Abstract
Cognitive decline is a global health concern that leads to significant impairment in daily functioning and quality of life. Limited large-scale cohort studies have concurrently examined the effects of lifestyle and social factors on cognitive status and the potential gender and age cohort differences in middle-aged and older adults. This longitudinal study examined the temporal associations between lifestyle and social factors and cognitive status in middle-aged and older adults in the United States. The sample comprised 2192 individuals (mean age = 71.6 years, SD = 6.6) drawn from two waves of the National Social Life, Health, and Aging Project conducted in 2010–11 and 2015–16. Lifestyle factors (vigorous physical activity, cigarette smoking, alcohol drinking, and sleep quality) and social factors (number of close social ties, frequency of volunteering, participation in group meetings, informal socialization, and religious services) were measured in 2010–11. Cognitive status was assessed via the Chicago Cognitive Function Measure at both waves. Regression analysis examined the effects of lifestyle and social factors on cognitive status and its change across the two waves. Past smoking and current drinking showed significant and positive effects on cognitive status. Maintaining robust social connections and active attendance in formal and informal social activities were significant predictors of healthier changes in cognitive status for those with normal cognition or mild cognitive impairment. Subgroup analysis revealed gender and age cohort differences in the effects of lifestyle and social factors on cognitive status, with females showing stronger effects for lifestyle and social factors than males. The present findings underscored the predominant influence of social factors over lifestyle factors on cognitive status and provided a more nuanced understanding of the social and lifestyle determinants across gender and age groups. Further research should aim to explore the causal direction of these associations, considering specific cognitive domains and underlying mechanisms.
Similar content being viewed by others
Introduction
Cognitive function refers to functioning in an exhaustive framework of different cognitive domains such as memory, executive function, orientation, attention, and abstraction. Dementia is a global health concern characterized by the deterioration of cognitive status that leads to significant impairment in daily functioning and quality of life. In the United States (US), ~6.5 million individuals are currently living with Alzheimer’s disease (AD), the most prevalent form of dementia, highlighting the substantial public health burden of this disease (World Health Organization, 2021). Mild cognitive impairment (MCI) refers to subclinical deficits in cognitive status that do not yet meet the diagnostic criteria for dementia (Petersen et al. 1999). MCI is a transitional stage between normal aging and dementia (Anderson, 2019), with 10 to 15 percent of the population over the age of 65 being affected by it. Despite the potentially significant role of modifiable factors on cognitive health in later life (Barnes and Yaffe, 2011; Welberry et al. 2023), how these factors contribute to changes in cognitive status is not fully understood. It is essential to gain a deeper understanding of the factors that influence the change in cognitive status in individuals with MCI. Further work is needed to identify interventions on modifiable factors to alter the course of cognitive decline and delay the onset of dementia.
Numerous studies have explored non-genetic risk factors for dementia in later life (Yaffe et al. 2009; Zhang et al. 2023). Lifestyle factors, such as physical activity (PA), cigarette smoking, alcohol consumption, and sleep, have been extensively studied (Shimada et al. 2018). PA has shown positive effects on cognitive status by increasing blood flow to the brain to support optimal brain function (Lin et al. 2018; Mandolesi et al. 2018). Recent evidence suggests a more pronounced impact of moderate to vigorous PA on cognitive status than mild PA (Mitchell et al. 2023). The relationship between smoking and cognitive health in later life is multifaceted. Research has shown that smoking is a risk factor for dementia via damage to the cardiovascular system, heightened oxidative stress, inflammation, and accumulation of toxic substances in the brain (Almeida et al. 2011). These factors could harm neurons and contribute to cognitive decline and dementia (Livingston et al. 2020). However, previous studies have suggested the neuroprotective effects of nicotine in cigarettes in lowering the risk of dementia (Chang et al. 2014; Durazzo et al. 2014). The presence of ambivalent forces creates a challenging landscape for understanding the precise relationship between past smoking and dementia risk (Peters et al. 2008). The impact of past smoking on the likelihood of developing dementia remains uncertain.
Alcohol consumption shows an intricate relationship with cognitive status, and the relationship may be due to complicated changes in cerebral vasculature and structure in older adults (Mukamal et al. 2003). Previous studies have associated low to moderate levels of alcohol consumption with better cognitive status compared to never-drinkers in American older adults (Gross et al. 2011; Mukamal et al. 2003; Zanjani et al. 2013; Zhang et al. 2020). However, individuals with daily alcohol consumption showed significantly poorer phonemic fluency and neurocognitive status than less frequent drinkers (Gross et al. 2011; Woods et al. 2016). There is likely a non-linear relationship between alcohol consumption and cognitive status (Listabarth et al. 2022), which warrants further investigation. Sleep is crucial for cognitive status across the lifespan. Subjective sleep quality and longer sleep latency have been found to predict better cognitive status (Diem et al. 2016; van Oostrom et al. 2018). However, the temporal effect of self-reported sleep quality on cognitive performance in healthy or cognitively impaired older adults remains largely unknown.
To a lesser extent, research has explored the role of social factors on cognitive s in later life. Limited evidence suggests that maintaining close relationships and engaging in social activities can help preserve cognitive status and slow down cognitive decline in older adults (Paiva et al. 2023; Penninkilampi et al. 2018; Tang et al. 2018). Social factors encompass such activities as participating in social events, maintaining connections with family and friends, and engaging in meaningful social interactions (Zunzunegui et al. 2004). A recent study (Kang, 2024) has linked neighborhood social cohesion with better cognitive performance via psychological distress in older adults. The cognitive benefits derived from social factors can be attributed to cognitive stimulation and emotional resilience from the exercises inherent in social interactions. However, unanswered questions remain whether social factors enhance cognitive status or delay the onset of dementia, as well as the specific types of social activities that are most effective.
