Abstract
We developed and evaluated the Digital Platform for Exercise (DPEx): a decentralized, patient-centric approach designed to enhance all aspects of clinical investigation of exercise therapy. DPEx integrated provision of a treadmill with telemedicine and remote biospecimen collection permitting all study procedures to be conducted in patient’s homes. Linked health biodevices enabled high-resolution monitoring of lifestyle and physiological response. Here we describe the rationale and development of DPEx as well as feasibility evaluation in three different cohorts of patients with cancer: a phase 0a development study among three women with post-treatment primary breast cancer; a phase 0b proof-of-concept trial of neoadjuvant exercise therapy in 13 patients with untreated solid tumors; and a phase 1a level-finding trial of neoadjuvant exercise therapy in 53 men with localized prostate cancer. Collectively, our study demonstrates the utility of a fully digital, decentralized approach to conduct clinical trials of exercise therapy in a clinical population.
Similar content being viewed by others
Introduction
Rigorous conduct of clinical trials investigating the efficacy and safety of therapeutic and non-therapeutic strategies have multiple barriers1,2. Arduous pre-study (eligibility confirmation) and on-study visits create significant challenges for patients lacking the necessary time and means to participate3. These are particularly pronounced in clinical trials of exercise therapy—endurance and/or resistance training prescribed according to a planned dose and schedule4.
To ensure evaluation of exercise therapy at high-fidelity—precisely dosed exercise at high adherence—investigators have relied on site-based approaches, with in-person monitoring to verify dose and safety5. A typical exercise therapy clinical trial entails multiple independent treatment sessions administered several times weekly, each requiring an on-site visit6,7,8. Other study-related procedures including informed consent, end point assessments, and biospecimen collection require additional in-person visits. Hence, patient burden is considerable due to inconvenience and high cost. Accrual is limited to only those residing within reasonable geographical proximity of the research center, leading to disparities in access and limiting participant diversity1; scarcity and premium expense of space at most medical centers as well as site scheduling constraints also limits enrollment. Consequently, many clinical trials of exercise therapy fail to achieve planned accrual goals, or experience suboptimal adherence in recruited patients5,9,10. Barriers to participation were exacerbated by restrictions related to the COVID-19 pandemic11,12.
To ameliorate these challenges, we developed and evaluated the Digital Platform for Exercise (DPEx), a decentralized, patient-centric solution designed to enhance all aspects of study conduct of exercise therapy clinical trials (Fig. 1). Here we describe the rationale and development of DPEx; we also report “proof-of-concept” evaluation of DPEx for clinical investigation of exercise therapy in three independent cohorts of patients with cancer.
Results
Rationale and development
Memorial Sloan Kettering Cancer Center (MSK) is a tertiary cancer center with a main campus on the Upper East Side of Manhattan in New York City with a large majority of patients residing in the surrounding New York, New Jersey, and Connecticut State areas. Hence, conduct of exercise therapy clinical trials adopting a conventional site-based model faced major barriers to patient recruitment that impeded rigorous trial design and performance, even before the COVID-19 pandemic13. DPEx was developed to directly address these barriers. The overarching objectives were to: (1) enhance patient identification, enrollment, and retention, (2) alleviate patient burden and increase patient access and diversity, (3) enhance exercise therapy administration and quantification, and (4) longitudinal, high-resolution phenotyping of lifestyle and patient physiology. Initial DPEx development was conducted from July 2018 to February 2019. This involved four main components: (1) telemedicine-based (remote) delivery of exercise therapy; (2) telemedicine-based (remote) conduct of cardiorespiratory fitness testing; (3) lifestyle patterns and physiological monitoring; and (4) eConsent. All technology solutions were reviewed and approved by MSK Information Security prior to use.
Telemedicine-based exercise therapy (ET)
Our first objective was to administer exercise therapy with the same individual patient precision, quantification, and real-time monitoring as in facility-based setting but in the convenience of patient’s homes—i.e., high-fidelity treatment delivery. Administration of exercise therapy at high-fidelity is paramount in efficacy-based trials wherein to adequately evaluate effect on study end points14. We first sought to identify an exercise equipment vendor with: (1) dedicated personnel to support clinical trial conduct, (2) availability of service technicians in New York and surrounding States, and (3) storage facilities and established distribution network with geographical proximity to permit timely treadmill delivery and extraction. A standard business service agreement was executed with Technogym, Inc. After testing multiple models, the Technogym Jog Forma model was selected based on the long treadmill deck and solid stability, considered necessary for the target clinical population of inactive, potentially aged patients. Additionally, Jog Forma treadmills include a support system permitting secure positioning of an electronic tablet to the console, enabling stable video conferencing during exercise therapy sessions. Professional enterprise licenses were procured for all study personnel permitting group-based remote exercise therapy sessions: use of the video conferencing platform multi-screen function to monitor up to three patients exercising at three unique locations simultaneously, in real-time. An initial fleet of 40 treadmills was distributed to three separate Technogym, Inc. storage facilities providing a geographical recruitment radius of 100 miles from MSK main campus.
Telemedicine-based cardiorespiratory fitness testing (CFT)
We next determined the feasibility and logistics of a CFT in the patient’s residence with real-time remote supervision and monitoring by study personnel. To optimize safety, we conducted pre-exercise participation cardiovascular screening using a multigated screening approach (i.e., medical chart review, physician approval, clearance via exercise screening survey) to identify any absolute (e.g., heart failure, acute myocardial infarction, ventricular tachycardia, acute infection) or relative (e.g., uncontrolled hypertension, ventricular aneurysm, hypertrophic cardiomyopathy) contraindications to a remotely-monitored CFT or moderate-intensity exercise as per American Thoracic Society guidelines15, and screening clearance via the Physical Activity Readiness-Questionnaire plus (PAR-Q + )16. The CFT serves three important purposes: (1) eligibility criteria: providing pre-exercise cardiovascular screening17, (2) study end point: objective measure that exercise therapy regimen was administered at high-fidelity (i.e., manipulation check), and (3) individualization of exercise therapy prescription18. We evaluated whether a standardized Balke-Ware incremental exercise “ramp” protocol19 could be remotely administered with sufficient flexibility (in terms of incremental walking speed and incline) to permit the patient population to achieve a pre-determined objective of 80% of age-predicted heart rate maximum within an 8–15-min timeframe. Safety procedures for a serious adverse event (SAE) during remotely delivered CFT and exercise therapy were established.
Lifestyle patterns and physiological monitoring
Monitoring of sleep and general physical activity as well as sedentary time are important lifestyle covariates that may confound exercise therapy fidelity whereas profiling of physiological outcomes enables dynamic mapping of response. We selected several Bluetooth-enabled health devices: activity and heart rate monitor (Withings Steel HR), blood pressure monitor (Withings BPM Connect), and a body composition scale (Withings Body + ). All devices were connected to a cloud-based, Health Insurance Portability and Accountability Act (HIPAA)-compliant technology platform (Validic Inc.). Splunk (v7.2.7) was utilized for data storage and custom dashboard for monitoring of connected device data; this also served as a notification system when a scheduled device measurement was missed.
eConsent
MSK’s proprietary electronic Consent module (MSK eConsent System, v.2) is an in-house stand-alone web-based application. We combined this module with the video conferencing platform to enable remote informed consent.
Phase 0a. Development cohort
Following verification of all operations and components, we next explored the feasibility of DPEx in a clinical trial setting. We recruited a convenience sample of three inactive, non-obese, post-treatment breast cancer patients. Patient characteristics are presented in Supplementary Table 1. All three patients previously participated in an exercise therapy trial conducted by the PI, with all being cleared to participate in moderate-intensity exercise20. The MSK Institutional Review Board (IRB) approved the study and all patients provided written informed consent prior to the initiation of any study procedures.
