Abstract
Social interaction is essential for human survival and well-being; however, aging often increases the risk of loneliness alongside cognitive changes. While research on aging has highlighted loneliness as a marker of various cognitive stages, the precise role of loneliness as a mediator of cognitive deficit in individuals with mild cognitive impairment (MCI) remains unclear. A total of 155 older adults ranging from 60 to 90 years old participated in this study, with 75 individuals diagnosed with MCI and 80 healthy controls. Outcome measures included MMSE, the Geriatric Depression Scale, and a standardized battery of neurocognitive functioning tests. In comparison to the health controls, individuals with MCI exhibited higher levels of perceived loneliness and depressive symptoms. Additionally, they demonstrated poorer performance on various neurocognitive tests. Perceived loneliness showed a positive association with depressive symptoms and a negative correlation with performance on tests assessing forward/backward digit span, vocabulary, similarity, symbol substitution, and color trails. The mediation analysis indicated that perceived loneliness significantly mediated the relationship between MCI status and executive function performance, accounting for approximately 6% of the total effect. These findings highlight the potential role of loneliness as a contributing psychosocial factor associated with cognitive performance in individuals with MCI. This understanding may inform future directions for disease monitoring and the design of targeted interventions in clinical trials addressing neurodegenerative conditions.
Similar content being viewed by others
Introduction
Beyond the absence of physical disability and disease, successful aging requires maintaining overall cognitive function (Depp et al., 2010; Tabbarah et al., 2002), which is linked to social engagement and well-being (Dause & Kirby, 2019; Zhou et al., 2020). While advances in aging-related healthcare have increased life expectancy (Lindgren, 2016; Lubitz et al., 2001), significant public health challenges persist in the form of cognitive impairments such as mild cognitive impairment (MCI) (Luck et al., 2010; Prince et al., 2013). MCI is more appropriately considered an intermediate state between normal cognitive aging and dementia, characterized by noticeable cognitive deficits that do not substantially interfere with daily functioning (Langa & Levine, 2014; Petersen & Negash, 2008). Although individuals with MCI are at increased risk for developing Alzheimer’s disease and related dementias, many do not progress to dementia. Some individuals meet the criteria for MCI due to non-progressive conditions, such as psychiatric disorders or medical illnesses, and may remain stable over time without further cognitive decline (Langa & Levine, 2014).
Understanding the factors influencing this progression is crucial for developing preventive strategies to mitigate severe cognitive decline among the aging population.
Various medical conditions and lifestyle factors have been identified as risk factors for MCI, including hypertension, diabetes, physical inactivity, smoking, and alcohol consumption (Eshkoor et al., 2015; Etgen et al., 2011). Interestingly, studies also link MCI with social and psychological problems, such as low social contact (Gardener et al., 2021), which can lead to loneliness (Yu et al., 2016). Loneliness, characterized as the subjective feeling of social isolation or lack of companionship, is common among older adults (Crewdson, 2016; Van As et al., 2022). As individuals age, they may experience life changes like retirement, loss of friends and family, children leaving home, and physical health challenges, all of which contribute to loneliness and isolation (Cohen-Mansfield et al., 2016; Cotterell et al., 2018). Furthermore, societal factors such as ageism and limited access to transportation or social activities can compound feelings of loneliness among older adults (Van Den Berg et al., 2016).
The significant link between loneliness and MCI can be explained through several mechanisms. Individuals who experience loneliness often undergo psychological distress (Taylor et al., 2018) and depression (Erzen & Çikrikci, 2018), which can contribute to neurodegenerative issues such as increased oxidative stress, dysregulation of the immune system, and overexpression of proinflammatory genes (Bakunina et al., 2015; Bhatt et al., 2020; Black et al., 2015). Moreover, lonely individuals frequently engage in health-damaging behaviors, including physical inactivity, poor dietary habits, reluctance to adhere to healthcare recommendations, and disrupted sleep patterns (Christiansen et al., 2016; Segrin & Passalacqua, 2010), all of which have been linked to accelerated cognitive deficits (Dominguez et al., 2021; Koch et al., 2019). Additionally, social isolation can result in a lack of cognitive and sensory stimulation, thereby contributing to an overall decline in cognitive function (Lautenschlager et al., 2008; Pitkala et al., 2011).
Studies specifically focusing on loneliness among individuals with MCI are relatively limited. Lara et al. (2019) conducted a meta-analysis, analyzing longitudinal studies to explore the relationship between loneliness and both MCI and dementia (Lara et al., 2019). The findings revealed a positive correlation between loneliness and dementia, consistent with previous research demonstrating a robust link between loneliness and various cognitive functions (Boss et al., 2015). However, the study by Lara et al. (2019) highlighted a lack of substantial evidence regarding the impact of loneliness on MCI, with only three relevant studies identified, none of which specifically examined the association between loneliness and MCI. Recent studies have investigated the influence of loneliness on individuals with MCI, focusing on demographic variations (Smith et al., 2021) or the adverse consequences of loneliness on mental health issues associated with MCI, such as decreased quality of life (Zafar et al., 2021).
