Abstract
Telehealth has been promoted as a solution to spatial healthcare access barriers, yet its role in addressing cancer care disparities remains uncertain, particularly in the context of digital divides in broadband availability and affordability. This study assessed spatial and telehealth accessibility to cancer care across 33,499 ZIP Code Tabulation Areas (ZCTA) in the United States using the two-step floating catchment area (2SFCA) and two-step virtual catchment area (2SVCA) methods, respectively. Incorporating physician locations, cancer incidence, travel time based on transportation networks, and broadband coverage and subscription rates, we found that accessibility declined from urban to rural areas and was lower in ZCTA with greater socioeconomic deprivation. Areas with higher proportions of Black and Hispanic populations showed modestly higher access scores, yet a three-way interaction among rurality, deprivation, and racial ethnic composition revealed compounded disadvantages. Telehealth reduced but did not eliminate these gaps, highlighting how its reliance on digital infrastructure may both alleviate and intensify disparities in cancer care access.
Similar content being viewed by others
Introduction
Equity in healthcare delivery remains a critical concern of public health policy1. The disparity in healthcare accessibility, driven by uneven distributions of healthcare resources and populations and the networks connecting them, presents a particular challenge for cancer services, where specialist care and ongoing treatment are critical2. Recent technological advances have promoted telehealth as a potential solution to overcome geographic barriers and improve healthcare access, particularly for underserved populations3,4.
In the United States, only about 3% of oncologists practice in rural areas, and as of 2020, approximately two-thirds of rural counties lacked an oncologist, affecting nearly 32 million residents (about 10% of the U.S. population)5. An estimated 28% to 36% of cancer patients experience travel times over one hour for receiving treatments such as chemotherapy or radiation therapy6. These barriers contribute to late-stage diagnoses and higher mortality in rural areas7. Disparities also vary by cancer type; for example, nearly a quarter of adolescents and young adults with acute lymphoblastic leukemia must travel over an hour to access a specialty center8. To address these gaps, telehealth has become an increasingly important tool in cancer care. Wherein, patients can receive consultations, follow-up, and supportive care remotely5. It facilitates multidisciplinary coordination, virtual tumor boards, and even clinical trial participation across geographic boundaries9. The COVID-19 pandemic catalyzed this transition, with telehealth rising from near 0% to over 10% of outpatient visits by 202110,11, especially among younger and urban patients. Studies during this period found high satisfaction among both patients and providers in cancer care, and systematic reviews confirm that remote follow-up care is comparable in safety and effectiveness to in-person visits12.
However, telehealth’s effectiveness in reducing disparities remains unclear. During the COVID-19 pandemic, telehealth expanded rapidly out of necessity, yet emerging evidence suggests it may exacerbate existing inequities13,14,15,16,17,18,19. The digital divide creates new barriers through both infrastructure availability and affordability challenges20,21. Roughly 22% of rural Americans lack high-speed internet, compared to 1.5% in urban areas10. Low-income and rural populations also face limited digital literacy and access to devices. Certain populations—including racial-ethnic minorities, elderly individuals, low-income groups, and rural residents—may face compounded disadvantages in telehealth access22,23. Without targeted efforts to close these digital gaps, telehealth may widen rather than reduce disparities.
The relationship between spatial and telehealth accessibility is complex. While telehealth may expand service reach, it often operates within existing healthcare networks and may inherit traditional access barriers24. Moreover, virtual visits rarely fully replace physical consultations, especially for cancer care, where both remote monitoring and in-person treatment are essential25,26,27. Structural barriers such as state licensing, reimbursement policies, and the need for in-person procedures (e.g., surgery, infusions, imaging) also limit the extent to which telehealth can replace traditional care. Thus, telehealth should be viewed as rather a complement than a substitute for physical healthcare infrastructure28,29.
Previous studies have documented disparities in spatial healthcare access but have not comprehensively examined how telehealth might alter these patterns30. Understanding these relationships is crucial as healthcare systems increasingly integrate virtual services. This study addresses that gap by comparing spatial and telehealth accessibility to cancer care across all U.S. ZIP Code Tabulation Areas (ZCTAs). For clarity, we define telehealth accessibility in this study as a virtual accessibility measure that builds upon traditional spatial accessibility by incorporating constraints for broadband availability and affordability. This measure does not capture actual telehealth utilization, but rather reflects the infrastructure-and-financially enabled potential for engaging in virtual care. Accordingly, throughout the manuscript, we refer to this as “virtual accessibility” or “potential virtual accessibility”, emphasizing its basis in spatial catchments and digital connectivity. We evaluate each area’s access to in-person oncology services and telehealth-enabling infrastructure, while accounting for geographic and sociodemographic variations. Our aim is to assess whether telehealth complements traditional care access, and to identify which populations or regions benefit most or least from virtual care. In doing so, we provide national insight into whether telehealth is helping bridge the spatial accessibility divide in cancer care or whether additional efforts are needed to improve equity.