Limited large-scale cohort studies have concurrently examined the effects of lifestyle and social factors on cognitive status in middle-aged and older adults. Furthermore, no existing studies have explored the potential gender differences and age cohort differences in the effects of lifestyle and social factors. It is essential to examine gender and age differences in the effects of lifestyle and social factors on cognitive status for the following reasons. Regarding lifestyle factors, gender roles, and societal expectations could affect lifestyle factors such as PA and drinking behavior. Investigating the potential interactions between these factors and gender could yield insights into gender disparities in determinants of cognitive health. Regarding the social factors, there are potential gender discrepancies in the social support networks and communication styles and needs. Having a better understanding of the gender differences in the quantity of social networks and social engagement could elucidate the mechanisms through which social factors affect cognitive health in middle-aged and older adults. Recognizing the potential differential effects across demographic subgroups could lead to personalized healthcare policies to address the unique needs across gender and age cohorts, which could, in turn, inform customized preventive interventions to enhance the cognitive status and quality of life of different subgroups.
In view of the research gaps, the present study utilized data from a population-based cohort study to examine the associations between lifestyle social factors, and cognitive status. We also aimed to evaluate and compare the effects of lifestyle and social factors on cognitive status across gender and age cohorts. By identifying the risk or protective factors of cognitive status and its change in the whole sample and across demographic subgroups, our study would uncover deeper insights into the promotion and maintenance of cognitive health in aging populations.
Methods
Participants and procedures
The present longitudinal study utilized data from the second and third waves of the National Social Life, Health, and Aging Project (NSHAP). The NSHAP dataset is a longitudinal, population-based study that examines the health and social factors of 3005 non-institutionalized middle-aged and older adults aged 57–85 recruited in the US in 2005–2006 (Waite and Das, 2010). In the present study, the NSHAP dataset was selected because of the longitudinal nature, sample representativeness of both middle-aged and older adult populations in America, and its detailed measures on social relationships and social activities for examination of cognitive aging. The second wave of data collection took place in 2010–2011, followed by the third wave in 2015–2016. Data from the first wave were not included due to substantial revisions and enhancements made to the measurement of cognitive abilities starting from the second wave (O’Doherty et al. 2021). The inclusion criteria of the participants in this study were participation in both Wave 2 and Wave 3 of the NSHAP, aged 60 or above, and community-dwelling. Exclusion criteria of the study participants included missing information on cognitive scores, institutionalization in nursing homes or hospitals, and the presence of significant psychiatric conditions. The final analytical sample consisted of 2192 individuals who participated in both waves of the NSHAP.
Measures
Cognitive status was assessed in the NSHAP by the Chicago Cognitive Function Measure (CCFM) (Shega et al. 2014). The CCFM was a multidimensional test of cognition for the NSHAP participants. The CCFM was developed based on the Montreal Cognitive Assessment (MoCA) via a standard protocol for selecting items and improving their clarity. It was designed to differentiate between normal age-related cognitive changes, MCI, and dementia within aging populations. The CCFM was administered by non-medically trained interviewers using Computer Assisted Personal Interviewing in ~12 min (Dale et al. 2018). The CCFM evaluated the global cognitive status via eight cognitive domains: orientation, animal naming, executive function, visuospatial construction, memory, attention, language, and abstraction. The CCFM score was rescaled to the scoring range (0–30) of MoCA for consistency with previous studies (Dale et al. 2018), and higher scores indicated better cognitive status. The participants were classified into three groups based on the following criteria: normal cognitive status (CCFM score = 26–30), MCI (CCFM score = 21–25), and dementia (CCFM score = 0–20) (Dautzenberg et al. 2020).
In terms of lifestyle factors, vigorous PA refers to participation in activities such as sports, exercise classes, heavy housework, or a job that involves physical labor for 30 min or more. The frequency of vigorous PA was assessed on a 6-point format: 0 (never), 1 (<1 time per month), 2 (1–3 times per month), 3 (1–2 times per week), 4 (3–4 times per week), and 5 (5 or more times per week). This predictor was dichotomized into a binary variable on whether respondents reported at least 3 times vigorous PA per week. Smoking status was classified into three levels: 0 (never smoked), 1 (formerly smoked but no longer smoking), and 2 (current smoker). Alcohol consumption was divided into four levels: 0 (never drank), 1 (previously drank over the past 12 months but not currently), 2 (currently drinking fewer than four days per week), and 3 (currently drinking four or more days per week). Self-reported sleep quality was assessed based on the question, “how often do you feel rested in the morning?”. The response was categorized into three levels: 0 (never or rarely), 1 (sometimes), and 2 (most of the time).
In terms of social factors, strong social ties were determined by participants self-reporting the number of individuals they felt very or extremely close to. Furthermore, the social engagement of the participants was assessed by a series of questions on their involvement in various activities, such as (1) doing volunteer work for religious, charitable, political, health-related, or other organizations, (2) attending organized group meetings, (3) socializing with friends or relatives, and (4) attending religious services. Frequency of engagement in social activities was rated on seven levels: 0 (never), 1 (less than once a year), 2 (about once a year), 3 (several times a year), 4 (about once a month), 5 (every week), and 6 (several times a week).
The study controlled for six socio-demographic factors, including age (in years), gender (male vs. female), race/ethnicity (Whites, Blacks, Hispanics, Others), living arrangements (living alone, living with a spouse, or others), educational attainment (below high school, high school diploma, some college, bachelor’s degree or above), and annual household income (in US dollars) categorized into four groups: 0–24,999, 25,000–49,999, 50,000–99,999, and 100,000 or higher.
