Abstract
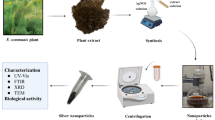
New strategies against antimicrobial resistance are urgently needed to address the challenges and health consequences posed by extensively drug-resistant (XDR) clinical isolates. This study explored how effective the green-synthesized silver nanoparticles alone or in combination with meropenem are in combating XDR Klebsiella pneumoniae. Klebsiella pneumoniae (K. pneumoniae) isolates were collected from several clinical labs and identified. After carrying out antimicrobial susceptibility testing, XDR isolates were selected for genotypic analysis using ERIC-PCR, and antibiotic resistance genes were identified. Silver nanoparticles (AgNPs) were synthesized using a Camellia sinensis (green tea) extract and characterized using UV-Vis spectroscopy, transmission electron microscopy (TEM), and X-ray diffraction (XRD). Particle size analysis was conducted to determine the physicochemical properties of the synthesized AgNPs. The AgNPs antibacterial effect alone or in combination with meropenem was carried out using the agar-well diffusion method, and the minimum inhibitory concentration (MIC), multiple antibiotic resistance (MAR) index and fractional inhibitory concentration index (FICI) were determined. Of the collected isolates, 67 were identified as K. pneumoniae, and 92.5% were considered XDR. Results showed that 10 (14.9%) and 57 (85.1%) isolates exhibited MAR index from 0.58 to 0.74, and 0.79-1.00, respectively. Upon genotypic analysis, 29 isolates were selected for further studies based on their unique or significant clustering patterns. The synthesized AgNPs exhibited strong antimicrobial activity against XDR K. pneumoniae strains, with inhibition zones ranging from 10 mm to 25 mm. The MIC of AgNPs ranged from 336.17 to 672.35 µg/mL. The fractional inhibitory concentration index (FICI) proved enhanced antimicrobial activity with partial (34.5%) and complete synergistic (65.5%) effects in the tested 29 nonclonal clinical isolates when AgNPs were combined with meropenem. In conclusion, a combination of AgNPs with meropenem is a useful alternative approach in combating XDR K. pneumoniae. Further studies are recommended for the use of this approach in clinical settings based on its benefits to enhance treatment outcomes.
Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article and supplementary file.
References
Herridge, W. P., Shibu, P., O’Shea, J., Brook, T. C. & Hoyles, L. Bacteriophages of Klebsiella spp., their diversity and potential therapeutic uses. J. Med. Microbiol. 69, 176–194 (2020).
Hamed, S. M. et al. Plasmid-mediated quinolone resistance in gram-negative pathogens isolated from cancer patients in Egypt. Microb. Drug Resistance 24, 785 (2018).
Al-Baz, A. A., Maarouf, A., Marei, A. & Abdallah, A. L. Prevalence and antibiotic resistance profiles of Carbapenem-Resistant Klebsiella pneumoniae isolated from tertiary care Hospital, Egypt. Egypt. J. Hosp. Med. 88, 2883–2890 (2022).
Choby, J. E., Howard-Anderson, J. & Weiss, D. S. Hypervirulent Klebsiella pneumoniae – clinical and molecular perspectives. J. Intern. Med. 287, 283–300 (2020).
Russo, T. A. & Marr, C. M. Hypervirulent Klebsiella pneumoniae. Clin. Microbiol. Rev. 32, 785 (2019).
Emam, S. M., Abdelrahman, S., Hasan, A. A. & Melouk, E. L. M. S. Hypervirulent Klebsiella pneumoniae at Benha university hospitals. Egypt. J. Hosp. Med. 90, 3592–3597 (2023).
Li, Y. & Ni, M. Regulation of biofilm formation in Klebsiella pneumoniae. Front. Microbiol. 14, 963 (2023).
Li, Y., Kumar, S. & Zhang, L. Mechanisms of antibiotic resistance and developments in therapeutic strategies to combat Klebsiella pneumoniae infection. Infect. Drug Resist. 17, 1107–1119 (2024).