Results
Figure 1 summarizes the study design of measuring spatial and virtual (telehealth) accessibility for cancer care in the United States by incorporating supply, demand, travel time, and internet availability and affordability factors.
This flowchart summarizes the integration of multiple data sources and methods to compute ZCTA–level spatial and virtual accessibility. Abbreviations used in the figure are defined as: ZCTA ZIP Code Tabulation Area, NPI National Provider Identifier, FCC Federal Communications Commission, OSRM Open Source Routing Machine, DHC Detailed Housing Characteristics, NCI National Cancer Institute, ACS American Community Survey, ADI Area Deprivation Index, FTE Full-Time Equivalent, 2SFCA Two-Step Floating Catchment Area, 2SVCA Two-Step Virtual Catchment Area. Figure generated using PowerPoint.
Gaps between spatial and virtual accessibility
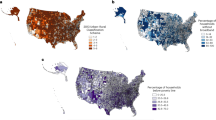
The spatial patterns of spatial accessibility (SA) and virtual accessibility (VA) exhibit strong consistency within with a Pearson correlation coefficient of 0.93. Figure 2A shows the variation of SA across ZIP code areas in the U.S., and Fig. 2B depicts the difference between SA and VA, i.e., As-v = SA–VA, with cold colors representing areas with improved virtual over spatial accessibility and warm colors indicating the opposite.
A Telehealth accessibility (Av) by the 2SVCA method (number of physicians per 1000 cancer incidents), B Difference between spatial and telehealth accessibility (As-v), C Population ratio with As-v < 0 across states in urban areas (UA), low-density areas (LD), rural areas (RA) and statewide average across all ZCTAs (All). The connecting lines are included to illustrate within-state variation across categories. Map generated using ArcGIS Pro 3.3.
Aggregating As-v to the state level reveals the variability across states. Figure 2C illustrates the proportion of the population for whom VA exceeds SA (As-v < 0), i.e., the extent to which virtual access outpaces spatial access. In Delaware, Utah, New Jersey, Illinois, Michigan, and Virginia, 61–72% of the total population experiences better virtual than spatial accessibility. Supplementary Fig. S1 breaks down how this portion also varies by rurality across the states. Overall, the highest percentage of urban population enjoys better virtual than spatial accessibility, then low-density (generally suburban) population, and the least in rural residents. However, in Connecticut, Rhode Island, and Illinois, more than half of the rural population (64–75%) does benefit from improved virtual accessibility over spatial accessibility. The finding suggests that telehealth services are more likely to improve urban and suburban residents for their cancer care accessibility than rural residents. In other words, rural areas need more help for targeted interventions to bridge the digital divide in cancer care access.
To further assess spatial clustering in accessibility, we conducted a Local Moran’s I analysis on both spatial accessibility scores and the difference between spatial and virtual accessibility (Fig. 3). Panel A highlights clusters of high-high (HH) and low-low (LL) spatial accessibility, with substantial LL clustering observed in rural areas of the Southeast and Midwest. Panel B presents clusters based on the difference between spatial and virtual accessibility scores (As-v), where HH areas indicate locations where virtual accessibility lags behind spatial accessibility, and LL areas reflect locations where virtual accessibility exceeds spatial access. The most prominent HH clusters appear in the Deep South and the Central Appalachia. Several Low-High (LH) outliers are also notable, including parts of Louisiana and eastern Texas, the corridor from eastern Washington through northern Idaho into western Montana, and areas near West Virginia, such as parts of Pennsylvania, Ohio, and North Carolina. Additional LH clustering is visible in southeastern New Mexico. In contrast, Low-Low (LL) clusters, where virtual accessibility significantly outperforms spatial accessibility, are primarily found in the Northeast, particularly in Massachusetts and New York, as well as in the Northern Plains region, including North and South Dakota. These complex spatial patterns suggest that disparities in potential telehealth access versus in-person accessibility are not only regionally concentrated but also heterogeneous in form, highlighting pockets of strong digital infrastructure amid broader virtual access deficits. This reinforces the need to develop geographically tailored telehealth interventions that consider local infrastructure, affordability, and demographic demand.
A Local spatial clusters of 2SFCA scores and B clusters of differences between spatial and virtual accessibility (As–v). HH High–High cluster, LL Low–Low cluster, LH Low–High outlier, HL High–Low outlier, N not statistically significant. These clusters reveal geographic concentrations of access advantages or disadvantages. Map generated using ArcGIS Pro 3.3.
