Abstract
To analyze the global burden of pancreatitis in women of childbearing age (WCBA) at the global, regional and national levels from 1990 to 2021. Data for pancreatitis incidence and deaths in females aged 15 to 49 years were downloaded from the Global Burden of Disease 2021 database. Estimated annual percentage changes (EAPCs) were calculated to describe the temporal trends. In 2021, the global numbers of incident cases and deaths of pancreatitis in the WCBA were 505,012 (409,536 to 627,684) and 7,002 (5,647 to 8,857), respectively. From 1990 to 2021, the global incidence and death rates of pancreatitis in the WCBA showed downward trends, with EAPCs of -0.15 (-0.21 to -0.09) and − 0.42 (-0.58 to -0.26), respectively. The most significant decreases in incidence and death rates were observed among females aged 40 to 44 years. Eastern Europe had the highest incidence and death rates in 2021. Countries with high socio-demographic index (SDI) showed the highest incidence rate, while showed greatest decrease in incidence during the past 32 years. The global pancreatitis incidence and death in WCBA has decreased since 1990, but the incidence is still high in countries with high-SDI. More efficient public health measures are needed to reduce the burden of pancreatitis.
Similar content being viewed by others
Introduction
Pancreatitis is an inflammatory disorder of the pancreas, and the incidence of pancreatitis continues to increase worldwide1. Acute pancreatitis can progress to severe acute pancreatitis, with a higher mortality rate, and may also lead to chronic pancreatitis. Currently, pancreatitis is a serious health problem in East Asia, the United States and European countries2,3,4,5. With increasing risk factors such as cholelithiasis, hyperlipidemia, and alcohol consumption, the prevalence of pancreatitis may continue to increase. Women are prone to cholelithiasis, and hormonal changes in women during pregnancy cause an increase in cholesterol, which can easily lead to the formation of gallstones. It is estimated that 12% of women will experience cholelithiasis during pregnancy, and up to 70% of reported pancreatitis cases are attributed to gallstone disease6. Moreover, hypertriglyceridemia is a known etiology of pancreatitis. During the third trimester of pregnancy, triglyceride levels can increase two to fourfold7.
The aim of Sustainable Development Goal 3.1 is to reduce the global maternal mortality ratio to less than 70 per 100,000 live births by 20308. Therefore, it is highly significant to fully assess the epidemiology of pancreatitis in women of childbearing age (WCBA). However, studies on the epidemiology of pancreatitis in WCBA have been conducted only in limited regions or countries. Assessing the incidence and mortality of pancreatitis and analyzing its change trends in WCBA will help to better understand the epidemiology of pancreatitis and promote women’s health. The Global Buden of Disease (GBD) Study provides useful data for epidemiological research9. In this study, we conducted a systematic analysis based on GBD 2021 to assess the global, regional and national temporal trends in the incidence and death of pancreatitis in the WCBA from 1990 to 2021.
Results
Overview of pancreatitis incidence and mortality in WCBA
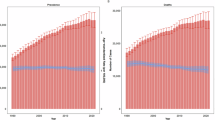
Globally, the incident cases of pancreatitis among women aged 15 to 49 years increased by 43.8% (95% UI: 39% to 49%) between 1990 and 2021, from 351,302 (276,609 to 448,102) to 505,012 (409,536 to 627,684) (Fig. 1). The incidence rate of pancreatitis among this age group decreased by 1.4%, from 26.3 per 100,000 people in 1990 to 25.9 per 100,000 people in 2021, with an EAPC of -0.15 (-0.21 to -0.09) (Table 1). In 2021, the number of deaths in WCBA was 7,002 (5,647 to 8,857), a 31.9% (8.9% to 58%) increase from 1990. The global death rate of pancreatitis in WCBA decreased by 9.5%, from 0.39 per 100,000 in 1990 to 0.36 per 100,000 in 2021, with an EAPC of -0.42 (-0.58 to -0.26).