Statistical analysis
Preliminary analysis was conducted to obtain the descriptive statistics of the sample in terms of means and proportions of the socio-demographic variables, lifestyle factors, and social factors. Transition in cognitive status from 2010–2011 to 2015–2016 was summarized by a 3 × 3 transition matrix. To explore the effects of social and lifestyle factors on cognitive status and its change, we conducted two types of analysis. Firstly, we conducted an ordinary least square regression on the entire sample in SPSS version 28.0 to investigate the associations between lifestyle and social factors measured at baseline and the cognitive status at follow-up utilizing a longitudinal design. Secondly, we leveraged the longitudinal nature of the data to conduct logit regression modeling on three temporal changes in cognitive status: including normal to MCI/dementia (reference group: normal to normal), MCI to dementia (reference group: MCI to MCI/normal), and MCI to normal (reference group: MCI to MCI/dementia) between the two waves. Missing data on other variables were imputed based on age, gender, race/ethnicity, and education (Royston, 2004). The statistical significance level was set in the present study at p < 0.05 level.
The model configurations were consistent across all five sets of regressions. Model 1 focused on the influence of four lifestyle factors, namely vigorous PA, smoking behavior, alcohol consumption, and sleep quality. Models 2 through 6 delve into the effects of various social factors, including close social ties (Model 2), frequency of volunteer work (Model 3), frequency of attending group meetings (Model 4), frequency of socializing with family and friends (Model 5), and frequency of attending religious services (Model 6). We did not simultaneously enter all the social factors in a single model due to the severe multicollinearity concern (as confirmed by a sensitivity analysis). Age, gender, race and ethnicity, living arrangements, education, and household income were included as control variables in all the regression models to account for their potential confounding effects. Subgroup analysis was conducted to explore potential differences in the effects of lifestyle and social factors on cognitive outcomes across genders (males and females) and age cohorts (middle-aged adults aged 60–70 and older adults aged 71–90). The sample sizes of the normal cognition and MCI subgroups and four demographic subgroups ranged from 734 to 1374 and each of the Models 1–6 had at most 20 predictor variables. The sample size to predictor ratios were high (36.7–68.7) to ensure that the regression analyses in the study were sufficiently powered.
Results
Sample profile
Table 1 presents descriptive statistics for the sample. The sample had a mean age of 71.56 years (SD = 6.6; median = 70 years), with females comprising 55.02% of the sample. The majority of participants identified as White (72.90%) and lived with a spouse either alone or with others (72.45%). Around half of them held a college education level or higher (58.26%) and had an annual household income of at least $50,000 (46.53%). The mean CCFM score decreased from 25.32 in 2010–2011 to 24.52 in 2015–2016. About 28.74% of participants experienced qualitative changes in cognitive categories over 5 years. The majority (75.69%) of the cognitively normal participants remained in the normal group, and 24.31% of them transitioned to MCI or dementia. Of the MCI group, 64.03% of them (N = 470) stayed as MCI, 10.90% of them (N = 80) progressed to dementia, and 25.07% of them (N = 184) returned to normal cognition.
Around 20% of participants reported no regular vigorous PA. Past smokers constituted 45.16% of the sample, and around half of the participants were current alcohol drinkers (55.75%), with 15.60% consuming alcohol four or more days per week. Around 66.29% of participants reported feeling rested in the morning either sometimes or most of the time. As for social factors, most participants reported engaging in volunteering and attending group meetings anywhere from “about once or twice a year” to “several times a year.” The most prevalent frequency of attending religious service ranged from “several times a year” to “about once a month.”
Effects of lifestyle and social factors on cognitive status
Table 2 presents the findings from the whole-sample analysis on the temporal associations between lifestyle and social factors at baseline and total CCFM score at follow-up. In our regression models, most of the control variables, except for gender, had significant effects on the global cognitive status and its change. Older age and being Blacks or Hispanics (compared to whites) were significantly linked with worse cognitive status and deterioration in cognitive status. Regarding the socioeconomic factors, higher education level and household income were positively associated with cognitive status and negatively associated with deterioration in cognitive status. Among the lifestyle factors, past smoking, currently drinking less than four days per week, and currently drinking four or more days per week were significantly associated with better cognitive status. However, no significant associations were found for vigorous PA or sleep quality. Four out of the five social factors showed significant and positive correlations with cognitive status. In particular, having 10–20 close social ties, engaging in volunteer work several times a week, attending group meetings every week, and socializing with family and friends every week demonstrated the strongest effect on cognitive status.
Logistic regressions of transition in cognitive status groups from 2010–2011 to 2015–2016
Tables 3 through 5 present the results from a subgroup analysis, focusing on specific changes in cognitive status groups. In the Normal-MCI/Dementia transition (Table 3), attending group meetings every week (OR = 0.63, 95% CI = 0.42–0.97) and several times a week (OR = 0.58, 95% CI = 0.35–0.97) were significant protective factors, while lifestyle factors showed no significant effects. Current smoking showed a marginal association with higher odds of this undesirable transition (OR = 1.48, 95% CI = 0.95–2.33). In the MCI-Dementia transition (Table 4), past smoking emerged as the only significant lifestyle factor, exhibiting a negative (protective) effect (OR = 0.53, 95% CI = 0.29–0.95). Among social factors, having 4–9 close ties (OR = 0.38, 95% CI = 0.16–0.90) and attending group meetings several times a year (OR = 0.18, 95% CI = 0.04–0.77) or every week (OR = 0.29, 95% CI = 0.10–0.85) emerged as protective factors. For the MCI-Normal transition (Table 5), volunteering several times a year (OR = 1.87, 95% CI = 1.03–3.41) and attending group meetings every week (OR = 1.99, 95% CI = 1.10–3.59) were identified as beneficial factors. The key findings on significant exposure factors are summarized in Supplementary Table 1.
