Abstract
As individuals age, they tend to spend more time indoors, underscoring the increasing importance of interior design for healthy aging. Although existing research on this topic is extensive, it lacks integration and consistency, thereby hindering the development of concrete design guidelines. This study employed a scoping review to systematically examine existing literature, clarifying how interior design factors—including indoor environmental quality, layout, and elements—affect the physical, physiological, and mental health of older adults. Following the PRISMA-ScR guidelines, 64 empirical studies published between 2005 and 2024 were analyzed, sourced from Web of Science, Scopus, and PubMed databases. This scoping review highlighted seven key interior design principles that influence older adults’ health: lighting, thermal environment and air quality, spatial layout, barrier-free design, space size, furniture, and relaxation design. The study also revealed evolving research trends through VOSviewer keyword analysis. Across the reviewed studies, differences in design recommendations appeared to reflect regional contexts and varying degrees of frailty among older adults. However, research on physiological responses to various interior design factors remains relatively limited. Future studies could benefit from integrating smart sensing technologies and interdisciplinary approaches to deepen the understanding of how interior design influences the health of older adults.
Similar content being viewed by others
Introduction
The global population is aging. According to the United Nations (2022), the proportion of individuals aged 65 and older is projected to increase from 9.7% in 2022 to 16.4% by 2050. This demographic shift will place substantial pressure on public health systems, societal infrastructure, and economic stability. Consequently, creating supportive environments for older adults not only improves their quality of life but also reduces the burden on caregivers and may offer potential economic benefits (van Hoof et al., 2010).
Aging presents challenges such as declining vision and hearing, reduced mobility, and increased feelings of loneliness, all requiring special consideration in interior design (Engineer et al., 2018; van Hoof et al., 2010). Interior design factors can significantly affect their physical, physiological, and mental health. For instance, lighting influences not only vision and decision-making behaviors (Wang and Leung, 2023) but also daily activities and independence (Falkenberg et al., 2019; Leung et al., 2023). Moreover, appropriate lighting design plays a critical role in regulating sleep patterns and circadian rhythms, potentially mitigating tendencies toward depression and anxiety (Desjardins et al., 2020; Figueiro et al., 2020; Hickman et al., 2007). Therefore, the influence of interior design factors on older adults’ health is multifaceted and complex. A comprehensive understanding of how indoor environments affect physical, physiological, and mental health is essential for designing safe and comfortable housing for this population.
Due to practical and methodological constraints, most empirical studies are limited to examining specific health outcomes or focusing on particular interior design factors (Lindemann et al., 2014; Torres et al., 2020; Figueiro et al., 2020). Consequently, research in this field tends to be fragmented, with concentrated efforts in some areas and notable gaps in others. To address this imbalance and synthesize existing knowledge, systematic and scoping reviews have become widely adopted approaches. These methods involve comprehensive keyword-based searches across major databases, followed by rigorous screening procedures to identify relevant literature. Many of these reviews adhere to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to ensure methodological transparency and reproducibility (Azim et al., 2023; Kropman et al., 2023; Colenberg et al., 2021). The selected studies can then be categorized and analyzed to clarify research patterns and inform future directions.
Currently, several studies have employed the PRISMA guidelines as a research method to integrate the correlation between the environment and physical health (Cai et al., 2024), mental health (Kropman et al., 2023), or personal well-being (Colenberg et al., 2021). Although there have been systematic reviews on environmental factors and the health of older adults, they mainly focus on the impact of neighborhood environments or outdoor environments on people (Barnett et al., 2017; Barnett et al., 2018; Peters et al., 2020; Zhou et al., 2022). As individuals age, they tend to spend more time indoors, rendering interior design an increasingly critical factor in supporting healthy aging. To date, no comprehensive review has synthesized findings across diverse interior design factors and their impact on various health dimensions. Therefore, this scoping review aims to bridge this gap by systematically mapping the literature on how interior design factors influence the physical, physiological, and mental well-being of older adults, thereby identifying research gaps and informing future studies and design practices. To support conceptual clarity, this review defines “interior design factors” as modifiable features within indoor environments such as lighting, layout, barrier-free design, and furniture.
Methods
This study employed a multi-stage scoping review process that combined structured literature screening, thematic classification, and bibliometric visualization. The methodological framework comprised three main components: (1) adherence to PRISMA-ScR guidelines for literature selection, (2) design-health mapping through a classification matrix, and (3) keyword co-occurrence analysis using VOSviewer to map conceptual patterns and visualize their temporal evolution.
Literature search and selection criteria (PRISMA-ScR)
This study adheres to the PRISMA-ScR guidelines (Tricco et al., 2018), a framework specifically developed to enhance the transparency and structure of scoping reviews. This method facilitates the systematic identification of evidence, mapping of key concepts, and clarification of research gaps in complex and multidisciplinary fields. Given the diverse range of interior design studies related to older adults’ physical, physiological, and mental health, a scoping review enables broader inclusion and thematic synthesis of heterogeneous findings.
The initial literature search was conducted in the Web of Science, Scopus, and PubMed databases, focusing on English-language articles published between 2005 and 2024. These databases were selected for their comprehensive coverage of multidisciplinary research in health, environmental design, and gerontology. The following keyword combination was used: (“older adult” OR “older people” OR elderly) AND (“housing” OR “interior” OR “indoor” OR “living” OR “home” OR “residential”) AND (“environment” OR “space”) AND (“physiological” OR “health” OR “intervention”). The search encompassed the title, abstract, and keywords of the articles. The keyword “physiological” was included to capture studies primarily focused on physiological measurements in older adults, while “health” was used as a broader term to encompass both physical and mental health. The keyword “intervention” was added to identify studies on environmental interventions aimed at improving the health of older adults.
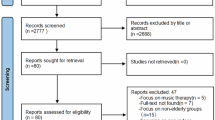
A two-stage screening process was employed to identify relevant studies. First, title and abstract screening was conducted to exclude irrelevant studies based on the following criteria: (1) Studies not directly related to the built environment, such as those in medicine or social sciences (n = 5872); (2) Articles with titles that did not explicitly describe indoor environments (n = 891). This initial screening resulted in 3426 articles. Second, a more rigorous abstract review was conducted to eliminate articles that did not explicitly address the relationship between interior design factors and older adult health. A keyword search of abstracts resulted in the removal of 2210 articles, and an individual screening of abstracts led to an additional exclusion of 1044 articles.
From the remaining 172 papers, further filtering was conducted based on the following criteria: (1) Non-quantitative research (n = 18): Studies employing solely qualitative research methods (e.g., narrative interviews, focus groups, and theoretical modeling) were excluded. Studies that included any quantitative analysis (i.e., mixed-methods designs) were retained; (2) Articles without full-text access (n = 8); (3) Studies not explicitly focusing on the relationship between interior design factors and physical, physiological, or mental health (n = 50); (4) Articles solely addressing basic building services (e.g., water supply, electricity) or non-modifiable architectural factors (e.g., building type, structural materials) (n = 32). This filtering process resulted in the selection of 64 papers. The study selection process and eligibility criteria are illustrated in Fig. 1.
