Abstract
Anaplastic thyroid carcinoma (ATC) is an aggressive cancer that requirements rapid diagnosis and multimodal treatment. Next-generation sequencing (NGS) aids in personalized therapies and improved trial enrollment. The role of liquid-based NGS in ATC remains unclear. This study analyzed ATC samples using tissue-based NGS, liquid-based NGS, or both platforms. Genetic alterations showed highly heterogeneity, including mutations in RAS/RAF/MEK/ERK, PI3K/AKT/mTOR, cell cycle regulation, other receptor tyrosine kinases, DNA damage response, mismatch repair, and chromatin remodeling. TP53 (65.4%) and BRAF (30.8%) were the most frequently mutated genes in tissue NGS. In paired samples, the concordance rates were 69.2% for TP53 and 84.6% for BRAF. One of two patients treated with dabrafenib and trametinib showed a copy number gain in post-treatment tissue NGS, potentially indicating resistance. Liquid biopsy provides valuable supplementary information when tissue samples are insufficient. Further studies are necessary to understand resistance mechanisms and develop strategies to overcome them in BRAF-targeted therapy.
Similar content being viewed by others
Introduction
Anaplastic thyroid cancer (ATC) accounted for 1.3–9.8% of all thyroid cancers based on various studies worldwide1. It is one of the most lethal malignancies with a median overall survival (OS) of only 4–6 months2,3 and disease-specific mortality of nearly 100%. To enhance survival, previous studies have focused on surgical techniques improvement, radiotherapy design, and the development of novel systemic treatments, including targeted- and immuno-therapies4,5,6,7, however, the treatment outcomes of ATC remain unsatisfactory. Several prognostic factors, including age, leukocytosis, acute symptoms, disease stage, tumor size, prior surgery, prior radiotherapy, and chemotherapy have been identified4,8,9, however, novel treatments are still required to overcome the aggressiveness of ATC.
The BRAF (V600E) mutation is commonly found in thyroid carcinoma, and the prevalence of BRAF mutations in ATC has been reported to be 35–40%10. Dabrafenib and trametinib are tyrosine kinase inhibitors (TKIs) against BRAF V600E and MEK1/2, respectively, and have demonstrated promising effects in BRAF-mutant ATC11,12. In our previous study, we retrospectively analyzed the effect of dabrafenib and trametinib on BRAF-mutated ATC in real-world practice and found that dabrafenib and trametinib were effective and significantly improved the OS of patients with ATC. However, the benefit was limited in BRAF-mutated ATC. Resistance inevitably occurs, and patients succumb to the disease soon after progression. Identifying additional possible targets and mechanisms of resistance to targeted therapy is critical for improving the survival of patients with ATC.
This study aimed to conduct comprehensive genomic profiling to identify common driver mutations in Taiwanese patients with ATC, assess the frequency of established genetic events in tumorigenesis, identify potential novel driver genetic events, and characterize candidates for targeted therapy. Furthermore, we aimed to investigate the role of liquid next-generation sequencing (NGS) and elucidate the resistance mechanisms associated with BRAF-targeted therapy.
Results
The baseline characteristics of 26 patients with ATC enrolled in the current study
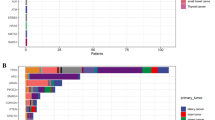
The overall cohort in the current study comprised 26 samples subjected to tissue NGS and 15 samples subjected to liquid NGS (Fig. 1a). Among the 26 patients who underwent tissue NGS, the median follow-up time was 5.4 months (range 0.3 to 35.7 months) until January 2024. The median age of the patients was 72.7 years, and their sex distribution was equal. Most patients exhibited a good or intermediate performance status (Eastern Cooperative Oncology Group Performance Status 0–1:61.5%), had no previous history of differentiated thyroid cancer (de novo ATC: 69.2%), and were diagnosed with distant metastases at the time of the initial ATC diagnosis (stage IVC: 57.7%). The detailed baseline characteristics are summarized in Table 1. Median OS was 6.3 months (95% CI: 1.8–10.8 months, Fig. 1b).