All patients had an existing rapport with the study team and were willing to troubleshoot emergent platform feasibility or logistical issues as well as provide critical feedback. Eligible and interested patients were sent a secure URL via the MyMSK patient portal connecting patients to a two-way, encrypted, video conferencing platform enabling simultaneous, real-time review of informed consent. Graphics were used to facilitate study details and procedures within the MSK eConsent module. All consenting patients were shipped the study kit (i.e., etablet, health devices, treadmill). Study staff then performed a two-way video orientation session using the study electronic tablet to overview use of all devices and conduct the pre-treatment CFT. Following baseline assessments, study staff scheduled the first exercise therapy session.
Exercise therapy comprised individualized, supervised treadmill walking (Jog Forma, Technogym, Inc.) five times weekly for four to six consecutive weeks (i.e., 20 to 30 independent sessions). All sessions were conducted at \(\approx\)70% of the individual patient’s exercise capacity, based on workload (the speed and incline) measured during the baseline CFT for \(\approx\)30 minutes per session (planned amount: 150 minutes/week)21. The primary end points were DPEx feasibility evaluated by: (1) digital device reliability (e.g., connection success rate) and logistics (e.g., time needed for study overview and consent, study-kit delivery, and orientation), (2) safety of CFT and exercise therapy sessions, (3) exercise therapy adherence, and adherence to health device use.
The development study was conducted between February 2019 and May 2019. Patients resided 1.2 miles to 9.4 miles from MSK main campus. Mean time for setup (e.g., study consent, study kit delivery, and orientation) from patient consent to conduct of the CFT was 3 days (range: 2 to 4 days). Two-way video conferencing connectivity success rate for ET was 100%: 79/79 exercise sessions had successful initial connection that persisted for the entirety of planned session duration. All CFTs were deemed acceptable, and no patients were lost-to-follow-up. Mean exercise therapy adherence was 94% (79 sessions attended of 84 planned). No serious adverse events (SAEs) were observed during any exercise therapy sessions. Mean adherence to health devices was 85% (range: 74-100%, 105 days monitored of 123 planned).
Phase 0b. Proof-of-concept trial
We next conducted a phase 0b proof-of-concept “window of opportunity” study of neoadjuvant exercise therapy. Clinical trial registration NCT03813615; Date of registration: January 21, 2019. In this trial, DPEx was enhanced to include optional remote (in-home) blood and stool biospecimen collection, continuous glucose monitoring (CGM), and dietary intake collection. CGM provides a useful dynamic biomarker to evaluate exercise therapy effects on host metabolic profile22. Dietary intake was evaluated for 3 consecutive days at baseline and postintervention in real-time using a dietary mobile application with photo recognition to identify food items, with automated calculation of caloric and nutrient intake (Bitesnap)23. We also introduced remote “group-based” exercise therapy sessions: use of the video conferencing platform multi-screen function to monitor up to three patients exercising at three unique locations simultaneously, with real-time monitoring.
The phase 0b was a prospective, single-arm study in inactive (i.e., < 90 minutes of moderate or vigorous exercise per week24) patients with histologically confirmed treatment-naïve breast, endometrial, or prostate cancer with at least a 2-week window from enrollment to scheduled surgical resection at MSK. The MSK IRB approved the study and all patients provided written informed consent prior to the initiation of any study procedures. Potential eligible patients were identified using two technology screening solutions: DataLine and Cohort Builder. DataLine uses structured queries and natural language processing to search the institution’s database warehouse (integration of all clinical and operational subject areas) to screen on specific eligibility criteria25: cancer diagnosis, visit type, geographical distance from MSK, primary language, and provider. Cohort Builder is an interactive webapp permitting users to integrate customized cohort eligibility criteria and data extraction (e.g., provider, scheduled surgery) logic, which is then displayed via one or more channels (e.g., interactive display, email, visualizations). Generated lists were then cross-referenced against MSK’s scheduling system to confirm surgery type and date. This recruitment process is deemed to present no more than minimal risk to the privacy of the patients who are screened, and minimal protected health information (PHI) was maintained as part of a screening log. To perform these procedures, a (partial) limited waiver of authorization was obtained from MSK IRB. The primary oncology team provider was then contacted by email to confirm eligibility and obtain permission for patient contact. Eligible and interested patients were sent a secure URL via the MyMSK patient portal connecting patients to a two-way, encrypted, video conferencing platform enabling simultaneous, real-time review of electronic informed consent. All consenting patients were shipped the study kit (i.e., electronic tablet, health devices, treadmill). Study staff then performed a two-way video orientation session using the electronic tablet to overview use of all devices, conduct the pretreatment CFT, and, if appropriate, schedule the first exercise therapy session. The (a) study schema and schedule of activities, and (b) type and sampling frequency of each assessment is presented in Fig. 2. Exercise therapy was delivered in an identical manner as in phase 0a with the exception exercise therapy was performed five times weekly for 3 to 12 consecutive weeks (i.e., 14 to 59 independent sessions), depending on the pre-operative window. Study end points were DPEx feasibility, digital device reliability, as well as rates of accrual, drop out, CFT safety, exercise therapy adherence, and adherence with health device use. The total time commitment and cost for DPEx versus a hypothetical site-based model (i.e., patient-matched virtual twin) was also estimated.
The study was conducted from June 2019 to February 2020. Digital patient screening averaged 10 minutes (\(\pm\) 5 minutes) per patient and time for the healthcare team to contact identified patients (to determine study interest) averaged 3 days (range: 1 to 5 days). The study overview averaged 20 minutes (\(\pm\) 5 minutes) while mean duration for electronic informed consent was 60 minutes (range: 45 to 90 minutes per patient). The major reason for non-accrual was lack of interest. A total 43 patients were deemed eligible and 13 (30%) agreed to participate (Supplementary Table 1). Patients resided a mean 38 miles (range: 1 to 70 miles) from the hospital main campus (Fig. 3a). Mean set up time from consent to CFT was 3 days (range: 2 to 6 days). All CFTs were deemed acceptable. Two-way video conferencing connectivity success rate across a total of 293 unique exercise therapy sessions was 100%. No patients were lost-to-follow-up. Mean length of exercise therapy was 5.5 weeks (range: 3 to 12 weeks) or mean of 23 (range: 14 to 48) completed unique sessions per patient. Mean adherence to exercise therapy was 87% (293 sessions attended of 336 planned; Fig. 3b). No SAEs were observed. Adherence to health devices is presented in Fig. 3b. Twelve patients (92%) consented to dietary intake monitoring, with a mean adherence of 75% (54 days monitored of 72 days planned). Ten patients (78%) consented to CGM, with a mean adherence of 86% (313 days monitored of 363 days planned). Twelve (92%) and ten (77%) patients consented to remote blood and stool collection, respectively, with acquisition and delivery achieved in 94% (66 completed of 70 planned) and 90% (52 completed of 58 planned), respectively. Mean time commitment to conduct all study procedures using the DPEx was 34 hours per patient (range: 21 to 70 hours) compared with an estimated mean of 81 hours (range: 59 to 159 hours) for a patient-matched virtual twin site-based model (Fig. 3c). Patient’s mean cost for study participation using the DPEx was $0 compared with an estimated mean cost of $837 (range: $231 to $1,629) for a patient-matched virtual twin site-based model (Fig. 3d). Investigator cost was $3,308 per patient (range: $2,425 to $4,126).
a geographical location of patients, b exercise therapy adherence and adherence with health device usage, c patient estimated time commitment versus matched site-based virtual twin, and d patient estimated cost versus matched site-based virtual twin. Box length and line indicates the median value. Each grey dot represents a single patient.