Classification and interior design-health mapping matrix
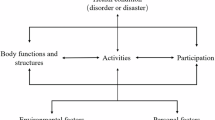
To gain deeper insights into the scope and findings of the selected studies and to allow for thematic mapping of interior design-health associations, we categorized the reported interior design factors and their relationship to older adults’ health. This categorization yielded three primary classifications of interior design factors: “Indoor Environment Quality (IEQ),” “Layout,” and “Elements.” The health classification of older adults was based on the WHOQOL definitions of “Physical Health” and “Mental Health.” In recent years, physiological measurements have been increasingly recognized as an objective method for health assessment, capable of providing real-time, quantitative health indicators, thus generating a significant body of research. Therefore, this study incorporated “Physiological Health” as an additional category to reflect the current state of the literature. The sub-categories within each classification are detailed below.
“IEQ” primarily encompassed the acoustic environment, lighting, thermal environment, and ventilation/air quality. “Layout” referred to functional spatial zones within the living environment, including the balcony, bathroom/toilet, bedroom, kitchen, and living room. Only studies that directly addressed the presence or configuration of these spaces in relation to health outcomes were included in this category. If a study addresses other interior design factors within these spaces, such as lighting in the living room, it is classified under the lighting subcategory of IEQ. “Elements” referred to smaller-scale design features. These elements are considered crucial design details and can impact the health of older adults in multiple ways. This study adapted the classification framework of Lee et al. (2013), modifying it to better align with the criteria of the present research. The final classification included barrier-free design (e.g., handrails, call buttons), color, curtains/louvers, flooring, furniture, indoor plants, materials, outside views, shower/toilet type, space size, and windows/doors.
Regarding health, “Physical Health” primarily encompasses “activities of daily living (ADL),” “pain and discomfort,” “mobility,” “sleep” and rest,” and “visual health.” This study also incorporates “fall risk” as a distinct category, given its impact on the safety and independent living capabilities of older adults. While some studies focus narrowly on specific physical conditions or functions, this study adopts a broader approach by including a subcategory of “general physical health,” enhancing the comprehensiveness and applicability of the classification system. “Physiological Health” concerns physiological measurements related to the physiological responses of older adults. The physiological indicators included in this study are: “body/skin temperature,” “cardiovascular response” (e.g., blood pressure, heart rate, HRV, and other cardiovascular-related measurements), “circadian rhythm” (sleep-related responses), “skin conductance” (using skin electrodes), and “EEG” (electroencephalogram). These indicators provide an objective perspective on the immediate responses of older adults in various environments. “Mental Health” is developed drawing upon the classifications within the WHOQOL framework (WHOQOL Group, 1998). In addition to delineating “feelings/emotions” and “cognitive state,” factors related to key mental health issues such as “anxiety,” “depression,” and “loneliness” are incorporated. Furthermore, research on geriatric mental health frequently addresses Alzheimer’s disease and other dementia-related concerns, often manifesting in behavioral symptoms like aggressive behavior or agitation. Therefore, “behavioral symptoms” are included to provide a more comprehensive assessment of the mental health status of older adults. Finally, to encompass general mental health evaluations, a “general mental health” factor is also added. This ensures the inclusion of studies that assess overall mental well-being, without a specific focus on particular emotional states.
Keyword co-occurrence map (VOSviewer)
To complement the interior design-health mapping matrix, keyword co-occurrence analysis was conducted using VOSviewer, a bibliometric and scientometric visualization tool (van Eck and Waltman, 2009; Gutiérrez-Salcedo et al., 2018). Numerous peer-reviewed publications have validated its utility across various disciplines. Its algorithms and visualization methods have been shown to produce stable and replicable results, establishing it as a credible and reliable tool for mapping research themes and keyword relationships. VOSviewer processes large textual data (e.g., titles, abstracts, and keywords) and visualizes relationships between frequently co-occurring terms. This tool facilitates rapid and clear understanding of connections between concepts or terms across research fields (Yang et al., 2024; Gutiérrez-Salcedo et al., 2018).
In this study, the full counting method was applied, in which each keyword pair was counted once per article. Keywords with a minimum occurrence of two were included in the analysis. To balance the influence of keyword frequency, association strength was applied as the normalization method. This approach adjusts for size differences in keyword occurrence, providing a more accurate reflection of the actual relationships between keywords (van Eck and Waltman, 2009).
Results
Our scoping review identified seven distinct patterns of health focus across the 64 included studies, reflecting a fragmented but gradually integrating research landscape (see Fig. 2). While physical health (n = 19) and physiological health (n = 17) have received comparable levels of attention, mental health (n = 9) has been less frequently addressed. Notably, studies incorporating multiple health dimensions remain limited, suggesting that integrative approaches are still in their early stages. Research addressing mental health appeared earliest, with the first publication in 2007, followed by research on physical health in 2012. However, studies explicitly focusing on physiological health did not emerge until 2014, reflecting a later recognition of this dimension as an independent research area. Regarding combined health dimensions, studies integrating physical and mental health were the most prevalent (n = 15). In contrast, research combining physical and physiological health was much less common, with only one publication. Similarly, studies merging physiological and mental health were limited to just two publications. A single study in 2020 addressed all three health dimensions. Overall, research on physiological health remains less explored compared to physical and mental health. Nonetheless, its integration with other health dimensions represents a relatively novel and evolving approach within the field.
Associations between interior design factors and physical health
Figure 3 presents a matrix of interior design factors and associated health outcomes across the 64 included studies. Among physical health factors, “fall risk,” “ADL,” and “mobility” were the most frequently examined outcomes, with “barrier-free design,” “lighting,” and “bathroom” configurations being the most frequently examined interior design factors.
“Pain and discomfort” and “general physical health” were both associated with “thermal environment,” “ventilation/air quality,” and “lighting.” There is currently no strong evidence linking other interior design factors to “pain and discomfort.” “Sleep and rest” was most frequently associated with “lighting,” with six studies confirming a significant relationship. In contrast, other interior design factors received relatively little attention in relation to “sleep and rest”; only one study each has identified a significant association with “color” and with “outside views.” “Visual health” has received limited research attention and has only been associated with “lighting,” “barrier-free design,” “furniture,” and “window/door” design. This imbalance underscores the need for further research into underexplored areas and into how a broader range of design features can support physical functioning across daily routines.
Associations between interior design factors and physiological health
Among the six physiological health outcomes reviewed, “cardiovascular response” was the most frequently studied, followed by “body/skin temperature” and “skin electrodes” (see Fig. 3).
Studies on physiological health have predominantly focused on “cardiovascular response,” with the thermal environment emerging as the most frequently examined factor (n = 9). This emphasis reflected the well-documented sensitivity of older adults to temperature fluctuations and the physiological stress linked to thermal discomfort. Only a few studies have examined the influence of “indoor plants,” “ventilation/air quality,” “color,” “material,” or “outside views,” highlighting a lack of diversity in the environmental variables explored and suggesting opportunities for broader future research.