Abdelaziz, S. M., Aboshanab, K. M., Yahia, I. S. & Yassien, M. A. & Hassouna, N. A. Correlation between the antibiotic resistance genes and susceptibility to antibiotics among the carbapenem-resistant gram-negative pathogens. Antibiotics 10, 785 (2021).
Poerio, N. et al. Fighting MDR-Klebsiella pneumoniae infections by a combined Host- and Pathogen-Directed therapeutic approach. Front. Immunol. 13, 963 (2022).
Chang, D., Sharma, L., Cruz, D. & Zhang, D. C. S. Clinical epidemiology, risk Factors, and control strategies of Klebsiella pneumoniae infection. Front. Microbiol. 12, 632 (2021).
Kamel, N. A., El-Tayeb, W. N., El-Ansary, M. R., Mansour, M. T. & Aboshanab, K. M. XDR-Klebsiella pneumoniae isolates harboring blaOXA-48: in vitro and in vivo evaluation using a murine thigh-infection model. Exp. Biol. Med. 244, 789 (2019).
Mabrouk, S. S., Abdellatif, G. R., Zaid, A. S. A. & Aboshanab, K. M. Propranolol restores susceptibility of XDR Gram-negative pathogens to meropenem and meropenem combination has been evaluated with either Tigecycline or Amikacin. BMC Microbiol. 23, 859 (2023).
Sheu, C. C., Chang, Y. T., Lin, S. Y., Chen, Y. H. & Hsueh, P. R. Infections caused by Carbapenem-Resistant enterobacteriaceae: an update on therapeutic options. Front. Microbiol. 10, 896 (2019).
Chen, Y. et al. Combination therapy for OXA-48 Carbapenemase-Producing Klebsiella pneumoniae bloodstream infections in premature infant: a case report and literature review. Infect. Drug Resist. 17, 1987–1997 (2024).
El-Sayed, S. E., Abdelaziz, N. A., El-Housseiny, G. S. & Aboshanab, K. M. Octadecyl 3-(3, 5-di-tert-butyl-4-hydroxyphenyl) propanoate, an antifungal metabolite of alcaligenes faecalis strain MT332429 optimized through response surface methodology. Appl. Microbiol. Biotechnol. 104, 7856 (2020).
Dutescu, I. A. & Hillier, S. A. Encouraging the development of new antibiotics: are financial incentives the right way forward? A systematic review and case study. Infect. Drug Resist. 14, 415–434 (2021).
Vivas, R., Barbosa, A. A. T., Dolabela, S. S. & Jain, S. Multidrug-Resistant bacteria and alternative methods to control them: an overview. Microb. Drug Resist. 25, 890–908 (2019).
Hetta, H. F. et al. Nanotechnology as a promising approach to combat multidrug resistant bacteria: a comprehensive review and future perspectives. Biomedicines 11, 413 (2023).
Hasan, W. L., Sari, R. & Hendradi, E. Green synthesis of antimicrobial silver nanoparticles using green tea extract: the role of concentration and pH. Jurnal Sains Farmasi Klinis. 11, 25–31 (2024).
Shokry, S. et al. Phytoestrogen β-Sitosterol exhibits potent in vitro antiviral activity against influenza A viruses. Vaccines (Basel) 11, 7856 (2023).
Mohamed Hassan, N., Badawy Dawood, A., mohamed, M., Sayed, S. A. & Mohamed, D. Distribution, characterization and antibiotic resistance of hypervirulent Klebsiella pneumoniae (hvKp) strains versus classical strains(CKp) causing healthcare associated infections in Sohag university hospitals. Microbes Infect. Dis. 2024, 256 (2024).
Miller, J. H. Experiments in Molecular Genetics (Cold Spring Harbor Laboratory, 1972).
CLSI. Performance standards for antimicrobial susceptibility testing. Clinical and Laboratory Standards Institute 2021. vol. M100-Ed31 (2021).
Magiorakos, A. P. et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 18, 268–281 (2012).
Krumperman, P. H. Multiple antibiotic resistance indexing of Escherichia coli to identify high-risk sources of fecal contamination of foods. Appl. Environ. Microbiol. 46, 165–170 (1983).