Our study aimed to examine whether perceived loneliness mediates the relationship between MCI status and cognitive performance compared to cognitively normal individuals. We incorporated various cognitive domains, such as executive function, memory, and verbal fluency, to provide comprehensive insight into how cognitive performance is influenced among lonely individuals with MCI. We used loneliness scores as mediators of the effect of MCI on these cognitive domains. This methodology enabled us to gain a more nuanced understanding of whether loneliness plays a distinctive role in the deterioration of different cognitive domains among individuals with MCI.
Methods
Participants
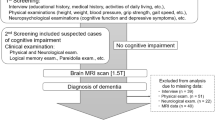
The study included 75 individuals with MCI (29 females) and 80 healthy controls (37 females). Participants for the MCI group were recruited from a medical center in Northern Taiwan and met the 2011 National Institute on Aging-Alzheimer’s Association (NIA-AA) criteria with a Clinical Dementia Rating (CDR) score of 0.5, confirmed by experienced and certified physicians and a clinical psychologist (Albert et al., 2011). The healthy control group (HC group) consisted of individuals with no history of neurological or psychiatric disorders, no signs of cognitive decline, a CDR score of 0, and a Mini-Mental State Examination (MMSE) score above the cutoff for their age and educational level (Uhlmann & Larson, 1991). Exclusion criteria for both groups included major psychiatric illnesses, other neurodegenerative disorders, brain trauma, active malignancy, recent hospitalization, or persistent infections. All participants had normal corrected vision and bilateral peripheral hearing.
Variables
Predictor variable
Group status (MCI vs. healthy control) was determined based on clinical evaluation, including scores on the Clinical Dementia Rating (CDR) (Morris, 1993) and Mini-Mental State Examination (MMSE) (Folstein et al., 1975), which assessed global cognitive and functional ability.
Outcome variables
Perceived loneliness was assessed using the UCLA Loneliness Scale (Russell et al., 1978), a widely validated instrument for evaluating subjective social isolation. Depressive symptoms were assessed using the Geriatric Depression Scale (GDS) (Yesavage et al., 1982). To characterize participants’ broader cognitive performance, a comprehensive neuropsychological test battery was administered. This included the forward and backward digit span, vocabulary, similarities, symbol substitution, and symbol search subtests from the Wechsler Adult Intelligence Scale (Wechsler, 1997), as well as semantic verbal fluency tasks involving categories such as animals, vegetables, fruits, and towns (Isaacs & Kennie, 1973). Executive function was assessed using the Color Trails Test (CTT) (Reitan & Wolfson, 1985), specifically the completion times for Part A (CTT-A) and Part B (CTT-B), which evaluates attention, processing speed, and mental flexibility. The time taken to complete each part of the CTT was recorded in seconds.
Statistical analysis
To compare demographic characteristics between the healthy control (HC) and mild cognitive impairment (MCI) groups, chi-square tests were used for categorical variables and independent-samples t-tests for continuous variables. For neuropsychological measures, analyses of covariance (ANCOVA) were conducted to evaluate group differences, with age and years of education included as covariates. Furthermore, initial exploratory analyses were conducted to examine correlations among all continuous variables. Partial correlations controlling for age and education were then performed to assess the associations between UCLA Loneliness Scale scores and neuropsychological test scores across all participants; the results were documented in a correlation matrix. Effect sizes for t-tests and ANCOVA were calculated using Cohen’s d and eta squared (η²), respectively. Statistical significance was set at p < 0.05. Adjusted R² values were also reported where applicable.
Mediation analysis
If our results show a significant association among the MCI-HC group difference, levels of loneliness, and performance on the neuropsychological assessments, we would conduct mediation analysis using a Matlab-based toolbox developed by Wager and colleagues (Wager et al., 2008). Following the mediation effect conceptual framework (Gunzler et al., 2013), the groups involved in this study would be assigned as the predictor variable, each independent neuropsychological test score as the outcome variable, and the UCLA loneliness score as the mediator variable. Mediation analyses were performed in a step-by-step manner. Path a estimates the effects of the predictor variable (i.e., group difference) on the mediator variable (i.e., the UCLA loneliness score). Path b denotes the link where the mediator must be directly related to the outcome (i.e., each neuropsychological test), controlling for the predictor. The mediation effect (a*b) must be significant, which involves testing the product of the path a and b coefficients. Alternatively, the inclusion of the mediator in the path model should significantly diminish the predictor-outcome association. The c effect represents the overall predictor-outcome relationship, while c’ denotes the direct effect controlling for the mediator. The significance of the a*b effect is tested against the difference between c and c’. The bootstrap method was used to determine statistical significance.
