Abstract
With expanded telehealth availability in primary care, its impact on quality of care and associated costs remains debated. Analyzing 199,829 Medicare beneficiaries in Mississippi (2019–2021), we found telehealth utilization associated with significant sociodemographic disparities, reduced inpatient admissions, and lower 30-day readmissions. By accounting for primary care utilization, our findings suggest that the higher absolute costs observed among telehealth users may reflect underlying healthcare needs rather than telehealth utilization.
Similar content being viewed by others
Introduction
Primary care is fundamental to functional healthcare systems, contributing to better health outcomes, illness prevention, and reduced per capita healthcare costs1. However, transportation barriers pose well-documented obstacles to accessing primary care, especially in rural and underserved areas. The COVID-19 pandemic drastically transformed healthcare delivery through telehealth, allowing remote access to healthcare services. The U.S. Medicare introduced a series of telehealth coverage expansions in 2020, including lifting geographic restrictions for originating sites. These changes enabled many primary care practices to adopt telehealth2,3.
While telehealth has shown promise as a cost-saving measure for Medicare beneficiaries4,5,6, debates continue about its future coverage, particularly regarding its impact on access, quality, and costs of primary care2,7,8,9,10. Recent studies have highlighted barriers to telehealth access for marginalized populations and have shown mixed results regarding its impact on healthcare costs and health outcomes2,5,6,7,8,9. Importantly, the pandemic brought severe disruptions to individuals, especially vulnerable populations, and drastic shifts in healthcare practices11, making it essential to account for dynamic factors when evaluating its impact. Mississippi, a predominantly rural and underserved state in the U.S., faces additional challenges in primary care access, with one-third of its population residing in primary care health professional shortage areas (HPSAs)12.
Motivated by these real-world challenges, we conducted a study to illustrate and evaluate the impact of telehealth for primary care on Medicare healthcare resource utilization (HCRU), spending, and medication adherence among Mississippi Medicare beneficiaries before and during the COVID-19 period. By incorporating both time-invariant and time-varying factors of beneficiary sociodemographics and primary care utilization practices, we explore the implications of telehealth in a dynamic healthcare environment. Furthermore, we highlight the digital divide and its influence on healthcare access and economic outcomes, offering nuanced insights to inform future evaluations, policy discussions, and practices.
Methods
Study design and participants
We conducted a retrospective cohort study using Mississippi Medicare claims data (2019–2021), with 2019 as the baseline year, to compare sociodemographic characteristics, healthcare resource utilization (HCRU), spending, and medication adherence between telehealth and non-telehealth primary care users. The study included adult beneficiaries (aged 18 and older) continuously enrolled in Medicare Parts A, B, and D who accessed primary care services. Beneficiaries with Part C coverage or entitlement due to end-stage renal disease were excluded. Details on the identification of primary care and telehealth services are provided in Supplementary “1.1 Telehealth for Primary Care Services.”
Variables
Demographic characteristics were treated as time-invariant, while socioeconomic and primary care utilization factors were considered time-varying. Primary outcomes included HCRU and spending. HCRU metrics comprised outpatient visits, Emergency Department (ED) visits, inpatient admissions, and 30-day readmissions. Spending was measured for medical and pharmacy expenditures, with each categorized into Medicare (Part D for pharmacy spending), out-of-pocket (OOP), and gross spending. Secondary outcomes focused on adherence to antidiabetic, antihypertensive, and antilipidemic medications among the multi-condition subgroup, comprising participants with diabetes, hypertension, and hyperlipidemia.
Detailed definitions and calculations of variables are provided in Supplementary “1.2 Variables.”
Statistical analysis
Descriptive statistics, along with Wilcoxon rank-sum tests, X2 tests, and odds ratio estimations, were used to summarize sociodemographic and primary care utilization differences between telehealth participants and non-telehealth participants from 2019–2021. We calculated the number and percentage of participants who accessed each provider type, along with the mean and standard deviation of the proportion of services provided by each provider type across participants.