Incidence and mortality by age subgroup
Globally, from 1990 to 2021, the incident cases of pancreatitis at least increased by 29% in every age subgroup in WCBA (15 to 19 years: from 30,751 to 41,803; 20 to 24 years: from 39,289 to 52,168; 25 to 29: years: from 49,080 to 63,403; 30 to 34 years: from 56,708 to 79,555; 35 to 39 years: from 62,476 to 86,773; 40 to 44 years: 58,045 to 86,536) and even increased nearly 70% for females aged 45 to 49 years (from 54,952 to 94,774). The different age groups exhibited different pancreatitis change pattern from 1990 to 2021 (Figure S1). Pancreatitis incidence rate across 25 to 49 years decreased at a noticeable rate during 1990 to 2021, especially among those aged 40 to 44 years (EAPC=-0.78, -0.89 to -0.67). Females aged 15 to 24 years showed upward trends, with a greater increase in people aged 15 to 19 years (EAPC = 0.45, 0.42 to 0.48). The death rate of pancreatitis decreased across all age subgroups in WCBA worldwide, especially among females aged 40 to 44 years (EAPC= -1.08, -1.22 to -0.93).
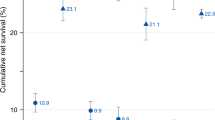
In 2021, the global incidence and death rates for pancreatitis per 100,000 in WCBA increased with age, with the highest incidence (40.2, 27.7 to 55.6) and death (0.92, 0.68 to 1.2) rates in 45 to 49 years age group (Fig. 2). Moreover, people over 35 years old accounted for more than 50% of the incident cases and deaths (Figure S2).
Regional and National trends
From 1990 to 2021, four of the 21 GBD regions showed decreasing trends in incident cases, and five of the 21 regions showed decreasing trends in the number of deaths of pancreatitis in WCBA (Figure S3). The largest increases in incidence and death rates of pancreatitis in WCBA were in South Asia and Eastern Europe, respectively, with EAPCs of 0.6 (0.52 to 0.68) and 2.12 (1.49 to 2.76), respectively. The greatest reductions in incidence and death rate of pancreatitis in WCBA were observed in high-income North America and high-income Asia Pacific, with EAPCs of -0.98 (-1.15 to -0.81) and -2.23 (-2.38 to -2.07), respectively (Table 2).
In 2021, among 21 GBD regions, the highest incidence rates of pancreatitis in WCBA were in Eastern Europe (86.4), high-income North America (50.4) and Southern Latin America (46.6). The highest regional incidence rate (86.4 in Eastern Europe) was 7.4 times higher than the lowest (11.6 in Tropical Latin America). Eastern Europe (2.4) also had the highest death rate from pancreatitis in WCBA in 2021.
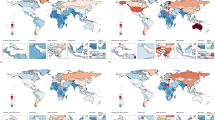
At the national level, Chile had the highest increase in the incidence of pancreatitis in WCBA from 1990 to 2021, with an EAPC of 1.4 (1.16 to 1.65), followed by Singapore (EAPC = 1.13, 1.01 to 1.24) and Mexico (EAPC = 1.1, 1 to 1.21) (Table S1). In the same period, Singapore showed the most substantial decrease in the death rate of pancreatitis in the WCBA, with an EAPC of -4.37 (-4.7 to -4.03). In 2021, four countries, including India, China, the United States and Russia, reported more than 30,000 incident cases of pancreatitis in WCBA. Fifty-eight countries/territories had at least the global average incidence rate in 2021, of which the highest incidence rates were observed in Russian Federation, Ukraine and Republic of Moldova. The highest death rates were also observed in these three countries (Fig. 3).
Incidence and death trends by sociodemographic index
From 1990 to 2021, the number of incident cases and deaths showed a basically unchanged or slightly decreasing trend in the high-SDI quintile, whereas the number of incident cases has more than doubled and the number of deaths increased by more than 60% in low-middle- and low-SDI quintiles. Incidence rates in the high- and high-middle-SDI quintiles showed downward trends, with EAPCs of -0.64 (-0.76 to -0.52) and -0.22 (-0.3 to -0.15), respectively. Except for the high-middle-SDI quintile, other four SDI quintiles showed downward trends in the death rate (Fig. 1).