Results
Demographic information and neuropsychological evaluations
Table 1 displays the demographic and neuropsychological data for both the HC and MCI groups. Since age and years of education differed significantly between the groups, these demographic factors were used as covariates in the analysis of group differences across psychosocial variables (loneliness and depression). For cognitive variables, age, education, and depression were included as covariates in the ANCOVA models. Overall, individuals with MCI exhibited higher levels of loneliness and more severe depressive symptoms compared to the healthy controls. As expected, the MCI cohort demonstrated pronounced cognitive impairments across all neuropsychological assessments when controlling age and education (see Table 1 and Fig. 1). Specifically, the MCI group scored lower on the MMSE, forward and backward digit span, semantic verbal fluency, vocabulary, similarity, symbol substitution, and symbol search tests, with effect sizes ranging from medium to large. Additionally, participants in the MCI group took significantly longer to complete parts A and B of the CTT, with large effect sizes indicating substantial differences compared to the health controls.
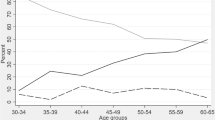
Correlations between loneliness and neuropsychological performance
The correlation analyses and descriptive statistics are presented in Table 2 and Fig. 2. We found that increased loneliness was associated with the lower performance on various cognitive tests, including the MMSE, forward digit span test, vocabulary test, similarity test, symbol substitution test, and symbol search test, even after controlling for age and education. Furthermore, higher levels of loneliness were also associated with a greater severity of depressive symptoms and longer completion times for parts A and B of CTT.
Scatterplots illustrate the correlations between UCLA Loneliness Scale scores and performance across a range of cognitive tests as well as scores on the Geriatric Depression Scale. Trend lines with 95% confidence intervals (shaded areas) are included for visual reference. Higher loneliness scores were generally correlated with poorer cognitive performance and greater depressive symptoms. **p < 0.01; *p < 0.05.
Mediation analysis results
Thus far, we have observed three significant findings: (1) a significant group difference in neuropsychological test performance; (2) a significant group difference in UCLA loneliness scale scores; and (3) significant associations between levels of loneliness and performance on the neuropsychological tests. Based on these statistically significant results, we conducted mediation analysis using bootstrap resampling. The mediation analysis revealed that loneliness significantly mediates the relationship between the MCI-HC group difference and performance on part A (a = 4.19, SE = 1.18, p < 0.001; b = 1.25, SE = 0.57, p = 0.01; c = 93.02, SE = 8.12, p < 0.001; c’ = 87.63, SE = 8.18, p < 0.001; ab = 5.38, Z = 2.59, p = 0.01). While the total effect (c) of group status on executive function performance was significant, the proportion of the effect mediated by perceived loneliness was calculated using the formula (ab/c). This analysis indicated that loneliness accounted for approximately 5.78% of the total effect on CTT-A, suggesting a modest but measurable indirect contribution of loneliness to the observed group differences in executive functioning. Regarding Part B of the Color Trails Test (CTT-B), the mediation analysis revealed significant effects for path a (a = 4.13, SE = 1.18, p < 0.001), path b (b = 2.17, SE = 1.09, p = 0.03), the total effect (c = 154.88, SE = 12.10, p < 0.001), and the direct effect (c’ = 145.50, SE = 11.23, p < 0.001). The indirect effect (ab = 9.39) was also significant (Z = 2.29, p = 0.02), indicating that perceived loneliness mediated approximately 6.06% of the total effect (see Figs. 3, 4). This suggests that increased levels of loneliness in individuals with MCI may contribute to a greater deficit in executive function performance, as evidenced by longer CTT completion times. However, analyses using loneliness as the mediator between the MCI-HC group difference and the rest of the neuropsychological tests did not yield significant results.
The path diagram in A shows the group label as the predictor variable (denoted as X), the UCLA loneliness scale scores as the mediator variable (denoted as M), and scores on parts A of the color trails tests (CTT) as the outcome variable (denoted as Y). The paths a and b represent the relationships between X and M and between M and X, respectively. The path a*b represents the mediation effect. The paths c and c’ respectively represent the total and indirect effects of the group on the CTT performance, and the latter was evaluated when the mediator variable was considered. The path coefficients and their standard errors were labeled above the paths. The relationships in the paths a, b, and c are visualized in B. The bootstrap method was used for each path to define 97.5% confidence intervals in the histograms shown in panel C (two-tailed). **p < 0.001; *p < 0.05.
The path diagram in A shows the group label as the predictor variable (denoted as X), the UCLA loneliness scale scores as the mediator variable (denoted as M), and scores on parts B of the color trails tests (CTT) as the outcome variable (denoted as Y). The paths a and b represent the relationships between X and M and between M and X, respectively. The path a*b represents the mediation effect. The paths c and c’ respectively represent the total and indirect effects of the group on the CTT performance, and the latter was evaluated when the mediator variable was considered. The path coefficients and their standard errors were labeled above the paths. The relationships in the paths a, b, and c are visualized in B. The bootstrap method was used for each path to define 97.5% confidence intervals in histograms shown in panel C (two-tailed). **p < 0.001; *p < 0.05.
Discussion
In this study, we found that individuals with MCI exhibited significantly higher levels of perceived loneliness and depressive symptoms compared to healthy controls. They also performed worse on a variety of neurocognitive tests, including those assessing executive function, memory, and processing speed. Importantly, our mediation analysis revealed that perceived loneliness significantly mediated the relationship between MCI and executive function performance. These findings suggest that loneliness may be an important psychosocial factor associated with cognitive functioning in individuals with MCI, underscoring the potential value of addressing loneliness in efforts to support cognitive health in this population.