To evaluate the effect of telehealth utilization on primary and secondary outcomes, we created a telehealth utilization indicator for each respective year and employed the Marginal Structural Modeling (MSM). Previous studies have shown that telehealth is often utilized by patients who require frequent primary care visits13,14. To address this, we applied Inverse Probability of Treatment Weighting (IPTW) to account for both sociodemographic and primary care utilization covariates15. This was followed by weighted mixed-effects models to control for time-invariant and time-varying confounders, incorporating individual-level random effects. A log link function was applied for HCRU and spending outcomes, with a Poisson distribution used for HCRU outcomes and a Gamma distribution for spending outcomes. The MSM analysis was conducted for the entire study population and the multi-condition subgroup (see details in Supplementary “1.3 Marginal Structural Modelling (MSM)”). Covariate balance was assessed using absolute standardized differences16. All absolute standardized differences were reduced to below 0.25 post-weighting, indicating sufficient balance (Fig. 1 and Supplementary Table 6).
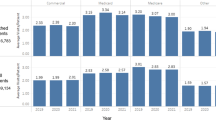
Panels a, b, c, and d illustrate the quarterly trends in outpatient visits, Emergency Department (ED) visits, inpatient admissions, and 30-day readmissions of telehealth (TH) and non-telehealth (non-TH) participants. The vertical dashed line indicates the last quarter (2019-Q4) prior to the onset of the public health emergency.
Two-tailed statistical tests with an alpha level of 0.05 were used to determine significance. All analyses were conducted using SAS (version 9.4, SAS Institute Inc., Cary, NC) and R statistical software.
This study was approved by the University of Mississippi Medical Center institutional review board with a waiver of informed consent and Health Insurance Portability and Accountability Act (HIPAA) authorization.
Results
Sociodemographic disparities
Among 199,829 identified Medicare beneficiaries, 73,252 (36.65%) utilized telehealth services in primary care during 2019–2021, including 1201 (0.60%) in 2019, 62,636 (31.34%) in 2020, and 32,431(16.22%) in 2021. Telehealth was more commonly accessed by participants who were younger (under 55 years), female, White, entitled due to disability, dually enrolled in Medicaid, residing in non-rural nor non-HPSA designated areas, and had a higher CCI (all P values < 0.001). Telehealth users had a higher Bice-Boxerman COCI and more primary care visits in 2019 (both P values < 0.001). Additionally, telehealth users accessed a broader range of primary care providers, though with a lower proportion of services from primary care physicians, surgeons, and other physicians (all P values < 0.001) (Table 1).
With overall trends reflecting fluctuations in the dynamic healthcare environment, primary care telehealth users consistently exhibited higher HCRU and spending compared to non-telehealth participants (Fig. 2, Supplementary Figs. 1, 2, Supplementary Tables 3–5). However, after applying the IPTW to account for time-invariant and time-varying confounders of sociodemographics and primary care practices, telehealth usage was significantly associated with a 2.3% increase in outpatient visits and a 5.4% increase in ED visits, but a 4.3% decrease in inpatient admissions and a 2.4% decrease in 30-day readmissions. Additionally, telehealth was associated with significant decreases in all spending outcomes: a 10.8% decrease in Medicare medical spending, a 27.0% decrease in beneficiary OOP medical spending, and an 11.6% decrease in gross medical spending. Decreases were also noted in all pharmacy spending categories, with a 14.9% decrease in Medicare Part D spending, a 0.8% decrease in beneficiary OOP pharmacy spending, and a 2.8% decrease in gross pharmacy spending (all P values ≤ 0.001) (Table 2).
Subgroup analysis of 43,257 participants with multiple chronic conditions, of whom 18,653 (43.12%) used primary care telehealth, revealed consistent patterns (Supplementary Table 8). Post-IPTW, primary care telehealth usage was associated with an increase in ED visits, but decreased all other HCRU and spending outcomes (all P values < 0.001) (Supplementary Table 11). Moreover, telehealth was also associated with a 1.6% decrease in antidiabetic medication adherence, a 1.0% decrease in antilipidemic medication adherence, but a 1.2% increase in antihypertensive medication adherence (all P values < 0.001) (Supplementary Table 12).
Discussion
Our findings demonstrate that telehealth in primary care is associated with reduced inpatient admissions, 30-day readmissions, and medical and medication spending, while highlighting persistent sociodemographic disparities in telehealth utilization. By accounting for time-invariant and time-varying factors, particularly primary care utilization patterns that reflect the dynamic healthcare environment during COVID-19 pandemic, we provide a nuanced yet thought-provoking perspective on its healthcare resource utilization, economic, and access implications.