The second most frequently studied physiological factor was “body/skin temperature,” which was only linked to thermal environment (n = 7), indicating a lack of research connecting body/skin temperature with other interior design elements. Other physiological measures, such as “skin electrodes,” were used to assess stress-related responses (e.g., nervousness, anxiety, emotional instability). These were applied in studies examining the effects of “lighting” (n = 1), “thermal” conditions (n = 2), and “indoor plants” (n = 1). These findings suggest that “lighting” and “temperature” influence not only subjective comfort but also measurable stress levels in older adults. In addition, two studies linked “lighting” to “circadian rhythm” regulation, reinforcing its role in maintaining sleep-wake cycle stability. One study investigated how interior “color” affected “EEG” activity, using this physiological measure to objectively assess older adults’ color preferences (Jung et al., 2022). Interestingly, all three studies that addressed the presence of “indoor plants” focused specifically on physiological health outcomes, suggesting a promising yet underexplored area of research into the restorative or stress-reducing effects of biophilic design. However, despite growing interest in biophilic design in general environmental research, its application in studies on the physiological health of older adults remains limited.
Associations between interior design factors and mental health
Among the six mental health outcomes reviewed, “depression” was the most frequently studied, followed by “general mental health” and “feelings/emotion” (see Fig. 3). “Lighting” was the most commonly cited environmental factor linked to “depression” (n = 5), followed by “bathroom/toilet” (n = 2). Notably, “bedrooms” did not appear in studies related to “depression”; however, one study found that the absence of a private bedroom was associated with increased “anxiety,” suggesting that the absence of private spaces may exacerbate anxiety instead of depression. No studies linked the balcony, kitchen, or living room to anxiety, potentially reflecting the unique mental functions of private versus communal environments.
For “general mental health,” diverse interior factors were implicated, including “lighting,” “acoustic environment,” “barrier-free design,” “color,” “furniture,” “space size,” and “window/door.” Regarding “feelings/emotions,” “lighting” again emerged as a dominant interior design factor (n = 4). A few studies explored the influence of interior design factors like “color,” “flooring,” “furniture,” “outside view,” and “window/door” on this category. Among these interior design factors, “furniture” stood out as the only factor significantly linked to loneliness, and was also associated with cognitive state, feelings/emotions, and general mental health. This suggests that furniture, due to its daily functional and emotional proximity, plays a critical yet under-recognized role in supporting older adults’ mental well-being. Further research is needed to explore the emotional impact of other interior design factors currently underrepresented in literature.
Discussion
This discussion delves into the associations between interior design factors and health, highlighting seven key interior design principles that influence older adults’ health. To support the analysis, VOSviewer was employed to visualize keyword co-occurrence patterns and to identify research trends and gaps across the reviewed literature. In the following figures, circle size represents the frequency of keyword co-occurrence, while color indicates the average publication year of the articles in which the keyword appeared. Purple represents earlier studies, whereas yellow indicates more recent publications. Ultimately, this study provides insights into the variations and underlying implications of these principles across diverse regions and populations.
Lighting to support rest and activity
Lighting has emerged as the most comprehensively studied interior design factor, particularly due to its effects on rest, mood, and daily functioning. Appropriate lighting design improves sleep quality, supports healthy circadian rhythms, reduces depressive symptoms, and assists older adults in daily life. Figure 4 presents the temporal keyword co-occurrence network of “lighting.” Early-stage research concentrated on sleep-related topics, mid-stage research shifted toward depression, and later studies introduced detailed design elements such as color temperature and visual environment.
Initial studies primarily explored lighting as a tool to improve sleep and circadian rhythms. Light therapy was shown to enhance melatonin secretion, sleep efficiency, and alleviate depression in individuals with dementia (Garre-Olmo et al., 2012; Leung et al., 2017; Hopkins et al., 2017). Subsequent research refined this approach through dynamic color temperature schemes, using blue-enriched light during the day, gradually lowering intensity, and shifting to warmer (yellow) light at night (Shishegar et al., 2021; Shishegar and Boubekri, 2022). More recent studies have expanded this focus to include visual environment design that supports daily activities. For instance, ambient lighting in living areas should exceed 200 lx, while task lighting should reach 500–750 lx to support visibility and independence (Wang and Leung, 2023). Additionally, spatially uniform luminance distribution and fixtures with adjustable brightness and color temperature have been shown to improve user satisfaction (Leung et al., 2023).
US-based studies highlighted a medicalized and interventionist approach focused on regulating biological rhythms through time-specific exposure (Hickman et al. 2007; Figueiro et al., 2020; Shishegar et al., 2021; Shishegar and Boubekri, 2022; Figueiro et al., 2023). In contrast, East Asian designs emphasized spatially integrated lighting strategies, such as navigation cues, differentiated illuminance levels and overall luminance balance (Leung et al., 2023), to support ADL and physical comfort (Fu et al., 2022; Wang and Leung, 2023). Together, these findings underscore the role of culturally and spatially tailored lighting strategies in enhancing rest, activity, and emotional regulation for older adults.
Personalized responses to thermal and air quality stressors
Over the past decade, research on thermal environments and older adults has expanded from subjective assessments to include more technologically integrated approaches. As shown in Fig. 5, early-stage keywords such as “physical performance” and “risk factor” appeared in darker colors, indicating that initial studies on thermal environments focused on temperature extremes in healthcare facilities (Garre-Olmo et al., 2012; Lindemann et al., 2014). Beginning around 2015, attention shifted toward “behavioral symptom,” “psychological symptom,” and objective physiological indicators such as “cardiovascular response” (Fink et al., 2015; Wang et al., 2019; Xiong et al., 2019). During this period, behavioral symptoms in relation to thermal conditions also gained attention (Tartarini et al., 2017). More recent studies have emphasized terms like “pain,” “disease,” and “arthritis,” suggesting a growing interest in the pathological consequences of thermal exposure among older adults (Guo et al., 2022; Zhou et al., 2023; Meade et al., 2024).
Figure 5 positions “thermal environment” and “ventilation/air quality” in close proximity, linked by a thick line, indicating that they were frequently examined together. Empirical evidence supported this co-occurrence: during two severe heatwave episodes, residents closed windows to avoid overheating, which led to increased indoor CO2 concentrations and elevated cardiovascular strain (Fink et al., 2015). The study also confirmed that combined thermal load and poor indoor air quality have a stronger impact on cardiovascular parameters than exposure alone. Regarding air quality improvement strategies, Chen et al. (2020) identified indoor plants as a practical and low-cost method to reduce indoor PM2.5 and TVOCs. Zhang et al. (2024a, 2024b) further reported that HVAC interventions have the strongest mediating effects through indoor cold exposure, followed by air pollution and wet exposure, and that HVAC behavior can help alleviate arthritis symptoms in older adults.