Tissue NGS
The genetic alterations of SNV in ATC were highly heterogeneous, involving several pathways, including RAS/RAF/MEK/ERK (73.1%), PI3K/AKT/mTOR (57.7%), cell cycle regulation (92.3%), other receptor tyrosine kinases (65.4%), DNA damage response (50.0%), and DNA mismatch repair (MMR, 34.6% including MLH1, MSH6, MSH2, and PMS1), and chromatin remodeling (76.9%) (Fig. 2 and Supplementary Fig. 1-2). While no mutations in PMS2 were detected in our cohort, it is important to clarify that PMS2 was carefully evaluated. Alongside the more widely recognized MMR genes (MLH1, MSH6, MSH2, and PMS2), PMS1 is also acknowledged as a DNA MMR gene according to OncoKB. Although 34.6% of patients with ATC harbor MMR mutations, all mutations were variants of uncertain significance (VUS), leading to the absence of MSI-H in the current cohort. Among 24 ATCs with evaluable TMB, only one ATC (TMB: 7.5 mut/Mb) had TMB-H (≥7.5 mut/Mb).
TP53 mutations were the most prevalent (65.4%) in this cohort. BRAF, NF1, NRAS, KRAS, and HRAS mutations accounted for 30.8%, 19.2%, 19.2%, 11.5%, and 3.8% of cases, respectively. All BRAF mutations were the V600E mutation. The KRAS mutations comprised one G12V, one Q61H, and one Q61K. The NRAS mutations included four Q61R mutations and one G13R mutation. Only one HRAS mutation (Q61R) was identified. Mutations in other receptor tyrosine kinases, including FGFR3 (19.2%) and ALK (15.4%), were the most frequent. Mutations in HER, FGFR, NTRK, KIT, PDGFR, MET, and ROS-1 were also found (Supplementary Fig. 2).
Regarding the PI3K/AKT/mTOR pathway, 57.5% of patients with ATC harbored genetic alterations. PTEN loss (19.2%) was the most common, followed by MTOR (11.5%) and PI3KCA (11.5%) mutations. In terms of the DNA damage response, BRCA2 and BRCA1 accounted for 15.4% and 11.5%, respectively. Due to the lack of paired normal tissue for further analysis, germline BRCA1/2 was suspected in some cases based on the variant allele frequency. Additionally, only a single mutation in BRCA1/2 was detected in each patient, which likely excludes the occurrence of second hits. Other genes involved in the DNA damage response were also identified.
CNV was also evaluated. Genes involved in receptor tyrosine kinase (42.3%), cell cycle (42.3%), and DNA damage response (38.5%) were the major pathways in ATC. The CNV details of specific genes are shown in Fig. 3 and Supplementary Fig. 3.
Liquid NGS
Overall, 15 patients underwent liquid NGS, including 13 with paired tissue NGS and two with insufficient tissue for NGS. TP53 and BRAF mutations were detected in four out of 15 (26.7%) patients (Fig. 4), which was lower than that detected by tissue NGS. In cases with limited tissue availability or where tissue NGS is not feasible, liquid biopsy, which detects a BRAF mutation, serves as a complementary method for genetic profiling. However, eight out of 15 patients had no detectable genetic alterations and required paired samples to assess the concordance between tissue and liquid NGS.
Paired tissue and liquid NGS
Among the 13 paired tissue and liquid NGS samples, no genetic alterations were found in seven liquid NGS reports, suggesting that liquid NGS has an intrinsic limitation in identifying genetic alterations in ATC (Fig. 5). Generally, liquid NGS did not reveal additional genetic alterations compared with tissue NGS, except for two samples that reported ATM and EGFR mutations that were not detected by tissue NGS (Fig. 5).
In five of the 13 ATC patients with BRAF mutations by tissue NGS, 3 (60%) were detected by liquid NGS, resulting in a sensitivity of 60% and specificity of 100% for BRAF detection by liquid NGS. The concordance rate for BRAF mutations was 84.6% and for TP53 was 69.2%.
Resistance
Two patients with ATC were treated with dabrafenib and trametinib, and on progression on targeted therapy (Fig. 6), they underwent a series of NGS analyses. The first patient experienced progression twice, which led to two additional tissue NGS analyses. No differences were found in terms of SNV, but a gain in copy number (copy number: 4–6) was observed for some genes (GNAS, AURKA, SRC, TOP1, etc.) in one patient.