Impact on healthcare access, resource utilization, and medication adherence
Telehealth was more commonly accessed by younger beneficiaries, females, White individuals, those entitled to Medicare due to disability, Medicaid enrollees, those residing in non-rural, non-HPSA regions, and individuals with a higher CCI. These findings align with existing literature6,17, highlighting a significant digital divide and suggesting that certain sociodemographic groups, particularly older adults, racial minorities, and those in rural or underserved areas with poor health status may face greater barriers to accessing telehealth.
The observed increase in outpatient and ED visits post-weighting for the entire sample suggests that telehealth may facilitate triaging and expanded access to care, enabling earlier interventions, which could ultimately reduce hospitalizations. Driven by convenience and the patient-perceived need for immediate medical attention, patients may use ED visits as a substitute for outpatient care, sometimes after contacting the office of primary care physicians18,19,20. However, these increases did not translate into higher inpatient or readmission rates. These were actually reduced, potentially indicating improved care coordination or more effective chronic condition management.
Subgroup analysis among beneficiaries with multiple chronic conditions further supported the robustness of most findings, while revealing nuances in outpatient utilization patterns for those with more complex healthcare needs. Unlike the entire sample, telehealth use in this subgroup was associated with a decrease in outpatient visits, likely reflecting both the more complex medical needs and telehealth-facilitated medication reconciliation or titration21, thus reducing the need for outpatient care.
The subgroup analysis also showed that telehealth was associated with improved adherence to antihypertensive medication but reduced adherence to antidiabetic and antilipidemic medications. This may reflect the relative ease of managing hypertension compared to diabetes, which often requires more frequent monitoring and treatment adjustments that are harder to achieve remotely22,23. Additionally, the COVID-19 pandemic limited in-person outpatient services, potentially affecting medication adherence. Future work should further examine how telehealth can complement in-person care to enhance service quality and medication adherence. Hyperlipidemia, in contrast, is typically asymptomatic, yet antilipidemic medications can cause side effects requiring closer follow-up and in-person consultations, potentially impacting adherence24. Moreover, antidiabetic and antilipidemic medications are generally more expensive than antihypertensive medications. As medication adherence often involves out-of-pocket costs, financial strains may further hinder adherence, particularly for patients managing multiple chronic conditions25.
While telehealth enhances access to primary care services, it may not fully address sociodemographic barriers or alleviate the financial burdens that impact medication affordability, which are crucial for effective chronic disease management. Together with the observed sociodemographic disparities in accessing telehealth, these findings underscore the urgent need to optimize the future telehealth policy to better address the complex needs of underserved populations and ensure the access to care for all.
Reconsidering quality and cost narratives
Some studies have linked telehealth services to lower quality, citing increases in hospitalizations for ambulatory care-sensitive (ACS) conditions9, including chronic and acute conditions such as hypertension and diabetes, for which hospitalization can be potentially preventable. However, ACS metrics were originally designed to assess access to care for the uninsured rather than the quality of care provided. Their widespread misuse as proxies for quality of care in recent years has raised concerns among many researchers26. Careful selection of outcomes and thoughtful interpretation are essential when translating statistical significance into practical policy recommendations7,8.
Contrary to recent studies that link telehealth to lower quality and higher costs8,9, our results indicate that telehealth use was associated with reductions across all medical and pharmacy spending categories. This difference may stem from our focus on telehealth within the primary care context, emphasizing accessibility, continuity, coordination, comprehensiveness, and whole-person care1. Unlike prior studies7,8,9, we adjusted for dynamic primary care utilization factors as confounders, serving as proxies for the key dimensions of primary care. As highlighted by a previous study13, telehealth was mostly utilized by patients whose medical needs required multiple primary care visits, further supporting the importance of these adjustments. By incorporating time-invariant and time-varying sociodemographic and primary care practice factors, our approach accounts for key aspects of the evolving healthcare environment during the COVID-19 pandemic, providing a more nuanced understanding of telehealth’s impact.
The persistent upstream of health disparities
Social determinants of health (SDoH) often drive patients’ healthcare needs, prompting them to use telehealth to fulfill primary care needs. Our findings, coupled with increased disparities, healthcare utilization and spending reported in other studies11,17, may reflect a higher underlying healthcare need rather than a direct consequence of telehealth usage itself. By careful adjustments, our findings suggest the need for future research to disentangle whether increased healthcare utilization is driven by patients’ needs leading to telehealth use, rather than telehealth use driving increased utilization and costs.
