Abstract
Exposure to adverse ergonomic factors is associated with elevated risk of work-related musculoskeletal disorders (WMSDs) in medical personnel. We aimed to reveal how different adverse ergonomic factors act individually and in combination to influence the risk of WMSDs in medical personnel. From June 2018 to December 2020, we applied multistage cluster random sampling to select a total of 6,099 medical personnel from 54 hospitals in 12 cities in China. All participants were aged over 18 years and had at least one year of hospital working experience. The weighted quantile sum (WQS) model was employed to evaluate the effect of mixed exposures of multiple adverse ergonomic factors on the risk of WMSDs. Compared to a single factor, multiple adverse ergonomic factors significantly increased the risk of WMSDs across body parts, with an OR ranging from 2.83 (95% CI: 2.33, 3.43) to 6.92 (95% CI: 4.91, 9.74). “Working in awkward positions” had the greatest impact on the risk of WMSDs in the neck, shoulder, upper back, and lower back, while “standing for prolonged periods of time” mostly affected the risk of WMSDs in the foot, leg, and knee. Compared with single factor exposure, mixed exposure resulted in a higher risk of WMSDs.
Similar content being viewed by others
Introduction
Work-related musculoskeletal disorders (WMSDs) refer to a group of chronic cumulative diseases caused by adverse ergonomic factors including high intensity exertion, repetitive operation, and poor posture, as well as irrational labor organization process, and adverse social and psychosocial factors, which mainly involve injuries to muscles, tendons, bones, cartilage, ligaments, and nerves in occupational activities, with the diseases of pain, discomfort, and activity limitation1,2. Early identification, assessment, and control of adverse ergonomic factors are crucial to the prevention of WMSDs. Previous studies have shown that 39,000 healthcare workers in Europe have experienced musculoskeletal pain3. The results of a systematic review of 36 observational studies showed that the prevalence of WMSDs in medical personnel is currently more than 75%4. The daily work of medical personnel is characterized by sedentary or long standing, high mental concentration, and manual operation, etc. Adverse ergonomic factors such as high-intensity exertion, prolonged sustained loading, frequent operation (repetitive exertion), poor posture, and protracted localized muscular tension may exist during the operation of medical devices and equipment, which lead to a high prevalence of WMSDs in all parts of the body5,6,7. In addition, healthcare workers often suffer from significant work-related stress and psychological burdens. Prolonged exposure to high-pressure environments may lead to chronic stress responses, further exacerbating muscle tension and fatigue8,9. Moreover, due to shift work and irregular working hours, sleep deprivation and poor sleep quality have become prevalent issues. Sleep deprivation not only impairs cognitive function and emotional regulation but may also reduce the body’s ability to recover, thereby increasing the risk of WMSDs10,11. Under such work characteristics, medical personnel are susceptible to WMSDs, resulting in cumulative strain and injuries to the relevant parts of the body12,13, making them a high-risk group for the development of WMSDs, second only to flight attendants14.
Existing studies have demonstrated that adverse ergonomic factors were associated with WMSDs in medical personnel. It is reported that higher rate of exposure to adverse ergonomic risk factors in those with WMSDs compared to those without WMSDs15. Vieira et al. conducted a systematic review of 32 observational studies on the association of exposure to adverse ergonomic risk factors with WMSDs in physical therapists and found that “repetitive tasks”, “working in fixed positions for long periods of time”, and “excessive surgical treatment of patients” were identified as the most common risk factors for WMSDs in hands and lower back16. Milhem et al.’s comprehensive narrative review of 13 studies on the relationship between adverse ergonomic factors exposure and WMSDs in medical personnel also demonstrated that adverse ergonomic factors such as “lifting”, “repetitive movements”, “long-term stationary posture”, and “heavy physical load” were the main risk factors for lower back pain17. An Australian study of 3,296 medical personnel also observed that “lifting or transferring heavy patients” was related to an increased risk of lower back diseases, and that “working in the same position for prolonged time” was associated with an elevated risk of upper back, lower back, and neck diseases18. A study in the UK involving 3,661 medical personnel also confirmed that “working in the same position for a long time” is the primary risk factor for back and lower limb pain, while “repeating the same task multiple times” is the major risk factor for upper limb WMSDs19.
Previous studies by our team have shown that adverse ergonomic factors including “working in awkward positions”, “repeating the operation many times per minute”, and “carrying more than 5 kg or 20kg heavy objects each time” were risk factors for WMSDs in medical personnel. However, it is still not clear how adverse ergonomic factors are related to the risk of developing WMSDs in various body parts of medical personnel, nor is it clear whether different levels of adverse ergonomic factors differentially affect the risk of developing WMSDs in different parts of the body. In addition, medical personnel may be exposed to multiple adverse ergonomic factors simultaneously during the course of their work, and thus the overall loadings of WMSDs depend on the level of exposure to these adverse ergonomic factors as well as the combination and characterization of the different adverse ergonomic factors. The WQS regression model can deal with high-dimensional data, preventing bias due to high correlations between many different adverse ergonomic factors, and thus avoiding the problems of overfitting and covariance, and can more effectively capture the relationship between the combined effects of mixed adverse ergonomic factor exposures and WMSDs20,21.
In the present study, a cross-sectional questionnaire survey was conducted among medical personnel in multi-city medical institutions in China to evaluate the associations between single and mixed exposures to multiple adverse ergonomic factors and the risk of WMSDs at different body parts, and to reveal how the different adverse ergonomic factors individually and in combination affect the occurrence of WMSDs, in order to provide the basis for the development of a multi-level and multi-angle strategy for the prevention and control of WMSDs.
Methods
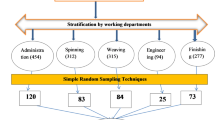
Study population and design
For this study, we employed a multi-phase cluster sampling approach to recruit healthcare professionals from 54 medical institutions nationwide (comprising 6 first-level hospitals, 17 secondary hospitals, and 31 tertiary hospitals), which ran from June 2018 to December 2020. Our study cohort encompassed participants aged over 18, with a minimum of one year of professional experience in hospital settings across 12 diverse Chinese provinces and municipalities. Additionally, healthcare professionals suffering from congenital spinal malformations or musculoskeletal impairments stemming from non-occupational sources, including trauma, infectious disorders, and cancerous tumors were excluded from the study. A total of 6,766 hospital personnel who were on duty at the time of the survey were distributed questionnaires, of which 6,485 hospital personnel successfully filled out and submitted the questionnaires (with a response rate of 95.8%), and after further exclusion of non-medical personnel (e.g. administrative and logistics personnel), a final total of 6,099 medical personnel were included as the study population.