The previous systematic review and meta-analysis explicitly mentioned that the evidence for the potential detrimental effect of loneliness on MCI is limited (Lara et al., 2019). Therefore, exploring whether and how loneliness influences cognitive impairment among individuals with MCI is a worthwhile scientific pursuit. In the current study, we found that the MCI group exhibited significantly lower performance on various cognitive tests compared to the healthy control group. This finding aligns with previous studies that have reported a significant association between loneliness and the deficits in overall cognitive functions, particularly among older adults (Boss et al., 2015; Crewdson, 2016) (Zhou et al., 2022). Furthermore, severe cognitive deterioration may hinder individuals with MCI from engaging in social activities, leading to feelings of loneliness (Lydon et al., 2021; Penninkilampi et al., 2018). This lack of social engagement deprives individuals with MCI of cognitive stimulation, thereby exacerbating cognitive decline (Lautenschlager et al., 2008; Pitkala et al., 2011). Thus, loneliness shows a pattern of association with cognitive difficulties similar to that observed for other mental health conditions in older adults, such as depression (Ismail et al., 2017; Ma, 2020). This is consistent with our finding that depression levels in the MCI group significantly differed from those in the healthy control group.
While previous studies generally focused on the direct effect of loneliness on MCI or the decline of global cognitive functions among individuals with MCI (Lara et al., 2019; Mian et al., 2024), the current study further examined the role of loneliness in mediating the relationship between group differences (i.e., MCI vs. HC) and performance on each neuropsychological test included in this study. Interestingly, although the level of loneliness was associated with scores on all neurocognitive measures, the indirect effect of loneliness was significant only for CTT Part A and Part B. Both parts of the CTT measure visual search, attention, and processing speed, with Part B specifically assessing cognitive flexibility, all components of executive function (Arbuthnott & Frank, 2000). The finding that perceived loneliness significantly mediated the relationship between MCI status and reaction time on the CTT, but not on other neuropsychological measures, suggests a domain-specific association. Executive functions assessed by the CTT—such as cognitive flexibility, processing speed, and attentional shifting—are particularly sensitive to early cognitive vulnerability and psychosocial stressors like loneliness. In contrast, tasks measuring crystallized intelligence or basic memory functions, which are often more resilient to emotional states and preserved in early MCI (Salmon & Bondi, 2009), showed no such mediation. Furthermore, reaction time tasks like the CTT may be more sensitive to subtle psychophysiological states linked to loneliness, while the fine-grained continuous measurement of CTT performance may have captured effects undetectable by other neuropsychological tests. These findings highlight that the association between loneliness and cognitive function in MCI may be most pronounced within executive and attentional domains rather than across all cognitive systems.
The mediating role of loneliness suggests that social exposure significantly influences executive function. Since executive function may involve a speeded motor component (Hayden & Welsh-Bohmer, 2012), as tested in CTT, the experience of social isolation and the resulting lack of motor activity among lonely older adults with MCI may contribute to the progression of executive function deterioration. This aligns with previous neuroscientific findings indicating that decreased frontal lobe white matter volume among older adults experiencing loneliness predicts lower performance in executive function, also tested using CTT Parts A and B (Lee et al., 2024). Furthermore, the feeling of loneliness is strongly associated with a sense of not mattering and devaluing the presence of others (McComb et al., 2020). The isolation and lack of social support among lonely older adults with MCI may be linked to greater deficits across various cognitive functions through their association with increased feelings of loneliness (Piette et al., 2023). This is consistent with previous studies, which found that caring for and valuing others predicts lower loneliness while also being associated with higher executive function (Somers et al., 2022).
Despite providing evidence that loneliness significantly mediates the effect of MCI on executive function performance, we acknowledge that not all previous studies have shown consistent findings. For instance, McVeigh et al. (2023) found no association between loneliness and social isolation with executive function among cognitively healthy older adults (McVeigh et al., 2023). This suggests that the mediating effect of loneliness may be exclusive to speeded-time-based executive functions, such as those assessed by CTT Parts A and B. Furthermore, unlike those with healthy cognitive functions, older adults with MCI may experience a dramatic shift from normal to impaired cognitive function, impairing their adaptability to their social context (Halpin et al., 2017). This could explain why loneliness has a different effect on executive function deterioration in individuals with MCI compared to cognitively healthy older adults. However, this claim warrants future exploration, possibly using a longitudinal approach. Additionally, we noted that the variables used in this study are not uniform. The predictor (i.e., MCI vs. HC group) is a binary variable, while the other variables are continuous. Although using the original CDR score (i.e., the score to sort the MCI group) to create a continuous MCI-related predictor is technically feasible, we decided to use the grouping as it is deemed more clinically relevant.