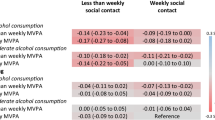
Subgroup analysis on effects of lifestyle and social factors on cognitive status
Supplementary Tables 2 and 3 report the effects of lifestyle and social factors on the cognitive outcomes in female and male respondents, respectively. The effects of age, race, living arrangement, and education were comparable across genders, and household income showed a stronger effect on cognitive status in males. For females, current drinking and four of the five social factors except for attending religious services were consistently and positively associated with better cognitive status. In contrast, these effects were comparatively weaker and non-significant in males, with volunteering once a year showing the only significant effect.
Supplementary Tables 4 and 5 report the effects of lifestyle and social factors on the cognitive outcomes in middle-aged (aged 60–70) and older respondents (aged 71–90), respectively. Most of the control variables showed comparable effects on cognitive status across age groups, except for a stronger negative effect of age on cognitive status in the older subgroup. Current drinking for at least four days per week was consistently associated with better cognitive status in both age groups. However, current smoking only showed a significant and negative effect on cognitive status in middle-aged adults. The number of close social ties only showed significant and positive effects in older adults but not in middle-aged adults.
Discussion
The present study systematically examined the temporal effects of lifestyle and social factors on global cognitive status and its change over a 5-year period. Our investigation pinpointed modifiable lifestyle and social factors that influenced cognition in later life and potentially decelerated the progression of dementia. Our investigation yielded interesting findings regarding lifestyle factors. Current smoking showed a detrimental effect on cognitive status in middle-aged adults aged 60–70. Ongoing smokers showed greater cognitive decline than never-smokers or quitters, with greater loss in gray matter over two years (Almeida et al. 2011). We found a beneficial effect of past smoking against the transition from MCI to dementia. These findings provide support for the cognitive enhancement effects of nicotine in normal aging and MCI groups (Chang et al. 2014; Durazzo et al. 2014). Our findings echoed recent findings on the health benefits of smoking cessation on a lower risk of dementia (Deal et al. 2020; Jeong et al. 2023).
Regardless of the frequency of drinking, the present study linked current drinking with better cognitive health but not with changes in cognitive status. This is consistent with the beneficial effects of moderate levels of alcohol intake on cognitive health (Gross et al. 2011; Mukamal et al. 2003). We observed a gradient relationship between alcohol consumption and cognitive status, with greater benefits observed in individuals who drank four or more days per week. The Mediterranean diet, which recommends a moderate intake of alcohol, has been associated with a lower risk of MCI and dementia (Frisardi et al. 2010). However, the NSHAP only assessed the frequency of drinking per week but not the actual amount of alcohol intake per day. Our present results could not differentiate between light, moderate, and heavy drinking. A network meta-analysis of 43 cohort studies (Liang et al. 2020) has found no smoking history, participation in physical exercise, and abstinence from drinking to be associated with lower risks of dementia. Our findings suggest the need for lifestyle intervention studies to modify the smoking and drinking behaviors in older adults with MCI.
Vigorous PA and sleep quality did not have any significant effects in the regression models. In separate analyses without controlling for education and income (not shown), vigorous PA showed a significant protective effect against transitioning from normal status to MCI or dementia. These suggest that the beneficial effect of PA on cognitive health could be confounded by socioeconomic status. The lack of a significant relationship between self-reported sleep quality and cognitive health across all model configurations is surprising. This finding contradicts the growing recognition that sleep quality leads to better cognitive performance (Noort et al. 2016; Sen and Tai, 2023; van Oostrom et al. 2018). Our results align with previous work reporting no association between sleep quality and cognitive performance in domains such as working memory, executive functions, and information processing (Miyata et al. 2013; Nebes et al. 2009; Zavecz et al. 2020). Additional research is needed to elucidate the complex relationship between sleep quality and cognitive status.
In terms of social factors, having four or more close social ties and attendance in group meetings were positively linked to cognitive scores after accounting for socio-demographic confounders. Different types of social factors showed varying roles in different cognitive outcomes. Consistent with previous literature (Crooks et al. 2008; Estrella et al. 2021; Holtzman et al. 2004), our results highlight the importance of engaging in various social activities to promote cognitive status. A recent NSHAP study found a longitudinal association between increased social isolation and anxiety symptoms over a 5-year period (Hwang et al. 2024). Among the nine lifestyle and social factors, weekly attendance in group meetings was the most consistent protective factor of improved cognitive status. Attending group meetings and participating in volunteer work involves social interaction and responsibilities, which likely tap into cognitive reserves and maintain cognitive sharpness through purposeful practice of attention and problem-solving to tackle complex tasks. Besides, these social roles could foster improved levels of self-confidence and self-esteem, which are linked with improved mood and better cognitive outcomes.
The present study found that around 25% of the individuals with MCI in Wave 2 returned to normal cognition in Wave 3. Our finding is consistent with the results of recent studies on MCI reversion, which suggest reversion rates from 20% to 48.3% in Swedish and Chinese samples. In particular, Overton et al. (2023) found that participants with regular alcohol consumption, living with someone, and lower body mass index showed a higher likelihood of reverting to normal cognition from MCI after 6–7 years. After controlling for education level, another recent study identified APOE4 allele, brain volume, neuropsychological test performance, and glomerular filtration rate as physiological and genetic predictors of reversion (Yu et al. 2024). To prevent cognitive decline and delay the onset of dementia, individuals with MCI may benefit from stronger social support networks within the communities. Specific activities, such as participating in hobbies and volunteering in community projects, have been shown to contribute to the reversal of MCI and support cognitive status (Shimada et al. 2019).
