doi.org/10.1093/aje/kwi023 (2005).
Geusens, P., van Geel, T. & van den Bergh, J. Can hip fracture prediction in women be estimated beyond bone mineral density measurement alone? Ther. Adv. Musculoskelet. Dis. 2 (2), 63–77. https://doi.org/10.1177/1759720X09359541 (2010).
McCloskey, E. V., Harvey, N. C., Johansson, H. & Kanis, J. A. FRAX updates 2016. Curr. Opin. Rheumatol. 28 (4), 433–441 (2016).
Harvey, N. C. et al. Predictive value of DXA appendicular lean mass for incident fractures, falls, and mortality, independent of prior falls, FRAX, and BMD: findings from the women’s health initiative (WHI). J. Bone Miner. Res. 36 (4), 654–661. https://doi.org/10.1002/jbmr.4239 (2021).
Harvey, N. C. et al. Falls predict fractures independently of FRAX probability: A Meta-Analysis of the osteoporotic fractures in men (MrOS) study. J. Bone Miner. Res. 33 (3), 510–516. https://doi.org/10.1002/jbmr.3331 (2018).
Cummings, S. R., Nevitt, M. C. & the Study of Osteoporotic Fractures Research Group. Non-skeletal determinants of fractures: the potential importance of the mechanics of falls. Osteoporos. Int. 4 (S1), S67–S70. https://doi.org/10.1007/BF01623439 (1994).
Hayes, W. C. et al. Impact near the hip dominates fracture risk in elderly nursing home residents who fall. Calcif Tissue Int. 52 (3), 192–198. https://doi.org/10.1007/BF00298717 (1993).
Schloemann, D. T., Ricciardi, B. F. & Thirukumaran, C. P. Disparities in the epidemiology and management of fragility hip fractures. Curr. Osteoporos. Rep. 21 (5), 567–577. https://doi.org/10.1007/s11914-023-00806-6 (2023).
Petit, M. P., Bryère, J., Maravic, M., Pallaro, F. & Marcelli, C. Hip fracture incidence and social deprivation: results from a French ecological study. Osteoporos. Int. 28 (7), 2045–2051. https://doi.org/10.1007/s00198-017-3998-z (2017).
Sterling, R. S. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin. Orthop. Relat. Res. 469 (7), 1913–1918. https://doi.org/10.1007/s11999-010-1736-3 (2011).
Sullivan, K. J., Husak, L. E., Altebarmakian, M. & Brox, W. T. Demographic factors in hip fracture incidence and mortality rates in California, 2000–2011. J. Orthop. Surg. Res. 11, 4. https://doi.org/10.1186/s13018-015-0332-3 (2016).
Flanagan, B. E., Hallisey, E. J., Adams, E. & Lavery, A. Measuring community vulnerability to natural and anthropogenic hazards: the centers for disease control and prevention’s social vulnerability index. J. Environ. Health. 80 (10), 34–36 (2018).
Mah, J. C., Penwarden, J. L., Pott, H., Theou, O. & Andrew, M. K. Social vulnerability indices: a scoping review. BMC Public. Health. 23 (1), 1253. https://doi.org/10.1186/s12889-023-16097-6 (2023).
Dargent-Molina, P. et al. Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet 348 (9021), 145–149. https://doi.org/10.1016/s0140-6736(96)01440-7 (1996).
Harvey, N. C. et al. FRAX predicts incident falls in elderly men: findings from MrOs Sweden. Osteoporos. Int. 27 (1), 267–274. https://doi.org/10.1007/s00198-015-3295-7 (2016).
Johansson, H., Kanis, J. A., Oden, A., Johnell, O. & McCloskey, E. BMD, clinical risk factors and their combination for hip fracture prevention. Osteoporos. Int. 20 (10), 1675–1682. https://doi.org/10.1007/s00198-009-0845-x (2009).
Edwards, M. H. et al. Clinical risk factors, bone density and fall history in the prediction of incident fracture among men and women. Bone 52 (2), 541–547. https://doi.org/10.1016/j.bone.2012.11.006 (2013).
Kanis, J. A. et al. Adjusting conventional FRAX estimates of fracture probability according to the number of prior falls in the preceding year. Osteoporos. Int. 34 (3), 479–487. https://doi.org/10.1007/s00198-022-06633-2 (2023).
Luukinen, H. et al. Fracture risk associated with a fall according to type of fall among the elderly. Osteoporos. Int. 11 (7), 631–634. https://doi.org/10.1007/s001980070086 (2000).
Hwang, H. F., Lee, H. D., Huang, H. H., Chen, C. Y. & Lin, M. R. Fall mechanisms, bone strength, and hip fractures in elderly men and women in Taiwan. Osteoporos. Int. 22 (8), 2385–2393. https://doi.org/10.1007/s00198-010-1446-4 (2011).
Ambrose, A. F., Cruz, L. & Paul, G. Falls and fractures: A systematic approach to screening and prevention. Maturitas 82 (1), 85–93. https://doi.org/10.1016/j.maturitas.2015.06.035 (2015).