Discussion
The poor prognosis associated with ATC is primarily attributed to the limited efficacy of conventional treatment modalities and an incomplete understanding of the underlying mechanisms driving ATC tumorigenesis. This study aimed to address these challenges by conducting comprehensive genomic profiling of 26 ATC cases in Taiwan and assessing the concordance between tissue and liquid NGS in 13 ATC cases. The genomic landscape of ATC revealed the intricate involvement of multiple pathways, including RAS/RAF/MEK/ERK (73.1%), PI3K/AKT/mTOR (57.7%), cell cycle regulation (92.3%), other receptor tyrosine kinases (65.4%), DNA damage response (50.0%), DNA mismatch repair (34.6%), and chromatin remodeling (76.9%). Liquid NGS demonstrated the capability to detect more BRAF mutations in cases where tissue was either unavailable or insufficient13. These findings underscore the highly heterogeneous genetic background of ATC, revealing previously unexplored genetic events. Notably, mutations in HER1/2/3, FGFR2/4, NTRK 1/2/3, and genes associated with the DNA damage response have been identified, presenting intriguing possibilities, as pharmaceuticals targeting these genes are currently in clinical or experimental use. Finally, the mutation landscape of the cohort was characterized, revealing diverse frequencies of recognized thyroid malignancy genes in the majority, though not all, of ATC cases.
The detection of driver mutations is a key factor in ATC treatment, as most patients cannot be cured by surgery alone. The commonly mutated genes were TP53 in 17/26 (65.4%) patients, and BRAF in 8/26 (30.8%) patients, which is consistent with previous reports14,15,16,17. Regarding the impact of BRAF and TP53 mutations on survival, no significant difference was observed between mutated and wild-type ATC (p = 0.729 for BRAF, p = 0.426 for TP53, Supplementary Fig. 4). In addition to tumor agnostic therapy, combination therapy with dabrafenib and trametinib is the only targeted therapy that has been approved for ATC harboring the BRAF V600E mutation since 2018, based on the ROAR study (BRF117019 study, NCT02034110)11,12. A few retrospective studies also confirmed the role of targeted therapy for BRAF-mutated ATC18,19. Tumor agnostic treatment was applied for ATC with NTRK fusion, RET fusion, and MSI-H, which were not found in the current cohort. However, other possible novel targets have been identified, providing evidence for the development of targeted therapies.
Regarding KRAS mutations, we identified one G12V, one Q61H, and one Q61K mutation. Sotorasib and adagrasib have been approved for patients with non-small cell lung cancer (NSCLC) harboring the KRAS G12C20. In 14 patients (10 with pancreatic ductal adenocarcinoma (PDAC) and four with NSCLC) harboring G12X mutations other than G12C and treated with RMC-6236 at least 8 weeks before the data cut-off date, the objective response rate was 36%21. Ongoing investigations into targeted therapies offer hope for the treatment of cancers with various KRAS mutations20.
Four patients with NRAS mutations were identified, including four with Q61R and one with G13R mutations. Currently, there is no approved treatment for cancers with NRAS mutations. However, MEK inhibitors such as cobimetinib, trametinib, and binimetinib may stabilize NRAS-mutated metastatic melanoma, with an objective response rate (ORR) of 18.2% and a disease control rate (DCR) of 48.5%22. Recently, the ORR reported was 46.7% in patients with NRAS-mutated melanoma treated with naporafenib (a pan-RAF kinase inhibitor, 200 mg twice a day) plus trametinib (1 mg once daily)23. SEACRAFT-1 is an open-label study designed to assess the safety and efficacy of naporafenib administered with trametinib in previously treated patients with locally advanced unresectable or metastatic RAS Q61X solid tumor malignancies including thyroid cancer (ClinicalTrials.gov Identifier: NCT05907304).
