Abstract
Snooze alarm use is a common, but poorly understood human behavior. We explore the prevalence and characteristics of snooze alarm use in more than 3 million nights collected in a global sample of users of a sleep monitoring smartphone application. On the nights that participants logged a sleep session, more than half (55.6%) of the sessions ended with a snooze alarm. Of the sleep sessions ending with snooze alarm, snooze alarm was pressed on average 2.4 times (95% CI: 2.4–2.5) and the average duration of snooze alarm use was 10.8 minutes (95% CI: 10.7–10.9). We observed significantly more snooze alarm use in women as compared to men. Long sleep sessions (> 9 h) were more likely to end with snooze alarm use than recommended duration (7 to 9 h) or short (< 7 h) sleep sessions. Sleepers who went to bed earlier used snooze alarm less, while those who went to bed later than usual used the snooze alarm more. Future research is needed to understand the impact of snooze alarm use on daytime performance.
Similar content being viewed by others
Introduction
Sleep is a biological imperative, the timing and duration of which is influenced by the interaction between time spent awake and internal circadian rhythms1,2. Humans often attempt to override these biological regulatory processes, for reasons that are in some cases under one’s control and in other cases out of one’s control (e.g., occupational, family obligations). Population trends over the past several decades reflect a global population falling short of healthy sleep targets (e.g., meeting their nightly 7 to 9 h recommended duration3,4, which may lead to other health concerns, including worsened mental health5,6,7, increased cardiovascular disease risk8,9,10,11,impaired cognitive function12,13, lower productivity14, and increased healthcare costs14.
Humans naturally wake after sufficient sleep, yet under conditions of insufficient sleep duration, often require assistance, such as the use of an alarm, to meet a prespecified wake time. Many rely on their mobile or smartphone to serve this function. Inherent to many alarm clocks is a ‘snooze’ function, which is programmed to alert again several minutes after an initial alarm (snoozing), presumably to allow the sleeper to get more rest15. However, sleep experts caution that the sleep one can get after hitting snooze is of poor quality, and that this habit should be avoided in favor of setting an alarm for the last realistic wake time to allow for as much consolidated, uninterrupted sleep as possible16.
There are surprisingly few scientific studies that have examined the prevalence of snooze alarm use. Available studies suggest that snooze alarm use is common, reported by anywhere between 30 and 60% of individuals, depending upon the population studied (e.g., students, employed adults). Two reports show that snooze alarm use is more common among evening as compared to morning chronotypes, and associated with short sleep duration15,17, and more feelings of drowsiness upon waking17. In a crossover study using polysomnography, habitual snooze alarm users were initially randomized to one of two conditions: sleep for their entire habitual sleep time and wake with a single alarm or wake up 30 min before their habitual wake time, then use the snooze alarm several times; subsequently they slept in the alternate condition17. Findings of this study revealed less sleep time, more arousals, and lower sleep efficiency in the snooze alarm condition as compared to the condition allowed to sleep a full duration and wake to a single alarm17. Finally, in a small convenience sample of participants from lucid dreaming social media groups, use of a snooze alarm was reported on average 1.5 times per day19.
Here we contribute to the literature on snooze alarm use by analyzing a large database derived from users of a sleep monitoring smartphone application (app) “SleepCycle.” Six months of data from 21,222 app users and more than 3 million sleep sessions from users across 4 continents facilitated our investigation of the prevalence of snooze alarm use in this population and its implications for sleep across countries, cultures, and climates.
Results
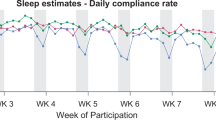
Among participants (n = 21,222), 54.2% were men, 45.5% women, and 0.3% other. Most participants resided in the United States (n = 8,871, 43.6%), followed by the United Kingdom (n = 2,575, 12.7%), Japan (n = 2,011, 9.9%), Australia (n = 1,326, 6.5%), and Germany (n = 1,258, 6.2%, see Supplement 1). Users contributed on average 142.2 (std = 21.4) sleep sessions during the tracking interval. On the nights that participants logged a sleep session, more than half (55.6%) of the sessions ended with a snooze alarm. Most users were classified as heavy snooze alarm users (i.e., those with more than 80% of sleep sessions ending with a snooze alarm, n = 5,855, 45.2%), followed by moderate snooze alarm users (i.e., those with 40–60% of sleep sessions ending with a snooze alarm, n = 3,614, 27.9%), and light snooze alarm users (i.e., those with fewer than 20% of sleep sessions ending with a snooze alarm, n = 3,492, 26.9%). In a plot of 500 randomly selected users in October 2022 (Fig. 1), robust within week variation is evident among the light snooze alarm users, with more snooze alarm use during the traditional work week and less snooze alarm use on the weekend.