Ethical considerations
The study was designed and conducted in accordance with the tenets of the Declaration of Helsinki 1996 (modified in 2013 at the 64th Assembly of the World Medical Association in Fortaleza, Brazil). All participants provided an written informed consent. Participants were informed that they could withdraw from the study at any stage of the interview. The proposal and questionnaire for this study were approved by the National Institute of Occupational Health and Poisoning Control, Chinese Centre for Disease Control and Prevention (NIOHP202122). The present investigation was undertaken adhering to the stringent guidelines of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) framework22.
Data collection
The study population’s prevalence of WMSDs and their exposure to pertinent ergonomic hazards over the preceding year were examined utilizing an electronically administered version of the Musculoskeletal Disorders Questionnaire, which had been adapted by the Institute of Occupational Health and Poison Control, affiliated with the Chinese Center for Disease Control and Prevention23. The questionnaire is derived from Nordic Musculoskeletal Questionnaires (NMQ)24 and Dutch Musculoskeletal Questionnaires (DMQ)25, and is divided into four sections including sociodemographic information, musculoskeletal diseases in different body parts, adverse ergonomic factors, and work organization factors. The questionnaire has been widely used in China and was shown to have excellent reliability (with Cronbach’s α coefficient of the questionnaire being 0.52–0.92) as well as structural validity (with the variances of common factors being greater than 0.4, explaining 55.17% of the total variance)26.The WMSDs were determined adopting the National Institute for Occupational Safety and Health (NIOSH) definition of the class of disorders in which the investigator experienced diseases of discomfort such as pain, stiffness, burning sensation, numbness, or tingling, and also met the following criteria: (1) discomfort has occurred within the past 1 year; (2) discomfort began after working at the current job; (3) no previous accidents or sudden injuries (affecting the localized area); (4) discomfort has occurred monthly or has lasted for more than 1 week.
Statistical analysis
A total of 6,099 questionnaire data were included in this study. Means ± standard deviations were used for continuous variables while counts and percentages for categorical variables. The association of individual adverse ergonomic factors with WMSDs was first analyzed using a multivariate logistic regression model. In the multivariate logistic regression model, adverse ergonomic factors (e.g., standing/sitting/kneeling for prolonged periods of time, working in awkward postures, using vibrator at work, carrying heavy objects, operate using hands or arms and repeating motions) were included as independent variables. The presence or absence of WMSDs at specific anatomical body sites (e.g., neck, shoulders, upper back, elbow, hands, lower back, legs, knees and feet) was defined as the binary dependent variable (yes/no), and the OR values and their 95% confidence intervals (CI) were applied to estimate the associations between adverse ergonomic factors and the risk of WMSDs. During the model construction process, we considered and adjusted for a range of potential confounders in the models, including sex (male and female), age, type of work (nurse, doctor, lab technician, and paramedic), body mass index (BMI, < 18.5, 18.5–23.9, and > 24 kg/m2), present work tenure (referring to the number of years of work from the current position, categorized as 1 to 5 years, 6 to 10 years, and more than 11 years), working experience (referring to the total number of years of work from the date of starting the job, categorized as 1 to 5 years, 6 to 10 years, 11 to 15 years, and more than 16 years), educational attainment (high school or below, college, and postgraduate and beyond), marital status (unmarried, married, and widowed or separated), frequency of physical exercise (never, sometimes, 2–3 times monthly, 1–2 times weekly, and > 2 times weekly), and hospital level (primary, secondary, and tertiary).
The Weighted Quantile Sum (WQS) model was then used to estimate the joint effect of multiple adverse ergonomic factors on WMSDs, quantifying the relative contribution of different adverse ergonomic factors to WMSDs through a model weight index, thereby identifying the key adverse ergonomic factors that contribute to the occurrence of WMSDs at various body sites. In the WQS regression, all adverse ergonomic factors were simultaneously included as independent variables and corresponded to WMSDs at each anatomical site (as the dependent variable). A bootstrap resampling procedure with 1,000 iterations was implemented to obtain stable estimates of factor weights. In each iteration, the dataset was randomly partitioned into a training subset (40% of the data) to estimate variable weights and a validation subset (60% of the data) to mitigate overfitting. The weights assigned to each adverse ergonomic factor were proportional to their estimated contribution to the risk of WMSDs, and the sum of all weights equaled 1. The model analytically assumes linear and additive effects between the independent variables, based on the creation of an empirically weighted index (WQS index), and the WQS index is incorporated into the logistic regression model. The regression coefficient of the WQS index reflects the combined effect of all ergonomic factors on WMSDs risk20. The WQS regression model demonstrates good specificity and sufficient sensitivity in identifying predictive factors, particularly for highly correlated variables. It effectively mitigates the impact of high multicollinearity on conventional regression results, making it widely applicable in studies examining the effects of multiple exposure factors on health outcomes21,27.
In the sensitivity analyses of the WQS model, we started with the crude model (Model 1); then, added all covariates and adjusted the ratio of validation set to training set 50% vs. 50% (Model 2); finally, added all covariates and adjusted the ratio of validation set to training set 70% vs. 30% (Model 3).
Data were analyzed using R (version 4.4.0), and the WQS regression were used the R package “gWQS”, and all statistical analyses were two tailed, with a p-value of < 0.05 being considered a statistically significant difference.