Finally, our findings underscore the significant impact of loneliness on the deterioration of various cognitive domains, particularly executive function. We recognize that loneliness is a complex social phenomenon. Addressing this social-psychological issue may be less straightforward than tackling the medical risk factors of MCI, which often involve intricate interactions between individuals, their environments, and personal beliefs and behaviors. Moreover, these factors may be influenced by societal norms, cultural values, and access to resources, which can vary widely across different populations (Barreto et al., 2021; de Jong Gierveld & Tesch-Römer, 2012). Therefore, addressing loneliness among older adults with MCI may necessitate a multi-faceted approach encompassing community outreach, social support programs, and mental health services. This can pose challenges due to limited resources, the stigma associated with cognitive decline, and the need for sustained, long-term efforts to achieve meaningful improvement (Lydon et al., 2021).
Limitations
Several limitations of this study must be noted. First, due to the cross-sectional design, the directionality of the relationship between loneliness and executive function in individuals with MCI must be interpreted with caution. Our findings cannot establish whether loneliness causes executive function problems or decline. Second, although we controlled for depressive symptoms and observed sustained results, other potential confounding factors that may influence both MCI status and executive function performance should be considered in future research. For instance, depressive symptoms commonly fluctuate over time in individuals with MCI and are strongly associated with executive dysfunction, primarily through their impact on motivation, attention, working memory, and prefrontal cortex functioning. Similarly, sleep disturbances, which are prevalent in individuals with MCI, have been linked to impaired executive processes due to neuroinflammation and frontal lobe dysfunction. Finally, reduced social support or engagement—conceptually related but distinct from loneliness—has been associated with poorer executive performance and increased cognitive vulnerability in older adults. Future studies should more comprehensively account for these and other covariates related to loneliness, MCI, and executive function to better clarify the observed associations. Finally, although we employed a Monte Carlo simulation approach with 10,000 iterations to assess the statistical significance of the indirect effect, which is considered to provide adequate precision and statistical power for detecting mediation effects (Schoemann et al., 2020; Wager et al., 2008), the relatively small sample size remains a limitation. Future studies with larger samples and longitudinal designs are recommended to further validate these findings and strengthen causal inferences.
Conclusion
Our findings are consistent with previous research indicating that feelings of loneliness are predictive of various cognitive dysfunctions among individuals with MCI. However, our study provides a novel contribution by demonstrating that loneliness significantly mediates the relationship between MCI and executive function, but not other cognitive domains. This suggests that loneliness may be more closely linked to executive function difficulties than to impairments in other cognitive areas, highlighting a specific pathway through which social factors could be related to cognitive outcomes in MCI. Therefore, medical efforts to address MCI may benefit from considering loneliness as a complex social phenomenon potentially influencing therapeutic outcomes for individuals with MCI.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to the inclusion of clinical patient data. However, the data may be made available by the corresponding author upon reasonable request and subject to appropriate institutional and ethical approvals.
References
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, Gamst A, Holtzman DM, Jagust WJ, Petersen RC, Snyder PJ, Carrillo MC, Thies B, Phelps CH (2011) The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7(3):270–279. https://doi.org/10.1016/j.jalz.2011.03.008
Arbuthnott K, Frank J (2000) Trail making test, part B as a measure of executive control: validation using a set-switching paradigm. J Clin Exp Neuropsychol 22(4):518–528. https://doi.org/10.1076/1380-3395(200008)22:4;1-0;ft518
Bakunina N, Pariante CM, Zunszain PA (2015) Immune mechanisms linked to depression via oxidative stress and neuroprogression. Immunology 144(3):365–373. https://doi.org/10.1111/imm.12443
Barreto M, Victor C, Hammond C, Eccles A, Richins MT, Qualter P (2021) Loneliness around the world: Age, gender, and cultural differences in loneliness. Pers Individ Dif 169:110066. https://doi.org/10.1016/j.paid.2020.110066
Bhatt S, Nagappa AN, Patil CR (2020) Role of oxidative stress in depression. Drug Discov today 25(7):1270–1276. https://doi.org/10.1016/j.drudis.2020.05.001