Sleep and snooze alarm behavior of 500 users selected at random in the month of October, sorted from least snooze alarm use to most snooze alarm use. Notes. White indicates no sleep session is logged. The 500 participants was comprised of users who logged sleep sessions regularly (i.e., on 50% of nights or more each month of the observation interval).
Within the light, moderate, and heavy snooze alarm use categories, visual inspection of raster plots (Supplement 2) reveals a few trends. Heavy snooze alarm users made use of snooze alarm on most days, used snooze alarms multiple times within each day, and demonstrated erratic bed/wake times. Light and moderate user categories appeared to use snooze alarm less frequently and demonstrate more consistent sleep times.
Of the sleep sessions ending with snooze alarm, users pressed the snooze alarm on average 2.4 times (95% CI: 2.4–2.5) and spent on average 10.8 min snoozing (95% CI: 10.7–10.9). In analyses of snooze alarm by type of user, heavy snooze alarm users pressed the snooze alarm on average 4.0 times (95% CI: 3.9–4.1) and snoozed on average 20.2 min (95% CI: 19.9–20.5). Moderate snooze alarm users pressed the snooze alarm on average 1.7 times (95% CI: 1.7–1.7) and spent 6.3 min snoozing (95% CI: 6.2–6.5). Light snooze alarm users pressed the snooze alarm 1.2 times (95% CI: 1.2–1.3) and spent on average 3.0 min snoozing (95% CI: 2.8–3.2).
Snooze alarm use by day of the week
Monday through Friday were the days when users most used their snooze alarm (Monday: 467,376; Tuesday: 486,994; Wednesday: 488,485; Thursday: 482,179; Friday: 474,096). Snooze behavior was less commonly used on Saturday (330,768) and Sunday (287,378) (Supplement 3). Within those individuals who used snooze alarm, users pressed the snooze alarm approximately 2.5 times, with slightly less snooze alarm use on the weekend (Saturday and Sunday) as compared to weekdays (Monday through Friday, F = 26.5, p < 0.001, Fig. 2, Panel A). Among the individuals who used snooze alarm, individuals snoozed 11 min on average, with less snooze alarm use on the weekend than on the weekdays (F = 8.9, p < 0.01, Fig. 2, Panel B).
Snooze alarm use by gender
The independent samples t-test revealed a significant difference by gender in snooze alarm use (women: 2.5 snooze alarms, 95% CI: 2.5–2.6; men: 2.3 snooze alarms, 95% CI 2.3–2.4). The effect size, as measured by Cohen’s D, was 1.1, indicating a large effect size. The independent samples t-test revealed a significant difference by gender in minutes spent snoozing (women:11.5 min, 95% CI: 11.2–11.7; men: 10.2 min, 95% CI: 10.0–10.4). The effect size was 2.8, indicating a large effect size.
Snooze alarm use by country
With respect to country of residence, there was little variation in snooze alarm behavior, but those users residing in Sweden demonstrated the highest average snooze alarm utilization(2.7 snooze alarms, 95% CI: 2.5–2.8), followed by Germany (2.5 snooze alarms, 95% CI: 2.4–2.6) and the United States (2.5, 95% CI: 2.4–2.5). Users residing in Japan had the lowest average snooze alarm utilization (2.2 snooze alarms, 95%CI: 2.2–2.3), as did users residing in Australia (2.2 snooze alarms, 95% CI: 2.2–2.3). Users residing in Sweden had the highest snooze alarm duration per sleep session (11.7 min, 95% CI: 10.9–12.7), followed by users residing in Brazil (11.3 min, 95% CI: 10.4–12.3) and the United States (11.3 min, 95% CI: 11.0–11.5). Users residing in Japan had the lowest snooze alarm duration per sleep session Japan (9.2 min, 95% CI: 8.8–9.7).