Equity efforts should span every level from the upstream of SDoH to access equity, service equity, and ultimately health equity. By focusing on these interconnected dimensions, future telehealth policies and interventions can better support underserved populations while ensuring that telehealth fulfills its promise of equitable and effective care. As recommended by Nakamoto et al., given the dynamic nature of the healthcare landscape, it is imperative to continuously monitor the policy impacts on quality and spending8. Before COVID-19, telehealth was primarily designed to provide accessible care for underserved populations. With its expansion during the pandemic, future efforts should carefully consider how to broaden access while addressing pre-existing disparities across the spectrum, from upstream SDoH to downstream health outcomes.
Limitations
Several limitations of this study should be noted. First, our focus on Medicare beneficiaries in Mississippi may limit the generalizability of our findings to other states or populations, particularly those in more urbanized or resource-rich regions. Second, although we controlled for time-invariant and time-varying sociodemographic and primary care practice confounding factors, the findings rely on the no unobserved confounders assumption. Provider-level information within primary care practices that was not captured may have influenced our findings. The rapid expansion of telehealth during the pandemic may have introduced temporary shifts in healthcare practices that are not fully reflected in our data.
Conclusions
Given the high demand for primary care in medically underserved regions, this perspective deepens the understanding of the effectiveness and equity of telehealth in primary care. By accounting for dynamic primary care utilization factors as proxies for key dimensions of primary care practices, our analysis provides a nuanced evaluation of telehealth’s impact. Our findings challenge the recent notion that observed increased costs are a consequence of telehealth use, suggesting they may instead reflect patients’ underlying healthcare needs. However, the persistent SDoH disparities in telehealth access underscore the need for targeted interventions to bridge the digital divide. As healthcare policies continue to evolve, further research is warranted to continuously explore how telehealth can be integrated into the healthcare system in a cost-effective, sustainable, and equitable manner that prioritizes quality care for all8,27,28.
Data availability
Data were obtained from the Centers for Medicare & Medicaid Services (CMS) under a data use agreement and are not publicly available.
References
Peikes, D., Taylor, E. F., O’Malley, A. S. & Rich, E. C. The Changing Landscape Of Primary Care: Effects Of The ACA And Other Efforts Over The Past Decade: A description of primary care delivery system reform models developed and tested over the past decade by the Center for Medicare and Medicaid Innovation, which was created by the Affordable Care Act. Health Aff. 39, 421–428 (2020).
Zhang Y, Lal LS, Chandra S, Swint JM. Shifting Patterns in Primary Care Telehealth Utilization Among Medicare Beneficiaries and Providers. J Prim Care Community Health. 16, 2025. https://doi.org/10.1177/21501319251323983.
Chang, J. E. et al. Rapid transition to telehealth and the digital divide:implications for primary care access and equity in a post-COVID era. Milbank Q. 99, 340–368 (2021).
Centers for Medicare & Medicaid Services. Proposed Rules (ed Department of Health and Human Services) 54982-55088 (Department of Health and Human Services, Federal Register, 2018).
Peña, M. T. et al. Telemental health use is associated with lower health care spending among Medicare beneficiaries with major depression. Med. Care 62, 132–139 (2024).
Zhang, Y. et al. Telemental Health Services Usage and Association with Health Care Utilization and Expenditures Among Vulnerable Medicare Beneficiaries in 2019: A Comparative Study Using Propensity Score Matching. Telemed. e-Health 30, 1848–1856 (2024).
Li, K. Y. et al. Association between primary care practice telehealth use and acute care visits for ambulatory care–sensitive conditions during COVID-19. JAMA Netw. Open 5, e225484–e225484 (2022).
Nakamoto, C. H., Cutler, D. M., Beaulieu, N. D., Uscher-Pines, L. & Mehrotra, A. The Impact Of Telemedicine On Medicare Utilization, Spending, And Quality, 2019–22: Study examines the impact of telemedicine use on spending, quality, and outcomes. Health Aff. 43, 691–700 (2024).
Saharkhiz, M. et al. Telehealth Expansion and Medicare Beneficiaries’ Care Quality and Access. JAMA Netw. Open 7, e2411006–e2411006 (2024).
Liu, T. et al. Primary Care Practice Telehealth Use and Low-Value Care Services. JAMA Netw. Open 7, e2445436–e2445436 (2024).
Zhang, Y. et al. Tele-mental health utilization trends with rural–urban disparities in Mississippi: 2020–2023. J. Rural Ment Health 48, 219–229 (2024).