In addition to measurable environmental factors, subjective perceptions of air quality significantly affect well-being. Older adults who rated their indoor air quality poorly reported lower health satisfaction and reduced residential satisfaction (Liu et al., 2023). These findings also revealed key regional and individual differences in thermal sensitivity and health outcomes. While research in China suggests a common comfort range of 24 °C–30 °C (Xiong et al., 2019), studies in North America support a slightly lower ideal range of 22 °C–26 °C (Meade et al., 2024), possibly reflecting differences in climate and building insulation. In the UK, a study found that moldy indoor odors in social housing increased the risk of asthma among older adults (Moses et al., 2019). Similarly, in China’s humid regions, damp indoor environments and persistent mold odors were significantly associated with joint pain and rheumatic diseases in older populations (Zheng et al., 2024). As for personal differences, during the most severe heatwave episodes, heart rate increments reached up to ~70% in older adults with cardiovascular disease, compared to ~50% in their healthy peers (Fink et al., 2015). Zhou et al. (2024) found that the comfortable temperature range for frail older adults is significantly narrower than for non-frail older adults: 24.0 °C–30.0 °C for non-frail individuals, 24.3 °C–29.3 °C for pre-frail individuals, and 25.9 °C–29.3 °C for frail individuals. Overall, these findings emphasized the critical need to tailor indoor thermal and air quality conditions based on both regional climate and individual health characteristics. These results also underscore the importance of integrating personalized and climate-adaptive design strategies into residential environments, not only to mitigate pain and discomfort but also to support broader physiological resilience and well-being in older adults.
Spatial layout, autonomy, and connected living
Among layout-related studies, bathroom configuration and bedroom privacy received the most attention, reflecting the critical role in supporting older adults’ health, safety, and autonomy. Key design factors included the completeness of facilities within each functional space, the spatial connectivity between functional spaces, and the ability to control one’s personal room (Bicket et al., 2010; Fang et al., 2023; Qiao et al., 2024; Zheng et al., 2024).
Given that many of the included studies focused on bathrooms/toilets, we used the VOSviewer temporal trend map of the keyword “bathroom/toilet” as the central axis for discussion. As shown in Fig. 6, earlier research emphasized functional features of these spaces. Purple-colored keywords such as assisted living, privacy, and physical performance were associated with studies highlighting safety, autonomy, and functional independence (Bicket et al., 2010; Yang and Sanford, 2012). For instance, Bicket et al. (2010) found that the installation of call buttons in the living space effectively reduced behavioral symptoms by enhancing older adults’ perceived safety and autonomy within their private environments. While older adults may require assistance in certain aspects of life, they still desire private space to preserve their dignity. Similarly, Yang and Sanford (2012) indicated that room characteristics could influence older adults’ social engagement, reflected in the keyword “social environment” on the VOSviewer map.
In subsequent years, green-coded keywords such as “home environment,” “fall,” “barrier-free design,” and “safety” indicated a shift toward spatial connectivity and risk reduction. Layouts that provide direct access between the bedroom and bathroom reduce nighttime walking distance and help prevent fall-related injuries (Iamtrakul et al., 2021). More recent keywords in yellow, such as “ADL,” “age in place,” “physical health,” and “mental health,” have reflected a growing emphasis on the integration of spatial features with daily functioning. For example, having a private toilet or bathroom is significantly associated with better mobility and ADL performance among older adults aging at home (Fang et al., 2023). Appropriate bathroom facilities enable older adults to maintain personal hygiene, which helps reduce frailty and vulnerability. In contrast, inadequate facilities can lead to hygiene difficulties and compromise overall well-being. In addition to their impact on physical health, limited bathroom facilities have also been significantly associated with higher levels of depression and anxiety among older adults in rural China (Zheng et al., 2024; Qiao et al., 2024).
US-based studies began earlier to investigate how the private use of bathrooms and bedrooms influences mental health and mobility (Bicket et al., 2010; Yang and Sanford, 2012). In recent years, Asian research has expanded, with a notable focus on room autonomy and its health implications, drawing attention to older adults’ anxiety and depression in the context of aging in place (Li and Zhou, 2020; Zheng et al., 2024; Qiao et al., 2024). However, studies focusing on other shared domestic spaces such as balconies, kitchens, and living rooms remain relatively limited. Future research could investigate how the degree of spatial privacy influences mental health outcomes, particularly the differential mechanisms behind anxiety and depression. Addressing these gaps will be crucial for developing inclusive layout strategies that not only support aging with dignity but also foster social connection and mental well-being in shared domestic environments.
Barrier-free design and visual support
Barrier-free design has long been recognized as essential for supporting older adults’ mobility and daily functioning. In recent years, it has also been increasingly associated with visual support strategies to enhance spatial awareness and emotional well-being (Leung et al., 2019b; Wu et al., 2022; Fang et al., 2023; Leung et al., 2023). For example, Wang and Leung (2023) reported that over 60% of older residents in care homes relied on walking aids, and 50% had at least one type of eye disease. Handrails with high color contrast (30% luminance contrast) against the background wall or those LED guiding light enhanced visibility and reduced fear of falling (Thölking et al., 2020; Wang and Leung, 2023).
Given the centrality of safety and accessibility in aging-related design, we used the temporal trend map of the keyword “barrier-free design” as the basis for discussion. As shown in Fig. 7, early studies predominantly focused on institutional environments such as nursing homes, healthcare facilities, and assisted living centers, where the priority was ensuring safety and mobility for residents with advanced disabilities or dementia (Bicket et al., 2010; Leung et al., 2019b). However, more recent research has increasingly emphasized the importance of the home environment and the concept of aging in place (Gell et al., 2020; Wu et al., 2022; Fang et al., 2023; Tonchoy et al., 2024; Das Gupta et al., 2024). This shift reflected both global demographic pressures and a growing recognition that many older adults prefer to age in place rather than relocate to institutional care. Correspondingly, current research on barrier-free design focuses on residential modifications that promote independence, safety, and quality of life among community-dwelling older adults.
Importantly, as visual health and perception are integral to both physical safety and emotional well-being, recent research increasingly links barrier-free design with visual support strategies, particularly for addressing “visual stimulation” needs and mitigating “visual impairment” risks (see Fig. 7). Figure 8 illustrates the broader network of “visual environment,” including lighting, furniture, window and door design, color schemes, and access to outside views. For example, warm and bright colors can enhance spatial awareness (Leung et al., 2017). Window design is associated with the amount of natural daylight entering the space, improving overall brightness and supporting safer, more comfortable walking conditions for older adults. Leung et al. (2024) suggested that the window-to-floor ratio of rooms in care homes should exceed that of general residential buildings, recommending a minimum of 1:4, while the ratio for living rooms or bedrooms should be at least 1:6. Recent trends have emphasized multi-sensory visual design, integrating color, natural light, and meaningful visual cues. For example, Leung et al. (2024) suggested using personalized door decorations to support wayfinding and memory recall in older adults with cognitive impairments. In addition, having visual access to natural scenery has been associated with positive emotional outcomes in older adults (Xiaoxue and Huang, 2024; Leung et al., 2024). Accordingly, placing beds or chairs near windows with appealing views is considered an effective design strategy to promote emotional well-being (Wang and Leung, 2023).
However, visual design preferences may differ based on room function, mental state, or cultural background. For example, Torres et al. (2020), studying older adults in Spain, emphasized that color preferences vary depending on room function (e.g., warm tones for activity rooms). Jung et al. (2022) found that in the United Arab Emirates, older adults with depression preferred contrasting color schemes (e.g., blue and yellow), while non-depressed participants leaned toward cool colors, suggesting that mental state may also affect color preferences. In other regions, studies from Hong Kong place less emphasis on individual preference and instead focus on the functional application of color for spatial cognition (Leung et al., 2017; Leung et al., 2024). These findings suggest that although assisted living environments primarily focus on physical safety and visual support, it is also important to incorporate culturally and psychologically informed design elements. This approach can provide more personalized care that enhances both physical safety and emotional well-being in later life.