Snooze alarm use by seasonality and hemisphere
Regarding seasonality, there was modest variation. The month with the most snooze alarm behavior was December (number of snooze alarms: 2.59, 95% CI: 2.56–2.62; snooze duration: 11.70 min, 95% CI: 11.52–11.89), while September had the lowest (number of snooze alarms: 2.40, 95% CI: 2.37–2.42; snooze duration: 10.58 min, 95% CI: 10.42–10.74). In the Northern Hemisphere, December was still the month with most snooze behavior (number of snooze alarms: 2.62 t, 95% CI: 2.59–2.64; snooze duration: 11.83 min, 95% CI: 11.64–12.02) and September was the lowest (number of snooze alarms: 2.40, 95% CI: 2.37–2.43; snooze duration:10.58 min, 95% CI: 10.42–10.74). In the Southern Hemisphere, July was the month with the most snoozing (number of snooze alarms: 2.35, 95% CI: 2.26–2.44; snooze duration: 10.2 min, 95% CI: 9.73–10.76), while November had the lowest (number of snooze alarms: 2.29, 95% CI: 2.21–2.37; snooze duration: 10.12 min, 95% CI: 9.64–10.67, Fig. 3).
Number of times snooze alarm was utilized, and the average minutes spent snoozing by month and by hemisphere. Notes. The orange line indicates snooze alarm behavior in countries in the Southern hemisphere by month. The blue line indicates snooze behavior in countries in the Northern hemisphere by month. The graphs depict average snooze alarm sessions by month (Panel A) and average minutes spent snoozing by month (Panel B).
Snooze alarm use by sleep variables
The most common sleep duration in the sample was 7 h (n = 531,167, 33.4%), followed by 8 h (n = 405,281, 25.5%). The least common sleep duration was 10 h (n = 32,607, 2.0%), followed by 5 h (n = 135,124, 8.5%). The most common sleep times were 11 p.m. (n = 437,071, 26.1%), 10 p.m. (n = 364,338, 21.7%), 12 a.m. (n = 328,328,19.6%), and 1 a.m. (n = 177,231, 10.6%), with all other sleep times representing less than 10% of the sample.
Average number of snooze alarm sessions varied by sleep duration (F = 7316.5, p-value < 0.001), with more snooze behavior following sleep sessions that were 8 h or more hours in duration (8 h: 3.12 snooze alarms, 95% CI: 3.12–3.13; 9 h: 4.17 snooze alarms, 95%CI; 4.15–4.20; 10 h: 5.85 snooze alarms, 95% CI: 5.79–5.91, 11 h: 7.64 snooze alarms, 95%CI: 7.46–7.83) and fewer snooze alarms following shorter duration sleep sessions (e.g., 6 h: 2.4 snooze alarms, 95% CI: 2.4–2.5) (Fig. 4, Panel A). Minutes spent snoozing also varied by sleep duration (F = 9149.7, p < 0.001), with longer snooze durations among those sleeping 8 or more hours ([(8 h: 14.73 min, 95%CI: 14.67–14.78; 9 h: 19.00 min, 95%CI: 18.88–19.12; 10 h: 25.70 min, 95%CI: 25.33, 26.07; 11 h: 35.04 min, 95%CI: 22.86–36.22), and shorter snooze alarm durations among those sleeping shorter durations (e.g., 6 h: 11.5 min, 95%CI: 11.4–11.5). (Fig. 4, Panel B).
Number of times snooze alarm was utilized (Panel A), and the average minutes of snooze alarm use (Panel B) by sleep duration hour. Notes. Blue circles indicate mean snooze sessions (Panel A) and duration of snooze alarm use (Panel B). The lines indicate the 95% confidence interval around each estimate, which are calculated based on mean error. Durations displayed on the x axis reflects durations from 0.00 to 0.00 for each hour. In other words, those in the ‘5’ hour duration could have slept from 5.00 h to 5.99 hours.
With respect to sleep times (i.e., the time at which a person intended to fall asleep), snooze alarm use was highest among those with a sleep time of 10:00 AM (number of snooze alarms: 4.9, s.d.=6.3; snooze duration: 25.8 min, s.d.=45.7). Snooze alarm use was lowest among those with a sleep time of 8:00 PM (number of snooze alarms: 2.5, s.d.=2.6; snooze duration: 11.3 min, s.d.=20.2, Fig. 5). Snooze alarm use was high among those with a wake time of 1:00 PM (number of snooze alarms: 6.7, s.d.=8.6; snooze duration: 37.6 min, s.d.=59.1). Snooze alarm use was low among those with a wake time of 3:00 AM (number of snooze alarms: 2.0, s.d.=1.9; snooze duration: 8.9 min, s.d.=42.82, Fig. 6).