Phase 1a. exercise level-finding trial
We next conducted a phase 1 level-finding trial of neoadjuvant exercise therapy in men with localized prostate cancer. Clinical trial registration NCT03813615; Date of registration: January 21, 2019. The primary feasibility and efficacy results of this trial have been previously published26. We leveraged this trial to further examine feasibility of the DPEx to administer higher levels of exercise therapy and in a larger patient cohort. Inactive (i.e., < 90 minutes of moderate or vigorous exercise per week24) patients with histologically confirmed treatment-naïve prostate cancer with at least a 2-week window from enrollment to scheduled surgical resection at MSK were eligible. The MSK IRB approved the study and all patients provided written informed consent prior to the initiation of any study procedures. Patients were allocated to six escalated exercise therapy dose levels (i.e., 90, 150, 225, 300, 375, and 450 minutes per week) across 3 to 7 individual sessions per week (over a 7-day period) for 2 to 12 consecutive weeks (i.e., 6 to 59 planned independent sessions) depending on the pre-operative window. All study procedures were conducted and evaluated in an identical manner as described in the phase 0b.
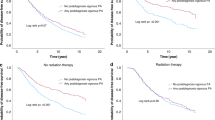
The study was conducted from July 2019 to February 2023. A total 131 patients were deemed eligible and 53 (40%) agreed to participate (Supplementary Table 2). Patients resided a mean 39 miles (range: 1 to 90 miles) from the hospital main campus (Fig. 4a). Mean set up time for DPEx from consent to the CFT was 5 days (range: 1 to 18 days). All CFTs were deemed acceptable. Two-way video conferencing connectivity success rate across a total of 951 unique exercise therapy sessions was 100%. Two patients (of 53 = 4%) dropped out due to not proceeding to surgical resection. Mean length of exercise therapy was 4 weeks (range: 2 to 12 weeks) or mean of 18 (range: 3 to 48) completed unique exercise therapy sessions per patient. Mean exercise therapy adherence across all dose levels was 88% (951 sessions attended of 1082 planned: Fig. 4b). No SAEs were observed.
a geographical location of patients by exercise therapy dose level. Each dot represents a single patient. MSK logo depicts location of Memorial Sloan Kettering Cancer Center (MSK) main hospital (Upper East Side of Manhattan, New York City), b exercise therapy adherence and adherence with health device usage, c patient estimated time commitment versus matched site-based virtual twin, and d patient estimated cost versus matched site-based virtual twin. Box length and line indicates the median value. Each grey dot represents a single patient.
Adherence to health devices is presented in Fig. 4b. Thirty-eight patients (72%) consented to dietary intake monitoring, with a mean adherence of 79% (173 days monitored of 219 days planned). Thirty-seven patients (70%) consented to CGM, with a mean adherence of 85% (810 days monitored of 948 days planned). Forty-four (83%) and 36 (68%) patients consented to remote blood and stool collection, respectively, with acquisition and delivery achieved in 77% (175 completed of 226 planned) and 90% (141 completed of 157 planned), respectively. The mean time commitment to conduct all study procedures using the DPEx across all dose levels was ~27 hours per patient (range: 9 to 70 hours) compared with a mean of ~68 hours (range: 15 to 159 hours) for a patient-matched virtual twin site-based model (Fig. 4c). Patient’s mean cost for study participation using the DPEx was $0 compared with an estimated mean cost of $707 (range: $66 to $2,426) for a patient-matched virtual twin site-based model (Fig. 4d). Investigator cost was $3,064 per patient (range: $2,425 to $4,126).
Discussion
Barriers to enrollment in clinical trials begin at the earliest stages of study conduct: patient screening and recruitment. In exercise therapy trials, investigators typically adopt one or a combination of three main approaches to screen and enroll patients: clinician referral, in-person recruitment, or mail contact. Each have important limitations. Clinician referral requires the oncologist or a member of the oncology team to be familiar with the study protocol and the specific eligibility requirements, which are often distinct from more familiar pharmacological protocols5. Trials of non-pharmacological interventions, especially if non-therapeutic, may be viewed as lower priority compared with therapeutic drug trials, especially given time constraints of oncology consultations. Success of clinician referral can be facilitated by having a dedicated member of the research team with detailed knowledge of the protocol attending in-clinic appointments. However, the number of potentially eligible patients is often low, and therefore inefficient and expensive. In response, investigators often use mail-based approaches, and although a greater number of patients are initially contacted, it is also inefficient as overall response rate is poor and many interested patients are ultimately ineligible for various reasons. Interested and eligible patients still require a site-based appointment for informed consent and baseline study assessments. As demonstrated in the present study, use of various technology solutions may hold significant promise to improve the efficiency and success of patient screening and enrollment, reduce study costs, and alleviate patient burden1,27,28. Nevertheless, a significant proportion of potentially eligible patients still decline participation. It will be important for future studies to ascertain the precise reasons for non-participation – e.g., lack of interest in exercise therapy or due to use of digital technology. Use of a technology affinity questionnaire during screening could identify and provide support those patients with such concerns.
Perhaps the most challenging aspect of clinical trials of exercise therapy is administration of the regimen itself. In the United States, nearly half of patients with advanced solid tumors drive more than 60 minutes (each way) to access a clinical trial29. Many face significant time and financial toxicities30. These present major barriers to participation in exercise therapy trials requiring at least two site visits per week over an extended period. Indeed, in our previous exercise-oncology trials using a site-based approach, ~30-40% of eligible patients declined participation due to geographical distance from the research center20,31,32. Additionally, investigator concerns regarding slow enrollment and poor adherence has directly impacted the nature and extent of the exercise therapy regimens investigated, with most clinical trials evaluating doses delivered two to three times weekly, despite national guidelines recommending five times weekly21. The substantial patient time and cost saving with DPEx is therefore important. The present study testing the effects of exercise therapy delivered up to 5-6 times weekly, with doses up to 450 minutes per week, and recruitment of patients an average of ~30-40 miles from the research center, likely would not have been possible without DPEx.
Limitations of site-based approaches, underscored by the COVID-19 pandemic, has ignited significant interest in the use of telemedicine / telehealth in exercise therapy trials and clinical exercise rehabilitation12,27,33,34,35. In general, these platforms consist of use of mobile health technology to promote increases in physical activity (via tailored notifications)36 or hybrid of telecare: remote monitoring of symptoms, vital parameters (such as ECG, blood pressure, weight) and exercise therapy sessions from external devices37. Exercise therapy regimens, however, are unstructured and conducted without remote, real-time monitoring limiting the ability to accurately deliver and quantify exercise therapy dose as well as modify the prescription (in real-time) in response to abnormal vital signs or symptoms38,39,40. Further, most other study procedures require site-based visits. DPEx alleviated patient burden whilst simultaneously enabling personalized delivery and accurate quantification collectively enabling implementation and testing of exercise therapy at high-fidelity. For investigators, use of such platforms may also offer financial benefit: higher costs of infrastructure to deliver remote exercise therapy with real time monitoring may be off-set by decreased costs of digital recruitment, faster accrual, and repurposing of premium expense site-based facility space.
Barriers to exercise therapy administration has also impacted the nature and extent of on-treatment monitoring, limiting correlative science investigation of intervention efficacy. Here we demonstrated the utility to deploy multiple wireless devices enabling passive and accurate monitoring of real-world data at high sampling resolution. This approach may provide novel insight into the integrated, longitudinal physiological response to exercise therapy and, in turn, facilitate identification of personalized digital biomarkers of treatment response; divergence from a patient’s pre-treatment baseline by real-time analysis could guide prescription modification to optimize exercise safety, tolerability, and efficacy27.