Accessibility Differences by Demographic Groups and Geographic Areas
As summarized in Table 1, national averages of 2SFCA and 2SVCA values are similar (15.16/15.02), but display substantial variations across population subgroups. Average accessibility scores are the highest in Asian (19.22/19.46), followed by Black (17.06/16.35), Hispanic (16.04/15.58), White (14.12/14.17), and American Indian populations (9.78/9.22). On average, Asian and White populations have higher virtual than spatial accessibility, while other racial groups show the inverse pattern. The strength of these disparities varies significantly by geographic and socioeconomic contexts. American Indian communities face particularly challenging circumstances, with their low accessibility scores correlating strongly with high Area Deprivation Index (ADI) values and limited 5G coverage. This pattern suggests compound disadvantages where technological and socioeconomic barriers reinforce each other.
Accessibility consistently declines from urban to low-density and then rural (urban: 18.98/18.87; low-density: 14.19/14.62; rural: 9.30/8.91, P < 0.001), so does increasing ADI as accessibility scores in areas of least deprivation (20.04/20.37) nearly double in most deprived areas (10.26/8.92, P < 0.001). More importantly, the disadvantage gaps between spatial and virtual access widen towards more rural or higher ADI areas (Fig. 4A, D). These patterns directly correspond to telecommunications infrastructure (less coverage in rural) and subscription (lower rate in areas of higher ADI), and their intersection in telehealth delivery may reinforce existing cancer care access disparities.
Population-weighted mean spatial and virtual accessibility scores (SA, VA) are displayed across dimensions of A Rurality (UA urban area, LD low density, RA rural area), B Black proportion, C Hispanic proportion, D ADI, E ADI and Black proportion, F ADI and Hispanic proportion, G Rurality and Black proportion, H Rurality and Hispanic proportion, and I Rurality and ADI. Difference (As-v = SA-VA) is illustrated by shaded bands: shaded areas above the primary line indicate spatial accessibility is greater than virtual (SA > VA), while areas below indicate virtual accessibility advantage (VA > SA). Figure generated using Python with Matplotlib.
Areas with higher Black population percentages show increasing accessibility scores but widening gaps between spatial and virtual accessibility (Fig. 4B). One-way ANOVA validates the observation, showing positive but modest effects of Black population concentration in Table 2 (2SFCA: 0.138, 2SVCA: 0.106, P < 0.001). It is an outcome of countervailing trends in telecommunications infrastructure, where declining internet affordability coexists with improving 5G coverage in areas of higher Black concentrations. Higher concentrations of Hispanic population generally correspond to increasing accessibility scores with a minor dip towards the highest percentages (Fig. 4C). Areas with higher percentage Hispanic generally correspond to stable internet affordability and increasing 5G coverage, resulting in more consistency between the two accessibility scores (2SFCA: 0.124, 2SVCA: 0.120, P < 0.001). Any of other racial-ethnic groups accounts for less than 6.5% population (Census, 2020)31 and is not examined in more depth.
Interaction Effects
Analysis of two-way interactions reveals nuanced relationships between demographic composition (i.e., racial-ethnic minority concentrations) and structural factors (such as ADI and rurality). The positive correlation between Black population concentration and accessibility remains evident across the full range of ADI, and both accessibility scores decrease with rising ADI (Fig. 4E). While the trend of declining accessibility with higher ADI remains consistent across various Hispanic concentrations, the downward slope tends to flatten in areas of higher Hispanic ratios (Fig. 4F). As a result, there is less clarity on the correlation between Hispanic concentration level and accessibility scores. As shown in Table 2, after controlling for interaction effects, the positive effect of higher Hispanic concentration on spatial accessibility is no longer significant (p = 0.051), and its effect on telehealth accessibility is even reversed to negative.
While accessibility decreases from urban toward rural areas, it demonstrates distinct patterns when interacting with racial-ethnic concentration levels or ADI. Figure 4G indicates that higher Black proportions correlate with better overall accessibility in urban areas, to a less degree in low-density areas, but reversely with lower accessibility in rural; and the gaps between spatial and virtual accessibility enlarge with increasing Black concentration across all three categories of rurality. The opposite correlation between Black concentration and accessibility in urban and rural areas is further supported by the negative and highly significant term of “Rurality: Black” (2SFCA: −0.045, 2SVCA: −0.046, P < 0.001) in the 3-way ANOVA in Table 2. This highlights the double disadvantages (i.e., poorer spatial and telehealth accessibility) experienced in rural areas with higher concentrations of Black population28. Similarly, as shown in Fig. 4H, the relationship between Hispanic proportion and accessibility varies by rurality. It is largely flat in urban areas but turns negative in suburban and rural areas. Once again in Fig. 4I, the accessibility scores decline with rising ADI across all areas of rurality, and the gap between spatial and virtual access is most pronounced in urban areas with the highest ADI, attributable to low broadband affordability there.