Other genetic alterations involving the DNA damage response (DDR) and cell cycle may have implications in specific targeted therapies. Currently, homologous recombination deficiency (HRD) is the only available predictive biomarker that can identify patients more likely to benefit from PARP inhibitors24. PARP inhibitor monotherapy has been extensively investigated in cancer subtypes commonly associated with HRD25. Furthermore, clinical trials of combination strategies with anti-angiogenesis and immunotherapy have aimed to enhance the efficacy of PARP inhibitors25. Studies targeting cell cycle checkpoints26, such as ATM27, ATR, and Wee128, are ongoing to tackle the DDR.
In our study, the rate of BRAFV600E detection by circulating tumor DNA (ctDNA) was 26.7%. This is comparable to the findings in 92 cases of ATC using the Guardant360 plasma NGS test, which showed a BRAFV600E detection rate of 27.2%29. However, this was lower than that reported in historical cohorts14,15,16,17 and in our tissue NGS (30.8%). However, the previous reports did not assess concordance between paired tissue and liquid NGS. Based on our findings, liquid NGS could be an alternative option for patients whose tissue is unavailable or insufficient, or when urgent treatment is required. However, it is important to note that liquid NGS cannot fully replace tissue NGS, as 7 out of 13 cases in our cohort showed no results from liquid NGS.
In the current cohort of 13 NGS pairs, the concordance rates were 84.6% for BRAF and 69.2% for TP53. This discrepancy in detection rates could potentially be attributed to the specific characteristics of ATC, including tumor burden and shedding. Supporting this, another study involving 23 patients with ATC at the University of Texas MD Anderson Cancer Center revealed that the reliability of inference based on concordance was highest in patients who underwent dual-platform sequencing before initiating definitive treatment17. In contrast, it was the lowest in patients who underwent cell-free circulating DNA (cfDNA) analysis after treatment17. Therefore, tissue NGS should remain the standard of care for determining therapeutic options for ATC unless the tissue is unavailable or insufficient for tissue NGS.
The identification of more novel targets and resistance mechanisms is required. However, no novel targets were identified in this study. We found some genes with increased copy numbers (copy number: 4–6) implying a possible resistance mechanism for BRAF-targeted therapy. However, more cases should be compiled and analyzed to confirm these data. Unlike the intrinsic and extrinsic acquired mutations in melanoma30 and NSCLC31, currently, there are not many reports on ATC. Recently, BRAF off-target resistance mechanisms in ATCs, including RAS mutations32,33 RAC1 mutations34, and copy number variations34 have been described. Further studies are warranted to understand the mechanisms of resistance to BRAF-targeted therapy in ATC.
The small number of cases remains the primary limitation of this study, reflecting the rarity of this cancer. However, the study is warranted given the aggressive nature of the disease. Due to the limited sample size, we have listed all detected mutations to provide comprehensive data, including putative drivers and VUS (Supplementary Table 1). For specific details on the oncogenicity of each mutation, we have also provided the detailed data as supplementary material (Supplementary Table 1), annotated using OncoKB results to categorize mutations as either putative drivers or VUS. Regarding co-occurrence or mutually exclusive relationships of specific genes, BRAF and TP53 mutations are not mutually exclusive. A mutual exclusivity analysis was performed using cBioPortal, and due to the small sample size, no significant co-occurrence or mutually exclusive relationships were observed between BRAF, TP53, and other genes (p < 0.05, q-value < 0.05). Detailed information on significant co-occurrence or mutually exclusive genes is provided in Supplementary Table 2.
This study provides clinical insights into the genomic landscape of ATC and identifies potential novel targets worthy of further investigation. Considering the multiple aberrant pathways present in these tumors, a multi-targeted therapeutic strategy is essential. While liquid biopsy alone may not be sufficient to identify driver mutations, it offers complementary information when the tissue is inadequate for NGS. Further studies are warranted to understand the resistance mechanisms of BRAF-targeted therapy and to find ways to overcome this resistance.