Versalovic, J., Koeuth, T. & Lupski, R. Distribution of repetitive DNA sequences in eubacteria and application to finerpriting of bacterial Enomes. Nucleic Acids Res. 19, 6823–6831 (1991).
Everitt, B. S., Landau, S., Leese, M. & Stahl, D. Cluster Analysis (Wiley, 2011). https://doi.org/10.1002/9780470977811.
Xia, Y., Liang, Z., Su, X. & Xiong, Y. Characterization of carbapenemase genes in Enterobacteriaceae species exhibiting decreased susceptibility to carbapenems in a university hospital in Chongqing, China. Ann. Lab. Med. 32, 270–275 (2012).
Colom, K. et al. Simple and reliable multiplex PCR assay for detection of blaTEM, BlaSHV and blaOXA-1 genes in Enterobacteriaceae. FEMS Microbiol. Lett. 223, 147–151 (2003).
Archambault, M. et al. Molecular characterization and occurrence of Extended-Spectrum β -Lactamase resistance genes among Salmonella enterica serovar corvallis from Thailand, Bulgaria, and Denmark. Microb. Drug Resist. 12, 192–198 (2006).
Du, J. et al. Phenotypic and molecular characterization of multidrug resistant Klebsiella pneumoniae isolated from a university teaching Hospital, China. PLoS One. 9, e95181 (2014).
Hatrongjit, R., Chopjitt, P., Boueroy, P. & Kerdsin, A. Multiplex PCR detection of common carbapenemase genes and identification of clinically relevant Escherichia coli and Klebsiella pneumoniae complex. Antibiotics 12, 76 (2022).
Park, C. H., Robicsek, A., Jacoby, G. A., Sahm, D. & Hooper, D. C. Prevalence in the united States of aac(6 ′) - Ib - cr encoding a Ciprofloxacin-Modifying enzyme. Antimicrob. Agents Chemother. 50, 3953–3955 (2006).
Ali, S. et al. Green synthesis of silver nanoparticles from camellia sinensis and its antimicrobial and antibiofilm effect against clinical isolates. Materials 15, 6978 (2022).
Rodrigues, A. S. et al. Advances in silver nanoparticles: a comprehensive review on their potential as antimicrobial agents and their mechanisms of action elucidated by proteomics. Front. Microbiol. 15, 8963 (2024).
Shehata, S., Elkholy, Y. N., Hussien, M. S. A., Yahia, I. S. & Aboshanab, K. M. Antibacterial, antibiofilm and cytotoxic activity of synthesized metal-incorporated mesoporous silica nanoparticles. AMB Express. 15, 130 (2025).
Khalil, M. A., El-Shanshoury, A. E. R. R., Alghamdi, M. A., Sun, J. & Ali, S. S. Streptomyces catenulae as a novel marine actinobacterium mediated silver nanoparticles: characterization, biological activities, and proposed mechanism of antibacterial action. Front. Microbiol. 13, 896 (2022).
Lopez-Carrizales, M. et al. In vitro synergism of silver nanoparticles with antibiotics as an alternative treatment in multiresistant uropathogens. Antibiotics 7, 50 (2018).
Taha, M. S. et al. Genotypic characterization of Carbapenem-Resistant Klebsiella pneumoniae isolated from an Egyptian university hospital. Pathogens 12, 121 (2023).
Hassuna, N. A., AbdelAziz, R. A., Zakaria, A. & Abdelhakeem, M. Extensively-Drug resistant Klebsiella pneumoniae recovered from neonatal sepsis cases from a major NICU in Egypt. Front. Microbiol. 11, 4526 (2020).
Attia, N., El-Ghazzawi, E., Elkhwsky, F., Metwally, D. & Ramadan, A. Klebsiella pneumoniae isolated from an Egyptian pediatric hospital: Prevalence, antibiotic resistance, biofilm formation, and genotyping. Microbes Infect. Dis. 2023, 1423 (2023).