Number of times snooze alarm was utilized (Panel A), and the average minutes of snooze alarm use (Panel B) by sleep time. Notes. Blue circles indicate the mean snooze alarm sessions by sleep hour (Panel A) and mean duration of snooze alarm use by sleep hour (Panel B). Blue bars indicate the 95% confidence interval around each estimate.
Number of times snooze alarm was utilized (Panel A), and the average minutes of snooze alarm use (Panel B) by wake time. Notes. Blue circles indicate the mean snooze alarm sessions by wake time hour (Panel A) and duration of snooze alarm use by wake time hour (Panel B). Blue bars indicate the 95% confidence interval around each estimate.
With respect to sleep and wake time variability, sleep at habitual bedtime was associated with 5–6 snooze alarms on average. Going to bed earlier than usual was associated with fewer snooze alarms compared to sleep at the habitual bedtime (bedtime variability z-scores for 1–4 snooze alarms ranged from − 0.05 to −0.02). Going to bed later than usual most often resulted in either not using the snooze alarm (0 snooze alarms; bedtime variability z-score = 0.04, 95% CI: 0.03–0.04) or 7 or more snooze alarms on average (bedtime variability z-scores for > 5 snooze alarms were all 0.003 and higher) (Fig. 7).
Within-subject bedtime variability by number of snooze alarm sessions. Notes. Z-scores are computed as the mean/standard deviation of a user’s bedtime on any given night. In other words, the variation from the user’s typical bedtime on a given night. The figure depicts variability between a person’s typical bedtime and the bedtime on a particular night (y axis) by the number of subsequent snooze alarm sessions the user undertakes (x axis). Sleep sessions that do not terminate in a snooze alarm are included in this analysis (depicted as 0 on the x axis).
Discussion
We examined use of snooze alarm in a large sample of users of a sleep tracking smartphone app over a six-month time interval. Overall, users pressed the snooze alarm approximately twice daily and spent on average 11 min snoozing, which equates to nearly one 6-hour night of sleep lost per month. Heavy snooze alarm users, however, snoozed approximately 4 times per day, resulting in more time snoozing (20 min), whereas light users of the snooze alarm averaged only one snooze alarm and 3.0 min snoozing on average. Our results reveal more snooze alarm Monday through Friday and less snooze alarm use on Saturday and Sunday, a finding which may be explained by fewer commitments on weekend mornings among certain employee or student populations. In addition, we observed that women’s snooze duration was slightly longer than men. It is possible the gender difference observed in snooze alarm behavior stems from the increased risk for insomnia among women as compared to men20. In addition, women shoulder a greater burden of childcare duties compared to men21, which may be on top of professional or other duties, therefore reducing the time available to women for sleep and increasing risk for sleep difficulties22, which may increase reliance upon snooze alarm.
We observed minimal month-to-month differences, although there was slightly more snooze alarm use in December and less in September among users who reside in the Northern hemisphere, and the opposite among those who reside in the Southern hemisphere, for whom snooze alarm use was more common during July and less common in November. These differences may be due to month-to-month differences in the timing of natural light exposure and less access to natural light during winter months, which could result in a delay to circadian rhythms23, consistent with previous research that has shown seasonal differences in sleep24.
We observed differences in snooze alarm use by sleep variables. First, we saw more snooze alarm use among longer sleepers, which is counter to other reports that indicate snooze alarm use is more common in short as compared to long sleepers15,17. In our study, those sleeping 10 h or longer hit the snooze alarm twice as many times as those sleeping 6 h (5 times v. 2 times) and snoozed for twice as long as those sleeping 6 h (25 min v. 12 min). It could be that short sleepers are cutting sleep short for occupational reasons (e.g., for an early work shift with a fixed start time) or caregiving responsibilities (e.g., to care for a young child or older adult), therefore, leaving a person unable to use the snooze alarm multiple times. On the other hand, the additional snooze behavior observed after long sleep sessions could be indicative of hypersomnia or compensatory sleep to recover from sleep deficiency. With respect to sleep and wake times, compared to those falling asleep at 8 p.m., those falling asleep at 10 a.m. pressed the snooze alarm more times per day on average (5 times v. 2.5 times) and snoozed for more than twice as long in total (26 min v. 11 min). Another explanation could be that those falling asleep at this time are shift workers or individuals who have stayed up all night, who may have inadequate time in bed, and hence, more reliance upon snooze alarm. Moreover, those with misaligned sleep may experience more fragmented sleep, and thus, greater reliance upon the snooze alarm.