In summary, the DPEx platform enhanced multiple aspects of exercise therapy clinical trial procedures whilst simultaneously improving access, patient burden, and ultimately patient experience. If validated in other oncology populations and settings, among larger cohorts over the longer-term, platforms like the DPEx hold promise to improve the rigor, depth, and scope of clinical investigation of personalized exercise therapy and perhaps other therapeutic strategies in clinical populations.
Methods
DPEx overview and Phase 0a Development Cohort
Trial design and patients
The objective of the phase 0a Development Cohort was to establish the logistics and central components of DPEx. We recruited a convenience sample of three inactive (i.e., < 90 minutes of moderate or vigorous exercise per week21) women with post-treatment early-stage breast cancer at MSK. All three patients previously participated in an exercise therapy trial conducted by our team (NCT01186367; principal investigator LWJ), with all being cleared to participate in moderate-intensity ET20. The rationale for this approach was that all patients had an existing rapport with the study team and were willing to troubleshoot emergent platform feasibility or logistical issues as well as provide critical feedback. Additional eligibility criteria were: (1) ≥ 1 year to <7 years after completion of all definitive therapy (i.e., surgery and adjuvant radiation or chemotherapy, as applicable), (2) self-reporting less than 90 minutes/week of moderate or vigorous intensity exercise as per the Godin Leisure Time Exercise Questionnaire41, (3) no contraindications to moderate-intensity exercise via screening of the electronic health record for absolute and relative exercise contraindications, as per American Thoracic Society guidelines15, and screening clearance via the Physical Activity Readiness-Questionnaire plus16, (4) body mass index (BMI) ≤ 40 kg/m2, (5) access to an email address or MyMSK patient portal, and (6) sufficient space to house the study treadmill in-home for the study period. The study period was for up to six weeks. MSK’s IRB approved all study procedures. Digital technology procedures were reviewed and deemed low risk by MSK Information Security. All patients provided written informed consent prior to the initiation of any study procedures. The MSK Institutional Review Board (IRB) approved the study and all patients provided written informed consent prior to the initiation of any study procedures. Clinical trial registration NCT03813615; Date of registration: January 21, 2019.
Study procedures
Potential eligible patients were contacted by study staff. Interested patients were provided with a detailed overview of study procedures. In those remaining interested, study staff confirmed other major eligibility criteria (e.g., sufficient space for in-home treadmill) and if all eligibility criteria were met, a convenient date and time was scheduled to conduct the informed consent discussion. Informed consent was performed using a video conferencing platform. Specifically, patients (located at their preferred location) received a secure link via the MyMSK patient portal which connected them to the video call; a member of the study team then shared their screen following verification of standard patient identification (spelling of first and last name, date of birth or MRN). The patient and study staff member were able to review the electronic consent module (MSK eConsent System, v2) simultaneously in real-time. Consenting patients were provided remote screen control to sign the informed consent, a copy was then sent to the patient via mail, email, or Portal Secure Messaging (PSM) depending on preference.
Following final verification of eligibility and “written” informed consent, patients were couriered a study kit containing an electronic tablet (Apple iPad Mini v.5) and multiple Bluetooth-enabled devices including activity and heart rate monitor (Withings Steel HR), blood pressure monitor (Withings BPM Connect), and a body composition scale (Withings Body + ). Patients were also shipped a commercial treadmill (Jog Forma, Technogym, Inc), with installation performed by Technogym, Inc., technicians. Next, study staff conducted a two-way video orientation session to overview use of all study devices and implement a submaximal CFT. This test was performed in the patients’ home, remotely administered, and supervised using the video conference platform. Following successful completion of all pre-treatment assessments, study staff then scheduled the first remote exercise therapy session. After study completion, all study devices were returned to MSK using a pre-paid courier service whereas the treadmill was extracted, serviced, and stored by Technogym, Inc. for future use.
Study treatment
Exercise therapy
Exercise therapy was initiated within seven days of informed consent. Exercise therapy was standardized between patients based on modality, dose intensity, progression, and schedule. Dedicated study personnel with at least Bachelor’s degrees in Exercise Science implemented the interventions and individually monitored all sessions. Exercise physiologists’ adherence to the protocol was reviewed on weekly basis by the study investigator (LWJ). All sessions were by appointment only using MSK’s electronic scheduling system (Epic Hyperspace), with patients contacted within 24 hours of a scheduled missed session. Rescheduling of missed sessions was permitted within the study intervention period.
Exercise therapy consisted of up to 30 individualized, supervised treadmill walking (Jog Forma, Technogym, Inc) sessions 5 times weekly for 4 to 6 consecutive weeks. After a one to two week ‘ramp-up’ period in which duration and/or intensity were progressively increased, all subsequent sessions starting in week three were conducted at ≈70% of the pre-treatment submaximal exercise capacity for ≈30 minutes per session (planned amount: 150 mins/week), consistent with current guidelines for patients with cancer21. The intensity of each session was individually prescribed to each patient on the basis of workload (the speed and incline) measured during the pre-exercise cardiorespiratory fitness test. The corresponding heart rates measured at each workload during the CFT were then used in each training session to verify correct intensity (for each patient).
All sessions were performed in the patients’ residence with remote supervision and monitoring by study personnel. Prior to the initiation of all sessions, the patient measured resting blood pressure (Withings BPM or BPM Connect) and heart rate (Polar FT1) using the devices provided in the study kit. Patients were also queried whether they adhered to MSK Exercise-Oncology Program’s pre-exercise guidelines20,42. The patient then verbally communicated the blood pressure and heart rate readings to the MSK Exercise-Oncology Program exercise physiologist supervising the session. The planned session was only initiated if vital signs were within acceptable limits according to MSK Exercise-Oncology Program’s guidelines20. In addition, the planned session was also not initiated if the exercise physiologist observed any concerns that may compromise participant safety and/or the integrity of the planned session. Next, participants were instructed to enter the specific speed (mph) and incline (%) into the treadmill to initiate an initial warm-up ( ~ 5 minutes), following by the planned treatment session. During each session, the exercise physiologist recorded exercise therapy dose metrics (duration, speed, incline), as well as any dose modifications, in real-time via clinical electronic recording forms synced with each patients’ electronic health record.
Safety and verification of all sessions was evaluated using continuous monitoring of heart rate recorded on electronic recording forms linked to the EHR. Toxicity grading was performed in accordance with National Cancer Institute’s Common Terminology Criteria for Adverse Events (CTCAE) v5.0. Adverse events (AEs) were reviewed by the attending exercise physiologist, then graded and attributed following exercise sessions. AEs not resolved at the end of a session were reviewed with the patient at the beginning of the next scheduled session. During the intervention phase, AEs requiring adjustments to the planned prescription were performed according to the MSK Exercise-Oncology Program standards of care and/or at the discretion of the principal investigator (LWJ).
All data was automatically synced daily into the institutional database for storage, and linked to Tableau for visualization, permitting staff to overview exercise-related data (compliance, events) in real-time. Dose modification was permitted and performed using standardized criteria. The planned dose of all sessions was quantified as metabolic equivalent task (MET)– hours per session. The planned intensity of each session was multiplied by the corresponding session duration to calculate METs per session; all sessions were summed to derive total planned cumulative MET-hours per patient38.
Assessments
Programmatic feasibility was evaluated by DPEx feasibility, which was assessed by component reliability and quality (e.g., connection success rate), logistics (e.g., time needed for study overview and consent, study-kit delivery, and orientation), and CFT and exercise therapy safety, exercise adherence, and adherence to health device use.