Cossman, R. E. et al. Access to primary care physicians differs by health insurance coverage in Mississippi. Obstetrics/Gynecology 91, 0 (2014).
Dixit, R. A., et al. The impact of expanded telehealth availability on primary care utilization. npj Digital Med. 5, 141 (2022).
Dhaliwal, J. K. et al. Expansion of telehealth in primary care during the COVID-19 pandemic: benefits and barriers. J. Am. Assoc. Nurse Pr. 34, 224–229 (2021).
Hernán, M. A., Brumback, B. & Robins, J. M. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology 11, 561–570 (2000).
Austin, P. C. & Stuart, E. A. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat. Med 34, 3661–3679 (2015).
Tilhou, A. S., Jain, A. & DeLeire, T. Telehealth Expansion, Internet Speed, and Primary Care Access Before and During COVID-19. JAMA Netw. Open 7, e2347686–e2347686 (2024).
Rocovich, C. & Patel, T. Emergency department visits: Why adults choose the emergency room over a primary care physician visit during regular office hours?. World J. Emerg. Med. 3, 91–97 (2012).
Vogel, J. A. et al. Reasons Patients Choose the Emergency Department over Primary Care: a Qualitative Metasynthesis. J. Gen. Intern. Med. 34, 2610–2619 (2019).
Hill, R., et al. Are patients who call a primary care office referred to the emergency department by non-healthcare personnel without the input of a physician? PeerJ 4, e1507 (2016).
Hanjani, L. S., Caffery, L. J., Freeman, C. R., Peeters, G. & Peel, N. M. A scoping review of the use and impact of telehealth medication reviews. Res. Soc. Adm. Pharm. 16, 1140–1153 (2020).
Flood, D., et al. Integrating hypertension and diabetes management in primary health care settings: HEARTS as a tool. Rev. Panam. Salud Publica 46, e150 (2022).
Zaman Huri, H. & Fun Wee, H. Drug related problems in type 2 diabetes patients with hypertension: a cross-sectional retrospective study. BMC Endocr. Disord. 13, 2 (2013).
Bates, T., Connaughton, V. & Watts, G. Non-adherence to statin therapy: a major challenge for preventive cardiology. Expert Opin. Pharmacother. 10, 2973–2985 (2009).
Barthold, D., Li, J. & Basu, A. Patient Out-of-Pocket Costs for Type 2 Diabetes Medications When Aging Into Medicare. JAMA Netw. Open 7, e2420724–e2420724 (2024).
Berenson, R. A. & Skopec, L. How Preventable Hospitalizations Became A Widely Used But Flawed Quality Measure. Health Aff. Forefr. https://doi.org/10.1377/forefront.20240531.688339 (2024).
Zhang, Y. et al. Framework for Evaluating and Developing Sustainable Telehealth Programs. Telemed. J. E Health 29, 1421–1425 (2023).
Berwick, D. M., Nolan, T. W. & Whittington, J. The triple aim: care, health, and cost. Health Aff. 27, 759–769 (2008).
Acknowledgements
This work is being funded by the Office for the Advancement of Telehealth (OAT), Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services (HHS) under cooperative agreement award no. 2 U66RH31459-04-00. The funder played no role in study design, data collection, analysis and interpretation of data, or the writing of this manuscript. We sincerely thank Dr. Thomas R. Belin for his insightful discussions on causal inference techniques employed in this work.
Author information
Authors and Affiliations
Contributions
Y.Z. conducted the analysis and prepared the initial draft. All authors contributed to the conceptualization and investigation of the study, and reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
L.S.L. is an employee of Immunovant, Inc. Other authors (Y.Z., S.C., and J.M.S.) declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Y., Lal, L.S., Chandra, S. et al. Primary care telehealth in a dynamic healthcare environment from digital divide to healthcare outcomes. npj Digit. Med. 8, 211 (2025). https://doi.org/10.1038/s41746-025-01599-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41746-025-01599-x
This article is cited by
-
Community nurses’ experiences with digital sensory interventions in remote primary care: a qualitative descriptive study of trust, privacy, and family dynamics
BMC Nursing (2025)
-
Association of telehealth use with endocrine therapy adherence, metastasis incidence and healthcare costs in breast cancer: A claims-based cohort study
Journal of Cancer Survivorship (2025)