Additional complex intersection effects are revealed in Table 2 by the three-way ANOVA. Overall, the effects on both accessibilities are strongest by rurality (−0.302/−0.315), then ADI (−0.245/−0.249), and last by Black (0.107/0.065) or Hispanic proportion. Rurality-ADI-Black interaction produces a small negative effect (−0.017) for spatial accessibility but becomes non-significant for virtual accessibility (P = 0.204). The three-way interaction among ADI, Black population concentration, and rurality in spatial accessibility (SA) leads to the most severe declines in accessibility in impoverished rural areas with high Black population concentration, with “triple constraints” (Supplementary Fig. S2). In contrast, the absence of a significant three-way interaction in virtual accessibility (VA), likely attributable to the “de-geographical” nature of telehealth. When rural areas have high-quality internet, VA remains relatively stable even in areas where SA is low. Conversely, when rural internet quality is poor, VA declines, but this decline does not appear to be exacerbated by high Black concentration or economic disadvantage. This suggests that even in communities with a lower proportion of Black residents (Black−) or in more affluent areas (ADI−), VA remains low when internet quality is poor, meanwhile areas with higher concentrations of Black residents may experience constrained virtual access due to limited infrastructure coverage and economic affordability.
In the 3-way ANOVA of rurality, ADI, and Hispanic proportions, both rurality (−0.357/−0.359) and poverty (−0.214/−0.229)also significantly reduce accessibility, but the pathways differ from those observed in interaction with Black concentration levels. In affluent areas (ADI−), SA disparities between Hispanic-majority rural and urban communities widen, a trend also seen in VA. Even in wealthier regions, rural Hispanic communities continue to face challenges related to insufficient internet infrastructure and limited telehealth service availability. This pattern differs from that seen among Black concentrated affluent areas, which do not exhibit the same VA decline, possibly due to greater access to targeted telehealth initiatives or community-based healthcare resources. In economically disadvantaged regions (ADI+), VA disparities between rural and urban Hispanic-majority communities are more pronounced. Moreover, while Hispanic-majority communities do not show a significant SA decline, they exhibit a more pronounced drop in VA, indicating that telehealth accessibility is more constrained than physical healthcare access. This may suggest that while these communities do not necessarily experience structural deficiencies in physical healthcare infrastructure, they face more significant barriers related to digital connectivity.
Discussion
The nationwide analysis of telehealth accessibility for cancer services reveals significant differences across geographic and socio-demographic dimensions. The results suggest that telehealth may potentially exacerbate existing access gaps without targeted interventions.
The disparities are particularly pronounced in three dimensions. First, the urban-rural divide shows the strongest effect on both spatial and virtual accessibility32. Rural areas consistently demonstrate lower accessibility, with telehealth showing even greater disparities than spatial access. Secondly, the ADI reveals a clear gradient in accessibility, with the most deprived areas showing markedly lower scores, particularly in virtual accessibility33,34. Thirdly, areas with higher Black and Hispanic concentrations show better spatial accessibility but face challenges in maintaining this advantage in telehealth access20.
Several factors contribute to these disparities. Our analysis of broadband infrastructure shows that rural areas face significant challenges in both availability and affordability of quality internet services. Even in areas with adequate infrastructure, low subscription rates suggest affordability remains a significant barrier. The situation is particularly concerning in areas with high ADI, where both spatial and virtual accessibility scores are lowest. Telehealth has not universally improved healthcare access and, in some cases, may exacerbate inequities due to economic and infrastructure barriers. These disparities are most pronounced among Black and Hispanic populations. The loss of spatial accessibility advantages in minority-concentrated areas during the transition to telehealth suggests the need for targeted interventions in these areas.
The study has several limitations. First, our analysis of accessibility is location-oriented and thus relies on area-based rather than individual-level data, which may mask within-area variations. Secondly, the assumption that telehealth services operate within spatial catchment areas may not hold as telehealth evolves. Thirdly, we focus on technical availability rather than quality of telehealth services. Fourthly, our measures of internet connectivity may not capture all aspects of digital access barriers. Finally, our ZIP Code-level cancer incidence estimates, used as demand data, were derived from county-level sources using validated interpolation and simulation methods35. While overall accuracy is high, we acknowledge that some uncertainty in cancer case estimates may remain in sparsely populated areas. We also recognize that cancer care delivery varies by cancer type and treatment modality. While our study provides an aggregate-level analysis, future work should explore cancer-type-specific spatial and telehealth access patterns to reflect more nuanced care needs.
In short, the transition to telehealth presents both opportunities and challenges for promoting healthcare equity. Without targeted interventions addressing both infrastructure and affordability barriers, telehealth may paradoxically widen rather than narrow healthcare access gaps. Future policies should focus on expanding broadband infrastructure in rural areas while simultaneously addressing affordability challenges in socioeconomically disadvantaged and minority-concentrated areas.