Patient feasibility was assessed by rates of accrual, lost-to-follow up, exercise safety and adherence; and adherence with health biodevice use. Exercise adherence was evaluated by attendance (proportion of attended to planned sessions). “Planned” and “completed” dose of exercise was quantified as METs/session, with relative dose intensity (RDI) defined as the ratio of total “completed” to total “planned” cumulative dose. Safety was evaluated by the type and prevalence of serious (e.g., important medical events) and non-serious adverse events during exercise therapy sessions or CFTs only.
Exercise capacity was evaluated by a submaximal treadmill CFT using a modified Balke-Ware protocol19. Briefly, treadmill speed was initially set at 1.8 mph to 4.0 mph (depending on individual patient) with incline set at 0% followed by a 2% increase in the second minute and a 1% increase every minute thereafter until 80% of patient-determined age‐predicted maximum heart rate (((220 – age) – resting HR) x 0.8) + resting HR or volitional fatigue was achieved.
The CFT was performed in the patients’ residence using the study treadmill with remote real-time supervision and monitoring by staff exercise physiologists using the video conferencing platform. Achievement of 80% of patient age-predicted heart rate maximum within an 8–15-minute timeframe without observing any adverse events was considered a valid assessment. Specifically, during a CTF, patients we informed of the heart rate target and requested to notify the supervising exercise physiologist when the heart rate target was achieved (measured via a watch heart rate monitor). The supervising exercise physiologist then recorded the time at which 80% of heart rate maximum was achieved. All assessment-related data was recorded using electronic recording forms synced with the EHR. The CFT was performed at baseline and repeated within seven days of the final intervention session at post-intervention.
Safety procedures for a SAE during at-home CFT or an exercise therapy session
The following action plan outlines three related but distinct SAE scenarios for when a patient is conducting either CFT or exercise therapy at their residence. Since all sessions / study procedures are remotely supervised via telemedicine / video conferencing, the three scenarios are as follows: (1) study staff can maintain verbal and visual communication with the participant, (2) staff only have verbal communication, and (3) staff only have visual communication. Specific details of the emergency procedures in each three scenarios are described below. If other participants are present in the virtual training space during an SAE, the session(s) will be safely terminated, and the call will be ended to devote sole attention to the participant experiencing the SAE.
Scenario #1: Visual and Verbal Communication
-
a.
Terminate the session by asking the patient to stop the treadmill
-
i.
If unable to stop the treadmill the patient will be asked to step off the moving belt
-
i.
-
b.
Ask the participant to sit down and angle the tablet to maintain visual communication
-
c.
Ask the participant to describe their symptom(s) per the following:
-
i.
Quantify their symptom, for example pain, on a scale of 0 – 10
-
ii.
When did the symptom first start, has it stopped?
-
iii.
Have you experienced this before, if so, when?
-
iv.
Is there anything that has alleviated this symptom in the past?
-
i.
-
d.
Assess the participant’s signs of dysfunction (e.g., pale pallor, inappropriate blood pressure, gait disturbance)
-
i.
If the symptom(s) do not resolve and is not deemed to be life-threatening the participant will be asked to call their physician or report to an urgent care facility
-
1.
Exercise-Oncology staff will confirm the patient has appropriate transportation to urgent care
-
a.
When appropriate the Exercise-Oncology staff will call transportation per the patient’s request
-
a.
-
1.
-
ii.
No further sessions will be conducted until the patient is able to contact their physician and clearance is received
-
iii.
If the symptom(s) resolve and it is not deemed to be life-threatening the participant will be asked to call their physician to see if further follow up is advised
-
1.
No further sessions will be conducted until the patient is able to contact their physician
-
1.
-
iv.
If the situation is deemed to be life-threatening the Exercise-Oncology staff will advise the patient to call 911 or call 911 on the patient’s behalf.
-
1.
The contact information listed in Epic Hyperspace will be used to inform emergency services of the location when the patient is not responsive
-
2.
Exercise-Oncology Staff will provide information and aid in following directions given by emergency services as appropriate
-
3.
The call will not be terminated until emergency services arrive and instructs to end the call.
-
4.
No further sessions will be conducted until the documentation stating the patient is cleared to exercise (by attending physician) is received by the program
-
1.
-
i.
-
e.
Record the SAE details in full and inform management and the Protocol PI (LWJ) as soon as possible.
-
i.
Follow up documentation will be dictated by management and will comply with institutional requirements.
-
i.
Scenario #2: Verbal Communication Only
(if verbal contact is lost, Exercise-Oncology staff will call the patient via phone at contact information provided in Epic Hyperspace):
-
a.
Terminate the session by asking the patient to stop the treadmill
-
ii.
If unable to stop the treadmill the patient will be asked to move away from the moving belt
-
ii.
-
b.
Ask the participant to sit down or remain relaxed in a comfortable position
-
iii.
If this was a fall and there is a risk of head, neck or back injury the Exercise-Oncology staff will follow BLS procedures and advise the patient not to move.
-
iii.
-
c.
Ask the participant to describe their symptom(s) per the following:
-
iv.
Quantify their symptom, for example pain, on a scale of 0 – 10
-
v.
When did the symptom first start, has it stopped?
-
vi.
Have you experienced this before, if so, when?
-
vii.
Is there anything that has alleviated this symptom in the past?
-
viii.
Do you feel cold or hot?
-
ix.
Do you have feeling in your fingers and toes?
-
x.
Do you have any scrapes, cuts, or bruises?
-
iv.
-
d.
Assess the patient’s responses
-
xi.
If the symptom(s) do not resolve and is not deemed to be life-threatening the participant will be asked to call their physician or report to an urgent care facility
-
1.
Exercise-Oncology staff will confirm the patient has appropriate transportation to urgent care
-
a.
When appropriate the Exercise-Oncology staff will call transportation per the patient’s request
-
a.
-
2.
No further sessions will be conducted until the patient is able to contact their physician and clearance is received
-
1.
-
xii.
If the symptom(s) resolves and is not deemed to be life-threatening the participant will be asked to call their physician to see if further follow up is advised
-
1.
No further sessions will be conducted until the patient is able to contact their physician
-
1.
-
xiii.
If the situation is deemed life-threatening the Exercise-Oncology staff will advise the patient to call 911 or call 911 on the patient’s behalf.
-
1.
The contact information listed in Epic Hyperspace will be used to inform emergency services of the location when the patient is not responsive
-
2.
Exercise-Oncology staff will provide information and aid in following directions given by emergency services as appropriate
-
3.
The call will not be terminated until emergency services arrive and instructs to end the call.
-
4.
No further sessions will be conducted until the documentation stating the patient is cleared to exercise is received by the program
-
1.
-
xi.
-
e.
Record the SAE details in full and inform management and the Protocol PI (LWJ) as soon as possible.
-
xiv.
Follow up documentation will be dictated by management and will comply with institutional requirements.
-
xiv.
Scenario #3: Visual Communication Only
-
a.
Call 911 on the patient’s behalf if unable to contact the patient via phone
-
i.
The contact information listed in Epic Hyperspace will be used to inform emergency services of the location when the patient is not responsive
-
ii.
Exercise-Oncology staff will provide information and aid in following directions given by emergency services as appropriate
-
iii.
The call will not be terminated until emergency services arrive and instructs to end the call.
-
iv.
No further sessions will be conducted until the documentation stating the patient is cleared to exercise is received by the program
-
i.
-
b.
Record the SAE details in full and inform management and the Protocol PI (LWJ) as soon as possible.
-
v.
Follow up documentation will be dictated by management and will comply with institutional requirements.
-
v.
Diurnal and nocturnal patterns
Patients wore a smartwatch (Withings Steel HR) with infrared (wrist) sensor providing continuous heart rate monitoring, activity tracking (step count, distance), and sleep monitoring. Patients were instructed to wear this device for the entire study period. Participants were instructed to wear the smart watch 24/7 for the entire length of the study period. Patients were considered non-adherent for a study day if there was no activity or sleep data available for the defined 24-hour period.