Space size and aging needs
Space size plays a fundamental role in shaping older adults’ mobility, autonomy, and mental well-being, influencing both daily function and long-term adaptation to aging. Leung et al. (2017) recommend a minimum of 25–35 m2 per person and a turning radius of 150 × 150 cm in older adults’ housing units. Sufficient space enabled the use of mobility aids and enhanced social interaction. In contrast, crowded conditions have been linked to a higher risk of poor mental health (Tao et al., 2018; Qiu et al., 2020).
Figure 9 illustrates the temporal trend map of the keyword “space size.” Earlier studies prioritized providing sufficient space to enhance physical function, privacy, and independent living, thereby reducing daily life risk factors (Cress et al., 2011; Tao et al., 2018; Leung et al., 2017). More recent research has shifted toward examining mental health outcomes. For instance, Qiu et al. (2020) reported that living in homes over 250 m2 was associated with ~66% lower odds of depression compared to homes under 50 m2. However, space needs may vary depending on cognitive status. For older adults with dementia, smaller, visually accessible spaces may improve wayfinding and reduce disorientation (Leung et al., 2024). This reflected a shift from the traditional “bigger is better” design paradigm toward a more context-sensitive and needs-based approach.
Research on space size and older adults’ health has largely emerged from Hong Kong and China (Leung et al., 2017; Tao et al., 2018; Qiu et al., 2020; Leung et al., 2024). However, cross-cultural differences may also shape design standards. Body dimensions, cultural living arrangements, and housing constraints all contribute to how aging-related spatial needs are defined. Older adults in Hong Kong or China generally face higher-density environments, with smaller housing units and multi-generational households, compared to their counterparts in Western countries. As a result, spatial data and recommendations derived from East Asian contexts may not be directly generalizable to Western settings. This underscores the need for space-size design strategies that are both culturally responsive and adaptable to the diverse physical and functional needs of older adults.
Functional and emotional roles of furniture
Furniture, including cabinets, beds, seating arrangements, and their spatial placement, not only supports physical function but also profoundly shapes older adults’ daily experiences, visual comfort, and social connection. For example, storage units higher than 120 cm or wardrobes deeper than 40 cm may be difficult to access due to age-related declines in strength and flexibility (Leung et al., 2017; Leung et al., 2019a). One study found that the usability of kitchen cabinets was positively correlated with older adults’ level of social participation (Yang and Sanford, 2012). In healthcare facility settings, inappropriate seating layouts can diminish social interaction; Leung et al. (2024) observed that residents in care homes spent only 13.4% of their time interacting with others, with 2.2% of these interaction attempts receiving no response, often due to poorly arranged dining furniture that obstructed visibility or proximity. Beyond physical and social functions, furniture placement also influences visual comfort. For instance, beds placed too close to bright windows may lead to eye fatigue, whereas strategic placement can improve visual clarity through extended viewing distances (Wang and Leung, 2023).
Figure 10 visualizes the evolving focus of furniture-related research over time. Early-stage keywords, shown in darker colors, reflected an emphasis on basic usability in private residences, particularly their impact on physical performance (Yang and Sanford, 2012; Leung et al., 2017; Leung et al., 2019a). The appearance of terms such as “kitchen,” “bathroom,” and “independent living” suggests that furniture in these specific spaces was viewed as essential for maintaining older adults’ autonomy in daily life. Since 2019, more studies have focused on care homes and nursing homes, extending the scope of furniture-related research to deeper health dimensions such as cognitive performance, loneliness, and satisfaction (Leung et al., 2019b; Leung et al., 2020; Wang and Leung, 2023; Leung et al., 2024). This evolution reflected a shift from purely functional considerations to emotional and symbolic roles, such as fostering a homelike atmosphere through furniture design. Notably, the majority of these recent studies originated in Hong Kong and were conducted by overlapping author teams. While this concentration suggested both regional expertise and a potential limitation in cultural generalizability, underlining the need for more diverse, cross-cultural research explores how furniture can support both the functional and emotional needs of aging populations in different cultural contexts.
Relaxing interior design
While certain interior elements have received limited empirical attention, their potential to support older adults’ well-being remains significant and underexplored. One particularly promising area is biophilic design, which incorporates elements such as “indoor plants,” “material,” and “outside view.” These features aimed to promote relaxation and enhance both psychological and physiological well-being in older adults. Yan and Guo (2023) found that a wood coverage ratio of ~30% elicited the most positive subjective responses from older adults, who perceived the space as more natural, warm, and comfortable. At a 90% coverage ratio, a significant calming effect was observed.
These studies often employed simulation, virtual reality, or physiological measurements to assess whether similar interior environments could effectively induce relaxation in older adults (Goto et al., 2014; Chen et al., 2020; Yan and Guo, 2023). For example, Xiaoxue and Huang (2024) demonstrated that even in entirely virtual environments, biophilic stimuli such as green walls or outdoor views significantly reduced participants’ stress and anxiety, as measured by heart rate, blood pressure, skin conductance, and STAI scores. These findings suggest that even visual simulations of nature can still offer measurable therapeutic benefits. This may offer an accessible and cost-effective strategy for older adults living in high-density or resource-constrained settings.
Notably, such research has been predominantly conducted in East and Southeast Asian contexts, including Japan, Taiwan, China, Hong Kong, and Thailand, where urban density, limited outdoor greenery, and rapid population aging may shape both the research and design priorities. Collectively, these findings build a strong case for incorporating visual biophilic strategies into interior design, especially in resource-constrained or high-density settings, where supporting emotional and physiological relaxation is critical for healthy aging.
Practical recommendations
Based on the reviewed evidence, seven key interior design principles from the discussion should guide the design of living spaces for older adults: lighting, thermal and air quality, spatial layout, barrier-free features, space size, furniture, and relaxation design. Designers are encouraged to provide dynamic color temperature with ambient levels above 200 lx and task lighting between 500–750 lx to support circadian rhythms and visual needs. Thermal comfort should ideally be maintained at around 26 °C, combined with proper ventilation to control CO2 and PM2.5 levels. Spatial layouts should ensure at least 25–35 m2 per person, with a minimum turning radius of 150 cm to accommodate mobility aids. Barrier-free features such as handrails with ≥30% luminance contrast, clear navigation cues, and call buttons can enhance safety and independence. Furniture should be both accessible (e.g., storage units no higher than 120 cm and no deeper than 40 cm) and emotionally familiar to foster social connection. Finally, incorporating biophilic elements, such as 30–90% wood coverage or views of natural scenery, can promote relaxation and emotional well-being, supporting a holistic approach to healthy aging.
Future research
This scoping review highlighted how interior design factors affected older adults’ physical, physiological, and mental health well-being. Among the three health domains reviewed, physiological health remained the least studied across most interior design factors. This gap limited our understanding of how interior spaces may influence not just subjective experience, but also measurable biological responses in older adults.
