Abstract
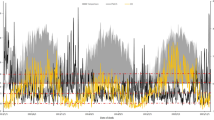
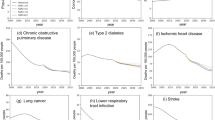
The harmful impact of fine particulate matter (PM2.5) air pollution on public health remains a pressing concern. Detrimental effects of such pollution on elderly populations can be exacerbated by the ageing process, making it necessary to identify vulnerable groups or regions, especially in the context of shifting demographics and healthcare disparities. Focusing on Japan, with its extreme ageing demographic, our study assesses the health impacts of PM2.5 across different age segments from a spatial–temporal perspective while considering the uneven distribution of medical resources across different regions. We find that the Baby Boomer generation, born in the 1950s, faces a statistical value of life that is approximately 52% higher than that of other generations, signifying that individuals of this generation are more likely to bear increased costs for health issues caused by long-term exposure to PM2.5. On the basis of 170,000 medical-clinic records across Japan, our research reveals that the disease burden exacerbated by mismatches in medical resources has become increasingly evident, affecting over 86% of the areas we studied, with remote regions in West Japan being particularly vulnerable. These findings highlight the amplified challenges posed by demographic shifts, the need for targeted health and environmental policies, and serve as a critical warning for regions facing similar issues.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
PM2.5 concentration data are publicly available on the website of the Atmospheric Composition Analysis Group of Washington University in St Louis51 (https://sites.wustl.edu/acag/). Population data are maintained by Li and Managi52. We obtained the age structure data and household asset data from the Statistics Bureau of Japan (https://www.stat.go.jp/english/). GDP data are available from the Japan Cabinet Office (https://www.cao.go.jp/index-e.html). Baseline mortality, life expectancy and survival probability data are also open access and can be obtained from the Global Burden of Disease Study 201953 (https://ghdx.healthdata.org/gbd-2019). Medical-clinic records data are developed by the Geospatial Information Authority of Japan, Ministry of Land, Infrastructure, Transport and Tourism, and are available from https://nlftp.mlit.go.jp/. Source data are provided with this paper.
Code availability
The code used to process and analyse the data is developed in Python 3.7, and is available from the corresponding authors upon reasonable request.
References
Bloom, D. E. & Luca, D. L. in Handbook of the Economics of Population Aging, Vol. 1A (eds Piggott, J. & Woodland, A.) 3–56 (North-Holland, 2016).
World Population Prospects 2022: Summary of Results UN DESA/POP/2022/TR/NO. 3 (United Nations, 2022).
Jarzebski, M. P. et al. Ageing and population shrinking: implications for sustainability in the urban century. npj Urban Sustain. 1, 17 (2021).
Hutton, D. Older People in Emergencies: Considerations for Action and Policy Development (World Health Organization, 2008).
World Population Ageing 2020 Highlights: Living Arrangements of Older Persons ST/ESA/SER.A/451 (United Nations, 2021).
Shrestha, L. B. Population aging in developing countries: the elderly populations of developing countries are now growing more rapidly than those in industrialized nations, thanks to health advances and declining fertility rates. Health Aff. 19, 204–212 (2000).
Higo, M. & Khan, H. T. Global population aging: unequal distribution of risks in later life between developed and developing countries. Glob. Soc. Policy 15, 146–166 (2014).
Lloyd-Sherlock, P. Population ageing in developed and developing regions: implications for health policy. Soc. Sci. Med. 51, 887–895 (2000).
Chand, M. & Tung, R. L. The aging of the world’s population and its effects on global business. Acad. Manag. Perspect. 28, 409–429 (2014).
Xu, F. et al. The challenge of population aging for mitigating deaths from PM2.5 air pollution in China. Nat. Commun. 14, 5222 (2023).
Thangavel, P., Park, D. & Lee, Y.-C. Recent insights into particulate matter (PM2.5)-mediated toxicity in humans: an overview. Int. J. Environ. Res. Public Health 19, 7511 (2022).
Wang, B. et al. The impact of long-term PM2.5 exposure on specific causes of death: exposure–response curves and effect modification among 53 million U.S. Medicare beneficiaries. Environ. Health 19, 20 (2020).