Anthropometrics and blood pressure
Body weight, BMI, and body composition were evaluated using a wireless scale (Withings Body + ), whereas resting blood pressure was evaluated using wireless blood pressure monitor (Withings BPM or BPM Connect). Patients were instructed to perform both assessments daily. Patients were considered adherent if at least one measure per device per study day was recorded.
Phase 0b “Proof-of-Concept” Trial
Trial design and patients
The objective of the proof-of-concept trial was to examine the application of DPEx to investigate the feasibility and efficacy of exercise therapy in the pre-operative “window of opportunity” setting. The rationale for testing DPEx in this setting was two-fold: (1) the demonstrated efficacy of exercise “prehabilitation” to improve surgical outcomes in certain cancer types is significantly hampered by the feasibility to implement high-fidelity exercise therapy in a short-duration (typically 2 to 8 weeks) between diagnosis and surgery, and (2) window-of-opportunity trials provide a platform to interrogate the tumor molecular response to exercise. In this trial, we enhanced the DPEx platform to also include optional remote (in-home) blood and stool biospecimen collection and continuous glucose monitoring (CGM). We also introduced remote conduct of “group-based” exercise therapy sessions: use of the video conferencing platform multi-screen function to monitor up to three patients exercising at three unique locations simultaneously, with real-time monitoring. The MSK IRB approved the study and all patients provided written informed consent prior to the initiation of any study procedures. Clinical trial registration NCT03813615; Date of registration: January 21, 2019.
We conducted a prospective, single-arm study in inactive patients (i.e., < 90 minutes of moderate or vigorous exercise per week21) with histologically confirmed treatment naïve breast, endometrial, or prostate cancer scheduled for surgical resection at MSK. Additional eligibility criteria were: (1) age >18 years, (2) at least a 2-week window from study enrollment to scheduled surgical resection, (3) self-reporting ≤90 minutes/week of moderate or vigorous intensity exercise as per the GLTEQ, (4) screening clearance via the PAR-Q + 16, (5) BMI ≤ 40 kg/m2, (6) access to an email address or MSK patient portal, (7) primary attending surgical oncologist approval, and (8) sufficient space to house the study treadmill in-home for the study period. The study period commenced from baseline enrollment until scheduled surgical resection. MSK’s IRB approved all study procedures and all patients provided written informed consent prior to the initiation of any study procedures. To maximize the potential efficacy of exercise therapy in context of the very short duration of the pre-operative “window” an a priori objective was treadmill delivery \(\le\)48 hours of informed consent; a 100-mile radius was considered the maximal delivery zone to achieve this goal.
Study procedures
Potential patients were identified via a weekly, trial specific DataLine query. DataLine uses structured queries and NLP to search the institution’s database warehouse (integration of all clinical and operational subject areas) to screen on trial-specific eligibility criteria: type of cancer diagnosis, visit type, geographical distance from MSK, primary language, and provider. The generated list was then cross-referenced against MSK’s scheduling system to confirm surgery type and date. The primary MD provider was then contacted by email to confirm eligibility and permission for patient contact. Informed consent, delivery, and set-up of the study kit, and conduct of the CFT were performed in an identical manner to that described in the phase 0a development study. Following baseline assessments, study staff arranged a convenient time for a mobile phlebotomy service (Phlebotek Solutions Inc.) to perform in-home blood collection and scheduled the first remote exercise therapy session. After study completion, all study devices were returned to MSK using a pre-paid courier service whereas the treadmill was extracted, serviced, and stored by Technogym, Inc. for future use.
Study treatment
Exercise therapy was implemented in an identical manner as that described in the Phase 0a Development Cohort with the exception that intervention length was dependent on the presurgical window for each patient.
Assessments
Feasibility
Programmatic and patient feasibility was assessed by logistics (e.g., time needed for patient screening, time for treadmill delivery, adherence with weekly remote biospecimen collection) as well as rates of accrual, LTF, CFT and exercise therapy safety and adherence, and adherence with health device use. Exercise therapy adherence / tolerability assessed by multiple endpoints including: rate of LTF (completion of postintervention assessments), attendance (ratio of total attended to planned treatments), permanent discontinuation (treatment discontinuation prior to postintervention assessments), treatment interruption (missing ≥ 3 consecutive planned sessions), dose modification [≥ 10% of sessions requiring modification (reduction / escalation) of intensity and/or duration], pre-treatment dose modification (reduction of pre-treatment session intensity), early session termination (termination of session prior to planned duration), and RDI42. Safety was evaluated by the type and prevalence of serious (i.e., life-threatening, hospitalization, significant incapacity, important medical events) and non-serious (e.g., knee, back pain) adverse events during exercise therapy sessions. Session heart rate and blood pressure response was compared to vitals obtained during the CFT; abnormal response was defined as ≥ 10 beats per min or ≥10 mmHg outside prescribed range.
Physiological response
Physiological response was assessed by evaluating change in: (1) diurnal and nocturnal patterns (i.e., sleep, sedentary, mobility (non-exercise) evaluated by a smartwatch (Withings Steel HR) with infrared (wrist) sensor; (2) exercise capacity evaluated by a submaximal treadmill CFT using a modified Balke-Ware protocol19 at baseline and post-intervention (prior to surgical resection). All emergency procedures were conducted in an identical manner to those described in the Development cohort; (2) anthropometrics (i.e., body weight, body composition) evaluated daily using a wireless scale (Withings Body + ); (3) heart rate and resting blood pressure were evaluated every 10 minutes 24/7 using the wireless smartwatch (Withings Steel HR) and daily using a wireless blood pressure monitor (Withings BPM Connect), respectively; and (4) interstitial fluid glucose (Abbott Freestyle Libre Pro) assessed every 15 minutes 24/7 up to 14 days per sensor (enough sensors were provided for the entire study period). Patients were also provided with a 50 mg glucose drink to evaluate glucose response at baseline and postintervention.
Time and financial cost
We estimated the total time commitment and cost for DPEx compared with a hypothetical, traditional site-based at MSK Main Campus on the Upper East Side of Manhattan in New York City model (i.e., patient-matched virtual twin). Calculation of patients’ total time commitment included the number of hours to complete all study assessments (at baseline, weekly/daily, and follow-up) and all planned exercise therapy sessions. Time commitment to a hypothetical medical facility-based approach also included estimated travel time from patient’s residence to MSK main campus, utilizing most convenient form of transportation (car or public transit), depending on geographical distance from MSK main campus. Total cost considered either the cost of gas, tolls, and parking, or a roundtrip MTA subway ride ($5.50), for each attended visit (assessment or exercise therapy session) for each patient, according to geographic location. Investigator cost of the DPEx included flat rate for treadmill delivery/installation and extraction ($500/each), digital health devices, CGM materials, Apple iPad, and other miscellaneous items, estimated associated shipping fees for equipment and assessments, as needed, and mobile phlebotomy services (e.g., in-home blood collection plus mileage reimbursement).
Remote blood collection
Remote (in-home) blood collection was coordinated using Workpath, Inc. Workpath – a HIPAA compliant platform – organizes, verifies, and dispatches mobile medical services. Using the Workpath dashboard and partnering with Phlebotek, Inc. a third-party mobile phlebotomy vendor, appointments were scheduled for a trained phlebotomist to visit a patients’ residence to collect fasted blood samples. The dashboard also permits real-time monitoring enabling blood collection and delivery to be tracked remotely by the Exercise Oncology Program study team. Participants were instructed to adhere to MSK’s Exercise-Oncology Program blood collection procedures prior to every blood collection. Blood collection was scheduled between 0700 and 1000 h, after a 12-hr water-only fast. Two separate 7 ml EDTA, one 10 ml Serum, and one 10 ml STRECK tube blood samples were obtained. Samples were then transported to a designated MSK facility for processing and stored at −80 °C. Blood collection was performed weekly.