Results
Characteristics of the study population
The summary of the fundamental attributes pertaining to the study’s participant is presented in Table 1, outlining their overarching characteristics. Out of 6,099 medical personnel, 76.2% (4650) of the participants were from tertiary hospitals. The mean age of our study population was (33.00 ± 8.37) years, with total number of females being 5,424 (88.90%). For BMI, the mean value was (22.40 ± 4.43) kg/m2, and 3,850 (63.10%) were in the normal BMI group. Among the medical personnel, 3,895 (63.90%), 1,709 (28.00%), 356 (5.84%), and 139 (2.28%) were nurses, doctors, paramedics, and lab technicians, respectively. Medical personnel with less than 15 years of service accounted for 76.4% (4,660), and 63.5% (3,873) of the study participants had worked in their current position for less than 10 years. 95.6% of the study participants had a bachelor’s degree or above, 97.3% were married, and the majority of the medical personnel never or seldom participated in physical activity (n = 4,919, 80.65%).
Association of individual adverse ergonomic factors with WMSDs at different body sites assessed by multivariate logistic regression model
Table S1 shows the association of individual adverse ergonomic factors exposures with the risk of WMSDs at different body sites. We observed that occasionally “standing for prolonged periods of time” was a protective factor for WMSDs in the neck (OR = 0.78, 95% CI: 0.64, 0.96), hands (OR = 0.67, 95% CI: 0.50, 0.91), shoulders (OR = 0.76, 95% CI: 0.62, 0.93), and upper back (OR = 0.70, 95% CI: 0.55, 0.88). However, frequently and very frequently “standing for prolonged periods of time” significantly increased the risk of WMSDs in the lower back (OR frequently = 1.31, 95% CI: 1.04, 1.67; OR very frequently = 1.86, 95% CI: 1.47, 2.38), legs (OR frequently = 2.00, 95% CI: 1.46, 2.82; OR very frequently = 2.92, 95% CI: 2.12, 4.11), knees (OR frequently = 2.02, 95% CI: 1.44, 2.09; OR very frequently = 3.25, 95% CI: 2.31, 4.67), and feet (OR frequently = 2.72, 95% CI: 1.90, 4.00; OR very frequently = 4.34, 95% CI: 3.03, 6.39). In addition, “sitting for prolonged periods of time” (occasionally, frequently, very frequently) were protective factors for legs (OR occasionally = 0.74, 95% CI: 0.62, 0.87; OR frequently = 0.69, 95% CI: 0.56, 0.85; OR very frequently = 0.54, 95% CI: 0.42, 0.70), knees (OR occasionally = 0.75, 95% CI: 0.63, 0.90; OR frequently = 0.71, 95% CI: 0.56, 0.88; OR very frequently = 0.63, 95% CI: 0.48, 0.82), and feet (OR occasionally = 0.74, 95% CI: 0.63, 0.87; OR frequently = 0.53, 95% CI: 0.42, 0.66; OR very frequently = 0.39, 95% CI: 0.29, 0.52). However, frequently and very frequently “sitting for prolonged periods of time” were associated with higher risk of WMSDs in the neck (OR frequently = 1.39, 95% CI: 1.18, 1.64; OR very frequently = 1.86, 95% CI: 1.54, 2.25), shoulders (OR frequently = 1.37, 95% CI: 1.16, 1.63; OR very frequently = 1.69, 95% CI: 1.39, 2.05), upper back (OR frequently = 1.28, 95% CI: 1.06, 1.55; OR very frequently = 1.37, 95% CI: 1.11, 1.70), and hands (OR very frequently = 1.35, 95% CI: 1.03, 1.77). The remaining adverse ergonomic factors such as “kneeling for prolonged periods of time”, “carrying more than 5 kg or 20 kg heavy objects each time”, and “operating using hands or arms”, “working in awkward positions”, “using vibrator at work”, and “repeating the operation many times per minute” were all risk factors for the development of WMSDs in various parts of the medical personnel, and the risk increased with the frequency of exposure (e.g., “working in awkward positions” was associated with WMSDs in the neck, OR occasionally = 1.76, 95% CI: 1.53, 2.03; OR frequently = 2.99, 95% CI: 2.54, 3.53; OR very frequently = 3.91, 95% CI: 3.17, 4.83, P− trend < 0.001, Fig. 1).
Associations between mixed exposures to multiple adverse ergonomic factors and WMSDs at different body sites evaluated by WQS model
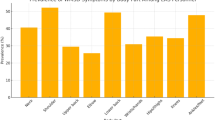
Figure 2 demonstrates the results of the WQS regression analyses between mixed exposures to multiple adverse ergonomic factors and WMSDs in different body parts of medical personnel. The risk of WMSDs at different body sites was elevated when exposed to multiple adverse ergonomic factors in comparison to exposure to a single adverse ergonomic factor. Especially when exposed to multiple adverse ergonomic factors concurrently, the risk of developing WMSDs in the hand (ORmultiple = 6.92, 95% CI: 4.91, 9.74) was found to be higher in comparison to the risk of developing WMSDs in the hand when exposed to any of the adverse ergonomic factors individually (ORindivisual = 1.20, 95% CI: 1.00, 1.45 ~ ORindivisual = 5.15, 95% CI: 3.67, 7.41). Among the adverse ergonomic factors studied, we observed that “working in awkward positions” had the most prominent effect (the largest weight index) on the risk of WMSDs in the neck (weight index: 0.327), shoulders (weight index: 0.313), upper back (weight index: 0.262), and lower back (weight index: 0.262) (Fig. 3). “Carrying more than 20kg heavy objects each time” (weight index: 0.229) and “working in awkward positions” (weight index: 0.177) had the most evident effect on the risk of WMSDs in the elbows (Fig. 3). For hands WMSDs, “kneeling for prolonged periods of time” (weight index: 0.224), “carrying more than 20kg heavy objects each time” (weight index: 0.212) and “repeating the operation many times per minute” (weight index: 0.170) were the top three weighted risk factors (Fig. 3). “Standing for prolonged periods of time” had the greatest impact on the risk of WMSDs in the feet (weight index: 0.413), legs (weight index: 0.313), and knees (weight index: 0.251) (Fig. 3). The results of sensitivity analyses showed that exposure to a mixture of adverse ergonomic factors was significantly associated with an increased risk of WMSDs in different parts of the medical workforce in the crude model, which is similar to the results of the main analysis. For the sensitivity analyses that have adjusted the ratio of the training sets and validation sets of the WQS model also did not change the main findings of our study (Table S2 and Table S3).