Countries with different SDI quintiles showed different epidemiological patterns. Among the five SDI quintiles, the incidence rates ranged from 20.5 (15.7 to 26.4) to 33.1 (29.3 to 38.2) in 2021, with countries in the high-SDI quintile having the highest incidence rate and countries in the low-SDI quintile having the lowest. The death rates ranged from 0.23 (0.22 to 0.25) in the high-SDI quintile to 0.56 (0.5 to 0.62) in the high-middle SDI quintile.
To understand the burden of pancreatitis in WCBA in relation to countries’ sociodemographic status, we examined the relationships between the incidence and death rates (in 2021) and the SDI (in 2021) (Fig. 4). The results revealed a positive correlation, in that countries with high SDI had relatively high incidence rate, whereas countries with low SDI had much lower incidence rate. The correlation curve of the death rate and SDI showed a smooth straight line. We found that some high-income countries, Estonia, Canada and Latvia, are well located in above the fitted curve, while some high-SDI countries are located below the fitted curve, including Singapore and Netherlands. The relationships between incidence and death rates (from 1990 to 2021) and the SDI (in 2021) across 21 GBD regions are shown in Figure S4.
Discussion
In this study, we explored the trends in the global incidence and death of pancreatitis in the WCBA from 1990 to 2021. The global incidence and death rates of pancreatitis in WCBA showed downward trends, but they still remain high in high- and high-middle-SDI regions. In consideration of the impact of pancreatitis on WCBA, more attention should be given to the burden of pancreatitis in this group in the future.
Globally, the pancreatitis is still a serious medical problem. Pregnancy is important for adult women, and severe pregnancy complications caused by gestational pancreatitis affect the quality of life and survival of mothers and children. Compared with general pregnant women, women with pancreatitis need to consider many clinical factors, including the effects of drug use on the fetus, the timing of surgical intervention, and the prevention of complications of severe pancreatitis. The occurrence of acute pancreatitis in women may be related to gallstones and cholestasis. Significantly elevated levels of estrogen and progesterone during pregnancy increase cholesterol levels and promote cholestasis10. Hypertriglyceridemia is another well-known etiology of acute pancreatitis. In the third trimester of pregnancy, the levels of triglyceride are approximately 2 to 4 times greater than normal value10. The global age-standardized mean body-mass index increased from 22.1 kg/m2 in 1975 to 24.4 kg/m2 in 2014 in women, and nearly 5.0% of the world’s women were severely obese11. By 2050, more than 1.31 billion people are projected to have diabetes12. Given the increases in the prevalence of diabetes, metabolic syndrome, and obesity, we should pay attention to hypertriglyceridemia-induced pancreatitis in females.
Pancreatitis has recently been observed much more frequently incidentally during pregnancy. In a 10-year retrospective study, acute pancreatitis occurred during pregnancy in 33.0 per 100,000 people13. Hospitalization data for women showed that the prevalence of acute pancreatitis was 20.02 per 100,000 people during pregnancy14. Acute pancreatitis also threatens the lives of women and newborns. The maternal and fetal mortality rates are as high as 3.3% and 11.6%, respectively, for acute pancreatitis during pregnancy15. Research has indicated that lactate dehydrogenase, triglyceride, cholesterol, and albumin levels are independent predictors of severe acute pancreatitis during pregnancy16. As the increased risks of maternal and fetal death are significantly correlated with the severity of acute pancreatitis during pregnancy, more prevention measures and effective methods to predict prognosis are necessary in the future.