Remote stool collection
Remote (in-home) stool collection was coordinated by study staff. At pre-intervention patients were shipped a stool collection kit that included collection tub and frame, ice packs, packing materials, pre-paid return shipping box and detailed instructions. Patients were instructed to collect the sample Monday to Thursday, then contact study staff immediately (via email or PSM) following sample collection. Once notified, study staff arranged UPS package pick-up. Another stool collection kit was then prepared and shipped to the patient for next collection. Stool collection was performed weekly, as appropriate.
CGM and oral glucose challenge
CGM was performed using the Abbott Freestyle Libre Pro system, providing measurement of interstitial glucose concentrations every 15 minutes for up to 14 days; the patient was provided with enough sensors to cover the entire study period, as necessary. Specifically, the CGM kit included a prepackaged sensor, applicator, and reader to activate the sensor. After 14 days of continual wear, the sensor was removed and returned to MSK study staff for analysis using a pre-paid courier service. The Abbott Freestyle Libre Pro system sensor does not meet the FDA Significant Risk (SR) definition under 21 CFR 812.3(m) and therefore was determined to be a Non-Significant Risk (NSR) device. For the oral glucose challenge assessment, the patient consumed a 50 g glucose drink (Azer Scientific) during the first and final week of the study period in a fasted state. The patient was instructed not to consume any food / water and not to exercise for at least one hour following drink consumption. This assessment was used as a manipulation check / test to verify utility of CGM to measure changes in interstitial glucose concentrations within the expected physiological limits.
Phase 1a Exercise Level-Finding Trial
Trial design and patients
We next conducted a phase 1 level-finding trial of neoadjuvant exercise therapy in men with localized prostate cancer. The primary objective was to identify the recommended phase 2 dose for future investigation. In the present context, we leveraged conduct of this trial to further examine feasibility of the DPEx to administer higher exercise therapy doses and in a larger patient cohort. Inactive patients (i.e., < 90 minutes of moderate or vigorous exercise per week) with histologically confirmed treatment-naïve prostate cancer with at least a 2-week window from enrollment to scheduled surgical resection at MSK were eligible. Patients were allocated to six escalated exercise therapy dose levels (i.e., 90, 150, 225, 300, 375, and 450 minutes per week) across 3 to 7 individual sessions per week (over a 7-day period) for 2 to 12 consecutive weeks (i.e., 6 to 59 planned independent sessions) depending on the pre-operative window. All aspects of study conduct including patient identification and enrollment and exercise therapy delivery and quantification, and dynamic monitoring of lifestyle and physiological changes were conducted in an identical manner as in phase 0b. DPEx feasibility end points, study procedures, exercise therapy and assessments were identical to those in the phase 0b study. The MSK IRB approved the study and all patients provided written informed consent prior to the initiation of any study procedures. Clinical trial registration NCT03813615; Date of registration: January 21, 2019.
Data integration, quality assurance, and storage
A Clinical Research Coordinator (CRC) under the close supervision of the Clinical Research Manager (CRM) in the Exercise Oncology Program was assigned to the study. The responsibilities of the CRC included project compliance, data collection, abstraction and entry, data reporting, regulatory monitoring, problem resolution and prioritization, and to coordinate the activities of the protocol study team. The data collected in this study was entered into a secure database (REDCap). The data for continuous lifestyle monitoring was stored in Splunk, a secure database and data visualizer. The principal investigator (LWJ) maintained ultimate responsibility for the study. Routine data quality reports were generated to assess missing data and inconsistencies. Accrual rates and extent and accuracy of evaluations and follow-up were monitored periodically throughout the study period and potential problems brought to the attention of the study team for discussion and action. Random-sample data quality and protocol compliance audits were conducted by the study team, under the direction of the CRM.
Information security assessment and data privacy
Security assessments were performed on all study devices, applications, and software to ensure that both the risk and potential for exploitation of such tools was permissible according to MSK standards. Risk assessment consisted of four stages: (1) profiling and scope of the project, (2) development and documentation of all technological and security aspects, (3) analyzation and testing as applicable for custom developed tools, and (4) review of the assessment and remediation of any identified risk. The risk assessment process ranged from several weeks to several months, depending on the complexity of each device / component. Risk assessment of all devices / components were either defined as no risk or low risk such that the vendor and/or Exercise Oncology Service team developed detailed remediation plans with achievable timelines and acceptance of the identified risk by the designated authority (MSK SVP) for implementation.
Data integration
Raw data was collected from all study devices during trial conduct and at postintervention. Diurnal and nocturnal patterns data from deidentified Withings Health Mate accounts were downloaded to a secure, dedicated MSK server. CGM data from sensors was extracted using Libreview software, which also allowed for raw data downloads to a secure MSK server. Data was then reviewed for inaccuracies and compiled into a master file for each patient by Exercise Oncology clinical trial personnel.
Study oversight
The trial was designed and conducted by the authors. All the authors confirm that the trial conformed to the protocol and attest to the accuracy and completeness of the data. The senior authors wrote the first draft of the manuscript. All authors had full access to the data and were involved in data interpretation, in writing and reviewing subsequent manuscript drafts, and in making the decision to submit the manuscript for publication. Study conduct was monitored by the data safety and monitoring board at MSK.
Data analysis
All presented data was summarized using descriptive statistics and no formal statistical testing was conducted. Figures were also combined using Inkscape (v0.92) and Keynote (v9.0.2).
Data availability
This paper reports on the development, feasibility, and initial utility of DPEx. Hence, no data is being made available in conjunction with this publication. Nevertheless, feasibility data will be made available for all reasonable requests and a minimal dataset will be provided necessary to interpret, replicate and build upon the methods or findings reported in the article.
Code availability
Not applicable as no code was used for data analysis in this manuscript.
References
Inan, O. T. et al. Digitizing clinical trials. NPJ Digit Med 3, 101 (2020).
Marquis-Gravel, G. et al. Technology-Enabled Clinical Trials: Transforming Medical Evidence Generation. Circulation 140, 1426–1436 (2019).
Li, B. T. et al. Reimagining patient-centric cancer clinical trials: a multi-stakeholder international coalition. Nat. Med 28, 620–626 (2022).
Steins Bisschop, C. N. et al. Control group design, contamination and drop-out in exercise oncology trials: a systematic review. PLoS One 10, e0120996 (2015).
Adams, S. C. et al. Comparing the reporting and conduct quality of exercise and pharmacological randomised controlled trials: a systematic review. BMJ Open 11, e048218 (2021).
Villareal, D. T. et al. Aerobic or Resistance Exercise, or Both, in Dieting Obese Older Adults. N. Engl. J. Med 376, 1943–1955 (2017).
Kraus, W. E. et al. Effects of the amount and intensity of exercise on plasma lipoproteins. N. Engl. J. Med 347, 1483–1492 (2002).
Hambrecht, R. et al. Effect of exercise on coronary endothelial function in patients with coronary artery disease. N. Engl. J. Med 342, 454–460 (2000).
Scott, J. M. et al. Efficacy of Exercise Therapy on Cardiorespiratory Fitness in Patients With Cancer: A Systematic Review and Meta-Analysis. J. Clin. Oncol. 36, 2297–2305 (2018).
Ward, T. J. C., et al. Change in VO2peak in response to aerobic exercise training and the relationship with exercise prescription in people with COPD: A systematic review and meta-analysis. Chest (2020).