Discussions
To the extent of our knowledge, this study pioneeringly investigates the relationship between mixed exposure to multiple adverse ergonomic factors and the likelihood of WMSDs affecting diverse body regions among medical personnel. Based on the results of our previous study assessing adverse ergonomic factors in association with the overall risk of WMSDs among medical personnel, the present study further evaluated the combined effects of various adverse ergonomic factors on WMSDs in various parts of the body, with a view to obtaining the proportion of risk factors contributing to WMSDs for the corresponding parts of the body in medical personnel, so as to target the implementation of risk level management and prevention strategies28. The findings of this study indicated that for medical personnel, as a high-risk group for WMSDs, exposure to adverse ergonomic factors is associated with the risk of WMSDs in various parts of the body, and the combined effect of multiple adverse ergonomic factors further increased the risk of WMSDs compared with the exposure to a single ergonomic risk factor. Therefore, we must pay attention to the combined effects of adverse ergonomic factors on WMSDs in various parts of the body among medical personnel in order to develop more scientific and reasonable ergonomic intervention strategies to prevent and reduce the disease burden of WMSDs.
In this study, the neck (41.7%), shoulder (33.5%), and lower back (26.3%) were the 3 sites with the highest prevalence rates among medical personnel, which is consistent with the results of a systematic review by Vieira et al. that included 32 studies on medical personnel and WMSDs16, suggesting that medical personnel perform their daily medical tasks with a variety of poor postures and work patterns that result in the higher burden on the neck, shoulders, and lower back. We found that “kneeling for prolonged periods of time”, “carrying more than 5–20 kg heavy objects each time”, “operating using hands or arms”, “working in awkward positions”, “using vibrator at work”, and “repeating the operation many times per minute” were all associated with an increased risk of WMSDs at different body sites of the medical personnel. Cromie et al. also suggested that “lifting or heavy loads”, “repetitive motion”, and “fatigue or painful poor posture” were the most important risk factors for the development of WMSDs in medical personnel18. In a series of previous studies, adverse ergonomic factors such as “working in awkward positions”29, “repetitive operations”30, “hand or arm manipulation to handle work”31, “using vibrators”32, and “kneeling for prolonged periods of time”33 were positively associated with the risk of WMSDs in medical personnel, which were all consistent with our findings, suggesting that exposure to adverse ergonomic factors has a significant impact on the occurrence of WMSDs in medical personnel, and that we need to reduce the risk of WMSDs in medical personnel by improving the work environment, optimizing work processes, and taking the necessary preventive measures. Notably, “sitting for prolonged periods of time” was a pronounced risk factor for the neck, shoulders, upper back, and hands; however, it was protective for the legs, knees, and feet, i.e., it reduced the risk of WMSDs in these body parts. Moreover, frequently and very frequently “standing for prolonged periods of time” significantly increased the risk for the lower back, legs, knees, and feet; however, occasionally “standing for prolonged periods of time” was inversely associated with the risk of WMSDs in the neck, shoulders, upper back, and hands. Similar to our results, Wang et al. also found that “standing for prolonged periods of time” was a protective factor for the neck, shoulder, and upper back WMSDs (OR = 0.77, 95% CI: 0.65, 0.91) in manufacturing workers34, suggesting that alternating between different positions may reduce the fatigue of the musculoskeletal system caused by keeping the same position for long hours. Some studies have also found that alternating between sitting and standing can maintain spinal rigidity by cyclically altering lumbar spine loading and reducing the creep effect of passive connective tissues (e.g., intervertebral discs, ligaments) compared to prolonged sitting and standing. Alternating between sitting and standing also reduces muscle fatigue by decreasing the continuous activation of the lumbar stabilizing muscles, which can significantly reduce lower back discomfort. Changes in work posture can also improve local circulation, reduce lactic acid buildup and metabolic waste retention, and may also indirectly reduce the risk of musculoskeletal injury35,36. Therefore, appropriate shifts between sitting and standing postures during work may be effective in reducing the risk of developing WMSDs.
We also observed significant positive associations between mixed exposure to multiple adverse ergonomic factors and WMSDs at different body sites, and the ORs of the joint effect were all greater than the ORs of the individual adverse ergonomic factors on the risk of WMSDs at different body sites, indicating that when medical personnel were simultaneously exposed to multiple adverse ergonomic factors, the risk of WMSDs in each part of the body was significantly higher than that when exposed alone. The possible biomechanical mechanisms for the synergistic effect of multiple adverse ergonomic factors may include awkward postures (e.g., trunk flexion, wrist deviation) which act as biomechanical catalysts alter joint kinematics and increase compressive/shear forces on connective tissue37. For example, sustained flexion of the lumbar region while lifting a patient decreases disc hydration and weakens the passive stability of the spine38. These changes create a biomechanical “baseline vulnerability” that lowers the threshold for injury when combined with other stressors. Repetitive motion and fatigue accumulation repetitive tasks place cyclical loads on muscles and tendons, depleting metabolic reserves and impairing tissue repair39. When superimposed with awkward postures, repetitive movements can exacerbate muscle loading. For example, repetitive shoulder abduction with cervical rotation may simultaneously overload the rotator cuff and cervical erector spinae muscles, leading to synergistic fatigue40. Prolonged static muscle contractions (e.g., standing during surgery, gripping instruments) compromise blood flow, causing ischemia-reperfusion injury and metabolic waste accumulation41. This ischemia weakens tissue toughness and makes tendons and discs more susceptible to damage from concurrent dynamic loading (e.g., transferring patients)42.