Black CN, Bot M, Scheffer PG, Cuijpers P, Penninx BW (2015) Is depression associated with increased oxidative stress? A systematic review and meta-analysis. Psychoneuroendocrinology 51:164–175. https://doi.org/10.1016/j.psyneuen.2014.09.025
Boss L, Kang D-H, Branson S (2015) Loneliness and cognitive function in the older adult: a systematic review. Int Psychogeriatr 27(4):541–553. https://doi.org/10.1017/s1041610214002749
Christiansen J, Larsen FB, Lasgaard M (2016) Do stress, health behavior, and sleep mediate the association between loneliness and adverse health conditions among older people. Soc Sci Med 152:80–86. https://doi.org/10.1016/j.socscimed.2016.01.020
Cohen-Mansfield J, Hazan H, Lerman Y, Shalom V (2016) Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int Psychogeriatr 28(4):557–576. https://doi.org/10.1017/s1041610215001532
Cotterell N, Buffel T, Phillipson C (2018) Preventing social isolation in older people. Maturitas 113:80–84. https://doi.org/10.1016/j.maturitas.2018.04.014
Crewdson JA (2016) The effect of loneliness in the elderly population: A review. Healthy Aging & Clinical Care in the Elderly 8:1. https://doi.org/10.4137/hacce.s35890
Dause TJ, Kirby ED (2019) Aging gracefully: social engagement joins exercise and enrichment as a key lifestyle factor in resistance to age-related cognitive decline. Neural Regen Res 14(1):39–42. https://doi.org/10.4103/1673-5374.243698
de Jong Gierveld J, Tesch-Römer C (2012) Loneliness in old age in Eastern and Western European societies: theoretical perspectives. Eur J Ageing 9(4):285–295. https://doi.org/10.1007/s10433-012-0248-2
Depp C, Vahia IV, Jeste D (2010) Successful aging: focus on cognitive and emotional health. Annu Rev Clin Psychol 6:527–550. https://doi.org/10.1146/annurev.clinpsy.121208.131449
Dominguez LJ, Veronese N, Vernuccio L, Catanese G, Inzerillo F, Salemi G, Barbagallo M (2021) Nutrition, physical activity, and other lifestyle factors in the prevention of cognitive decline and dementia. Nutr 13(11):4080. https://doi.org/10.3390/nu13114080
Erzen E, Çikrikci Ö (2018) The effect of loneliness on depression: A meta-analysis. Int J Soc Psychiatry 64(5):427–435. https://doi.org/10.1177/0020764018776349
Eshkoor SA, Hamid TA, Mun CY, Ng CK (2015) Mild cognitive impairment and its management in older people. Clin Interv Aging 687-693. https://doi.org/10.2147/cia.s73922
Etgen T, Sander D, Bickel H, Förstl H (2011) Mild cognitive impairment and dementia: the importance of modifiable risk factors. Dtsch Ärzteblatt Int 108(44):743. https://doi.org/10.3238/arztebl.2011.0743
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198. https://doi.org/10.1016/0022-3956(75)90026-6
Gardener H, Levin B, DeRosa J, Rundek T, Wright CB, Elkind MS, Sacco RL (2021) Social connectivity is related to mild cognitive impairment and dementia. J Alzheimer’s Dis 84(4):1811–1820. https://doi.org/10.3233/jad-210519
Gunzler D, Chen T, Wu P, Zhang H (2013) Introduction to mediation analysis with structural equation modeling. Shanghai Arch Psychiatry 25(6):390–394. https://doi.org/10.3969/j.issn.1002-0829.2013.06.009
Halpin SN, Dillard RL, Puentes WJ (2017) Socio-emotional adaptation theory: charting the emotional process of Alzheimer’s disease. Gerontologist 57(4):696–706. https://doi.org/10.1093/geront/gnw046
Hayden KM, Welsh-Bohmer KA (2012) Epidemiology of cognitive aging and Alzheimer’s disease: contributions of the cache county utah study of memory, health and aging. Curr Top Behav Neurosci 10:3–31. https://doi.org/10.1007/7854_2011_152
Isaacs B, Kennie AT (1973) The Set test as an aid to the detection of dementia in old people. Br J Psychiatry 123(575):467–470. https://doi.org/10.1192/bjp.123.4.467
Ismail Z, Elbayoumi H, Fischer CE, Hogan DB, Millikin CP, Schweizer T, Mortby ME, Smith EE, Patten SB, Fiest KM (2017) Prevalence of depression in patients with mild cognitive impairment: a systematic review and meta-analysis. JAMA Psychiatry 74(1):58–67. https://doi.org/10.1001/jamapsychiatry.2016.3162
Koch M, Fitzpatrick AL, Rapp SR, Nahin RL, Williamson JD, Lopez OL, DeKosky ST, Kuller LH, Mackey RH, Mukamal KJ (2019) Alcohol consumption and risk of dementia and cognitive decline among older adults with or without mild cognitive impairment. JAMA Netw Open 2(9):e1910319. https://doi.org/10.1001/jamanetworkopen.2019.10319
Langa KM, Levine DA (2014) The diagnosis and management of mild cognitive impairment: a clinical review. Jama 312(23):2551–2561. https://doi.org/10.1001/jama.2014.13806
Lara E, Martín-María N, De la Torre-Luque A, Koyanagi A, Vancampfort D, Izquierdo A, Miret M (2019) Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Res Rev 52:7–16. https://doi.org/10.1016/j.arr.2019.03.002
Lautenschlager NT, Cox KL, Flicker L, Foster JK, Van Bockxmeer FM, Xiao J, Greenop KR, Almeida OP (2008) Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease: a randomized trial. Jama 300(9):1027–1037. https://doi.org/10.1001/jama.300.9.1027