Finally, those with variable sleep due to going to bed earlier tended to use the snooze alarm less on those days, whereas people with variable sleep due to going to bed later tended to use the snooze alarm more on those days. It is possible this reflects sleep patterns of shift workers, or those with occupational schedules largely out of their control, but future work is needed as the present analysis did not have data on occupation. Our study adds to the available evidence in the scientific literature on snooze alarm use. One of the primary contributions of our study is a global sample of smartphone users. Previous studies examining snooze alarm behavior have included populations with limited generalizability, such as an online convenience sample or groups of employed individuals at a single employer. Previous research on snooze alarm behavior revealed that average snooze alarm duration ranged from 22 to 27 minutes per day,15,17 while our study reveled an average of 11 minutes of snooze alarm use per day. The average snooze alarm duration observed in previous studies of 22 to 27 minutes align more with the heavy snooze alarm user category in the present study. Whereas previous studies have relied on self-report, a strength of our study is objective snooze alarm data. It is possible that previous studies overestimated the amount of time a person typically spends snoozing after their first alarm.
Limitations
The strengths of our study include a large, international sample, allowing us to capture objective snooze alarm behavior across cultures and climates. Despite these strengths, there are several limitations. First, there may be variability in the accuracy of sleep timing data provided by the app. The sleep duration variable used in the present analysis likely overestimates actual sleep duration, as it does not account for sleep latency or awakenings. We are not certain that all users attempt sleep immediately after pressing “Start,” and it is likely that the sleep latency, or time it takes to fall asleep, varies widely from one person to the next. Relatedly, we define sleep duration as the time between sleep and first alarm/wake times. The sleep duration variable used here thus reflects time in bed, a construct that captures all time spent in bed, not necessarily time spent sleeping. However, time in bed definitions include time spent in bed after first waking, such as the time including snooze alarm use25, which is not included in our definition of sleep duration; thus we retain the term sleep duration throughout this manuscript. Nevertheless, sleep duration analyses should be interpreted with caution. Also, we examine snooze alarm use by sleep time variability but not wake time variability. Future research may explore these associations. Second, although the snooze alarm data (e.g., number of times the snooze alarm is utilized and the minutes spent snoozing) employed in this study is objective, we cannot be certain that users were sleeping between alarms. It is possible that users are awake in between snooze alarms checking emails or scrolling social media. Therefore, it is likely that we overestimate snooze alarm use in the present analysis. Third, we do not have age information, only gender, for demographic characteristics of the sample. Moreover, our sample of SleepCycle users may not be reflective of the general population, although one version of the software is freely available for all smartphone users worldwide. Finally, we do not have self-reported information, such as feelings of restoration or grogginess after waking from sleep.
Conclusion
We characterize snooze alarm use in a large international sample of sleepers. We observe that use of snooze alarm is common, and averages 11 min per sleep session. Snooze alarm use was relatively stable, with a few small differences by day of the week and region. We observed that women utilize snooze alarms slightly more frequently than men, and longer sleep sessions were characterized by more snooze alarm use than healthy sleep duration and short sleep sessions (6 h or less). Finally, going to bed earlier than normal was associated with less snooze alarm use, while going to bed later than usual was associated with more snooze alarm use. Therefore, heavier snooze alarm use may be part of the phenotype of poor sleep health. Given that snooze alarm use is discouraged by experts due to the sleep fragmentation it causes, messages that discourage snooze alarm in favor of setting the latest possible alarm may be a viable strategy for public health communication efforts to promote sleep.
Materials and methods
Data collection
We obtained snooze alarm, sleep, and demographic data from a sleep monitoring smartphone-based application (app), SleepCycle (Gothenburg, Sweden). Users of the app have the opportunity to consent for their data to be included in research. Informed consent was obtained from all the participants and/or their legal guardians. Data are not publicly available, but were obtained upon request to SleepCycle. All methods were carried out in accordance with relevant guidelines and regulations.