To assess the robustness of our findings, we experimented with Median Family Income (MFI) or Median Household Income (MHI) in place of ADI. As shown in Supplementary Tables S1, S2, and S3, all three indicators showed similar directional effects across racial and ethnic groups. Models using ADI produced slightly higher R² values for both spatial and virtual accessibility. MFI and MHI also generated consistent patterns and can serve as alternative socioeconomic indicators in related analyses. In three-way ANOVA models, certain interaction effects, such as the combination of rurality, deprivation, and Black population concentration were no longer statistically significant when ADI was replaced with MFI or MHI. These findings indicate that while ADI provided marginally stronger explanatory power in this analysis, income-based indicators may also be appropriate depending on the research context.
Methods
2SFCA and 2SVCA Methods
The Two-Step Floating Catchment Area (2SFCA) method measures spatial accessibility (SA) at demand location i:
where Sj represents cancer service capacity defined as the full-time equivalent (FTE) count of cancer physicians (including hematology, medical oncology, and radiation oncology specialists) at supply location j, Dk is number of cancer cases at ZCTA k, and dkj denotes travel time between them. The first step calculates an initial ratio of supply capacity Sj to the total demand ∑Dk from m locations within a catchment range (\({d}_{{kj}}\le {d}_{0}\)) around the supply location j as a measure of its availability. The second step sums up those initial ratios for supply locations j of n locations within a catchment range (\({d}_{{ij}}\le {d}_{0}\)) around a demand location i to measure its spatial accessibility (SAi). In essence, SA is a series of supply-to-demand ratios, each of which reflects the proportion of available supply allocated to nearby demand within a catchment area. Its value may read as “number of physicians per 1000 cancer cases”2.
Telehealth rarely works completely independently of physical visits to healthcare providers, and rather as supplementary consultation to reduce travel burdens for patients36. Although it reduces the need for in-person travel, telehealth typically operates within local provider catchments. Therefore, virtual service takes effect within each provider’s spatial catchment area as conceptualized in the 2SFCA. The Two-Step Virtual Catchment Area (2SVCA) method builds upon the 2SFCA to measure telehealth or virtual accessibility (VA):
where f(bj) and f(bk) reflect broadband availabilities (including fixed and wireless broadband such as 5G) at supply and demand locations, respectively; and ai (ak) and aj represent broadband subscription rates for demand and supply locations, respectively. In other words, only demand and supply locations with broadband coverage are possible to participate in telehealth, and furthermore, only those portions of residents or service providers with broadband subscriptions can engage in it. The affordability variable ensures that underserved populations are not omitted but proportionally represented in the accessibility scores. Specifically, the final scores are discounted by ai to reflect the overall community’s effective access to telehealth services, including those without subscriptions. Two new constraints, broadband availability f and affordability a are added into the 2SVCA formulation, and other variables remain the same as the 2SFCA28,29.
VA scores are also interpreted as the number of physicians per 1000 cancer cases, as it is built directly upon the spatial constraint structure of the 2SFCA and differs only in that it discounts the effective supply and demand values based on internet availability and affordability. As a result, its core structure remains a supply-to-demand ratio, with interpretation units consistent across both models. This structural consistency enables direct comparison between spatial and virtual accessibility outcomes. Both 2SFCA and 2SVCA methods used 60 min as threshold d0 (catchment area range) to calculate accessibility scores, consistent with prior research showing that this threshold captures approximately 70% of Medicare cancer care travel times6. Sensitivity analysis comparing 45- and 60-minute thresholds indicated consistent spatial patterns and trends.
Physicians and cancer incidences data
The supply-side analysis began with the National Provider Identifier Registry’s 8,523,268 records. Through systematic filtering using specialized taxonomy codes (Hematology & Oncology, Medical Oncology, and Radiation Oncology), we identified 25,461 cancer service providers. We developed a full-time equivalent (FTE) allocation algorithm accounting for physicians with multiple (x) service locations, assigning 1/x FTE to each location. This conservative and parsimonious approach reflects the absence of detailed scheduling data and helps avoid over-representation of multi-site providers in location-based accessibility estimates. This process yielded 31,484 provider records distributed across 9967 unique locations, defining S in Eqs. 1–2.
Cancer case estimation followed a hierarchical geographic framework integrating multiple authoritative data sources. At the national level, we combined the National Cancer Institute’s (NCI) State Cancer Profiles (2016–2020) with detailed demographic data from Detailed Housing Characteristics population data. This study used aggregated cancer incidence estimates across all types. The 2016–2020 period was chosen as it corresponds to the most recent and complete dataset available for cancer incidence reporting across the U.S. State-level processing employed multi-constraint Monte Carlo simulation techniques to address suppressed values, generating complete incidence estimates stratified by age (<50, 50–65, 65+), sex (male, female), and racial/ethnic groups (Non-Hispanic White, Non-Hispanic Black, Non-Hispanic American Indian and Alaska Native, Non-Hispanic Asian and Pacific Islander, Hispanic, Other). Subsequently, we implemented county-level downscaling incorporating local cancer registries and population characteristics. Missing county data underwent Monte Carlo simulation with geographic constraints, ensuring spatial consistency of estimates. The final ZCTA-level estimates emerged from a combination of cross-county population interpolation and Monte Carlo-based geo-imputation. This methodology achieved 92.3% accuracy in validation against known cancer statistics, providing reliable small-area estimates of cancer incidence37. The demand data included 33,499 ZCTAs with interpolated 2016–2020 cancer counts, defining D in Eqs. 1–235.