In recent years, there has been a growing emphasis on Smart Healthy Age-Friendly Environments (SHAFE), which integrate smart technologies with age-conscious design principles to foster environments that are responsive, supportive, and empowering (van Boekel et al., 2024). Although most of the studies included in this review did not explicitly adopt SHAFE frameworks, many findings align with SHAFE objectives. For example, future research could explore the implementation of lighting systems that mimic natural daylight patterns to support circadian rhythms and reduce the risk of depression and anxiety. Similarly, temperature regulation systems that automatically adapt to individual needs or offer customizable controls could enhance thermal comfort and physiological stability. Research could also examine the integration of ergonomic principles into smart furniture systems for older adults. These may include adjustable beds and responsive seating that support physical comfort, as well as customized colors and materials that reflect users’ memories and cultural preferences. Such design strategies can help reinforce a sense of identity and familiarity. As SHAFE principles evolve, future design strategies should balance technological innovation with emotional and cultural resonance to ensure that environments are not only smart and safe but also comforting and deeply human.
Moreover, although not part of the 64 studies reviewed, emerging research has increasingly incorporated physiological monitoring systems and environmental sensors to objectively assess older adults’ responses to indoor conditions. For example, Bui et al. (2024) explored fall detection, Rodrigues et al. (2024) examined sedentary behavior tracking, and Jouini et al (2023) investigated real-time physiological data monitoring. These wearable technologies offer promising tools for real-time feedback, early intervention, and evidence-based validation of design impacts. Future interdisciplinary collaborations between interior design, gerontology, and digital health are needed to advance both empirical knowledge and practical applications in creating responsive, health-promoting environments for aging populations.
Conclusion
This study develops a structured classification system for both interior design factors (IEQ, layout, and elements) and health outcomes (physical, physiological, and mental health). This framework provides a clear and organized way to understand the complex relationships between these domains. The use of VOSviewer for keyword co-occurrence analysis offers a visual representation of the key themes and their evolution over time within the research field. This approach helps clarify both historical focus and emerging trends in the study of interior design and older adult health.
This study offers several key contributions for stakeholders involved in promoting the well-being of older adults. For policymakers and urban planners, it provides a comprehensive understanding of how specific interior design factors within residential environments impact physical, physiological, and mental health. Architects and interior designers can leverage the identified associations and research gaps to create innovative and person-centered designs that proactively address the diverse needs of the aging population. Furthermore, healthcare professionals and caregivers can gain valuable insights into the environmental influences on their patients’ and clients’ health outcomes. Understanding these connections can lead to more holistic care strategies that incorporate modifications to the living environment as part of health management and preventative measures. Finally, for older adults themselves and their families, this research underscores the significant role of the home environment in maintaining independence, well-being, and quality of life. It empowers them to make informed decisions about housing choices and home adaptations that can positively influence their health and support aging in place.
Despite a rigorous screening process following PRISMA-ScR guidelines, it is possible that some relevant studies were not included, particularly those where the relationship between design and health was implicit or not clearly stated in titles or abstracts. Nonetheless, the findings highlight several key gaps, especially the limited number of studies examining physiological responses to interior design factors. As technologies such as wearable sensors and smart environmental monitors evolve, future studies should explore their application in interior design research to enhance precision and empirical depth. However, existing empirical studies remain largely concentrated in high-density Asian cities, where spatial constraints and rapid aging shape both design practices and research priorities. To build more generalizable knowledge, future research should include cross-cultural comparisons that examine how interior design strategies perform across diverse living environments and sociocultural contexts.
Data availability
All the data analyzed in this study are provided in the published article and its supplementary information files.
References
Azim FT, Ariza-Vega P, Gardiner PA, Ashe MC (2023) Indoor built environment and older adults’ activity: a systematic review. Can J Aging 42(2):241–258. https://doi.org/10.1017/S0714980822000241
Barnett A, Zhang CJ, Johnston JM, Cerin E (2018) Relationships between the neighborhood environment and depression in older adults: a systematic review and meta-analysis. Int Psychogeriatr 30(8):1153–1176
Barnett DW, Barnett A, Nathan A, Van Cauwenberg J, Cerin E (2017) Built environmental correlates of older adults’ total physical activity and walking: a systematic review and meta-analysis. Int J Behav Nutr Phys 14:1–24. https://doi.org/10.1186/s12966-017-0558-z
Bicket MC, Samus QM, McNabney M, Onyike CU, Mayer LS, Brandt J, Rabins P, Lyketsos C, Rosenblatt A (2010) The physical environment influences neuropsychiatric symptoms and other outcomes in assisted living residents. Int J Geriat Psychiatry 25(10):1044–1054. https://doi.org/10.1002/gps.2460
Bui T, Liu J, Cao J, Wei G, Zeng Q (2024) Elderly fall detection in complex environment based on improved YOLOv5s and LSTM. Appl Sci 14(19):9028
Cai J, Yang M, Zhang N, Chen Y, Wei J, Wang J, Liu W (2024) Effects of residential damp indicators on asthma, rhinitis, and eczema among children: a systematic review and meta-analysis of the literature in the past 33 years. Build Environ 251:111226
Chen RY, Ho KF, Hong GB, Chuang KJ (2020) Houseplant, indoor air pollution, and cardiovascular effects among elderly subjects in Taipei, Taiwan. Sci Total Environ 705:135770
Colenberg S, Jylhä T, Arkesteijn M (2021) The relationship between interior office space and employee health and well-being—a literature review. Build Res Inf 49(3):352–366
Cress ME, Orini S, Kinsler L (2011) Living environment and mobility of older adults. Gerontology 57(3):287–294. https://doi.org/10.1159/000322195
Das Gupta D, Kelekar U, Turner SC (2024) Older adult falls in the community: does unsafe home environment have a risk role through the mediating effect of functional limitations? Gerontologist 64(5):gnad139
Desjardins S, Lapierre S, Vasiliadis HM, Hudon C (2020) Evaluation of the effects of an intervention intended to optimize the sleep environment among the elderly: an exploratory study. Clin Inter Aging 15:2117–2127. https://doi.org/10.2147/cia.S277252