Methods
Patients and clinical characteristics
This study included data from patients with histologically confirmed ATC at Chang Gung Memorial Hospital (CGMH), Linkou, between 2011 and 2023 and encompassed both prospective (after 2021/03/08) and retrospective (2000/01 ~ 2021/02) cohorts delineated by the date from Institutional Review Board of Chang Gung Medical Foundation approval (IRB#202100148B0). The requirement for informed consent was waived for the retrospective cohort and was obtained from the prospective cohort. All patients (or their legal proxies/guardians) provided informed consent for study participation and the publication of anonymized case details. The analysis focused on patients with adequate quality and quantity of archived tissues available for NGS assays. Additionally, liquid biopsy samples for NGS were collected from prospective cohorts of treatment-naïve ATC patients. The main cohort, comprising tissue and liquid NGS samples, was obtained prior to systemic treatment and radiotherapy. For the resistance cohort, samples were collected following BRAF-targeted therapy, as detailed in the results section. The retrospective records encompassed clinical characteristics, including age at diagnosis, sex, staging, metastatic sites, treatment history (including prior surgery and radiotherapy), and OS outcomes.
Sample processing and next-generation sequencing (NGS)
Samples with inadequate quality that failed quality control were excluded from analysis by ACTOnco®+ (ACT Genomics, Taipei, Taiwan), an NGS panel sequencing more than 440 genes. Nucleotide variation (SNV), copy number variation (CNV), microsatellite instability (MSI), and tumor mutational burden (TMB) were evaluated. For details of the NGS methodology, please refer to our earlier study35.
TMB was determined using the sequenced regions of ACTOnco®+ to estimate the number of somatic nonsynonymous mutations per megabase across all protein-coding genes (whole exome). TMB calculation predicted somatic variants and applied a machine-learning model with cancer hotspot correction. TMB results are categorized as “TMB-High” (≥7.5 muts/Mb), “TMB-Low” (<7.5 muts/Mb), or “Cannot Be Determined” (the tumor purity of the sample is <30%). The extracted RNA was reverse transcribed and used for library construction. Sequencing was conducted using an Ion Proton or Ion S5 sequencer. To ensure the sequencing quality, the average unique RNA Start Sites (SS) per control Gene Specific Primer 2 (GSP 2) should be ≥10.
For the fusion analysis, the sequenced reads were aligned to the human reference genome, non-contiguous genome regions were identified, filters were applied to exclude false-positive events, and annotated using the Quiver Gene Fusion Database maintained by ArcherDX. The samples with detected fusions were required to meet the following criteria: (1) Number of unique start sites (SS) for the GSP2 ≥ 3; (2) Number of supporting reads spanning the fusion junction ≥ 5; (3) Percentage of supporting reads spanning the fusion junction ≥10%; (4) Fusions annotated in Quiver Gene Fusion Database.
ACTMonitor®+ Genomic DNA was extracted from patients’ plasma, followed by library construction and sequencing for the hotspot regions of 50 genes. Sequencing was performed using an Ion Torrent sequencing system (Thermo Fisher Scientific). Variants that met the following criteria were retained: variants with an allele frequency of ≥0.5%, and hotspot variants with an allele frequency of ≥0.2%. This test provided a uniform coverage of the targeted regions, enabling target base coverage at 2000x of ≥70% with a mean coverage of ≥7000x. The datasets are accessible through the Gene Expression Omnibus under the data series GSE281660.
Statistical analysis
Continuous variables were expressed as median ± SD, while categorical variables were presented as numbers (%). OS was defined as the duration from the date of diagnosis to the date of death or the last follow-up and is presented as the median (95% confidence interval [CI]). Concordance between the two platforms was calculated using the following formula: concordance = number of concordant results/overall population.
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The datasets of tissue and liquid NGS are available at Gene Expression Omnibus, data series GSE281660.
References
Smallridge, R. C. & Copland, J. A. Anaplastic thyroid carcinoma: pathogenesis and emerging therapies. Clin. Oncol. 22, 486–497 (2010).
Lee, D. Y. et al. Recurrence and survival after gross total removal of resectable undifferentiated or poorly differentiated thyroid carcinoma. Thyroid 26, 1259–1268 (2016).
Zhang, L. et al. Novel recurrent altered genes in chinese patients with anaplastic thyroid cancer. J. Clin. Endocrinol. Metab. 106, 988–998 (2021).
