Abstract
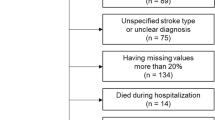
Dysphagia is a common and debilitating complication in patients with lateral medullary infarction (LMI), affecting up to 100% of cases and significantly impairing quality of life. Accurate classification of early dysphagia severity is essential for timely intervention and personalized rehabilitation planning. This study aimed to develop and validate a deep learning algorithm using acute-phase diffusion-weighted MRI to classify dysphagia severity in LMI patients. A retrospective cohort of 163 patients with confirmed acute LMI was analyzed. Dysphagia severity was determined by videofluoroscopic swallowing studies (VFSS), categorizing patients into severe and non-severe groups. Lesion regions were manually labeled and preprocessed for model training. Transformer-based deep learning architecture, the Hierarchical Vision Transformer (Hier-ViT), was employed due to its capacity to model spatial hierarchies and global image context. The model achieved an accuracy of 0.85, with a precision of 0.70, recall of 0.75, F1-score of 0.72, and an area under the ROC curve (AUC) of 0.69. These findings suggest that Hier-ViT can effectively classify dysphagia severity in LMI patients using early MRI, offering a potential tool for early risk stratification. While the model shows a high accuracy, the modest AUC suggests that further refinement and multi-modal integration are necessary to improve its discriminative power in imbalanced clinical datasets.
Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Barer, D. The natural history and functional consequences of dysphagia after hemispheric stroke. J. Neurol. Neurosurg. Psychiatry. 52, 236–241 (1989).
Clavé, P. & Shaker, R. Dysphagia: current reality and scope of the problem. Nat. Reviews Gastroenterol. Hepatol. 12, 259–270 (2015).
Ekberg, O., Hamdy, S., Woisard, V., Wuttge–Hannig, A. & Ortega, P. Social and psychological burden of dysphagia: its impact on diagnosis and treatment. Dysphagia 17, 139–146 (2002).
Vuilleumier, P., Bogousslavsky, J. & Regli, F. Infarction of the lower brainstem: Clinical, aetiological and MRI-topographical correlations. Brain 118, 1013–1025 (1995).
Lee, H. & Sohn, C. H. Axial lateropulsion as a sole manifestation of lateral medullary infarction: a clinical variant related to rostral–dorsolateral lesion. Neurol. Res. 24, 773–774 (2002).
Dieterich, M. & Brandt, T. Wallenberg’s syndrome: lateropulsion, cyclorotation, and subjective visual vertical in thirty-six patients. Annals Neurology: Official J. Am. Neurol. Association Child. Neurol. Soc. 31, 399–408 (1992).
Nowak, D. A. & Topka, H. R. The clinical variability of Wallenberg’s syndrome: The anatomical correlate of ipsilateral axial lateropulsion. J. Neurol. 253, 507–511 (2006).
Norrving, B. & Cronqvist, S. Lateral medullary infarction: prognosis in an unselected series. Neurology 41, 244–244 (1991).
Sacco, R. L. et al. Wallenberg’s lateral medullary syndrome: Clinical-magnetic resonance imaging correlations. Arch. Neurol. 50, 609–614 (1993).
Ertekin, C., Aydogdu, I., Tarlaci, S., Turman, A. B. & Kiylioglu, N. Mechanisms of dysphagia in suprabulbar palsy with lacunar infarct. Stroke 31, 1370–1376 (2000).
Steuer, I. & Guertin, P. A. Central pattern generators in the brainstem and spinal cord: an overview of basic principles, similarities and differences. Rev. Neurosci. 30, 107–164 (2019).
Vigderman, A. M., Chavin, J. M., Kososky, C. & Tahmoush, A. J. Aphagia due to pharyngeal constrictor paresis from acute lateral medullary infarction. J. Neurol. Sci. 155, 208–210 (1998).
Car, A. Inputs to the swallowing medullary neurons from the peripheral afferent fibers and the swallowing cortical area. Brain Res. 178, 567–572 (1979).
Kim, T. J. et al. Dysphagia may be an independent marker of poor outcome in acute lateral medullary infarction. J. Clin. Neurol. 11, 349–357 (2015).