Feng, S., Gao, D., Liao, F., Zhou, F. & Wang, X. The health effects of ambient PM2.5 and potential mechanisms. Ecotoxicol. Environ. Saf. 128, 67–74 (2016).
Yin, H. et al. Population ageing and deaths attributable to ambient PM2.5 pollution: a global analysis of economic cost. Lancet Planet. Health 5, e356–e367 (2021).
Liu, J. et al. Transition in air pollution, disease burden and health cost in China: a comparative study of long-term and short-term exposure. Environ. Pollut. 277, 116770 (2021).
Pope, C. 3rd Epidemiology of fine particulate air pollution and human health: biologic mechanisms and who’s at risk? Environ. Health Perspect. 108, 713–723 (2000).
Bloom, D. E. et al. Macroeconomic implications of population ageing and selected policy responses. Lancet 385, 649–657 (2015).
World Economic and Social Survey 2007: Development in an Ageing World (United Nations, 2007).
Masereka, E. M. et al. in Health Insurance Across Worldwide Health Systems (ed. Tavares, A. I.) Ch. 3 (IntechOpen, 2024); https://doi.org/10.5772/intechopen.1003279
Du, X., Du, Y., Zhang, Y., Zhu, Y. & Yang, Y. Urban and rural disparities in general hospital accessibility within a Chinese metropolis. Sci. Rep. 14, 23359 (2024).
Health at a Glance 2023: OECD Indicators (OECD Publishing, 2023)
Yan, D. et al. The effect of fine particulate matter (PM2.5) pollution on health inequality: an intergenerational perspective. Environ. Geochem. Health 46, 195 (2024).
Fingerman, K. L., Pillemer, K. A., Silverstein, M. & Suitor, J. J. The Baby Boomers’ intergenerational relationships. Gerontologist 52, 199–209 (2012).
Mudrazija, S. & Butrica, B. A. How does debt shape health outcomes for older Americans? Soc. Sci. Med. 329, 116010 (2023).
Knickman, J. R. & Snell, E. K. The 2030 problem: caring for aging Baby Boomers. Health Serv. Res. 37, 849–884 (2002).
Cooper, M. A burden on future generations? How we learned to hate deficits and blame the baby boomers. Sociol. Rev. 69, 743–758 (2021).
Tynkkynen, L.-K. et al. Health system reforms and the needs of the ageing population—an analysis of recent policy paths and reform trends in Finland and Sweden. Eur. J. Ageing 19, 221–232 (2022).
Yin, H., McDuffie, E. E., Martin, R. V. & Brauer, M. Global health costs of ambient PM2.5 from combustion sources: a modelling study supporting air pollution control strategies. Lancet Planet. Health 8, e476–e488 (2024).
Feng, Y. et al. Long-term exposure to ambient PM2.5, particulate constituents and hospital admissions from non-respiratory infection. Nat. Commun. 15, 1518 (2024).
Liao, L., Du, M. & Chen, Z. Air pollution, health care use and medical costs: evidence from China. Energy Econ. 95, 105132 (2021).
Yang, J. & Zhang, B. Air pollution and healthcare expenditure: implication for the benefit of air pollution control in China. Environ. Int. 120, 443–455 (2018).
Chen, F. & Chen, Z. Cost of economic growth: air pollution and health expenditure. Sci. Total Environ. 755, 142543 (2021).
McCurry, J. Japan will be model for future super-ageing societies. Lancet 386, 1523 (2015).
Burnett, R. et al. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc. Natl Acad. Sci. USA 115, 9592–9597 (2018).
Plackett, B. Tackling the crisis of care for older people: lessons from India and Japan. Nature 601, S12–S14 (2022).
Employment Status Survey 2022 (Statistics Bureau of Japan, 2023); https://www.stat.go.jp/english/data/shugyou/index.html
Clark, R., Ogawa, N., Lee, S.-H. & Matsukura, R. Older workers and national productivity in Japan. Popul. Dev. Rev. 34, 257–274 (2008).
Christophers, B. Intergenerational inequality? Labour, capital, and housing through the ages. Antipode 50, 101–121 (2018).
Minami, U. et al. Effects of the change in working status on the health of older people in Japan. PLoS ONE 10, e0144069 (2015).