The higher incidence rate in the high-SDI quintile may be attributed to the use of advanced and complete diagnostic tools. The development of computed tomography and magnetic resonance imaging has improved the detection rate of pancreatitis17,18. At the regional level, Europe had high incidence rates for pancreatitis in WCBA. The incidence of acute pancreatitis continues to increase in most parts of Europe19. It was reported that the incidence ranged from 5.6 per 100,000 people in Albania, to 100.0 per 100,000 in the Poland19. Alcohol use and gallstone diseases are the most common etiologies of pancreatitis in Eastern Europe. Per capita alcohol consumption increased from the 1970s to the 1990s in many European countries19. In 2020, more than 50% of females aged 15 to 39 years in Eastern Europe were consuming in excess of the non-drinker equivalence20. It was also reported that the age-standardized incidence rate of pancreatitis was much higher in females than in males in Eastern Europe21. We noticed that females aged 15 to 24 years showed increase trends in incidence of pancreatitis. Among the population aged 15 to 49 years, alcohol use is the leading global risk factor for risk-attributable disease burden, causing 2.3% disability adjusted of life years for females22. In view of the harm of alcohol overuse, health education for adolescents and young adults should be developed in the future. Cholelithiasis is also a common cause of acute pancreatitis1. According to GBD 2019, the incidence and prevalence of gallbladder and biliary diseases was much higher in Europe and America23,24. The prevalence of gallstones ranges from 11% to 35% in America adults and from 5.9% to 21.9% in Europe25,26. However, it was reported that Asia (5.1%) had lower prevalence of gallstones27.
The worldwide decline in the pancreatitis death rate may be due to advances in medical care. Currently, the treatment of pancreatitis mainly includes intravenous fluid resuscitation, analgesia, enteral nutrition and organ support28. Recently, great progress has been made in the etiology, diagnosis, and treatment of complications of pancreatitis29. With the progress of clinical nutrition, critical care medicine and endoscopic technology, the treatment of pancreatitis is moving toward standardization. The extensive application of multidisciplinary team model is also an inevitable trend in the standardized treatment of pancreatitis.
To reduce the burden of pancreatitis in women in the future, we should pay attention to this disease in WCBA. Prevention of acute pancreatitis requires concerted contributions from health care professionals from different disciplines, including primary care physicians, gastroenterologists, surgeons, radiologists, endocrinologists, dietitians, and public health experts30. Depending on the cause, preventive interventions include cholecystectomy for biliary pancreatitis, a reduction in alcohol use for alcoholic pancreatitis, strict control of blood lipids for hypertriglyceridemia-induced pancreatitis, and a reduction in the risk factors associated with post-ERCP pancreatitis. As obesity is a risk factor for new gallstones during pregnancy, the first recommendation is to pay attention to diet and weight to prevent the formation of new gallbladder diseases. Additionally, the increase in the serum triglyceride level during pregnancy should be screened for, and the diet should be modified if necessary. Moreover, health education among women is also necessary, especially for biliary and pancreatic health. As we observed an increasing incidence of pancreatitis in females aged 15 to 24, we should also focus on alcohol consumption among young females. Severe acute pancreatitis and chronic pancreatitis patients need multidisciplinary management. The important factors to reduced complications and mortality include fluid resuscitation, nutritional support and analgesia. For instance, early enteral nutrition may reduce mortality in patients with moderate or severe acute pancreatitis31. Moreover, a multicenter retrospective study found that epidural analgesia in acute pancreatitis patients admitted to the intensive care unit was associated with lower 30-day mortality32. More prospective studies evaluating acute pancreatitis mortality are needed in the future.
This study had several limitations. First, incomplete or developing disease registries in low-income countries can lead us to underestimate the incidence of pancreatitis. The GBD study used statistical modeling methods, especially at the national level, and the data in the GBD study relied on modeling data due to the lack of raw data. Next, pancreatitis included in the GBD database was not classified by disease type, such as acute pancreatitis, chronic pancreatitis, or autoimmune pancreatitis, which may limit our broad exploration. Additionally, we should note the hysteresis property of GBD data. Future work should pay attention to more raw epidemiological data on pancreatitis in WCBA, especially in low-middle and low-income countries. The economic burden caused by pancreatitis should also be further studied.
Overall, the global pancreatitis incidence and death in WCBA has decreased since 1990, but the incidence is still high in some high-SDI-countries. Significant increase in pancreatitis incidence occurred in females aged 15 to 24 years. We should pay attention to risk factors for pancreatitis in WCBA, including alcohol use, gallstones, and hypertriglyceridemia. More efficient public health measures are needed to reduce the burden of pancreatitis.