Engineer A, Sternberg, Esther M, Najafi B (2018) Designing interiors to mitigate physical and cognitive deficits related to aging and to promote longevity in older adults: a review. Gerontology 64(6):612–622. https://doi.org/10.1159/000491488
Falkenberg HK, Kvikstad TM, Eilertsen G (2019) Improved indoor lighting improved healthy aging at home—an intervention study in 77-year-old Norwegians. J Multidiscip Health 12:315–324. https://doi.org/10.2147/jmdh.S198763
Fang S, Liang H, Liang Y (2023) Relationship between person, environmental factors, and activities of daily living performance among physically disabled older adults living at home: a structural equation model. BMC Geriatr 23(1):285. https://doi.org/10.1186/s12877-023-04000-2
Figueiro MG, Sahin L, Kalsher M, Plitnick B, Rea MS (2020) Long-term, all-day exposure to circadian-effective light improves sleep, mood, and behavior in persons with dementia. J Alzheimers Dis Rep. 4(1):297–312. https://doi.org/10.3233/adr-200212
Fink R, Eržen I, Medved S, Kastelec D (2015) Experimental research on physiological response of elderly with cardiovascular disease during heat wave period. Indoor Built Environ 24(4):534–543
Fu Y, Wu Y, Gao W, Hui R (2022) The effect of daylight illumination in nursing buildings on reading comfort of elderly persons. Buildings 12(2):214
Garre-Olmo J, López-Pousa S, Turon-Estrada A, Juvinyà D, Ballester D, Vilalta-Franch J (2012) Environmental determinants of quality of life in nursing home residents with severe dementia. J Am Geriatr Soc 60(7):1230–1236. https://doi.org/10.1111/j.1532-5415.2012.04040.x
Gell NM, Brown H, Karlsson L, Peters DM, Mroz TM (2020) Bathroom modifications, clutter, and tripping hazards: prevalence and changes after incident falls in community-dwelling older adults. J Aging Health 32(10):1636–1644
Goto S, Kamal N, Puzio H, Kobylarz F, Herrup K (2014) Differential responses of individuals with late-stage dementia to two novel environments: a multimedia room and an interior garden. J Alzheimers Dis 42(3):985–998
Guo M, Zhou M, Li BZ, Du CQ, Yao RM, Wang LX, Yang X, Yu W (2022) Reducing indoor relative humidity can improve the circulation and cardiorespiratory health of older people in a cold environment: a field trial conducted in Chongqing, China. Sci Total Environ 817:152695. https://doi.org/10.1016/j.scitotenv.2021.152695
Gutiérrez-Salcedo M, Martínez MÁ, Moral-Munoz JA, Herrera-Viedma E, Cobo MJ (2018) Some bibliometric procedures for analyzing and evaluating research fields. Appl Intell 48(5):1275–1287. https://doi.org/10.1007/s10489-017-1105-y
Hickman SE, Barrick AL, Williams CS, Zimmerman S, Connell BR, Preisser JS, Mitchell M, Sloane PD (2007) The effect of ambient bright light therapy on depressive symptoms in persons with dementia. J Am Geriatr Soc 55(11):1817–1824. https://doi.org/10.1111/j.1532-5415.2007.01428.x
Hopkins S, Morgan PL, Schlangen LJM, Williams P, Skene DJ, Middleton B (2017) Blue-enriched lighting for older people living in care homes: effect on activity, actigraphic sleep, mood and alertness. Curr Alzheimer Res 14(10):1053–1062. https://doi.org/10.2174/1567205014666170608091119
Iamtrakul P, Chayphong S, Jomnonkwao S, Ratanavaraha V (2021) The association of falls risk in older adults and their living environment: a case study of rural area, Thailand. Sustainability 13(24):13756. https://doi.org/10.3390/su132413756
Jouini R, Houaidia C, Saidane LA (2023) Hidden markov model for early prediction of the elderly’s dependency evolution in ambient assisted living. Ann Telecommun 78(9):599–615
Jung CL, Mahmoud NSA, El Samanoudy G, Al Qassimi N (2022) Evaluating the color preferences for elderly depression in the United Arab Emirates. Buildings 12(2):234. https://doi.org/10.3390/buildings12020234
Kropman D, Appel-Meulenbroek R, Bergefurt L, LeBlanc P (2023) The business case for a healthy office; a holistic overview of relations between office workspace design and mental health. Ergonomics 66(5):658–675
Lee Y, Hwang J, Lim S, Kim JT (2013) Identifying characteristics of design guidelines for elderly care environments from the holistic health perspective. Indoor Built Environ 22(1):242–259. https://doi.org/10.1177/1420326x12471101
Leung MY, Famakin I, Kwok T (2017) Relationships between indoor facilities management components and elderly people’s quality of life: a study of private domestic buildings. Habitat Int 66:13–23. https://doi.org/10.1016/j.habitatint.2017.05.002
Leung MY, Famakin IO, Wang CD (2019a) Developing an integrated indoor built environment-quality of life model for the elderly in public and subsidized housing. Eng Constr Arch Manag 26(7):1498–1517. https://doi.org/10.1108/ecam-02-2018-0054
Leung MY, Wang CD, Chan IYS (2019b) A qualitative and quantitative investigation of effects of indoor built environment for people with dementia in care and attention homes. Build Environ 157:89–100. https://doi.org/10.1016/j.buildenv.2019.04.019
Leung MY, Sieh L, Yin RZ (2023) An integrated model for luminous environment and quality of life of older people in care and attention homes. Build Environ 244:110821. https://doi.org/10.1016/j.buildenv.2023.110821
Leung MY, Wang C, Li L (2024) Impact of indoor visual environment on emotional and behavioral symptoms of older people with dementia. Build Environ 265:111980
Leung MY, Wang CD, Wei XY (2020) Structural model for the relationships between indoor built environment and behaviors of residents with dementia in care and attention homes. Build Environ 169:106532. https://doi.org/10.1016/j.buildenv.2019.106532
Li CS, Zhou Y (2020) Residential environment and depressive symptoms among Chinese middle-and old-aged adults: a longitudinal population-based study. Health Place 66:102463. https://doi.org/10.1016/j.healthplace.2020.102463
Lindemann U, Oksa J, Skelton DA, Beyer N, Klenk J, Zscheile J, Becker C (2014) Effect of cold indoor environment on physical performance of older women living in the community. Age Ageing 43(4):571–575. https://doi.org/10.1093/ageing/afu057
Liu F, Li YF, Gao XZ, Du JT (2023) The association between perceived housing environment and health and satisfaction among the older adults during the COVID-19 pandemic: a cross-sectional survey in Northern China. Buildings 13(11):2875. https://doi.org/10.3390/buildings13112875
Meade RD, Akerman AP, Notley SR, Kirby NV, Sigal RJ, Kenny GP (2024) Effects of Daylong exposure to indoor overheating on thermal and cardiovascular strain in older adults: a randomized crossover trial. Environ Health Perspect 132(2):027003. https://doi.org/10.1289/ehp13159
Moses L, Morrissey K, Sharpe RA, Taylor T (2019) Exposure to indoor mouldy odour increases the risk of asthma in older adults living in social housing. Int J Environ Res Public Health 16(14):2600
Peters M, Muellmann S, Christianson L, Stalling I, Bammann K, Drell C, Forberger S (2020) Measuring the association of objective and perceived neighborhood environment with physical activity in older adults: challenges and implications from a systematic review. Int J Health Geogr 19:1–20
Qiao DP, Wu SH, Xiang LH, Zhang N (2024) Association of residential environment with depression and anxiety symptoms among older adults in China: a cross-sectional population-based study. Build Environ 257:111535. https://doi.org/10.1016/j.buildenv.2024.111535
Qiu QW, Li J, Li JY, Xu Y (2020) Built form and depression among the Chinese rural elderly: a cross-sectional study. BMJ Open 10(12):e038572. https://doi.org/10.1136/bmjopen-2020-038572