Statistics on foreign residents (formerly known as registered foreigners). Immigration Services Agency of Japan https://www.moj.go.jp/isa/policies/statistics/toukei_ichiran_touroku.html (2023).
Dilley, L., Gkartzios, M. & Odagiri, T. Developing counterurbanisation: making sense of rural mobility and governance in Japan. Habitat Int. 125, 102595 (2022).
Medical Care Act No. 79 (Ministry of Justice of Japan, 2018)
Batalova, J. Immigrant Health-Care Workers in the United States (Migration Policy Institute, 2023).
Kamo, H. Care worker shortage and the regional characteristics of foreign candidate acceptance for certified care workers in Japan. Ann. Assoc. Econ. Geogr. 65, 280–294 (2019).
Japan is looking for Specified Skilled Workers! Ministry of Foreign Affairs of Japan https://www.mofa.go.jp/mofaj/ca/fna/ssw/us/ (2023).
Otomo, R. Healthcare, language and a free-trade agreement: institutional logics of on-the-job Japanese language training for migrant healthcare workers. Multilingua 39, 343–367 (2020).
Hirano, Y. O., Tsubota, K. & Ohno, S. Factors associated with the recruitment of foreign nurses in Japan: a nationwide study of hospitals. Hum. Resour. Health 18, 88 (2020).
Regarding the Number of Foreign Residents as of the End of June 2020 (Immigration Services Agency of Japan, 2023).
Eitner, C., Enste, P., Naegele, G. & Leve, V. in The Silver Market Phenomenon: Marketing and Innovation in the Aging Society (eds. Kohlbacher, F. & Herstatt, C.) 309–324 (Springer, 2011).
The Silver Economy: Final Report (European Union, 2018).
van Donkelaar, A. et al. Monthly global estimates of fine particulate matter and their uncertainty. Environ. Sci. Technol. 55, 15287–15300 (2021).
Li, C. & Managi, S. Gridded datasets for Japan: total, male, and female populations from 2001–2020. Sci. Data 10, 81 (2023).
Global Burden of Disease Study 2019 (GBD 2019) Results (Institute for Health Metrics and Evaluation, 2020); https://ghdx.healthdata.org/gbd-2019
Guan, C., Wu, S., Xu, W. & Zhang, J. Global, regional, and national burden of ischaemic heart disease and its trends, 1990–2019. Public Health 223, 57–66 (2023).
Marelli, A. J., Mackie, A. S., Ionescu-Ittu, R., Rahme, E. & Pilote, L. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation 115, 163–172 (2007).
The Economic Consequences of Outdoor Air Pollution (OECD, 2016).
Narain, U. & Sall, C. Methodology for Valuing The Health Impacts Of Air Pollution: Discussion of Challenges and Proposed Solutions (World Bank Group, 2016).
World Bank & Institute for Health Metrics and Evaluation. The Cost of Air Pollution: Strengthening the Economic Case for Action (World Bank Group, 2016).
Acknowledgements
We thank for Z. Chen (University of Tokyo, Tokyo, Japan) for his help and insightful comments regarding the figures of the paper. This research is also funded by Japan Society for the Promotion of Science KAKENHI B (grant number JP24K03146, Y.Y.) and KAKENHI C (grant number JP23K11542, L.Y.).
Author information
Authors and Affiliations
Contributions
X.X. and Y.L. conceptualized the research question and designed the analytical framework. X.X. and L.H. conducted the data collection, preprocessing, modelling and statistical analyses. Visualizations were created by X.X. and Y.L. The paper was draughted by X.X. and L.H., and it was critically reviewed and revised by Y.L., Y.Y. and L.Y. All authors discussed the results and edited the final paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Sustainability thanks Pin Wang and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–25, Methods, Tables 1–8 and ref. 1.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, X., Huang, L., Yao, L. et al. Rising socio-economic costs of PM2.5 pollution and medical service mismatching. Nat Sustain 8, 265–275 (2025). https://doi.org/10.1038/s41893-025-01509-9
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41893-025-01509-9
This article is cited by
-
Climate adaptation and resilience must account for context and culture
Nature Health (2026)
-
Advances in particulate matter filtration via output-oriented triboelectric nanogenerators: from energy harvesting to system integration
Advanced Composites and Hybrid Materials (2025)