Methods
Data source
Data on incidence and death were gathered from the GBD 2021 result tool (http://ghdx.healthdata.org/gbd-results-tool). The GBD 2021 provided global epidemiological data for 371 diseases from 1990 to 2021 33. The data sources of the GBD study included household surveys, civil registrations, disease registries, disease notifications and other sources33. Each type of data was identified through systematic reviews of published studies, published reports, primary data sources such as health surveys, and datasets provided by GBD collaborators. The data extraction and estimation methods have been described in previous publications33,34. In this study, we selected data from 1990 to 2021 in five socio-demographic index (SDI) quintiles, 21 GBD regions and all countries/territories. The World Health Organization defines WCBA as women aged 15 to 49 years35.
Case definition
According to GBD 2021 Diseases and Injuries Collaborators, pancreatitis is defined as inflammation of the pancreas, including acute and chronic pancreatitis. Acute pancreatitis involves active inflammation and injury to the pancreas, resulting in severe upper abdominal pain and nausea, inappropriate release of pancreatic contents, and a systemic inflammatory response; chronic pancreatitis involves permanent damage to the pancreas from longstanding or recurrent inflammation. We used the 10th International Classification of Diseases code list to identify the disease and the code for acute pancreatitis is K85 and for chronic pancreatitis is K86 33.
SDI
The SDI is a composite indicator based on the geometric mean of total fertility (younger than 25 years), mean education (15 years and older), and lag-distributed income per capita36. The SDI values of all regions and countries/territories from 1990 to 2021 can be downloaded at: https://ghdx.healthdata.org/record/global-burden-disease-study-2021-gbd-2021-socio-demographic-index-sdi-1950–2021.
Data analysis and reporting
The indicators in GBD 2021 include mean estimates and 95% uncertainty intervals (UIs, the 2.5th and 97.5th percentiles among the 500 draws)37. All rates are reported per 100,000 persons. We calculated the estimated annual percentage changes (EAPCs) to assess the temporal trends of the incidence and death rates. If the EAPC and its lower 95% confidence interval (CI) boundary were both greater than zero, an increasing trend was deemed. If the EAPC and its upper 95% CI boundary were both lower than zero, a decreasing trend was deemed38. Total percentage change was used to represent the number change from 1990 to 2021. Data statistical analyses and visualization were performed in R software (version 4.2.2).
Data availability
The datasets for this study can be found in the Global Health Data Exchange query tool (https://vizhub.healthdata.org/gbd-results/).
References
Lee, P. J. & Papachristou, G. I. New insights into acute pancreatitis. Nat. Rev. Gastroenterol. Hepatol. 16, 479–496. https://doi.org/10.1038/s41575-019-0158-2 (2019).
Han, K. et al. Burden of pancreatitis and associated risk factors in China, 1990 to 2019: a systematic analysis for the global burden of disease study 2019. Chin. Med. J. (Engl). 135, 1340–1347. https://doi.org/10.1097/cm9.0000000000002164 (2022).
Shmelev, A., Sill, A. M., Horrigan, T. & Cunningham, S. C. Trends and seasonality in hospitalizations for acute alcohol-related and biliary pancreatitis in the USA. Hepatobiliary Pancreat. Dis. Int. 20, 173–181. https://doi.org/10.1016/j.hbpd.2020.10.003 (2021).
Sarri, G., Guo, Y., Iheanacho, I. & Puelles, J. Moderately severe and severe acute pancreatitis: a systematic review of the outcomes in the USA and European Union-5. BMJ Open. Gastroenterol. 6, e000248. https://doi.org/10.1136/bmjgast-2018-000248 (2019).
Otsuki, M. Chronic pancreatitis in Japan: epidemiology, prognosis, diagnostic criteria, and future problems. J. Gastroenterol. 38, 315–326. https://doi.org/10.1007/s005350300058 (2003).
Luthra, A. K. et al. Endoscopic intervention and cholecystectomy in pregnant women with acute biliary pancreatitis decrease early readmissions. Gastrointest. Endosc. 89, 1169–1177. https://doi.org/10.1016/j.gie.2018.11.026 (2019).