Users of the app may elect to use the app as an alarm clock. Those who elect to use the app as an alarm are prompted to select either a traditional snooze (i.e., an alarm clock that has a predetermined duration for snooze that may go off at a time of their choosing) or a smart snooze (i.e., an alarm clock that will wake the person up in a time that depends upon where the person is in their sleep cycle). Our dataset included users who elected to use the traditional snooze feature (hereafter simply termed ‘snooze alarm’) as opposed to the smart snooze feature, logged sleep sessions 50% or more of the nights in each month of the monitoring interval; used the app on an iPhone as opposed to Android device; and consented for their data to be used in research. We obtained sleep recordings from 21,222 unique users between July 1, 2022 and December 31, 2022. Finally, we selected sleep sessions that lasted 4 h or longer. Our final dataset included 3,017,276 sleep sessions.
Snooze alarm
After the original alarm goes off a user may elect to either turn the alarm off or hit the snooze alarm. A snooze alarm lasting 5 min in duration is the default setting on this app, but users may elect a different snooze duration of their choosing in the app settings. In our dataset, a snooze alarm duration of 5 min is by far the most common (89% of sessions ending with snooze), followed by 10 min (4% of sessions ending with snooze). A user that turned off their first alarm and did not elect to snooze would have no snooze sessions recorded for that day. If, however, a user elected to snooze, the number of snooze alarms and total minutes spent snoozing would be recorded. It is possible that a user terminates the snooze alarm before the snooze alarm goes off, in which case, the amount of time spent snoozing would be captured (which would be less than the default snooze alarm duration). We obtained data detailing the number of times users elected to snooze and the duration of snoozing following each sleep session.
We created three categories out of the sample for sub-analyses of: light, moderate, and heavy snooze alarm users. We defined heavy snooze alarm use as those with more than 80% of sleep sessions ending with a snooze alarm, moderate users as those with 40–60% of sessions ending with a snooze alarm, and light snooze alarm users as those with fewer than 20% of sessions ending with snooze alarm.
Sleep
We obtained data detailing each sleep session for users. Specifically, we collected sleep and wake timing for each sleep session. Sleep and wake times were derived from user actions. Specifically, when a user opens the app they are prompted to press ‘Start’ when they want to start trying to fall asleep. We defined ‘sleep time’ as the user action (pressing ‘Start’). We defined ‘wake time’ as the original alarm that wakes the user. We also obtained ‘sleep duration’ from SleepCycle, which is calculated as the difference between the above-defined sleep and wake times. Snoozing is not included in the sleep duration estimate for each sleep session. We computed a measure of sleep time variability, which is the consistency or inconsistency of sleep times, using the times provided by SleepCycle26.
Statistical analysis
We visualized snooze alarm use in the month of October using raster plots to explore patterns of use across a typical month by selecting 500 users at random in the month of October. We created raster plots for 12 randomly selected users to visually display sleep and snooze alarm use per user in the month of October in light, moderate, and heavy snooze categories.
We calculated average snooze alarm use per person. In order to account for repeated observations per person in the dataset, we extract an average and confidence interval for each user by bootstrapping the distribution of averages across users. We examined average snooze behavior by day of the week using ANOVA. We examine differences in snooze behavior by gender using an independent samples t-test to obtain a Cohen’s D statistic. We define a Cohen’s D of 0.2 to be a small effect, 0.5 to be a medium effect, and 0.8 or higher to be a large effect27. Next, we explored differences in snooze alarm use by sleep duration using ANOVA. Finally, we explored snooze alarm behavior, sleep/wake timing, and sleep time variability. Analyses of snooze behavior by sleep duration were limited to sleep sessions longer than 4 h, to avoid including naps in our analysis. For sleep duration analyses, we explored snooze behavior between sleep durations of the same hour from :00 to :99. For instance, we categorized sleep durations lasting between 4.00 h and 4.99 h as “4 hours.”
Finally, we computed the relationship between snooze alarm use and sleep time variability. Sleep variability was computed by calculating a z-score for the sleep timing of each session. Specifically, we subtracted the sleep time for each session from the average sleep time per user, then divided by the standard deviation of the average sleep time per user26. We plotted this measure of sleep timing variability by snooze alarm utilization to visualize the relationship between sleep timing variability and snooze alarm utilization.
Data availability
Original files were obtained from SleepCycle through Daniel Sääf (Previous Data Analyst at SleepCycle). Data are not publicly available. All requests should be made to the corresponding author (Dr. Robbins; rrobbins4@bwh.harvard.edu).
References
Borbély, A. A. A two process model of sleep regulation. Hum. Neurobiol. (1982).
Borbély, A. The two-process model of sleep regulation: beginnings and outlook. J. Sleep. Res. 31, e13598 (2022).