Are, C. & Shaha, A. R. Anaplastic thyroid carcinoma: biology, pathogenesis, prognostic factors, and treatment approaches. Ann. Surg. Oncol. 13, 453–464 (2006).
McIver, B. et al. Anaplastic thyroid carcinoma: a 50-year experience at a single institution. Surgery 130, 1028–1034 (2001).
Smallridge, R. C. et al. American thyroid association guidelines for management of patients with anaplastic thyroid cancer. Thyroid 22, 1104–1139 (2012).
Dierks, C. et al. Combination of lenvatinib and pembrolizumab is an effective treatment option for anaplastic and poorly differentiated thyroid carcinoma. Thyroid 31, 1076–1085 (2021).
O’Neill, J. P. & Shaha, A. R. Anaplastic thyroid cancer. Oral Oncol. 49, 702–706 (2013).
Sugitani, I. et al. Prognostic factors and treatment outcomes for anaplastic thyroid carcinoma: ATC Research Consortium of Japan cohort study of 677 patients. World J. Surg. 36, 1247–1254 (2012).
Cabanillas, M. E., Ryder, M. & Jimenez, C. Targeted therapy for advanced thyroid cancer: kinase inhibitors and beyond. Endocr. Rev. 40, 1573–1604 (2019).
Subbiah, V. et al. Dabrafenib and Trametinib treatment in patients with locally advanced or metastatic BRAF V600-mutant anaplastic thyroid cancer. J. Clin. Oncol. 36, 7–13 (2018).
Subbiah, V. et al. Dabrafenib plus trametinib in patients with BRAF V600E-mutant anaplastic thyroid cancer: updated analysis from the phase II ROAR basket study. Ann. Oncol. 33, 406–415 (2022).
Yang, C. Y. et al. Upfront liquid next-generation sequencing in treatment-naive advanced non-small cell lung cancer patients: a prospective randomised study in the Taiwanese health system. Eur. J. Cancer 193, 113310 (2023).
Wu, H. et al. Anaplastic thyroid cancer: outcome and the mutation/expression profiles of potential targets. Pathol Oncol. Res. 21, 695–701 (2015).
Kunstman, J. W. et al. Characterization of the mutational landscape of anaplastic thyroid cancer via whole-exome sequencing. Hum. Mol. Genet. 24, 2318–2329 (2015).
Kasaian, K. et al. The genomic and transcriptomic landscape of anaplastic thyroid cancer: implications for therapy. Bmc Cancer 15, 984 (2015).
Sandulache, V. C. et al. Real-time genomic characterization utilizing circulating cell-free DNA in patients with anaplastic thyroid carcinoma. Thyroid 27, 81–87 (2017).
Chang, C. F. et al. The impact of BRAF targeting agents in advanced anaplastic thyroid cancer: a multi-institutional retrospective study in Taiwan. Am. J. Cancer Res. 12, 5342–5350 (2022).
da Silva, T. N. et al. Target therapy for BRAF mutated anaplastic thyroid cancer: a clinical and molecular study. Eur. J. Endocrinol. 188, https://doi.org/10.1093/ejendo/lvac011 (2023).
Santarpia, M. et al. Targeted therapies for KRAS-mutant non-small cell lung cancer: from preclinical studies to clinical development-a narrative review. Transl. Lung Cancer Res. 12, 346–368 (2023).
Arbour, K. et al. 652O Preliminary clinical activity of RMC-6236, a first-in-class, RAS-selective, tri-complex RAS-MULTI (ON) inhibitor in patients with KRAS mutant pancreatic ductal adenocarcinoma (PDAC) and non-small cell lung cancer (NSCLC). Ann. Oncol. 34, S458 (2023).
Salzmann, M. et al. MEK inhibitors for pre-treated, NRAS-mutated metastatic melanoma: a multi-centre, retrospective study. Eur. J. Cancer 166, 24–32 (2022).
de Braud, F. et al. Initial evidence for the efficacy of naporafenib in combination with trametinib in nras-mutant melanoma: results from the expansion arm of a phase ib, open-label study. J. Clin. Oncol. 41, 2651–2660 (2023).