Rodrigues IB, Tariq S, Kouroukis A, Swance R, Adachi J, Bray S et al (2024) Mapping sedentary behaviour (MAPS-B) in winter and spring using wearable sensors, indoor positioning systems, and diaries in older adults who are pre-frail and frail: a feasibility longitudinal study. Plos one 19(5):e0290197
Shishegar N, Boubekri M (2022) Lighting up living spaces to improve mood and cognitive performance in older adults. J Environ Psychol 82:101845. https://doi.org/10.1016/j.jenvp.2022.101845
Shishegar N, Boubekri M, Stine-Morrow EAL, Rogers WA (2021) Tuning environmental lighting improves objective and subjective sleep quality in older adults. Build Environ 204:108096. https://doi.org/10.1016/j.buildenv.2021.108096
Tao YQ, Lau SSY, Gou ZH, Fu JY, Jiang BY, Chen XW (2018) Privacy and well-being in aged care facilities with a crowded living environment: case study of Hong Kong Care and Attention Homes. Int J Environ Res Public Health 15(10):2157. https://doi.org/10.3390/ijerph15102157
Tartarini F, Cooper P, Fleming R, Batterham M (2017) Indoor air temperature and agitation of nursing home residents with dementia. Am J Alzheimers Dis Other Dement 32(5):272–281
The WHOQOL Group (1998) Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychol Med 28(3):551–558. https://doi.org/10.1017/S0033291798006667
Thölking TW, Lamers ECT, Rikkert M (2020) A guiding nightlight decreases fear of falling and increases sleep quality of community-dwelling older people: a quantitative and qualitative evaluation. Gerontology 66(3):295–303. https://doi.org/10.1159/000504883
Tonchoy P, Seangpraw K, Ong-Artborirak P, Kantow S, Auttama N, Choowanthanapakorn M, Boonyathee S (2024) Mental health, fall prevention behaviors, and home environments related to fall experiences among older adults from ethnic groups in rural Northern Thailand. Heliyon 10(17):e37306
Torres A, Serra J, Llopis J, Delcampo A (2020) Color preference cool versus warm in nursing homes depends on the expected activity for interior spaces. Front Arch Res 9(4):739–750. https://doi.org/10.1016/j.foar.2020.06.002
Tricco AC, Lillie E, Zarin W et al (2018) PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169(7):467–473. https://doi.org/10.7326/M18-0850
United Nations (2022) World population prospects 2022. Department of Economic and Social Affairs. https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/wpp2022_summary_of_results.pdf. Accessed 31 July 2024
van Boekel D, Cabrita M, van Staalduinen W, do Rosário Cabrita M, Masiero F, Uriarte SU, Georgoulis D, Dantas C (2024) Dynamic transnational inter-ecosystem framework for smart and inclusive age-friendly environments: The Transnational Local-Sphere Model. Tech Soc Sci J 63(1):279–295. https://doi.org/10.47577/tssj.v63i1.11899
van Eck NJ, Waltman L (2009) How to normalize cooccurrence data? An analysis of some well-known similarity measures. J Am Soc Inf Sci Technol 60(8):1635–1651
van Hoof J, Kort HSM, Duijnstee MSH, Rutten PGS, Hensen JLM (2010) The indoor environment and the integrated design of homes for older people with dementia. Build Environ 45(5):1244–1261. https://doi.org/10.1016/j.buildenv.2009.11.008
Wang CD, Leung MY (2023) Effects of subjective perceptions of indoor visual environment on visual-related physical health of older people in residential care homes. Build Environ 237:110301. https://doi.org/10.1016/j.buildenv.2023.110301
Wang Z, Yu H, Luo M, Wang Z, Zhang H, Jiao Y (2019) Predicting older people’s thermal sensation in building environment through a machine learning approach: Modelling, interpretation, and application. Build Environ 161:106231. https://doi.org/10.1016/j.buildenv.2019.106231
Wu S, Fu Y, Yang Z (2022) Housing condition, health status, and age-friendly housing modification in Europe: the last resort? Build Environ 215:108956. https://doi.org/10.1016/j.buildenv.2022.108956
Xiaoxue S, Huang X (2024) Promoting stress and anxiety recovery in older adults: assessing the therapeutic influence of biophilic green walls and outdoor view. Front Public Health 12:1352611. https://doi.org/10.3389/fpubh.2024.1352611
Xiong J, Ma T, Lian ZW, de Dear R (2019) Perceptual and physiological responses of elderly subjects to moderate temperatures. Build Environ 156:117–122. https://doi.org/10.1016/j.buildenv.2019.04.012
Yan D, Guo Q (2023) Effect of indoor wall wood coverage on the elderly group—a case study of activity rooms in old-age buildings. Buildings 13(8):2086
Yang HY, Sanford JA (2012) Home and community environmental features, activity performance, and community participation among older adults with functional limitations. J Aging Res 2012(1):625758. https://doi.org/10.1155/2012/625758
Yang Z, Hotterbeex P, Marent P-J, Cerin E, Thomis M, van Uffelen J (2024) Physical activity, sedentary behaviour, and cognitive function among older adults: a bibliometric analysis from 2004 to 2024. Ageing Res Rev 97:102283. https://doi.org/10.1016/j.arr.2024.102283
Zhang Y, Mei Y, Yu W, Guo M, Li B, Zhou H et al (2024a) Association of indoor dampness indicators with rheumatic diseases/symptoms in older adults: a comparative cross-sectional study in Chongqing and Beijing. Environ Sci Pollut Res 31(8):11633–11646
Zhang Y, Yu W, Zhou H, Guo M, Wang C, Li B, Yang X (2024b) The impact of residential winter HVAC usage behavior on arthritis in older adults: a PLS-SEM analysis. J Build Eng 98:111137
Zheng Z, Wang Y, Chen L, Sun N, Huang W (2024) The influence of residential facilities on depression and frailty of the elderly in rural China: evidence from the China health and retirement longitudinal study. Front Arch Res 13(6):1215–1227
Zhou HX, Yu W, Zhao KY, Shan HY, Zhou S, Wei S, Ouyang LY (2024) Thermal demand characteristics of elderly people with varying levels of frailty in residential buildings during the summer. J Build Eng 84:108654. https://doi.org/10.1016/j.jobe.2024.108654
Zhou JJ, Kang R, Bai X (2022) A meta-analysis on the influence of age-friendly environments on older adults’ physical and mental well-being. Int J Environ Res Public Health 19(21):13813
Zhou S, Li B, Du C, Yao R, Ouyang L, Zhou H, Kosonen R, Melikov AK, Shang L, Liu H (2023) Developing thermal prediction models for the elderly under temperature step changes. Build Environ 245:110902. https://doi.org/10.1016/j.buildenv.2023.110902
Figueiro MG, Pedler D, Plitnick B, Zecena E, Leahy S (2023) Tailored lighting intervention (TLI) for improving sleep-wake cycles in older adults living with dementia. Front Physiol 14:1290678
Acknowledgements
The authors are grateful for the funding supported by the National Science and Technology Council (NSTC) in Taiwan, under grant no. 113-2221-E-011-040-MY2.
Author information
Authors and Affiliations
Contributions
Yu-Wei Yu: conceptualization, methodology, formal analysis, investigation, data curation, writing—original draft. Yi-Kai Juan: conceptualization, methodology, resources, writing—review & editing, supervision, funding acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The ethical approval was not required, as the study conducted did not involve any ethical concerns or issues.
Informed consent
This article does not contain any studies with human participants performed by any of the authors. Informed consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yu, YW., Juan, YK. Impact of interior design factors on the physical, physiological, and mental health of older adults—a scoping review. Humanit Soc Sci Commun 12, 956 (2025). https://doi.org/10.1057/s41599-025-05332-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1057/s41599-025-05332-7