Implications
The present findings contributed to existing literature on cognitive aging by offering a more nuanced understanding of the social and lifestyle determinants. The present analysis was based on a large NSHAP dataset which was a longitudinal, population-based study of both middle-aged and older adults in America. The representativeness of the sample lent greater support to the external validity of the results. In comparison to lifestyle factors, our results highlight the greater protective role of social factors in promoting cognitive status in middle-aged and older adults. Besides, the sample diversity allowed an in-depth examination of the effects of lifestyle and social factors on cognitive status across gender and age groups. The subgroup analysis across genders showed that the beneficial effects of current drinking, number of close social ties, attending group meetings, and socializing with family and friends were only significant in females but not males. The stronger associations between the social factors and cognitive status of females in the present NSHAP sample are in line with and add to the findings of previous studies (Kotwal et al. 2016; Lee et al. 2020; Thomas, 2011). Future research could examine potential determinants of cognitive status in other domains such as the physiological, psychological, and environmental domains.
Apart from the gender differences, the present study also revealed interesting differences in the lifestyle and social determinants across age groups. For instance, the detrimental effect of current smoking was only significant in middle-aged adults. The number of close social ties showed a stronger effect on cognitive status in older adults. On the one hand, volunteering, attending group meetings, and socializing with families and friends all showed significant effects on cognitive status in both age groups. On the other hand, the beneficial effects of these social factors manifested in lower frequency (about once a year or several times a year) for middle-aged adults, while a higher frequency (every week or several times a week) of these social activities is required for older adults. An ecological momentary assessment study (Zhaoyang et al. 2018) found age differences in adults’ daily social interactions, with middle-aged adults reporting lower positive ratings in daily social interaction quality and older adults reporting lower negative ratings. These age discrepancies could be attributed to higher levels of loneliness among older adults than the middle-aged group (Luhmann and Hawkley, 2016). Our findings appear to suggest a greater need for socialization, particularly for older adults who are prone to social isolation and loneliness.
From a practical perspective, the present findings identified a few novel avenues by informing practical interventions to focus on the enrichment of the socialization experience of middle-aged and older adults in the community. This could be achieved through the provision of opportunities such as community and mentorship programs to promote social interaction and a sense of group identity. Our results suggest that older adults could benefit from engaging in formal social roles that involve significant interaction and responsibilities, such as attending group meetings or participating in volunteer work. Individuals could regularly participate in group meetings such as book clubs, community gatherings, or volunteering activities. Maintaining a strong social network with family members, friends, or neighbors also plays a significant role in preserving cognitive health in older adults. Older adults who actively engage in hobbies such as gardening or painting may experience cognitive benefits that help maintain their mental acuity. These social activities provide cognitive stimulation and opportunities for problem-solving and help maintain cognitive sharpness in later life. Intervention studies should be conducted to offer targeted programs to address the socialization needs of middle-aged and older adults for better cognitive aging.
Limitations
Several study limitations warrant discussion. Firstly, the measures of lifestyle and social factors were limited to essential features and based on single-item measures in the NSHAP. The associated measurement errors in single-item measures could bias the estimates of the regression models. The incorporation of validated measures such as the International Physical Activity Questionnaire and Pittsburgh Sleep Quality Index would facilitate their effect manifestation. Secondly, the study sample comprised solely the completers in both Wave 2 and Wave 3 of the NSHAP. Item missingness has been inversely associated with cognitive status in the NSHAP (Hawkley et al. 2014). The higher non-response rate at follow-up among those with poorer cognitive status implies potential attrition bias in our findings due to cognitive impairment. We did not examine how baseline cognitive status was linked to mortality during the study period. Since subjects with dementia were more likely to die during the study period, this limitation implies that our findings might have represented conservative estimates of the effects of lifestyle and social factors on cognitive status. Thirdly, over half (58.3%) of the NSHAP sample held at least a college education level, and the relatively high level of education could limit the representativeness of the sample. Caution is warranted in interpreting the present findings among those with lower levels of education and income.
Fourthly, the study focused on the global cognitive status without assessing separate cognitive domains. Further studies should elucidate the potential role of modifiable factors on various cognitive domains. There are potential misclassification errors in using the CCFM score to derive the normal, MCI, and dementia subgroups and examination of transitions across discrete cognitive status could not distinguish minor changes around thresholds from sizeable changes. Fifthly, despite the longitudinal study design, the possibility of reverse causation remains. Deterioration in cognitive abilities may lead to a reduction in social networks and social participation before the study period. Reverse causation might play a role in the positive association between past smoking, current drinking, and better cognitive status. Future panel studies should collect multiple measurements over a longer follow-up period to gauge the cross-lagged effects between the social and lifestyle factors and cognitive status in older adults. Finally, apart from social and lifestyle factors, psychological factors could also contribute to cognitive performance. A recent study (Kang, 2023) has found significant associations between episodic memory performance and certain Big Five personality traits such as openness (positive correlation) and neuroticism and agreeableness (negative correlations) in middle-aged and older adults.
Conclusion
The present study systematically examined the temporal effects of lifestyle and social factors on global cognitive status and its change over a 5-year period. The results suggest a potential influence of social factors on cognitive outcomes over time. Maintaining strong social connections and participating in various social activities may play a role in promoting healthier cognitive status changes in older adulthood. Further research should aim to explore the causal direction of these associations, considering specific cognitive domains and underlying mechanisms. This can enhance our understanding of the impact of lifestyle and social determinants on cognitive health.
Data availability
The raw NSHAP dataset is publicly available from the National Archive of Computerized Data on Aging repository, https://doi.org/10.3886/ICPSR34921.v4 and https://doi.org/10.3886/ICPSR36873.v4. The syntax codes used in the current analysis are available from the fourth author upon reasonable request.