Lee H, Yong SY, Choi H, Yoon GY, Koh S (2024) Association between loneliness and cognitive function, and brain volume in community-dwelling elderly. Front Aging Neurosci 16:1389476. https://doi.org/10.3389/fnagi.2024.1389476
Lindgren B (2016) The rise in life expectancy, health trends among the elderly, and the demand for health and social care. Stockholm: The National Institute of Economic Research (NIER), 38. https://www.konj.se/media/i51ncnuz/working-paper-142-the-rise-in-life-expectancy-health-trends-among-the-elderly-and-the-demand-for-health-and-social-care.pdf
Lubitz J, Greenberg LG, Gorina Y, Wartzman L, Gibson D (2001) Three decades of health care use by the elderly, 1965–1998. Health Aff 20(2):19–32. https://doi.org/10.1377/hlthaff.20.2.19
Luck T, Luppa M, Briel S, Riedel-Heller SG (2010) Incidence of mild cognitive impairment: a systematic review. Dement Geriatr Cogn Disord 29(2):164–175. https://doi.org/10.1159/000272424
Lydon EA, Nguyen LT, Nie Q, Rogers WA, Mudar RA (2021) An integrative framework to guide social engagement interventions and technology design for persons with mild cognitive impairment. Front Public Health 9:750340. https://doi.org/10.3389/fpubh.2021.750340
Ma L (2020) Depression, anxiety, and apathy in mild cognitive impairment: current perspectives. Front Aging Neurosci 12:9. https://doi.org/10.3389/fnagi.2020.00009
McComb SE, Goldberg JO, Flett GL, Rose AL (2020) The double jeopardy of feeling lonely and unimportant: state and trait loneliness and feelings and fears of not mattering. Front Psychol 11:563420. https://doi.org/10.3389/fpsyg.2020.563420
McVeigh KS, Mehl MR, Polsinelli AJ, Moseley SA, Sbarra DA, Glisky EL, Grilli MD (2023) Loneliness and social isolation are not associated with executive functioning in a cross-sectional study of cognitively healthy older adults. Aging Neuropsychol Cogn 1–18. https://doi.org/10.1080/13825585.2023.2270208
Mian M, Tahiri J, Eldin R, Altabaa M, Sehar U, Reddy PH (2024) Overlooked cases of mild cognitive impairment: implications to early Alzheimer’s disease. Ageing Res Rev, 102335. https://doi.org/10.1016/j.arr.2024.102335
Morris JC (1993) The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology 43(11):2412–2414. https://doi.org/10.1212/wnl.43.11.2412-a
Penninkilampi R, Casey AN, Singh MF, Brodaty H (2018) The association between social engagement, loneliness, and risk of dementia: a systematic review and meta-analysis. J Alzheimers Dis 66(4):1619–1633. https://doi.org/10.3233/jad-180439
Petersen RC, Negash S (2008) Mild cognitive impairment: an overview. CNS Spectr 13(1):45–53. https://doi.org/10.1017/s1092852900016151
Piette JD, Roberts JS, Marinec N, Chen J, Yon S, Maly M, Swalwell K, Hampstead B (2023) Providing a purposeful and stimulating volunteer opportunity for older adults with mild cognitive impairment: a pilot study. Alzheimer Dis Assoc Disord 37(2):149–151. https://doi.org/10.1097/WAD.0000000000000528
Pitkala KH, Routasalo P, Kautiainen H, Sintonen H, Tilvis RS (2011) Effects of socially stimulating group intervention on lonely, older people’s cognition: a randomized, controlled trial. Am J Geriatr Psychiatry 19(7):654–663. https://doi.org/10.1097/jgp.0b013e3181f7d8b0
Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP (2013) The global prevalence of dementia: a systematic review and metaanalysis. Alzheimer’s Dement 9(1):63–75.e62. https://doi.org/10.1016/j.jalz.2012.11.007
Reitan RM, Wolfson D (1985) The Halstead-Reitan neuropsychological test battery: Theory and clinical interpretation. https://www.scirp.org/reference/referencespapers?referenceid=1420410
Russell D, Peplau LA, Ferguson ML (1978) Developing a measure of loneliness. J Pers Assess 42(3):290–294. https://doi.org/10.1207/s15327752jpa4203_11
Salmon DP, Bondi MWJA R. O. P. (2009) Neuropsychological assessment of dementia. 60(1), 257–282 https://doi.org/10.1146/annurev.psych.57.102904.190024
Schoemann A, Boulton A, Short S (2020) Monte Carlo power analysis for indirect effects
Segrin C, Passalacqua SA (2010) Functions of loneliness, social support, health behaviors, and stress in association with poor health. Health Commun 25(4):312–322. https://doi.org/10.1080/10410231003773334
Smith L, Bloska J, Jacob L, Barnett Y, Butler L, Trott M, Odell‐Miller H, Veronese N, Kostev K, Bettac EL (2021) Is loneliness associated with mild cognitive impairment in low‐and middle‐income countries? Int J Geriatr Psychiatry 36(9):1345–1353. https://doi.org/10.1002/gps.5524
Somers CL, Gill-Scalcucci S, Flett GL, Nepon T (2022) The utility of brief mattering subscales for adolescents: Associations with learning motivations, achievement, executive function, hope, loneliness, and risk behavior. J Psychoeduc Assess 40(1):108–124. https://doi.org/10.1177/07342829211055342
Tabbarah M, Crimmins EM, Seeman TE (2002) The relationship between cognitive and physical performance: MacArthur Studies of Successful Aging. J Gerontol Ser A: Biol Sci Med Sci 57(4):M228–M235. https://doi.org/10.1093/gerona/57.4.m228
Taylor HO, Taylor RJ, Nguyen AW, Chatters L (2018) Social isolation, depression, and psychological distress among older adults. J Aging Health 30(2):229–246. https://doi.org/10.1177/0898264316673511