Konstantinopoulos, P. A., Ceccaldi, R., Shapiro, G. I., & D’Andrea, A. D. Homologous recombination deficiency: exploiting the fundamental vulnerability of ovarian cancer. Cancer Discov. 5, 1137–1154 (2015).
Genta, S., Martorana, F., Stathis, A. & Colombo, I. Targeting the DNA damage response: PARP inhibitors and new perspectives in the landscape of cancer treatment. Crit. Rev. Oncol. Hematol. 168, 103539 (2021).
Wu, C. E., Pan, Y. R., Yeh, C. N. & Lunec, J. Targeting P53 as a future strategy to overcome gemcitabine resistance in biliary tract cancers. Biomolecules 10, https://doi.org/10.3390/biom10111474 (2020).
Pan, Y. R., Wu, C. E. & Yeh, C. N. ATM inhibitor suppresses gemcitabine-resistant BTC growth in a polymerase theta deficiency-dependent manner. Biomolecules 10, https://doi.org/10.3390/biom10111529 (2020).
Chen, C. P. et al. Wee1 inhibition by MK1775 potentiates gemcitabine through accumulated replication stress leading to apoptosis in biliary tract cancer. Biomed. Pharmacother. 166, 115389 (2023).
Tarasova, V. D. et al. Characterization of the thyroid cancer genomic landscape by plasma-based circulating tumor DNA next-generation sequencing. Thyroid, https://doi.org/10.1089/thy.2023.0204 (2023).
Tangella, L. P., Clark, M. E. & Gray, E. S. Resistance mechanisms to targeted therapy in BRAF-mutant melanoma - A mini review. Biochim. Biophys. Acta Gen. Subj. 1865, 129736 (2021).
Facchinetti, F. et al. Molecular mechanisms of resistance to BRAF and MEK inhibitors in BRAF(V600E) non-small cell lung cancer. Eur. J. Cancer 132, 211–223 (2020).
Porter, A. & Wong, D. J. Perspectives on the treatment of advanced thyroid cancer: Approved therapies, resistance mechanisms, and future directions. Front. Oncol. 10, 592202 (2020).
Cabanillas, M. E. et al. Acquired secondary ras mutation in BRAF(V600E)-mutated thyroid cancer patients treated with BRAF inhibitors. Thyroid 30, 1288–1296 (2020).
Bagheri-Yarmand, R. et al. RAC1 alterations induce acquired dabrafenib resistance in association with anaplastic transformation in a papillary thyroid cancer patient. Cancers 13, https://doi.org/10.3390/cancers13194950 (2021).
Chang, J. W. et al. Genomic and tumour microenvironmental biomarkers of immune checkpoint inhibitor response in advanced Taiwanese melanoma. Clin. Transl. Immunol. 12, e1465 (2023).
Acknowledgements
We thank the Research Specimen Processing Laboratory and Common Laboratory of Chang Gung Memorial Hospital, Linkou, for technical and funding support. This work was financially supported by grants from Linkou Chang-Gung Memorial Hospital (CMRPG3L0911 ~ 3, CMRPG3M0521 ~ 2, CMRPG3M0971 ~ 2, CMRPG3P0181, and CMRPG3P0101 to CEW) and the National Science and Technology Council (109-2314-B-182-080-MY3, 111-2811-B-182-017, 113-2628-B-182-001-MY3, and 113-2811-B-182-024 to CEW).
Author information
Authors and Affiliations
Contributions
C.N.Y. contributed to conceptualization, investigation, visualization, draft-review and editing; S.F.L. was involved in conceptualization, investigation, and visualization; C.L.W. contributed to methodology and investigation; M.J.L. and I.W.C. carried out methodology and formal analysis; C.P.C. was involved in visualization and investigation; C.F.C. contributed to methodology and formal analysis; Q.A.W. carried out methodology and investigation; C.E.W. was in charge of conceptualization, methodology, supervision, writing original draft, and draft-review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yeh, CN., Lin, SF., Wu, CL. et al. Genomic landscape and comparative analysis of tissue and liquid-based NGS in Taiwanese anaplastic thyroid carcinoma. npj Precis. Onc. 9, 16 (2025). https://doi.org/10.1038/s41698-025-00802-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41698-025-00802-2