References
Almeida OP, Garrido GJ, Alfonso H, Hulse G, Lautenschlager NT, Hankey GJ, Flicker L (2011) 24-Month effect of smoking cessation on cognitive function and brain structure in later life. NeuroImage 55(4):1480–1489. j.neuroimage.2011.01.063
Anderson ND (2019) State of the science on mild cognitive impairment (MCI). CNS Spectr 24(1):78–87. https://doi.org/10.1017/S1092852918001347
Barnes DE, Yaffe K (2011) The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol 10(9):819–828. https://doi.org/10.1016/s1474-4422(11)70072-2
Chang RC-C, Ho Y-S, Wong S, Gentleman SM, Ng H-K (2014) Neuropathology of cigarette smoking. Acta Neuropathol 127(1):53–69. https://doi.org/10.1007/s00401-013-1210-x
Crooks VC, Lubben J, Petitti DB, Little D, Chiu V (2008) Social network, cognitive function, and dementia incidence among elderly women. Am J Public Health 98(7):1221–1227. https://doi.org/10.2105/ajph.2007.115923
Dale W, Kotwal AA, Shega JW, Schumm LP, Kern DW, Pinto JM et al. (2018) Cognitive function and its risk factors Among older US adults living at home. Alzheimer Dis Assoc Disord 32(3):207–213. https://doi.org/10.1097/wad.0000000000000241
Dautzenberg G, Lijmer J, Beekman A (2020) Diagnostic accuracy of the Montreal Cognitive Assessment (MoCA) for cognitive screening in old age psychiatry: Determining cutoff scores in clinical practice. Avoiding spectrum bias caused by healthy controls. Int J Geriatr Psychiatry 35(3):261–269. https://doi.org/10.1002/gps.5227
Deal JA, Power MC, Palta P, Alonso A, Schneider ALC, Perryman K et al. (2020) Relationship of cigarette smoking and time of quitting with incident dementia and cognitive decline. J Am Geriatr Soc 68(2):337–345. https://doi.org/10.1111/jgs.16228
Diem SJ, Blackwell TL, Stone KL, Yaffe K, Tranah G, Cauley JA et al. (2016) Measures of sleep-wake patterns and risk of mild cognitive impairment or dementia in older women. Am J Geriatr Psychiatry 24(3):248–258. https://doi.org/10.1016/j.jagp.2015.12.002
Durazzo TC, Mattsson N, Weiner MW, Alzheimer’s Disease Neuroimaging I (2014) Smoking and increased Alzheimer’s disease risk: a review of potential mechanisms. Alzheimer’s Dement 10(3S):S122–S145. https://doi.org/10.1016/j.jalz.2014.04.009
Estrella ML, Durazo-Arvizu RA, Gallo LC, Tarraf W, Isasi CR, Perreira KM et al. (2021) Psychosocial factors associated with cognitive function among middle-aged and older Hispanics/Latinos: the Hispanic Community Health Study/Study of Latinos and its Sociocultural Ancillary Study. J Alzheimer’s Dis 79(1):433–449. https://doi.org/10.3233/jad-200612
Frisardi V, Panza F, Seripa D, Imbimbo BP, Vendemiale G, Pilotto A, Solfrizzi V (2010) Nutraceutical properties of Mediterranean diet and cognitive decline: possible underlying mechanisms. J Alzheimer’s Dis 22(3):715–740. https://doi.org/10.3233/jad-2010-100942
Gross AL, Rebok GW, Ford DE, Chu AY, Gallo JJ, Liang KY et al. (2011) Alcohol consumption and domain-specific cognitive function in older adults: longitudinal data from the Johns Hopkins Precursors Study. J Gerontol B Psychol Sci Soc Sci 66(1):39–47. https://doi.org/10.1093/geronb/gbq062
Hawkley LC, Kocherginsky M, Wong J, Kim J, Cagney KA (2014) Missing data in Wave 2 of NSHAP: prevalence, predictors, and recommended treatment. J Gerontol B Psychol Sci Soc Sci 69(Suppl 2):S38–S50. https://doi.org/10.1093/geronb/gbu044
Holtzman RE, Rebok GW, Saczynski JS, Kouzis AC, Wilcox Doyle K, Eaton WW (2004) Social network characteristics and cognition in middle-aged and older adults. J Gerontol B Psychol Sci Soc Sci 59(6):P278–P284. https://doi.org/10.1093/geronb/59.6.p278
Hwang Y, Massimo L, Aryal S, Hirschman KB, Cacchione PZ, Hodgson NA (2024) Does cognitive impairment moderate the relationship between social isolation and anxiety? A 5-year longitudinal study of a nationally representative sample of community residing older adults. BMC Geriatr 24(1):63. https://doi.org/10.1186/s12877-024-04685-z
Jeong S-M, Park J, Han K, Yoo J, Yoo JE, Lee CM et al. (2023) Association of changes in smoking intensity with risk of dementia in Korea. JAMA Netw Open 6(1):e2251506–e2251506. https://doi.org/10.1001/jamanetworkopen.2022.51506
Kang W (2023) Associations between big five personality traits and episodic memory performance in young, middle-aged, and older people: evidence from the immediate and delayed word recall tasks. Pers Individ Differ 202:111967. https://doi.org/10.1016/j.paid.2022.111967
Kang W (2024) Psychological distress mediates the associations between neighborhood social cohesion (NSC) and cognitive performance in older adults. Curr Psychol 43(8):7144–7152. https://doi.org/10.1007/s12144-023-04887-5
Kotwal AA, Kim J, Waite L, Dale W (2016) Social function and cognitive status: results from a US nationally representative survey of older adults. J Gen Intern Med 31(8):854–862. https://doi.org/10.1007/s11606-016-3696-0
Lee S, Lee S, Lee E, Youm Y, Cho HS, Kim WJ (2020) Gender differences in social network of cognitive function among community-dwelling older adults. Geriatr Gerontol Int 20(5):467–473. https://doi.org/10.1111/ggi.13906