Rinne, P. P., Laitinen, M. K., Huttunen, T., Kannus, P. & Mattila, V. M. The incidence and trauma mechanisms of acetabular fractures: A nationwide study in Finland between 1997 and 2014. Injury 48 (10), 2157–2161. https://doi.org/10.1016/j.injury.2017.08.003 (2017).
Cauley, J. A. Defining ethnic and Racial differences in osteoporosis and fragility fractures. Clin. Orthop. Relat. Res. 469 (7), 1891–1899. https://doi.org/10.1007/s11999-011-1863-5 (2011).
Cheng, S. Y. et al. Geographic trends in incidence of hip fractures: a comprehensive literature review. Osteoporos. Int. 22 (10), 2575–2586. https://doi.org/10.1007/s00198-011-1596-z (2011).
Ellis, A. A. & Trent, R. B. Hospitalized fall injuries and race in California. Inj. Prev. 7 (4), 316–320. https://doi.org/10.1136/ip.7.4.316 (2001).
Kanis, J. A., Johansson, H., Oden, A. & McCloskey, E. V. Guidance for the adjustment of FRAX according to the dose of glucocorticoids. Osteoporos. Int. 22 (3), 809–816. https://doi.org/10.1007/s00198-010-1524-7 (2011).
Kanis, J. A. et al. Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporos. Int. 31 (1), 1–12. https://doi.org/10.1007/s00198-019-05176-3 (2020).
Leslie, W. D. & Morin, S. N. New developments in fracture risk assessment for current osteoporosis reports. Curr. Osteoporos. Rep. 18 (3), 115–129. https://doi.org/10.1007/s11914-020-00590-7 (2020).
CDC SVI Documentation 2018 | Place and Health | ATSDR. Accessed November 8. https://www.atsdr.cdc.gov/placeandhealth/svi/documentation/SVI_documentation_2018.html (2023).
Lee, J. The association between physical activity and risk of falling in older adults: A systematic review and meta-analysis of prospective cohort studies. Geriatr. Nurs. 41 (6), 747–753. https://doi.org/10.1016/j.gerinurse.2020.05.005 (2020).
Bernhart, J. A. et al. Leveraging household structure for increasing adult physical activity in a Low-Income, African American community. Health Promot Pract. 21 (4), 582–590. https://doi.org/10.1177/1524839918814731 (2020).
Meghani, N. A. A., Hudson, J., Stratton, G. & Mullins, J. Older adults’ perspectives on physical activity and sedentary behaviour within their home using socio-ecological model. PLOS ONE. 18 (11), e0294715. https://doi.org/10.1371/journal.pone.0294715 (2023).
Ryu, E. et al. Individual housing-based socioeconomic status predicts risk of accidental falls among adults. Ann. Epidemiol. 27 (7), 415–420e2. https://doi.org/10.1016/j.annepidem.2017.05.019 (2017).
Jones, S., Johansen, A., Brennan, J., Butler, J. & Lyons, R. A. The effect of socioeconomic deprivation on fracture incidence in the united Kingdom. Osteoporos. Int. 15 (7), 520–524. https://doi.org/10.1007/s00198-003-1564-3 (2004).
Ekbrand, H., Ekman, R., Thodelius, C. & Möller, M. Fall-related injuries for three ages groups - Analysis of Swedish registry data 1999–2013. J. Saf. Res. 73, 143–152. https://doi.org/10.1016/j.jsr.2020.02.016 (2020).
Kanis, J. A. et al. FRAX® and its applications to clinical practice. Bone 44 (5), 734–743 (2009).
Bergström, U., Björnstig, U., Stenlund, H., Jonsson, H. & Svensson, O. Fracture mechanisms and fracture pattern in men and women aged 50 years and older: a study of a 12-year population-based injury register, Umeå, Sweden. Osteoporos. Int. 19 (9), 1267–1273. https://doi.org/10.1007/s00198-007-0549-z (2008).
Acknowledgements
The authors would like to acknowledge the patients and healthcare professionals whose data and experiences form the backbone of this study, contributing significantly to our understanding of fall-induced injuries.
Author information
Authors and Affiliations
Contributions
Conceptualization or Design: S.A.E., A.T. – Developed the study’s overall research strategy and goals. Data Acquisition, Analysis, or Interpretation: A.T., E.S., G.C., S.H., S.A.E., M.B.H., S.A.L., J.N.D. – Collected the data, conducted the analysis, and interpreted the research results. Manuscript Drafting or Revision: A.T., E.S., G.C., S.A.E., M.B.H., S.A.L., J.N.D. – Contributed to writing the initial draft of the manuscript and participated in revising it critically for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Taseh, A., Sirls, E., Casey, G. et al. Social vulnerability index enhances FRAX prediction of hip fractures in fall patients. Sci Rep 15, 14704 (2025). https://doi.org/10.1038/s41598-025-99373-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-99373-2