Uhlmann RF, Larson EB (1991) Effect of education on the mini-mental state examination as a screening test for dementia. J Am Geriatr Soc 39(9):876–880. https://doi.org/10.1111/j.1532-5415.1991.tb04454.x
Van As BAL, Imbimbo E, Franceschi A, Menesini E, Nocentini A (2022) The longitudinal association between loneliness and depressive symptoms in the elderly: a systematic review. Int Psychogeriatr 34(7):657–669. https://doi.org/10.1017/s1041610221000399
Van Den Berg P, Kemperman A, De Kleijn B, Borgers A (2016) Ageing and loneliness: The role of mobility and the built environment. Travel Behav Soc 5:48–55. https://research.tue.nl/en/publications/ageing-and-loneliness-the-role-of-mobility-and-the-built-environm
Wager TD, Davidson ML, Hughes BL, Lindquist MA, Ochsner KN (2008) Prefrontal-subcortical pathways mediating successful emotion regulation. Neuron 59(6):1037–1050. https://doi.org/10.1016/j.neuron.2008.09.006
Wechsler D (1997) Wechsler Adult Intelligence Scale--Third Edition (WAIS-III) [Database record]. https://www.pearsonassessments.com/en-us/Store/Professional-Assessments/Cognition-%26-Neuro/Wechsler-Adult-Intelligence-Scale-%7C-Third-Edition/p/100000243?srsltid=AfmBOopnAPEguAi0uovApXff2uj0P5nYpYnzztGnajvhZLKsj_ZCJ29x
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17(1):37–49. https://doi.org/10.1016/0022-3956(82)90033-4
Yu J, Lam CL, Lee TM (2016) Perceived loneliness among older adults with mild cognitive impairment. Int Psychogeriatr 28(10):1681–1685. https://doi.org/10.1017/s1041610216000430
Zafar J, Malik NI, Atta M, Makhdoom IF, Ullah I, Manzar MD (2021) Loneliness may mediate the relationship between depression and the quality of life among elderly with mild cognitive impairment. Psychogeriatrics 21(5):805–812. https://doi.org/10.1111/psyg.12749
Zhou N, Huang CM, Cai Q, Tzeng OJL, Huang HW (2022) The effects of aging and perceived loneliness on lexical ambiguity resolution. Front Psychol 13:978616. https://doi.org/10.3389/fpsyg.2022.978616
Zhou Y, Chen Z, Shaw I, Wu X, Liao S, Qi L, Huo L, Liu Y, Wang R (2020) Association between social participation and cognitive function among middle-and old-aged Chinese: A fixed-effects analysis. J Glob Health, 10(2). https://doi.org/10.7189/jogh.10.020801
Funding
The National Science and Technology Council (NSTC 113-2321-B-418-003; 112-2410-H-155-030-MY2; 113-2410-H-038-034-) and Yuan Ze University and Far Eastern Memorial Hospital Academic Cooperation Advance Research (Project number: 150008) funded the study in Taiwan.
Author information
Authors and Affiliations
Contributions
CC and Y-TF conceived and conceptualized the study. CC, YFC, YSH, YHC, YTL, and Y-TF contributed to acquisition, analysis, or interpretation of data for the work. CC, VMT, and Y-TF conducted the necessary literature reviews and drafted the first manuscript. VMT, YFC, YSH, YHC, YTL, YC, YLC, RMM, TTL, OJLT advised on review and editing the manuscript.
Corresponding author
Ethics declarations
Competing interests
Authors declare no competing interests.
Ethical approval
This study was approved by the Research Ethics Review Committee of Far Eastern Memorial Hospital on September 13, 2021. The approval number associated with this confirmation is 110192-1. All research activities were performed in accordance with the principles of the Declaration of Helsinki.
Informed consent
Written informed consent was obtained from all participants by trained research personnel at the time of enrollment, which took place between January 2022 and September 2023. The consent process was conducted in person and included a comprehensive verbal explanation of the study’s aims, procedures, potential risks and benefits, and participants’ rights, including the right to withdraw at any time without penalty. Given that the participant pool included older adults diagnosed with mild cognitive impairment, the procedure was carefully adapted to ensure comprehension and voluntariness. Trained staff used simplified, age-appropriate language and verified participants’ understanding through structured comprehension checks prior to obtaining consent. When necessary, caregivers were present to support the decision-making process; however, all participants were deemed capable of providing consent independently. Participants were informed that their data would be anonymized and used exclusively for academic research purposes. The consent covered study participation, use of collected data for analysis, and publication of anonymized results. All participants signed a standardized written consent form voluntarily before any study-related procedures were initiated.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, C., Tahamata, V.M., Chuang, YF. et al. Perceived loneliness mediates the relationship between mild cognitive impairment and executive function deficits. Humanit Soc Sci Commun 12, 991 (2025). https://doi.org/10.1057/s41599-025-05367-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1057/s41599-025-05367-w