Liang JH, Lu L, Li JY, Qu XY, Li J, Qian S et al. (2020) Contributions of modifiable risk factors to dementia incidence: a bayesian network analysis. J Am Med Dir Assoc 21(11):1592–1599.e1513. https://doi.org/10.1016/j.jamda.2020.04.006
Lin TW, Tsai SF, Kuo YM (2018) Physical exercise enhances neuroplasticity and delays Alzheimer’s disease. Brain Plast 4(1):95–110. https://doi.org/10.3233/bpl-180073
Listabarth S, Groemer M, Waldhoer T, Vyssoki B, Pruckner N, Vyssoki S et al. (2022) Cognitive decline and alcohol consumption in the aging population-a longitudinal analysis of the Survey of Health, Ageing and Retirement in Europe. Eur Psychiatry 65(1):e83. https://doi.org/10.1192/j.eurpsy.2022.2344
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S et al. (2020) Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396(10248):413–446. https://doi.org/10.1016/s0140-6736(20)30367-6
Luhmann M, Hawkley LC (2016) Age differences in loneliness from late adolescence to oldest old age. Dev Psychol 52(6):943–959. https://doi.org/10.1037/dev0000117
Mandolesi L, Polverino A, Montuori S, Foti F, Ferraioli G, Sorrentino P, Sorrentino G (2018) Effects of physical exercise on cognitive functioning and wellbeing: biological and psychological benefits. Front Psychol 9:509. https://doi.org/10.3389/fpsyg.2018.00509
Mitchell JJ, Blodgett JM, Chastin SF, Jefferis BJ, Wannamethee SG, Hamer M (2023) Exploring the associations of daily movement behaviours and mid-life cognition: a compositional analysis of the 1970 British Cohort Study. J Epidemiol Commun Health 77(3):189–195. https://doi.org/10.1136/jech-2022-219829
Miyata S, Noda A, Iwamoto K, Kawano N, Okuda M, Ozaki N (2013) Poor sleep quality impairs cognitive performance in older adults. J Sleep Res 22(5):535–541. https://doi.org/10.1111/jsr.12054
Mukamal KJ, Kuller LH, Fitzpatrick AL, Longstreth Jr WT, Mittleman MA, Siscovick DS (2003) Prospective study of alcohol consumption and risk of dementia in older adults. JAMA 289(11):1405–1413. https://doi.org/10.1001/jama.289.11.1405
Nebes RD, Buysse DJ, Halligan EM, Houck PR, Monk TH (2009) Self-reported sleep quality predicts poor cognitive performance in healthy older adults. J Gerontol Ser B 64B(2):180–187. https://doi.org/10.1093/geronb/gbn037
Noort MV, Struys E, Perriard B, Staudte H, Yeo S, Lim S, Bosch P (2016) Schizophrenia and depression: the relation between sleep quality and working memory. Asian J Psychiatr 24:73–78. https://doi.org/10.1016/j.ajp.2016.08.023
O’Doherty K, Lawrence D, Wiencrot A, Walsh S, Satorius J, Burgess E et al. (2021) Ongoing refinement and innovation in the data collection protocols of the third round of the national social life, health, and aging project. J Gerontol B Psychol Sci Soc Sci 76:S215–S225. https://doi.org/10.1093/geronb/gbab179
van Oostrom SH, Nooyens ACJ, van Boxtel MPJ, Verschuren WMM(2018) Long sleep duration is associated with lower cognitive function among middle-age adults - the Doetinchem Cohort Study Sleep Med 41:78–85. https://doi.org/10.1016/j.sleep.2017.07.029
Overton M, Sjögren B, Elmståhl S, Rosso A (2023) Mild cognitive impairment, reversion rates, and associated factors: comparison of two diagnostic approaches. J Alzheimers Dis 91(2):585–601. https://doi.org/10.3233/jad-220597
Paiva AF, Cunha C, Voss G, Delerue Matos A (2023) The interrelationship between social connectedness and social engagement and its relation with cognition: a study using SHARE data. Ageing Soc 43(8):1735–1753. https://doi.org/10.1017/S0144686X2100129X
Penninkilampi R, Casey AN, Singh MF, Brodaty H (2018) The association between social engagement, loneliness, and risk of dementia: a systematic review and meta-analysis. J Alzheimer’s Dis 66(4):1619–1633. https://doi.org/10.3233/jad-180439
Peters R, Poulter R, Warner J, Beckett N, Burch L, Bulpitt C (2008) Smoking, dementia and cognitive decline in the elderly, a systematic review. BMC Geriatr 8:36. https://doi.org/10.1186/1471-2318-8-36
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E (1999) Mild cognitive impairment: clinical characterization and outcome. Arch Neurol 56(3):303–308. https://doi.org/10.1001/archneur.56.3.303
Royston P (2004) Multiple imputation of missing values. Stata J 4(3):227–241
Sen A, Tai XY (2023) Sleep duration and executive function in adults. Curr Neurol Neurosci Rep. 23(11):801–813. https://doi.org/10.1007/s11910-023-01309-8
Shega JW, Sunkara PD, Kotwal A, Kern DW, Henning SL, McClintock MK et al. (2014) Measuring cognition: the Chicago cognitive function measure in the national social life, health and aging project, wave 2. J Gerontol B Psychol Sci Soc Sci 69(Suppl 2):S166–S176. https://doi.org/10.1093/geronb/gbu106
Shimada H, Doi T, Lee S, Makizako H (2019) Reversible predictors of reversion from mild cognitive impairment to normal cognition: a 4-year longitudinal study. Alzheimers Res Ther 11:1–9. https://doi.org/10.1186/s13195-019-0480-5
Shimada H, Makizako H, Lee S, Doi T, Lee S (2018) Lifestyle activities and the risk of dementia in older Japanese adults. Geriatr Gerontol Int 18(10):1491–1496. https://doi.org/10.1111/ggi.13504