We identified the major adverse ergonomic factors that contribute the most to the risk of developing WMSDs at different body sites, such as “working in awkward positions”, which had the most significant effect (the highest weight index) on the risk of WMSDs in the neck (weights: 0.327), shoulders (weights: 0.313), upper back (weights: 0.262), and lower back (weights: 0.262). This could potentially be attributed to medical personnel performing tasks such as surgeries or sedentary work involving typing on computers and writing medical records for long hours. Uncomfortable postures may lead to stiffness and compression of the skeletal and muscular regions, resulting in pain and discomfort43. In addition, prolonged periods of fixed postures may also increase the loads on the muscles around the joints, which may lead to pain in the joints and muscles44. A systematic review of 25 studies on computer users showed that computer use for long hours significantly increased the risk of neck, shoulder, upper back, and lower back disorders45. In addition, a study of 928 Chinese medical personnel found that “working in awkward positions” was correlated with the elevated risk of WMSDs in the neck, shoulders, and back46. The article by Gupta et al. mentioned that when working in awkward positions, the body’s position is significantly shifted away from neutral, with the thighs parallel to the floor when seated, and that tilting causes the pelvis to move backward, flattening the lumbar curve, while at the same time the head naturally tilts forward when performing delicate manipulations with the hands (e.g., surgery), which in turn leads to an increase in muscle tension in the neck and shoulders, and an elevation of intervertebral disc pressures, which in turn accelerated wear and tear on the vertebrae, discs, muscles, and ligaments, which is why WMSDs mainly occurs in the neck and back47,48. The adoption of correct working postures or use of ergonomic musculoskeletal support systems (e.g., use of assistive mobility devices and supportive devices), as well as interventions with organizational factors (e.g., appropriate rest after work, rational workload planning), are of practical significance in reducing WMSDs in medical personnel49,50. Additionally, the available evidence suggested that physical activity and exercise is a low side effects intervention, and in particular regular aerobic exercise (e.g., swimming, walking) has a wide range of benefits for chronic neck, shoulder, and low back pain, improving pain severity and physical functioning, as well as consequent quality of life51. Furthermore, the use of spinal manipulative therapy (SMT) and mobilization (MOB) can also be effective in relieving low back and neck pain52.
Our results indicated that “carrying more than 20kg heavy objects each time” (weight index: 0.229), “working in awkward positions” (weight index: 0.177) and “repeating the operation many times per minute” (weights: 0.136) were risk factors that have a greater impact on the risk of developing WMSDs in the elbow. Zhou et al.’s study on elbow WMSDs also suggested that “lifting heavy objects (more than 20 kg each time)”, “working in awkward positions” and “repetitive operations” were risk factors for WMSDs in the elbow53, which is consistent with our findings. In this study, “kneeling for prolonged periods of time” was the most heavily weighted risk factor for the WMSDs in the hand, probably because medical personnel are required to kneel or squat when changing medications, giving injections, taking biological samples, or performing cardiac compressions at the bedside, where the other joint muscles are relatively immobilized, and the manipulation and pressure are concentrated in the hand54,55. “Standing for prolonged periods of time” was the risk factor that has the greatest impact on the risk of developing WMSDs in the legs (weights: 0.313), knees (weights: 0.251), and feet (weights: 0.413), probably due to the need for medical personnel to remain in a standing position or walking for long periods of time, which may lead to overuse of the muscles of the hips, knees, ankles, and peripheral joints, thereby resulted in injuries56. Meanwhile, Coggon et al. indicated that when medical personnel moved heavy objects (patients), the forces were concentrated in the hip and knee joints, and the increased forces on these joints also increase the risk of WMSDs in the lower extremities57.
The National Plan for Prevention and Control of Occupational Diseases in China from 2021 to 2025 suggested that given the difficulty of preventing and controlling occupational and work-related diseases in China, and that diseases such as WMSDs are becoming increasingly serious, thus cutting-edge basic research and research on key technologies for prevention, diagnosis, as well as treatment and rehabilitation are warranted58. The Action for a Healthy China from 2019 to 2030 also proposed to prevent and control the occurrence of WMSDs through measures such as the promotion of advanced process technologies and the adjustment of work and rest schedules. Since WMSDs have been recently included in China’s catalog of occupational diseases on December 16, 2024, it is particularly urgent to conduct in-depth research on WMSDs to identify their risk factors, establish diagnostic criteria, explore effective treatments, and develop preventive measures59. Given that medical personnel are a large occupational group in China, and their prevalence of WMSDs is second only to that of flight attendants, the prevention, diagnose, and treatment of WMSDs should not be ignored. To address this challenge, the first task is to systematically identify and assess the adverse ergonomic factors that contribute to the risk of WMSDs among medical personnel, and to develop relevant training programs for high-risk groups such as medical personnel to raise their awareness and attention to WMSDs. At the same time, medical institutions should be committed to improving the working environment of medical personnel, such as optimizing the work layout and adjusting the workflow to reduce the exposure to ergonomic factors. In addition, the active promotion and application of ergonomic medical equipment and devices is an important measure to alleviate the musculoskeletal loads of medical personnel during long working hours. Specifically, in our study, it was found that poor working posture was the factor that caused the greatest impact on the neck, shoulders, and back. Poor posture mainly involves the caregivers to move the patients, they should be as close as possible to the body, keep the waist straight, assisting the patients to walk should be close to the body to assist in the movement and to minimize the occurrence of twisted posture of the neck, shoulders, and back. Secondly, the patient’s bedside examination (such as ultrasound), biological sample collection, and dressing change, the examination should be as close as possible to the examination bed to avoid back bending. Surgical procedures with delicate manipulation should be in a sitting position as much as possible to provide elbow and arm support. Thirdly, carrying heavy objects has a high impact on the elbow, which can be assisted by training and exoskeleton systems to reduce the gravity load on the elbow. For hand WMSDs, “kneeling for prolonged periods of time”, “carrying heavy objects over 20 kg”, and “repeating the operation many times per minute” had the greatest hazard weights. The ergonomic musculoskeletal support system such as assisted exertion devices and the use of support devices as well as the intervention of organizational factors such as work breaks, and planning the workload methodically are of practical importance. “Prolonged standing” had the greatest impact on WMSDs in all parts of the lower quadrants, which suggested that medical staff should alternate positions on different work surfaces, such as sitting and standing, in order to minimize the loads formed by standing work on all parts of the lower quadrants and thus reduce the occurrence of WMSDs on the lower body parts.