Osama, D., El-Mahallawy, H., Mansour, M. T., Hashem, A. & Attia, A. S. Molecular characterization of Carbapenemase-Producing Klebsiella pneumoniae isolated from Egyptian pediatric cancer patients including a strain with a rare Gene-Combination of β-Lactamases. Infect. Drug Resist. 14, 335–348 (2021).
Shehab El-Din, E. M. R., El-Sokkary, M. M. A., Bassiouny, M. R. & Hassan, R. Epidemiology of neonatal sepsis and implicated pathogens: a study from Egypt. Biomed. Res. Int. 2015, 1–11 (2015).
Maleki, N., Tahanasab, Z., Mobasherizadeh, S., Rezaei, A. & Faghri, J. Prevalence of CTX-M and TEM β-lactamases in Klebsiella pneumoniae isolates from patients with urinary tract Infection, Al-Zahra Hospital, Isfahan, Iran. Adv. Biomed. Res. 7, 7859 (2018).
Moosavian, M. & Emam, N. The first report of emerging mobilized colistin-resistance Mcr genes and ERIC-PCR typing in Escherichia coli and Klebsiella pneumoniae clinical isolates in Southwest Iran. Infect. Drug Resist. 12, 1001–1010 (2019).
Parsaie Mehr, V., Shokoohizadeh, L., Mirzaee, M. & Savari, M. Molecular typing of Klebsiella pneumoniae isolates by enterobacterial repetitive intergenic consensus (ERIC)-PCR. Infect. Epidemiol. Microbiol. 3, 112–116 (2017).
Ferreira, R. L. et al. High prevalence of Multidrug-Resistant Klebsiella pneumoniae harboring several virulence and β-Lactamase encoding genes in a Brazilian intensive care unit. Front. Microbiol. 9, 8569 (2019).
Zafer, M. M., Bastawisie, E., Wassef, M. M., Hussein, M., Ramadan, M. A. & A. F. & Epidemiological features of nosocomial Klebsiella Pneumoniae: virulence and resistance determinants. Future Microbiol. 17, 27–40 (2022).
Hussein, N. H., Kareem, F., Hussein, S., AL-Kakei, S. N. & Taha, B. M. The predominance of Klebsiella pneumoniae carbapenemase (KPC-type) gene among high-level carbapenem-resistant Klebsiella pneumoniae isolates in Baghdad, Iraq. Mol. Biol. Rep. 49, 4653–4658 (2022).
Raheel, A., Azab, H., Hessam, W., Abbadi, S. & Ezzat, A. Detection of carbapenemase enzymes and genes among carbapenem-resistant Enterobacteriaceae isolates in Suez Canal university hospitals in Ismailia, Egypt. Microbes Infect. Dis. 1, 24–33 (2020).
Rai, M. K., Deshmukh, S. D., Ingle, A. P. & Gade, A. K. Silver nanoparticles: the powerful nanoweapon against multidrug-resistant bacteria. J. Appl. Microbiol. 112, 841–852 (2012).
Morgan, R. N. & Aboshanab, K. M. Green biologically synthesized metal nanoparticles: biological applications, optimizations and future prospects. Future Sci. OA 10, 8569 (2024).
El-Housseiny, G. S., Aboulwafa, M. M. & Aboshanab, K. A. & Hassouna, N. A. H. Optimization of rhamnolipid production by P. aeruginosa isolate P6. J. Surfactants Deterg. 19, 14523 (2016).
Huq, M. A., Ashrafudoulla, M., Rahman, M. M., Balusamy, S. R. & Akter, S. Green synthesis and potential antibacterial applications of bioactive silver nanoparticles: a review. Polym. (Basel). 14, 742 (2022).
Abada, E., Mashraqi, A., Modafer, Y., Al Abboud, M. A. & El-Shabasy, A. Review green synthesis of silver nanoparticles by using plant extracts and their antimicrobial activity. Saudi J. Biol. Sci. 31, 103877 (2024).
Dash, S. S., Samanta, S., Dey, S., Giri, B. & Dash, S. K. Rapid green synthesis of biogenic silver nanoparticles using cinnamomum Tamala leaf extract and its potential antimicrobial application against clinically isolated Multidrug-Resistant bacterial strains. Biol. Trace Elem. Res. 198, 681–696 (2020).