Kim, H., Chung, C. S., Lee, K. H. & Robbins, J. Aspiration subsequent to a pure medullary infarction: lesion sites, clinical variables, and outcome. Arch. Neurol. 57, 478–483 (2000).
Chun, M. H., Kim, D. & Chang, M. C. Comparison of dysphagia outcomes between rostral and caudal lateral medullary infarct patients. Int. J. Neurosci. 127, 965–970 (2017).
Gupta, H. & Banerjee, A. Recovery of dysphagia in lateral medullary stroke. Case Rep. Neurol. Med. 2014, 404871 (2014).
Kim, H., Lee, H. J. & Park, J. W. Clinical course and outcome in patients with severe dysphagia after lateral medullary syndrome. Ther. Adv. Neurol. Disord. 11, 1756286418759864 (2018).
Jang, S. H. & Kim, M. S. Dysphagia in lateral medullary syndrome: a narrative review. Dysphagia 36, 329–338 (2021).
Cho, Y. J., Ryu, W. S., Lee, H., Kim, D. E. & Park, J. W. Which factors affect the severity of dysphagia in lateral medullary infarction? Dysphagia 35, 414–418 (2020).
Miller, D. D. & Brown, E. W. Artificial intelligence in medical practice: the question to the answer? Am. J. Med. 131, 129–133 (2018).
LeCun, Y., Bengio, Y. & Hinton, G. Deep learning. nature 521, 436–444 (2015).
Lundervold, A. S. & Lundervold, A. An overview of deep learning in medical imaging focusing on MRI. Z. fuer medizinische Physik. 29, 102–127 (2019).
Islam, J. & Zhang, Y. Brain MRI analysis for Alzheimer’s disease diagnosis using an ensemble system of deep convolutional neural networks. Brain Inf. 5, 1–14 (2018).
Laukamp, K. R. et al. Fully automated detection and segmentation of meningiomas using deep learning on routine multiparametric MRI. Eur. Radiol. 29, 124–132 (2019).
Perkuhn, M. et al. Clinical evaluation of a multiparametric deep learning model for glioblastoma segmentation using heterogeneous magnetic resonance imaging data from clinical routine. Invest. Radiol. 53, 647–654 (2018).
Yoo, Y. et al. Deep learning of joint myelin and T1w MRI features in normal-appearing brain tissue to distinguish between multiple sclerosis patients and healthy controls. NeuroImage: Clin. 17, 169–178 (2018).
Kleesiek, J. et al. Deep MRI brain extraction: A 3D convolutional neural network for skull stripping. NeuroImage 129, 460–469 (2016).
Li, H., Parikh, N. A. & He, L. A novel transfer learning approach to enhance deep neural network classification of brain functional connectomes. Front. NeuroSci. 12, 491 (2018).
Liu, Z. et al. In Proceedings of the IEEE/CVF International Conference on Computer Vision. 10012–10022.
Cao, H. et al. In European Conference on Computer Vision. 205–218 (Springer).
Cantone, M., Marrocco, C., Tortorella, F. & Bria, A. Convolutional networks and transformers for mammography classification: an experimental study. Sensors 23, 1229 (2023).
Acknowledgements
We thank the Department of Medical Information at Dongguk University Ilsan Hospital for their support in accessing radiologic data.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT). (No. RS-2023-00252208)
Author information
Authors and Affiliations
Contributions
T.L. collected clinical and imaging data, performed data preprocessing and annotation, and drafted the manuscript. K.N. developed and implemented the deep learning model and contributed to data analysis. B.H.K. critically reviewed the manuscript and contributed to overall interpretation. J.-W.P. conceptualized and supervised the study, provided critical revisions, and served as corresponding author. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Consent to participate/consent to publish
Informed consent was waived by the IRB due to the retrospective nature of the study using de-identified patient data.
Ethics approval
This study was approved by the Institutional Review Board of Dongguk University Ilsan Hospital (IRB No. 2024-07-004). All methods were carried out in accordance with relevant guidelines and regulations.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, T., Kim, B.H., Nam, K. et al. Classification of dysphagia severity after lateral medullary infarction with deep learning. Sci Rep (2026). https://doi.org/10.1038/s41598-026-40751-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-40751-9