Liu, Y. Prevalence of healthy sleep duration among adults—United States, 2014. MMWR. Morbidity and mortality weekly report 65, (2016).
Stranges, S., Tigbe, W., Gómez-Olivé, F. X., Thorogood, M. & Kandala, N. B. Sleep problems: an emerging global epidemic?? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep 35, 1173–1181 (2012).
Becker, N. B., Jesus, S. N., João, K. A. D. R., Viseu, J. N. & Martins, R. I. S. Depression and sleep quality in older adults: a meta-analysis. Psychol. Health Med. 22, 889–895 (2017).
Lopresti, A. L., Hood, S. D. & Drummond, P. D. A review of lifestyle factors that contribute to important pathways associated with major depression: diet, sleep and exercise. J. Affect. Disord. 148, 12–27 (2013).
Minkel, J. D. et al. Sleep quality and neural circuit function supporting emotion regulation. Biol. Mood Anxiety Disord. 2, 22 (2012).
Buxton, O. M. & Marcelli, E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the united States. Soc. Sci. Med. 71, 1027–1036 (2010).
Gangwisch, J. E. et al. Short sleep duration as a risk factor for hypertension. Hypertension 47, 833–839 (2006).
Anothaisintawee, T., Reutrakul, S., Van Cauter, E. & Thakkinstian, A. Sleep disturbances compared to traditional risk factors for diabetes development: systematic review and meta-analysis. Sleep. Med. Rev. 30, 11–24 (2016).
Huang, T., Mariani, S. & Redline, S. Sleep irregularity and risk of cardiovascular events: the Multi-Ethnic study of atherosclerosis. J. Am. Coll. Cardiol. 75, 991–999 (2020).
Robbins, R. et al. Examining sleep deficiency and disturbance and their risk for incident dementia and all-cause mortality in older adults across 5 years in the united States. Aging (Albany NY). 13, 3254–3268 (2021).
Bubu, O. M. et al. Sleep, Cognitive impairment, and Alzheimer’s disease: A systematic review and Meta-Analysis. Sleep 40, (2017).
Hafner, M., Stepanek, M., Taylor, J., Troxel, W. M. & Van Stolk, C. Why sleep matters — the economic costs of insufficient sleep. (2016). https://www.rand.org/pubs/research_reports/RR1791.html
Mattingly, S. M., Martinez, G., Young, J., Cain, M. K. & Striegel, A. Snoozing: an examination of a common method of waking. Sleep 45, zsac184 (2022).
Robbins, R. et al. Sleep Myths: an expert-led study to identify false beliefs about sleep that impinge upon population sleep health practices. Sleep. Health. 5, 409–417 (2019).
Sundelin, T., Landry, S. & Axelsson, J. Is snoozing losing? Why intermittent morning alarms are used and how they affect sleep, cognition, cortisol, and mood. J. Sleep. Res. e14054 https://doi.org/10.1111/jsr.14054 (2023).
Ogawa, K., Kaizuma-Ueyama, E. & Hayashi, M. Effects of using a snooze alarm on sleep inertia after morning awakening. J. Physiol. Anthropol. 41, 43 (2022).
Smith, B. V. & Blagrove, M. Lucid dreaming frequency and alarm clock snooze button use. Dreaming 25, 291–299 (2015).
Zeng, L. N. et al. Gender difference in the prevalence of insomnia: A Meta-Analysis of observational studies. Front. Psychiatry 11, (2020).
Jolly, S. et al. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann. Intern. Med. 160, 344–353 (2014).
Czeisler, M. É. et al. Sleep and mental health among unpaid caregivers of children, adults, and both: united States, 2022. Sleep. Health. 10, S201–S207 (2024).
Lee, H. J., Rex, K. M., Nievergelt, C. M., Kelsoe, J. R. & Kripke, D. F. Delayed sleep phase syndrome is related to seasonal affective disorder. J. Affect. Disord. 133, 573–579 (2011).
Robbins, R. et al. Four-Year trends in sleep duration and quality: A longitudinal study using data from a commercially available sleep tracker. J. Med. Internet. Res. 22, e14735 (2020).
Robbins, R. et al. Self-reported sleep duration and timing: A methodological review of event definitions, context, and timeframe of related questions. Sleep. Epidemiol. 1, 100016 (2021).
Kobayashi, D. et al. High sleep duration variability is an independent risk factor for weight gain. Sleep. Breath. 17, 167–172 (2013).