The present study has some limitations. First, the cross-sectional questionnaire survey was used in this study, which may be subject to recall bias concerning the exposure of adverse ergonomic factors and the risk of WMSDs, and the strength of the argument for a causal relationship between adverse ergonomic factors and WMSDs was insufficient. Second, despite efforts to ensure representativeness (e.g., stratified cluster sampling), potential selection bias may still exist due to non-response. Moreover, according to the National Bureau of Statistics of China, women make up the majority of medical personnel in China (more than 80%), which leads to the high proportion of female respondents in our study, thereby limits the generalizability of results across genders, particularly given potential sex-based differences in symptom reporting and ergonomic exposures. Third, the study population was confined to healthcare workers in China; thus, findings may not extend to other occupational groups (e.g., industrial or agricultural workers). Moreover, although many potential confounders were accounted for in our analyses, we cannot rule out the possibility of residual confounding, such as psychosocial stress and sleep deprivation. Despite these limitations, our findings provide robust evidence on the role of ergonomic exposures in WMSDs, particularly in identifying key modifiable risk factors for targeted workplace interventions. In the follow-up study, multidisciplinary integration (such as ergonomics, biomechanics, physiology, etc.) can be considered to conduct in-depth researches on the pathogenesis of WMSDs, so as to provide more scientific basis for the development of effective prevention and control strategies in the future.
Conclusions
Our findings suggested that the prevalence of WMSDs among medical personnel was jointly influenced by multiple adverse ergonomic factors, and that mixed exposure to multiple adverse ergonomic factors would further increase the risk of WMSDs at various body sites compared with exposure to a single adverse ergonomic factor. Our results provided a scientific basis for multi-level and multi-angle development of WMSDs prevention and control strategies for medical personnel, and suggested that hospital management should strengthen the occupational health protection of medical personnel and reduce the risk of WMSDs among medical personnel by carrying out ergonomics related training programs, optimizing the working environment, promoting the use of ergonomic equipment, and arranging the working hours and intensity reasonably.
Data availability
The data that support the findings of this study are available by email wuchuansha@wust.edu.cn upon reasonable request.
References
Gomez-Galan, M., Perez-Alonso, J., Callejon-Ferre, A. J. & Lopez-Martinez, J. Musculoskeletal disorders: OWAS review. Ind. Health. 55, 314–337. https://doi.org/10.2486/indhealth.2016-0191 (2017).
Dong, Y. D., He, L. H. & Zhang, Z. B. [Research progress on pain-related biomarkers of work-related musculoskeletal disorders]. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 38, 70–73. https://doi.org/10.3760/cma.j.issn.1001-9391.2020.01.018 (2020).
European Agency for Safety and Health at Work. Musculoskeletal disorders in the healthcare sector (2020). Retrieved from https://osha.europa.eu/sites/default/files/publications/documents/Discussion_paper_MSDs_in_health_care_sector.pdf
Jacquier-Bret, J. & Gorce, P. Prevalence of body area Work-Related musculoskeletal disorders among healthcare professionals: A systematic review. Int. J. Environ. Res. Public Health. 20 https://doi.org/10.3390/ijerph20010841 (2023).
Klussmann, A., Gebhardt, H., Liebers, F. & Rieger, M. A. Musculoskeletal symptoms of the upper extremities and the neck: a cross-sectional study on prevalence and symptom-predicting factors at visual display terminal (VDT) workstations. BMC Musculoskelet. Disord. 9, 96. https://doi.org/10.1186/1471-2474-9-96 (2008).
Almhdawi, K. A. et al. Predictors and prevalence of lower quadrant work-related musculoskeletal disorders among hospital-based nurses: A cross-sectional study. J. Back Musculoskelet. Rehabil. 33, 885–896. https://doi.org/10.3233/BMR-191815 (2020).
SofiaT. Prevalence of foot and ankle musculoskeletal disorders in nurses of Lahore Pakistan. J. Med. Res. null (2018).
Zheng, B. et al. The Prevalence and Correlated Factors of Occupational Stress, Cumulative Fatigue, and Musculoskeletal Disorders among Information Technology Workers: A Cross-Sectional Study in Chongqing, China. Healthcare 11, (2023). https://doi.org/10.3390/healthcare11162322
Lu, Y. et al. The mediating role of cumulative fatigue on the association between occupational stress and depressive symptoms: A Cross-Sectional study among 1327 Chinese primary healthcare professionals. Int. J. Environ. Res. Public Health. 19 https://doi.org/10.3390/ijerph192315477 (2022).
Gomez-Duran, E. L., Forero, C. G. & Martin-Fumado, C. On-call-related sleep deprivation and hypomania in healthcare workers. Sleep. Med. 99, 30–33. https://doi.org/10.1016/j.sleep.2022.07.006 (2022).
Tahir, S. et al. The prevalence of fibromyalgia among Doctors in the tertiary care hospital: A cross-sectional study. Annals Med. Surg. 84 https://doi.org/10.1016/j.amsu.2022.104931 (2022).
Clari, M. et al. Prevalence of musculoskeletal disorders among perioperative nurses: a systematic review and META-analysis. BMC Musculoskelet. Disord. 22, 226. https://doi.org/10.1186/s12891-021-04057-3 (2021).
Nankongnab, N. et al. Occupational hazards, health conditions and personal protective equipment used among healthcare workers in hospitals, Thailand. Hum. Ecol. Risk Assess. 27, 804–824. https://doi.org/10.1080/10807039.2020.1768824 (2021).
Jia, N. et al. Epidemiological data of Work-Related musculoskeletal Disorders - China, 2018–2020. China CDC Wkly. 3, 383–389. https://doi.org/10.46234/ccdcw2021.104 (2021).
Alwabli, Y. et al. Work-Related musculoskeletal disorders among medical practitioners in the hospitals of Al’Qassim region, Saudi Arabia. Cureus 12, e8382. https://doi.org/10.7759/cureus.8382 (2020).
Vieira, E. R., Schneider, P., Guidera, C., Gadotti, I. C. & Brunt, D. Work-related musculoskeletal disorders among physical therapists: A systematic review. J. Back Musculoskelet. Rehabil. 29, 417–428. https://doi.org/10.3233/BMR-150649 (2016).
Milhem, M., Kalichman, L., Ezra, D. & Alperovitch-Najenson, D. Work-related musculoskeletal disorders among physical therapists: A comprehensive narrative review. Int. J. Occup. Med. Environ. Health. 29, 735–747. https://doi.org/10.13075/ijomeh.1896.00620 (2016).