Tang F, Chi I, Zhang W, Dong X (2018) Activity engagement and cognitive function: findings from a community-dwelling U.S. Chinese aging population study. Gerontol Geriatr Med 4:1–8. https://doi.org/10.1177/2333721418778180
Thomas PA (2011) Gender, social engagement, and limitations in late life. Soc Sci Med 73(9):1428–1435. https://doi.org/10.1016/j.socscimed.2011.07.035
Waite LJ, Das A (2010) Families, social life, and well-being at older ages. Demography 47(S):S87–S109. https://doi.org/10.1353/dem.2010.0009
Welberry HJ, Tisdell CC, Huque MH, Jorm LR (2023) Have we been underestimating modifiable dementia risk? An alternative approach for calculating the combined population attributable fraction for modifiable dementia risk factors. Am J Epidemiol 192(10):1763–1771. https://doi.org/10.1093/aje/kwad138
Woods AJ, Porges EC, Bryant VE, Seider T, Gongvatana A, Kahler CW et al. (2016) Current heavy alcohol consumption is associated with greater cognitive impairment in older adults. Alcohol Clin Exp Res 40(11):2435–2444. https://doi.org/10.1111/acer.13211
World Health Organization (2021) Global status report on the public health response to dementia. World Health Organization, Geneva
Yaffe K, Fiocco AJ, Lindquist K, Vittinghoff E, Simonsick EM, Newman AB et al. (2009) Predictors of maintaining cognitive function in older adults: the Health ABC study. Neurology 72(23):2029–2035. https://doi.org/10.1212/WNL.0b013e3181a92c36
Yu HH, Tan CC, Huang SJ, Zhang XH, Tan L, Xu W (2024) Predicting the reversion from mild cognitive impairment to normal cognition based on magnetic resonance imaging, clinical, and neuropsychological examinations. J Affect Disord 353:90–98. https://doi.org/10.1016/j.jad.2024.03.009
Zanjani F, Downer BG, Kruger TM, Willis SL, Schaie KW (2013) Alcohol effects on cognitive change in middle-aged and older adults. Aging Ment Health 17(1):12–23. https://doi.org/10.1080/13607863.2012.717254
Zavecz Z, Nagy T, Galkó A, Nemeth D, Janacsek K (2020) The relationship between subjective sleep quality and cognitive performance in healthy young adults: evidence from three empirical studies. Sci Rep 10(1):4855. https://doi.org/10.1038/s41598-020-61627-6
Zhang R, Shen L, Miles T, Shen Y, Cordero J, Qi Y et al. (2020) Association of low to moderate alcohol drinking with cognitive functions from middle to older age among US adults. JAMA Netw Open 3(6):e207922. https://doi.org/10.1001/jamanetworkopen.2020.7922
Zhang Y, Chen SD, Deng YT, You J, He XY, Wu XR et al. (2023) Identifying modifiable factors and their joint effect on dementia risk in the UK Biobank. Nat Hum Behav 7(7):1185–1195. https://doi.org/10.1038/s41562-023-01585-x
Zhaoyang R, Sliwinski MJ, Martire LM, Smyth JM (2018) Age differences in adults’ daily social interactions: an ecological momentary assessment study. Psychol Aging 33(4):607–618. https://doi.org/10.1037/pag0000242
Zunzunegui MV, Koné A, Johri M, Béland F, Wolfson C, Bergman H (2004) Social networks and self-rated health in two French-speaking Canadian community dwelling populations over 65. Soc Sci Med 58(10):2069–2081. https://doi.org/10.1016/j.socscimed.2003.08.005
Acknowledgements
The National Social Life, Health, and Aging Project is supported by the National Institute on Aging and the National Institutes of Health (R01AG021487; R37AG030481; R01AG033903; R01AG043538; R01AG048511).
Author information
Authors and Affiliations
Contributions
All authors have contributed substantially to the article. MW designed the study, conducted data analysis, and wrote the initial manuscript. TCTF conducted data analysis, reviewed the literature, and critically reviewed and revised the manuscript. HZ, JHC, YL, and DS critically reviewed and revised the manuscript. All authors have given their final approval for the version to be published. All authors have agreed to take responsibility for all aspects of the work to ensure that questions about the accuracy or integrity of any part of the work are properly investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to publish
This study does not contain individual participant data.
Ethical approval
The present study was based on secondary, publicly available data from the NSHAP. The NSHAP protocol was approved by the Social and Behavioral Sciences Institutional Review Board at the University of Chicago (Federal Wide Assurance No. FWA00005565) and the Institutional Review Board of the National Opinion Research Center (FWA00000142). All research procedures and measures were performed in accordance with the Declaration of Helsinki.
Informed consent
Written informed consent was obtained from all individual participants in the original NSHAP study. Only de-identified data were made available to researchers.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wen, M., Zheng, H., Chen, JH. et al. Contribution of social and lifestyle factors to cognitive status and 5-year change among middle-aged and older Americans. Humanit Soc Sci Commun 12, 214 (2025). https://doi.org/10.1057/s41599-025-04521-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-025-04521-8