Cohen, J. A power primer. Psychol. Bull. 112, 155 (1992).
Acknowledgements
We acknowledge input to discussions regarding this manuscript from Jason Patrick Sullivan and Dr. Laura Barger.
Author information
Authors and Affiliations
Contributions
Drs. Robbins, Weaver Quan, Saaf, Gradisar, and Czeisler all conceptualized the analysis. Dr. Robbins prepared the manuscript and provided high level leadership on the project. Dr. Sääf led the analysis for the paper. All authors critically reviewed and critiqued the manuscript. Drs. Robbins, Weaver Quan, Saaf, Gradisar, and Czeisler approved the final version.
Corresponding author
Ethics declarations
Competing interests
Dr. Robbins reports consulting fees from Oura Ring Ltd., Savoir Beds Ltd., byNacht GmbH, Hilton Hotels International, Sonesta Hotels International, The Institute for Healthier Living Abu Dhabi. Dr. Robbins is on the Medical Advisory Board to Oura Ring, Equinox Fitness Clubs, and Somnum Pharmaceuticals. Dr. Czeisler reports grants and/or contracts from American Academy of Sleep Medicine Foundation, Axsome Therapeutics, CDC Foundation, Delta Airlines, Guidehouse, Inc., Jazz Pharmaceuticals PLC Inc, Puget Sound Pilots, Federal Aviation Administration, Lusome, Ouraring Inc, Sonesta Hotels International and Sutter Health/Eli Lilly during the conduct of the study; reports personal fees from Axsome Therapeutics, Institute of Digital Media and Child Development, National Sleep Foundation, Vanda Pharmaceuticals Inc, and With Deep, Inc, during the conduct of the study; reports research/education support to Brigham and Women’s Hospital from Apnimed, Inc., Avadel Pharmaceuticals, Casey Feldman Foundation, DR Capital, Eisai Co., LTD, f.lux Software, LLC, Idorsia Pharmaceuticals LTD, Mary Ann & Stanley Snider via Combined Jewish Philanthropies, Harmony Biosciences LLC, Jazz Pharmaceuticals PLC, Inc, Johnson & Johnson, NeuroCare, Inc., Optum, Peter Brown and Margaret Hamburg, Philips Respironics Inc, Regional Home Care, ResMed Foundation, Sleep Number Corp., Stuart F. and Diana L. Quan Charitable Fund, Summus, Inc., Takeda Pharmaceutical Co., LTD, ResMed, Sanofi, Philips, Vanda Pharmaceuticals and Whoop, Inc. during the conduct of the study; and is the incumbent of an endowed professorship provided to Harvard University by Cephalon Inc. during the conduct of the study; report serving as an expert witness for Adam Davis Law Firm; City of San Francisco; Cloward Trial Lawyers, Covington and Burling LLP; Haglund Kelley LLP; Law Offices of James L Mitchell; Law Office of Yolanda Huang; Paul Byrd Law Firm PLLC; Paul, Weiss, Rifkind, Wharton & Garrison LLP; Perdue & Kidd; Shaked Law Firm PA; Rabb and Rabb PLLC; Reyes Law Firm; Smith LaCien LLP; Stephens Law Firm; and Zehl & Associates, PC, in legal cases, including those involving Advanced Power Technologies, Aegis Chemical Solutions LLC, Amtrak, C&J Energy Services, FedEx, Greyhound Lines, Inc., Harmony Biosciences LLC, Puget Sound Pilots, Steel Warehouse, Product & Logistics Services LLC, San Francisco Sheriff’s Department, Schlumberger Technology Corp., UPS, and Vanda Pharmaceuticals during the conduct of the study; reports having an equity interest in Vanda Pharmaceuticals, and Signos, Inc. during the conduct of the study; and reports receiving royalties from McGraw Hill and Philips Respironics for the Actiwatch-2 and Actiwatch Spectrum devices during the conduct of the study. Dr. Czeisler’s interests were reviewed and are managed by the Brigham and Women’s Hospital and Mass General Brigham in accordance with their conflict-of-interest policies. Dr. Michael Gradisar is employed by SleepCycle. No other authors have competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Robbins, R., Sääf, D., Weaver, M.D. et al. Snooze alarm use in a global population of smartphone users. Sci Rep 15, 16942 (2025). https://doi.org/10.1038/s41598-025-99563-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-99563-y