Travel cost and internet data
Travel accessibility measurement began with comprehensive distance calculations between all provider-ZCTA pairs nationwide. We implemented a 60-mile threshold to identify potential service areas while maintaining computational efficiency. For qualifying pairs, we calculated precise travel times using the Open Source Routing Machine (OSRM) node in Geospatial Analytics extension for KNIME38,39, incorporating real-world road networks and typical travel conditions. This process generated 3,408,974 valid origin-destination pairs, defining dij in Eqs. 1, 2. All travel times were measured between population-weighted centroids of ZCTAs to better approximate residential location patterns.
Our evaluation of virtual (telehealth) accessibility incorporated both infrastructure availability and economic affordability dimensions (Fig. 5). The availability analysis processed the FCC Fixed Broadband Data across six major technologies, including cable, copper, fiber to the premises, licensed fixed wireless, unlicensed fixed wireless, and LBR wireless. These data covered both residential and business services, and population-weighted averages of service quality were calculated at the ZCTA level. Additionally, we integrated 5G network coverage data, determining population-weighted coverage rates for mobile broadband access. Each ZCTA received composite availability scores reflecting both fixed and mobile broadband options, i.e., parameter f(b) for internet availability in Eqs. 1, 2. A location was considered to have sufficient broadband if either fixed broadband ( ≥100 Mbps download, ≥20 Mbps upload) or 5G coverage ( ≥80% population coverage) was available. Internet affordability, i.e., parameter a in Eqs. 1, 2, was measured by household broadband subscription rates from the American Community Survey (2020). These rates serve as a practical proxy for affordability due to their availability at the ZCTA level and their relevance to actual internet adoption. However, we acknowledge that this measure does not fully reflect the complexity of financial barriers, such as pricing burdens, device costs, or broader digital access inequities.
A various types of fixed broadband availability, B availability for fixed broadband, C. 5G-NR coverage, D mobile availability based on 5G-NR, E internet availability integrating fixed broadband and mobile, and F broadband affordability. In B and D, each ZCTA is assigned a binary value based on broadband availability: 1 for at least one criterion (either fixed broadband ≥100/20 Mbps in A or 5G coverage ≥80% in C), 0 for not meeting either criterion. Map generated using ArcGIS Pro 3.3.
Geographic and demographic data
Human behavior including health care utilization varies across distinctive physical and social environments. A long tradition in public health studies focuses on the effect of urbanicity (or rurality) on health behavior and outcome40. It is especially relevant for the study as telehealth infrastructure and access varies across areas of various levels of urbanicity. While scholars and government entities debate over specific definitions of urbanicity41, most favor more categories across the continuum over a rural-versus-urban dichotomous definition42. This study utilized the 2020 Census housing density thresholds defined in Urban Area Criteria by U.S. Census Bureau43, defining urban (≥425 units/mile²), low-density (200–424 units/mile²), and rural (<200 units/mile²) areas. These categories serve as the basis for ‘rurality’ gradient. While the definition is inherently related to population density, it reflects broader structural and infrastructural disparities across the urban–suburban–rural continuum. The Area Deprivation Index (ADI) underwent population-weighted calculation at the block group level to provide neighborhood-level socioeconomic context. ADI captures multi-dimensional deprivation—including income, education, housing quality, and employment—and is widely used in health geography and public health research as a more comprehensive contextual measure than single-variable metrics such as median household income (MHI) or median family income (MFI)44,45. Racial and ethnic population distributions employed natural breaks classification to maintain meaningful group distinctions while avoiding artificial categorization (Fig. 6).
A Cancer service providers (points), B cancer counts at the ZCTA level, C ADI index, D rurality (RA urban area, LD low density area, RA rural area), and E Black and F Hispanic population portions based on natural breaks. C shows decile ranks of the Area Deprivation Index (ADI); for example, ‘5–6’ denotes ZCTAs in the 5th to 6th decile range. D uses the following classification: RA Rural Area, LD Low Density, UA Urban Area. E, F display accessibility scores using sequential color bands; value ranges can be inferred by adjacent threshold intervals. Map generated using ArcGIS Pro 3.3.