Mekky, A., Farrag, A., Sofy, A. & Hamed, A. Antibacterial and antifungal activity of Green-synthesized silver nanoparticles using Spinacia Oleracea leaves extract. Egypt. J. Chem. 0, 0–0 (2021).
Ahmed, T., Ogulata, R. T. & Gülnaz, O. Multifarious uses of UV-VIS spectroscopy for green synthesis of silver nanoparticles for antibacterial textiles. Text. Leather Rev. 7, 176–202 (2024).
Elsaid, E., Ahmed, O., Abdo, A. & Abdel Salam, S. Antimicrobial and antibiofilm effect of silver nanoparticles on clinical isolates of multidrug resistant Klebsiella pneumoniae. Microbes Infect. Dis. 0, 0–0 (2023).
Mogole, L., Omwoyo, W., Viljoen, E. & Moloto, M. Green synthesis of silver nanoparticles using aqueous extract of Citrus sinensis peels and evaluation of their antibacterial efficacy. Green. Process. Synthesis. 10, 851–859 (2021).
Nishibuchi, M., Chieng, Nishibuchi, M. & Loo, Y. Y. Synthesis of silver nanoparticles by using tea leaf extract from camellia sinensis. Int. J. Nanomed. 2012, 4263. https://doi.org/10.2147/IJN.S33344 (2012).
Mariselvam, R. et al. Green synthesis of silver nanoparticles from the extract of the inflorescence of Cocos nucifera (Family: Arecaceae) for enhanced antibacterial activity. Spectrochim. Acta Mol. Biomol. Spectrosc. 129, 537–541 (2014).
Logeswari, P., Silambarasan, S. & Abraham, J. Synthesis of silver nanoparticles using plants extract and analysis of their antimicrobial property. J. Saudi Chem. Soc. 19, 311–317 (2015).
Jemal, K., Sandeep, B. V. & Pola, S. Synthesis characterization, and evaluation of the antibacterial activity of Allophylus serratus leaf and leaf derived callus extracts mediated silver nanoparticles. J. Nanomater. 2017, 1–11 (2017).
Desouky, E., Shalaby, M., Gohar, M. & Gerges, M. Evaluation of antibacterial activity of silver nanoparticles against multidrug-resistant gram negative bacilli clinical isolates from Zagazig university hospitals. Microbes Infect. Dis. 1, 15–23 (2020).
Haji, S. H., Ali, F. A. & Aka, S. T. H. Synergistic antibacterial activity of silver nanoparticles biosynthesized by carbapenem-resistant Gram-negative bacilli. Sci. Rep. 12, 15254 (2022).
Acknowledgements
The authors would like to acknowledge the open-access funding provided by the Science, Technology & Innovation Funding Authority (STDF) in cooperation with the Egyptian Knowledge Bank (EKB) and Springer Nature’s transformative agreement.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
Conceptualization, EME, EH, GSH, and KMA; methodology, EME, and EH; validation, E GSH, and KMA; analysis, GSH, and KMA; investigation, EME, EH, GSH, and KMA; writing-original draft preparation, EME, and EH; writing-review and editing, GSH, and KMA; supervision, EH, GSH, and KMA. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was approved by the Faculty of Pharmacy, Ain Shams University Research Ethics Committee (ACUC-FP-ASU RHDIRB2020110301, REC# 402), with the waiving of the patient consent since there was no patient contact and the isolates were obtained from unidentified clinical specimens discharged from the general microbiology diagnostic laboratory of the hospital. All methods were performed in accordance with the Declaration of Helsinki. https://www.wma.net/policies-post/wma-declaration-of-helsinki/.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elmasry, E.M., Hegazy, E., El-Housseiny, G.S. et al. Camellia sinensis-synthesized silver nanoparticles and meropenem combination against extensively drug-resistant Klebsiella pneumoniae. Sci Rep (2026). https://doi.org/10.1038/s41598-026-38375-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-38375-0