Cromie, J. E., Robertson, V. J. & Best, M. O. Work-related musculoskeletal disorders in physical therapists: prevalence, severity, risks, and responses. Phys. Ther. 80, 336–351. https://doi.org/10.1093/ptj/80.4.336 (2000).
Glover, W., McGregor, A., Sullivan, C. & Hague, J. Work-related musculoskeletal disorders affecting members of the chartered society of physiotherapy. Physiotherapy 91, 138–147. https://doi.org/10.1016/j.physio.2005.06.001 (2005).
Carrico, C., Gennings, C., Wheeler, D. C. & Factor-Litvak, P. Characterization of weighted quantile sum regression for highly correlated data in a risk analysis setting. J. Agricultural Biol. Environ. Stat. 20, 100–120. https://doi.org/10.1007/s13253-014-0180-3 (2014).
Tanner, E. M. et al. Early prenatal exposure to suspected endocrine disruptor mixtures is associated with lower IQ at age seven. Environ. Int. 134, 105185. https://doi.org/10.1016/j.envint.2019.105185 (2020).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370, 1453–1457. https://doi.org/10.1016/s0140-6736(07)61602-x (2007).
Yang, L. et al. Introduction of Musculoskeletal Disorders Questionnaire with Questionnaire Attached., (2009). https://d.wanfangdata.com.cn/periodical/gywsyzyb200901025
Kuorinka, I. et al. Standardised nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 18, 233–237. https://doi.org/10.1016/0003-6870(87)90010-x (1987).
Hildebrandt, V. H., Bongers, P. M., van Dijk, F. J. H., Kemper, H. C. G. & Dul, J. Dutch musculoskeletal questionnaire: description and basic qualities. Ergonomics 44, 1038–1055. https://doi.org/10.1080/00140130110087437 (2010).
Du, W. W., Wang, S., Wang, J. X., He, L. H. & Zhu, Z. H. J. Z. L. D. W. S. Z. Y. B. Z. Z. [The assessment of reliability and validity of musculoskeletal questionnaire]. 30, 335–338 (2012).
Loftus, C. T. et al. Maternal exposure to urinary polycyclic aromatic hydrocarbons (PAH) in pregnancy and childhood asthma in a pooled multi-cohort study. Environ. Int. 170, 107494. https://doi.org/10.1016/j.envint.2022.107494 (2022).
Liu, F. et al. The association between adverse ergonomic factors and work-related musculoskeletal symptoms among medical staff in China: a cross-sectional study. Ergonomics 66, 2212–2222. https://doi.org/10.1080/00140139.2023.2193868 (2023).
Rafeemanesh, E., Khooei, A., Niroumand, S. & Shirzadeh, T. A study on musculoskeletal complaints and working postures in pathology specialists in Iran. BMC Musculoskelet. Disord. 22, 1012. https://doi.org/10.1186/s12891-021-04870-w (2021).
Gurgueira, G. P. & Alexandre, N. M. Medical reports recommending work restrictions at a teaching hospital in Brazil. Rev. Latinoam. Enferm. 14, 510–516. https://doi.org/10.1590/s0104-11692006000400007 (2006).
Pompeii, L. A., Lipscomb, H. J., Schoenfisch, A. L. & Dement, J. M. Musculoskeletal injuries resulting from patient handling tasks among hospital workers. Am. J. Ind. Med. 52, 571–578. https://doi.org/10.1002/ajim.20704 (2009).
Michalak-Turcotte, C. Controlling dental hygiene work-related musculoskeletal disorders: the ergonomic process. J. Dent. Hygiene: JDH. 74, 41–48 (2000).
Spector, J. T., Adams, D. & Silverstein, B. Burden of work-related knee disorders in Washington State, 1999 to 2007. J. Occup. Environ. Med. 53, 537–547. https://doi.org/10.1097/JOM.0b013e31821576ff (2011).
Wang, F. J. et al. [Occurrence pattern of musculoskeletal disorders and its influencing factors among manufacturing workers]. Beijing da xue xue bao. Yi xue ban = Journal of Peking University. Health sciences 52, 535–540, (2020). https://doi.org/10.19723/j.issn.1671-167X.2020.03.021
Gallagher, K. M., Campbell, T. & Callaghan, J. P. The influence of a seated break on prolonged standing induced low back pain development. Ergonomics 57, 555–562. https://doi.org/10.1080/00140139.2014.893027 (2014).
Park, J. H. & Srinivasan, D. The effects of prolonged sitting, standing, and an alternating sit-stand pattern on trunk mechanical stiffness, trunk muscle activation and low back discomfort. Ergonomics 64, 983–994. https://doi.org/10.1080/00140139.2021.1886333 (2021).
Gallagher, S. & Heberger, J. R. Examining the interaction of force and repetition on musculoskeletal disorder risk: a systematic literature review. Hum. Factors. 55, 108–124. https://doi.org/10.1177/0018720812449648 (2013).
Bazrgari, B., Shirazi-Adl, A. & Arjmand, N. Analysis of squat and stoop dynamic liftings: muscle forces and internal spinal loads. Eur. Spine J. 16, 687–699. https://doi.org/10.1007/s00586-006-0240-7 (2007).
van der Beek, A. J. & Frings-Dresen, M. H. Assessment of mechanical exposure in ergonomic epidemiology. Occup. Environ. Med. 55, 291–299. https://doi.org/10.1136/oem.55.5.291 (1998).
Akesson, I., Balogh, I. & Hansson, G. A. Physical workload in neck, shoulders and wrists/hands in dental hygienists during a work-day. Appl. Ergon. 43, 803–811. https://doi.org/10.1016/j.apergo.2011.12.001 (2012).
Visser, B. & van Dieen, J. H. Pathophysiology of upper extremity muscle disorders. J. Electromyogr. Kinesiol. 16, 1–16. https://doi.org/10.1016/j.jelekin.2005.06.005 (2006).
Jones, T. & Kumar, S. Physical ergonomics in low-back pain prevention. J. Occup. Rehabil. 11, 309–319. https://doi.org/10.1023/a:1013304826873 (2001).