Newton, R. U., Hart, N. H. & Clay, T. Keeping Patients With Cancer Exercising in the Age of COVID-19. JCO Oncol. Pr. 16, 656–664 (2020).
Scherrenberg, M., et al. The future is now: a call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur J Prev Cardiol, 2047487320939671 (2020).
Li, G. et al. Digitalized Adaptation of Oncology Trials during and after COVID-19. Cancer Cell 38, 148–149 (2020).
Sasso, J. P. et al. A framework for prescription in exercise-oncology research. J. Cachexia Sarcopenia Muscle 6, 115–124 (2015).
American Thoracic, S. & American College of Chest, P. ATS/ACCP Statement on cardiopulmonary exercise testing. Am. J. Respir. Crit. Care Med 167, 211–277 (2003).
Warburton, D. E. et al. Evidence-based risk assessment and recommendations for physical activity clearance: Consensus Document 2011. Appl Physiol. Nutr. Metab. 36, S266–S298 (2011).
Kenjale, A. A. et al. Pre-exercise participation cardiovascular screening in a heterogeneous cohort of adult cancer patients. Oncologist 19, 999–1005 (2014).
Jones, L. W., Eves, N. D., Haykowsky, M., Joy, A. A. & Douglas, P. S. Cardiorespiratory exercise testing in clinical oncology research: systematic review and practice recommendations. Lancet Oncol. 9, 757–765 (2008).
Balke, B. & Ware, R. W. An experimental study of physical fitness of Air Force personnel. US Armed Forces Med J. 10, 675–688 (1959).
Scott, J. M. et al. Effects of Exercise Therapy Dosing Schedule on Impaired Cardiorespiratory Fitness in Patients With Primary Breast Cancer: A Randomized Controlled Trial. Circulation 141, 560–570 (2020).
Campbell, K. L. et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med Sci. Sports Exerc 51, 2375–2390 (2019).
Boule, N. G., Haddad, E., Kenny, G. P., Wells, G. A. & Sigal, R. J. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA 286, 1218–1227 (2001).
Bite AI Inc. Bitesnap - Photo Food Journal. (2020).
Ligibel, J. A., et al. Exercise, Diet, and Weight Management During Cancer Treatment: ASCO Guideline. J Clin Oncol, JCO2200687 (2022).
Tao, J. J., et al. Real-World Outcomes of an Automated Physician Support System for Genome-Driven Oncology. JCO Precis Oncol 3(2019).
Jones LW, M. C., et al. Phase 1a, decentralized trial of neoadjuvant exercise therapy in prostate cancer. JAMA Oncol (in press).
Pandey, A. C., Golbus, J. R. & Topol, E. J. Cardiac rehabilitation in the digital era. Lancet 398, 16 (2021).
Adams, D. V., Long, S. & Fleury, M. E. Association of Remote Technology Use and Other Decentralization Tools With Patient Likelihood to Enroll in Cancer Clinical Trials. JAMA Netw. Open 5, e2220053 (2022).
Galsky, M. D. et al. Geographic accessibility to clinical trials for advanced cancer in the United States. JAMA Intern Med 175, 293–295 (2015).
Gupta, A., Eisenhauer, E. A. & Booth, C. M. The Time Toxicity of Cancer Treatment. J. Clin. Oncol. 40, 1611–1615 (2022).
Scott, J. M. et al. Timing of exercise therapy when initiating adjuvant chemotherapy for breast cancer: a randomized trial. Eur. Heart J. 44, 4878–4889 (2023).
Scott, J. M. et al. Effects and tolerability of exercise therapy modality on cardiorespiratory fitness in lung cancer: a randomized controlled trial. J. Cachexia Sarcopenia Muscle 12, 1456–1465 (2021).
Meyer, M. et al. Current state of home-based exercise interventions in patients with congenital heart disease: a systematic review. Heart 106, 333–341 (2020).
Chan, C., Yamabayashi, C., Syed, N., Kirkham, A. & Camp, P. G. Exercise Telemonitoring and Telerehabilitation Compared with Traditional Cardiac and Pulmonary Rehabilitation: A Systematic Review and Meta-Analysis. Physiother. Can. 68, 242–251 (2016).
Cheville, A. L., Moynihan, T., Herrin, J., Loprinzi, C. & Kroenke, K. Effect of Collaborative Telerehabilitation on Functional Impairment and Pain Among Patients With Advanced-Stage Cancer: A Randomized Clinical Trial. JAMA Oncol. 5, 644–652 (2019).
Jeganathan, V. S. et al. Virtual AppLication-supported Environment To INcrease Exercise (VALENTINE) during cardiac rehabilitation study: Rationale and design. Am. Heart J. 248, 53–62 (2022).
Orzechowski, P. et al. Assessment of ECG during hybrid comprehensive telerehabilitation in heart failure patients-Subanalysis of the Telerehabilitation in Heart Failure Patients (TELEREH-HF) randomized clinical trial. Ann. Noninvasive Electrocardiol. 26, e12887 (2021).
Nilsen, T. S. et al. Novel Methods for Reporting of Exercise Dose and Adherence: An Exploratory Analysis. Med Sci. Sports Exerc 50, 1134–1141 (2018).
O’Connor, C. M. et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 301, 1439–1450 (2009).
McIsaac, D. I. et al. Home-based prehabilitation with exercise to improve postoperative recovery for older adults with frailty having cancer surgery: the PREHAB randomised clinical trial. Br. J. Anaesth. 129, 41–48 (2022).
Godin, G. & Shephard, R. J. A simple method to assess exercise behavior in the community. Can. J. Appl Sport Sci. 10, 141–146 (1985).
Scott, J. M. et al. Feasibility, safety, and efficacy of aerobic training in pretreated patients with metastatic breast cancer: A randomized controlled trial. Cancer 124, 2552–2560 (2018).
Acknowledgements
This trial was funded by a grant from Gateway for Cancer to LWJ. LWJ was supported in part by funding from the National Cancer Institute (CA164751, CA244866, CA272678), AKTIV Against Cancer, and the Memorial Sloan Kettering Cancer Center Support Grant/Core Grant (P30 CA008748). PCB and LYL were supported by the UCLA Cancer Center Support Grant (P30 CA016042).
Author information
Authors and Affiliations
Contributions
W.P.U. Conceptualization, project administration, writing – review and editing; M.G.M. Data curation, supervision, methodology, project administration, writing – review and editing; C.P.L. Data curation, supervision, project administration, writing – review and editing; G.A.F. Methodology, project administration, writing – review and editing; S.S.C. Data curation, project administration, writing – review and editing; S.E.E. Conceptualization, formal analysis, writing – review and editing; L.Y.L. Formal analysis, visualization, writing – review and editing; B.L.T. Formal analysis, visualization, writing – review and editing; C.S.M. Methodology, formal analysis, writing – review and editing; J.A.L. Methodology, formal analysis, writing – review and editing; K.J.V.Z. Data curation, writing – review and editing; G.J.G. Data curation, writing – review and editing; J.J.M. Data curation, writing – review and editing; C.T.D. Resources, writing – review and editing; B.E. Data curation, writing – review and editing; V.P.L. Data curation, writing – review and editing; J.A.E. Data curation, writing – review and editing; J.M.S. Methodology, writing – review and editing; P.C.B. Methodology, visualization, supervision, writing – review and editing; L.W.J. Conceptualization, methodology, funding acquisition, writing – original draft, and review and editing. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The Authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Underwood, W.P., Michalski, M.G., Lee, C.P. et al. A digital, decentralized trial of exercise therapy in patients with cancer. npj Digit. Med. 7, 304 (2024). https://doi.org/10.1038/s41746-024-01288-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41746-024-01288-1