Mądro, A. Pancreatitis in Pregnancy-Comprehensive review. Int. J. Environ. Res. Public Health. 19 https://doi.org/10.3390/ijerph192316179 (2022).
Bhowmik, J., Biswas, R. K. & Ananna, N. Women’s education and coverage of skilled birth attendance: an assessment of sustainable development goal 3.1 in the South and Southeast Asian region. PLoS One. 15, e0231489. https://doi.org/10.1371/journal.pone.0231489 (2020).
Murray, C. J. L. The global burden of disease study at 30 years. Nat. Med. 28, 2019–2026. https://doi.org/10.1038/s41591-022-01990-1 (2022).
Maringhini, A., Rossi, M., Patti, R., Maringhini, M. & Vassallo, V. Acute pancreatitis during and after pregnancy: A review. J. Clin. Med. 13 https://doi.org/10.3390/jcm13072028 (2024).
NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 387, 1377–1396. https://doi.org/10.1016/s0140-6736(16)30054-x (2016).
GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the global burden of disease study 2021. Lancet 402, 203–234. https://doi.org/10.1016/s0140-6736(23)01301-6 (2023).
Eddy, J. J., Gideonsen, M. D., Song, J. Y. & Grobman, W. A. O’Halloran, P. Pancreatitis in pregnancy. Obstet. Gynecol. 112, 1075–1081. https://doi.org/10.1097/AOG.0b013e318185a032 (2008).
Maringhini, A., Dardanoni, G., Fantaci, G., Patti, R. & Maringhini, M. Acute pancreatitis during and after pregnancy: incidence, risk factors, and prognosis. Dig. Dis. Sci. 66, 3164–3170. https://doi.org/10.1007/s10620-020-06608-5 (2021).
Luo, L. et al. Clinical characteristics of acute pancreatitis in pregnancy: experience based on 121 cases. Arch. Gynecol. Obstet. 297, 333–339. https://doi.org/10.1007/s00404-017-4558-7 (2018).
Yang, D. J. et al. Development and validation of a prediction model for moderately severe and severe acute pancreatitis in pregnancy. World J. Gastroenterol. 28, 1588–1600. https://doi.org/10.3748/wjg.v28.i15.1588 (2022).
Hamm, R. G. Acute pancreatitis: causation, diagnosis, and classification using computed tomography. Radiol. Technol. 93, 197ct–219ct (2021).
Manikkavasakar, S. et al. Magnetic resonance imaging of pancreatitis: an update. World J. Gastroenterol. 20, 14760–14777. https://doi.org/10.3748/wjg.v20.i40.14760 (2014).
Roberts, S. E. et al. The incidence and aetiology of acute pancreatitis across Europe. Pancreatology 17, 155–165. https://doi.org/10.1016/j.pan.2017.01.005 (2017).
GBD 2020 Alcohol Collaborators. Population-level risks of alcohol consumption by amount, geography, age, sex, and year: a systematic analysis for the global burden of disease study 2020. Lancet 400, 185–235. https://doi.org/10.1016/s0140-6736(22)00847-9 (2022).
Jiang, W., Du, Y., Xiang, C., Li, X. & Zhou, W. Age-period-cohort analysis of pancreatitis epidemiological trends from 1990 to 2019 and forecasts for 2044: a systematic analysis from the global burden of disease study 2019. Front. Public. Health. 11, 1118888. https://doi.org/10.3389/fpubh.2023.1118888 (2023).
GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet 392, 1015–1035. https://doi.org/10.1016/s0140-6736(18)31310-2 (2018).
Li, Z. Z. et al. Global, regional, and National burden of gallbladder and biliary diseases from 1990 to 2019. World J. Gastrointest. Surg. 15, 2564–2578. https://doi.org/10.4240/wjgs.v15.i11.2564 (2023).
Li, J. et al. Global burden of gallbladder and biliary diseases: A systematic analysis for the global burden of disease study 2019. J. Gastroenterol. Hepatol. 37, 1389–1399. https://doi.org/10.1111/jgh.15859 (2022).