Statistical analysis
Accessibility scores were standardized to FTE cancer service providers per 1000 cancer cases. We first conducted population-weighted analyses to examine accessibility variations across geographic and demographic dimensions. One-way ANOVA was used to assess individual effects of rurality, Area Deprivation Index, and racial/ethnic composition, while three-way ANOVA examined their interactions. This multivariate approach is commonly used in public health research to evaluate intersectional effects across population groups and place-based indicators. For statistical significance, P < 0.001 was used given multiple comparisons. Detailed ANOVA assumptions, diagnostics, and sensitivity analyses are provided in the Supplementary Materials.
Data availability
The data underlying this article are available in Harvard Dataverse under the title Telehealth Infrastructure for Cancer Care in the United States: https://doi.org/10.7910/DVN/OIFW0D.
Code availability
The code used to process and analyze the datasets is available from the corresponding author upon reasonable request.
References
Administration, H. R. S. Medically Underserved Areas and Populations (MUA/Ps). https://bhw.hrsa.gov/shortage-designation/muap (2021).
Wang, F. Measurement, optimization, and impact of health care accessibility: a methodological review. Ann. Assoc. Am. Geogr. 102, 1104–1112 (2012).
Kruse, C. S. et al. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open 7, e016242 (2017).
Moffatt, J. J. & Eley, D. S. The reported benefits of telehealth for rural Australians. Aust. Health Rev. 34, 276–281 (2010).
Moscovice, I. S. et al. Availability of cancer care services and the organization of care delivery at critical access hospitals. Cancer Med. 12, 17322–17330 (2023).
Onega, T. et al. The interaction of rurality and rare cancers for travel time to cancer care. J. Rural Health 39, 426–433 (2023).
Charlton, M., Schlichting, J., Chioreso, C., Ward, M. & Vikas, P. Challenges of rural cancer care in the United States. Oncology 29, 633–640 (2015).
Parsons, H. M. et al. Travel-time barriers to specialized cancer care for adolescents and young adults with acute lymphoblastic leukemia. JNCI Cancer Spectr. 8, pkae046 (2024).
Lopez, A. M. Telehealth in cancer care: inequities, barriers, and opportunities. Cancer J. 30, 2–7 (2024).
(FCC), F. C. C. 2020 Broadband Deployment Report, https://www.fcc.gov/reports-research/reports/broadband-progress-reports/2020-broadband-deployment-report (2021).
Pritchett, J. C. et al. Patient-and provider-level factors associated with telehealth utilization across a multisite, multiregional cancer practice from 2019 to 2021. JCO Oncol. Pract. 19, 750–758 (2023).
Xiao, K., Yeung, J. C. & Bolger, J. C. The safety and acceptability of using telehealth for follow-up of patients following cancer surgery: a systematic review. Eur. J. Surg. Oncol. 49, 9–15 (2023).
Gajarawala, S. N. & Pelkowski, J. N. Telehealth Benefits and Barriers. J. Nurse Pract.17, 218–221 (2021).
An, M. H., You, S. C., Park, R. W. & Lee, S. Using an extended technology acceptance model to understand the factors influencing telehealth utilization after flattening the COVID-19 Curve in South Korea: Cross-sectional Survey Study. JMIR Med. Inf. 9, e25435 (2021).
Wosik, J. et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 27, 957–962 (2020).
Snoswell, C. L. et al. Determining if telehealth can reduce health system costs: scoping review. J. Med. Internet Res. 22, e17298 (2020).
Shachar, C., Engel, J. & Elwyn, G. Implications for telehealth in a postpandemic future: regulatory and privacy issues. JAMA 323, 2375–2376 (2020).
Monaghesh, E. & Hajizadeh, A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 20, 1193 (2020).
Koonin, L. M. et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic - United States, January-March 2020. Mmwr. Morbidi. Mortal. Wkly. Rep. 69, 1595–1599 (2020).
Cortelyou-Ward, K. et al. Navigating the digital divide: barriers to telehealth in rural areas. J. Health Care Poor Underserved 31, 1546–1556 (2020).
Lythreatis, S., Singh, S. K. & El-Kassar, A.-N. The digital divide: A review and future research agenda. Technol. Forecast. Soc. Change 175, 121359. https://doi.org/10.1016/j.techfore.2021.121359 (2022).
Campos-Castillo, C. & Anthony, D. Racial and ethnic differences in self-reported telehealth use during the COVID-19 pandemic: a secondary analysis of a US survey of internet users from late March. J. Am. Med. Inform. Assoc. 28, 119–125 (2021).
Chuo, J., Macy, M. L. & Lorch, S. A. Strategies for evaluating telehealth. Pediatrics 146, https://doi.org/10.1542/peds.2020-1781 (2020).
Tuckson, R. V., Edmunds, M. & Hodgkins, M. L. Telehealth. N. Engl. J. Med. 377, 1585–1592 (2017).
Dorsey, E. R. & Topol, E. J. State of Telehealth. N. Engl. J. Med. 375, 154–161 (2016).