Wu, S., He, L., Li, J., Wang, J. & Wang, S. Visual display terminal use increases the prevalence and risk of work-related musculoskeletal disorders among Chinese office workers: a cross-sectional study. J. Occup. Health. 54, 34–43. https://doi.org/10.1539/joh.11-0119-oa (2012).
ozvurmaz, S. & Mandiracioglu, A. Prevelans of upper extremity musculoskeletal complaints and its relationship with risk factors for bank employees working with computer. Ulutas Med. J. 3 https://doi.org/10.5455/umj.20160922084115 (2017).
Demissie, B., Bayih, E. T. & Demmelash, A. A. A systematic review of work-related musculoskeletal disorders and risk factors among computer users. Heliyon 10, e25075. https://doi.org/10.1016/j.heliyon.2024.e25075 (2024).
Wang, J. et al. Work-Related musculoskeletal disorders and risk factors among Chinese medical staff of obstetrics and gynecology. Int. J. Environ. Res. Public Health. 14 https://doi.org/10.3390/ijerph14060562 (2017).
Gupta, S. Ergonomic applications to dental practice. Indian J. Dent. Res. 22, 816–822. https://doi.org/10.4103/0970-9290.94677 (2011).
Lis, A. M., Black, K. M., Korn, H. & Nordin, M. Association between sitting and occupational LBP. Eur. Spine J. 16, 283–298. https://doi.org/10.1007/s00586-006-0143-7 (2007).
Foster, N. E. et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet 391, 2368–2383. https://doi.org/10.1016/S0140-6736(18)30489-6 (2018).
Jaromi, M., Nemeth, A., Kranicz, J., Laczko, T. & Betlehem, J. Treatment and ergonomics training of work-related lower back pain and body posture problems for nurses. J. Clin. Nurs. 21, 1776–1784. https://doi.org/10.1111/j.1365-2702.2012.04089.x (2012).
Geneen, L. J. et al. Physical activity and exercise for chronic pain in adults: an overview of Cochrane reviews. Cochrane Database Syst. Rev. 4 https://doi.org/10.1002/14651858.CD011279.pub3 (2017).
Bronfort, G., Haas, M., Evans, R. L. & Bouter, L. M. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 4, 335–356. https://doi.org/10.1016/j.spinee.2003.06.002 (2004).
Zhou, Z. et al. Risk and related factors of elbow musculoskeletal diseases: a nationwide cross-sectional survey in China. J. Occup. Health. 66 https://doi.org/10.1093/joccuh/uiae031 (2024).
Wai, E. K., Roffey, D. M., Bishop, P., Kwon, B. K. & Dagenais, S. Causal assessment of occupational carrying and low back pain: results of a systematic review. Spine J. 10, 628–638. https://doi.org/10.1016/j.spinee.2010.03.027 (2010).
de Jong, J. P. et al. The incidence of acute traumatic tendon injuries in the hand and wrist: a 10-year population-based study. Clin. Orthop. Surg. 6, 196–202. https://doi.org/10.4055/cios.2014.6.2.196 (2014).
Sun, W. et al. Prevalence of Work-Related musculoskeletal disorders among nurses: A Meta-Analysis. Iran. J. Public. Health. 52, 463–475. https://doi.org/10.18502/ijph.v52i3.12130 (2023).
Hulshof, C. T. J. et al. The effect of occupational exposure to ergonomic risk factors on osteoarthritis of hip or knee and selected other musculoskeletal diseases: A systematic review and meta-analysis from the WHO/ILO joint estimates of the Work-related burden of disease and injury. Environ. Int. 150, 106349. https://doi.org/10.1016/j.envint.2020.106349 (2021).
Interpretation of the National Plan for Prevention and Control of Occupational Diseases (2021–2025), (2021). https://www.gov.cn/zhengce/2021-12/26/content_5664659.htm
Evaluation plan on ‘Healthy China’ released, (2019). https://english.www.gov.cn/policies/latestreleases/201907/15/content_WS5d2c7b11c6d05cbd94d67a12.html
Acknowledgements
We would like to express our gratitude to the team members who were instrumental in the distribution and collection of data, as well as all medical personnel who participated in the questionnaire survey.
Funding
This work was supported by the Open Fund Project of Hubei Provincial Key Laboratory of Occupational Hazard Identification and Control (OHIC2023Y06), the Project of Occupational Health Risk Assessment and National Occupational Health Standard Formulation of National Institute of Occupational Health and Poison Control (Project No.131031109000150003), The Project of Occupational Health Risk Assessment and the National Occupational Health Standard Formulation of the National Institute of Occupational Health and Poison Control (102393220020090000020) and National Key R&D Program - Research on Key Technologies and Intervention Strategies for the Prevention and Control of Work-related Diseases and Occupational Injuries (2022YFC2503205), and Joint Foundation of Hubei Provincial Key Laboratory of Occupational Hazard Identification and Control (JF2024-Y25).
Author information
Authors and Affiliations
Contributions
Fei Liu responsible for Conceptualization, Methodology, Validation, Funding acquisition, Writing - Review & Editing; Yongxian Duan responsible for Methodology, Software, Formal analysis, Writing - Original Draft, Visualization, Fei Liu and Yongxian Duan contributed equally to this work; Zhongxu Wang responsible for Investigation, Resources, Data Curation, Supervision, Project administration, Funding acquisition; Ruijie Ling, Qing Xu, Jingzhi Sun, Yimin Liu, Yan Yang, Gang L, Huadong Zhang, Dongxia Li, Rugang Wang, Jing Liu, Tianlai Li, Jixiang Liu responsible for Investigation, Resources, Data Curation; Xingyue Geng, Wenxuan Xiong, Zhuoya Li responsible for Validation, Visualization; Ning Jia responsible for Investigation, Resources, Data Curation, Supervision, Funding acquisition; Chuansha Wu responsible for Conceptualization, Methodology, Writing - Review & Editing. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The proposal and questionnaire for this study were approved by the National Institute of Occupational Health and Poisoning Control, Chinese Centre for Disease Control and Prevention (NIOHP202122).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, F., Duan, Y., Wang, Z. et al. Mixed adverse ergonomic factors exposure in relation to work-related musculoskeletal disorders: a multicenter cross-sectional study of Chinese medical personnel. Sci Rep 15, 14705 (2025). https://doi.org/10.1038/s41598-025-99477-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-99477-9