Aerts, R. & Penninckx, F. The burden of gallstone disease in Europe. Aliment. Pharmacol. Ther. 18 (Suppl 3), 49–53. https://doi.org/10.1046/j.0953-0673.2003.01721.x (2003).
Elwood, D. R. Cholecystitis. Surg. Clin. N. Am. 88, 1241–1252. https://doi.org/10.1016/j.suc.2008.07.008(2008).
Wang, X. et al. Global epidemiology of gallstones in the 21st century: A systematic review and Meta-Analysis. Clin. Gastroenterol. Hepatol. 22, 1586–1595. https://doi.org/10.1016/j.cgh.2024.01.051 (2024).
Szatmary, P. et al. Acute pancreatitis: diagnosis and treatment. Drugs 82, 1251–1276. https://doi.org/10.1007/s40265-022-01766-4 (2022).
Mederos, M. A., Reber, H. A. & Girgis, M. D. Acute pancreatitis: A review. Jama 325, 382–390. https://doi.org/10.1001/jama.2020.20317 (2021).
Petrov, M. S. & Yadav, D. Global epidemiology and holistic prevention of pancreatitis. Nat. Rev. Gastroenterol. Hepatol. 16, 175–184. https://doi.org/10.1038/s41575-018-0087-5 (2019).
Gardner, T. B. Acute pancreatitis. Ann. Intern. Med. 174 Itc17-itc32 (2021).
Jabaudon, M. et al. Thoracic epidural analgesia and mortality in acute pancreatitis: A multicenter propensity analysis. Crit. Care Med. 46, e198–e205. https://doi.org/10.1097/ccm.0000000000002874 (2018).
GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet 403, 2133–2161. https://doi.org/10.1016/s0140-6736(24)00757-8 (2024).
GBD 2021 Demographics Collaborators. Global age-sex-specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950–2021, and the impact of the COVID-19 pandemic: a comprehensive demographic analysis for the global burden of disease study 2021. Lancet 403, 1989–2056. https://doi.org/10.1016/s0140-6736(24)00476-8 (2024).
Cao, F. et al. Global, regional and National Temporal trends in prevalence for musculoskeletal disorders in women of childbearing age, 1990–2019: an age-period-cohort analysis based on the global burden of disease study 2019. Ann. Rheum. Dis. 83, 121–132. https://doi.org/10.1136/ard-2023-224530 (2024).
GBD 2021 Forecasting Collaborators. Burden of disease scenarios for 204 countries and territories, 2022–2050: a forecasting analysis for the global burden of disease study 2021. Lancet 403, 2204–2256. https://doi.org/10.1016/s0140-6736(24)00685-8 (2024).
Patwardhan, V. et al. Differences across the lifespan between females and males in the top 20 causes of disease burden globally: a systematic analysis of the global burden of disease study 2021. Lancet Public Health. 9, e282–e294. https://doi.org/10.1016/s2468-2667(24)00053-7 (2024).
Xu, T. et al. Disease burden of Parkinson’s disease in China and its provinces from 1990 to 2021: findings from the global burden of disease study 2021. Lancet Reg. Health West. Pac. 46, 101078. https://doi.org/10.1016/j.lanwpc.2024.101078 (2024).
Acknowledgements
The authors thank the Global Health Data Exchange for providing the data and AJE (www.aje.com) for language help.
Funding
This research was funded by Public Hospital High-quality Development of Scientific Research Project of Chinese Health Promotion Foundation (GL-C032).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by Wenkai Jiang, Ru He and Wence Zhou. The first draft of the manuscript was written by Wenkai Jiang and Ru He. Data visualization and methodology were provided by Huiqi Sun, Tianxin Zhao and Xinru Liu. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jiang, W., He, R., Sun, H. et al. Global incidence and mortality of pancreatitis in women of childbearing age from 1990 to 2021. Sci Rep 15, 14753 (2025). https://doi.org/10.1038/s41598-025-99435-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-99435-5