Kaplan, B. Access, equity, and neutral space: telehealth beyond the pandemic. Ann. Fam. Med. 19, 75 (2021).
Moen, E. L. et al. Cross-state travel for cancer care and implications for telehealth reciprocity. JAMA Netw. Open 8, https://doi.org/10.1001/jamanetworkopen.2024.61021 (2025).
Wang, F., Zeng, Y., Liu, L. & Onega, T. Disparities in spatial accessibility of primary care in Louisiana: From physical to virtual accessibility. Front. Public Health 11, 1154574. https://doi.org/10.3389/fpubh.2023.1154574 (2023).
Liu, L., Alford-Teaster, J., Onega, T. & Wang, F. Refining 2SVCA method for measuring telehealth accessibility of primary care physicians in Baton Rouge, Louisiana. Cities 138, 104364. https://doi.org/10.1016/j.cities.2023.104364 (2023).
Skinner, H. J. et al. Comparison of care accessibility, costs, and quality with face-to-face and telehealth epilepsy clinic visits. Epilepsy Behav. 127, 108510. https://doi.org/10.1016/j.yebeh.2021.108510 (2022).
Bureau, U. S. C. QuickFacts of United States, https://www.census.gov/quickfacts/fact/table/US/PST045223 (2025).
Gagnon, M.-P., Duplantie, J., Fortin, J.-P. & Landry, R. Implementing telehealth to support medical practice in rural/remote regions: what are the conditions for success?. Implement. Sci. 1, 18 (2006).
Hirko, K. A. et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J. Am. Med. Inform. Assoc. : JAMIA 27, 1816–1818 (2020).
Blandford, A., Wesson, J., Amalberti, R., AlHazme, R. & Allwihan, R. Opportunities and challenges for telehealth within, and beyond, a pandemic. Lancet Glob. Health 8, e1364–e1365 (2020).
Liu, L. Wang, F. & Onega, T. Cancer incidence data at the ZCTA Level in the U.S. interpolated by multi-constraint Monte Carlo simulation. Sci. Data (2025).
Sorensen, M. J., Bessen, S., Danford, J., Fleischer, C. & Wong, S. L. Telemedicine for surgical consultations–pandemic response or here to stay?: a report of public perceptions. Ann. Surg. 272, e174–e180 (2020).
Liu, L., Cowan, L., Wang, F. & Onega, T. A multi-constraint Monte Carlo Simulation approach to downscaling cancer data. Health & Place 91, 103411, https://doi.org/10.1016/j.healthplace.2024.103411 (2025).
Liu, L. et al. Geospatial Analytics Extension for KNIME. SoftX. 25, 101627. https://doi.org/10.1016/j.softx.2023.101627 (2024).
Luxen, D. & Vetter, C. in Proceedings of the 19th ACM SIGSPATIAL International Conference on Advances in Geographic Information Systems 513–516 (Association for Computing Machinery, Chicago, Illinois, 2011).
Wang, F. Why public health needs GIS: a methodological overview. Ann. GIS 26, 1–12 (2020).
Levit, L. A. et al. Closing the rural cancer care gap: three institutional approaches. JCO Oncol. Pract. 16, 422–430 (2020).
Hall, S. A., Kaufman, J. S. & Ricketts, T. C. Defining urban and rural areas in US epidemiologic studies. J. Urban Health 83, 162–175 (2006).
Bureau, C. Urban Area Criteria for the 2020 Census-Final Criteria, https://www.federalregister.gov/documents/2022/03/24/2022-06180/urban-area-criteria-for-the-2020-census-final-criteria (2022).
Kind, A. J. & Buckingham, W. R. Making neighborhood-disadvantage metrics accessible—the neighborhood atlas. N. Engl. J. Med. 378, 2456 (2018).
Health, U. o. W. S. o. M. a. P. 2022 Area Deprivation Index v2.0, https://www.neighborhoodatlas.medicine.wisc.edu/ (2025).
Acknowledgements
The research is funded by the National Cancer Institute (NCI) under Grant No. R01CA267990-01 (Onega and Wang as MPIs), and partially supported by the National Science Foundation (NSF) grant #1841403 (Liu). Points of view or opinions in this article are those of the authors and do not necessarily represent the official position or policies of the NCI or the NSF.
Author information
Authors and Affiliations
Contributions
L.L., T.O. and F.W. conceived the study. L.L. and F.W. developed the methodology, performed the analyses, and drafted the manuscript. T.O. contributed to methodological refinement and manuscript review. E.L.M., A.N.A.T., R.E.S., Q.W. and L.C. contributed to the development of methods and provided critical revisions. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, L., Onega, T., Moen, E.L. et al. Digital divides in telehealth accessibility for cancer care in the United States. npj Digit. Med. 8, 534 (2025). https://doi.org/10.1038/s41746-025-01931-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41746-025-01931-5