Abstract
Burn induces a systemic response affecting multiple organs, including the liver. Since the liver plays a critical role in metabolic, inflammatory, and immune events, a patient with impaired liver often exhibits poor outcomes. The mortality rate after burns in the elderly population is higher than in any other age group, and studies show that the liver of aged animals is more susceptible to injury after burns. Understanding the aged-specific liver response to burns is fundamental to improving health care. Furthermore, no liver-specific therapy exists to treat burn-induced liver damage highlighting a critical gap in burn injury therapeutics. In this study, we analyzed transcriptomics and metabolomics data from the liver of young and aged mice to identify mechanistic pathways and in-silico predict therapeutic targets to prevent or reverse burn-induced liver damage. Our study highlights pathway interactions and master regulators that underlie the differential liver response to burn injury in young and aged animals.
Similar content being viewed by others
Introduction
Over 450,000 people are affected by burn injuries yearly, resulting in 40,000 hospital admissions in the United States alone1. Although there have been significant advances in burn injury therapeutics, burns are still a leading cause of morbidity and mortality worldwide2. Burns extend beyond the skin, inflicting damage on distant organs and exacerbating the already poor outcomes in burn victims, particularly when multiple organs experience failure3. Thus, deepening our understanding of how different organs respond to burns can help identify targets to direct organ-specific treatments and improve the outcomes of burn patients.
The liver is among the critical organs affected after burns, displaying significant morphological alterations, such as hepatomegaly and fatty infiltration4. Compared to controls, liver weight increases significantly 2 to 7 days post-burn in rodents5. Burn-induced liver damage (BILD) is associated with edema formation and at the same time may lead to cell damage and the release of hepatic enzymes5. Liver enzymes, such as aspartate aminotransferase (AST) and alanine aminotransferase (ALT), are sensitive indicators of hepatocyte injury6. Clinical evidence reveals that serum AST and ALT peaked during the first week post-burn7. Because the liver orchestrates metabolic functions, inflammatory processes, and immune events during basal and stress conditions, a burn patient with an impaired liver is more vulnerable to metabolic and infectious complications leading to unfavorable outcomes than one with a healthy liver4. Gong et al. studied the mortality risk of burn patients finding that the survival rates were significantly lower in burn patients with elevated liver transaminases than in those with normal values8. Liver damage after burns has been associated with multifactorial events; hypoperfusion, proinflammatory cytokines, cell death signaling, edema, fatty changes, and mitochondrial dysfunction5. However, BILD pathophysiology is not entirely understood, highlighting a critical gap in burn injury knowledge.
Using a clinically relevant murine burn injury model, our laboratory and others demonstrated that the liver exhibits molecular and histological changes following cutaneous burns9,10,11. Also, we showed that these alterations were exacerbated in aged animals, as noted by elevated liver injury markers, increased lipid deposits, heightened oxidative stress, and accentuated histological evidence of hepatic damage10. These observations highlight changes in the liver of burn-aged animals that indicate increased susceptibility of this organ to acute stressors.
Comprehensive genetic and metabolic studies can help elucidate the nature of the differences in liver response to burns between young and aged individuals. While transcriptomics determines the functional response to burn injury and helps predict its master regulators, metabolomics provides a downstream and closer to phenotype description of the biological processes that occur in the liver12,13. Here, we deepened the study of hepatic parenchymal cellular interaction by analyzing transcriptomics and metabolomics in the liver of mice after burn injury.
Additionally, we employed an in silico analysis of the databases obtained from the transcriptomics and metabolomics to predict drugs that might prevent or treat the liver pathology observed in mice after burn injury.
Results
Overview of the unsupervised analysis among the experimental groups
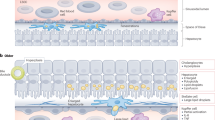
Four groups of liver samples from the young sham, young burn, aged sham, and aged burn groups were collected 24 h after the burn injury. This time point was selected based on previous animal experiments showing systemic differences, specifically in the liver, between young and aged mice after burn10,14. Transcriptional analysis was performed by RNA-seq and targeted metabolomics with mass spectrometry (Fig. 1a). The samples maintained an adequate group separation observed in unsupervised analysis by principal component analysis of transcriptomic data (Fig. 1b). The first component identified and separated the sham and burn treatments (PC1 = 60.8%). The second component separated young and aged groups (PC2 = 14.3%).
a Experimental mice model. b PCA (Principal Component Analysis) overview of sample clustering. c Volcano plot showing differential liver gene expression between aged and young mice in sham conditions (without burn). d KEGG pathway overrepresentation analysis of genes up-regulated in aged mice. N = 3 per group.
Hepatic transcriptomics in young and aged sham animals
At first, we focused on characterizing the differences between aged and young sham groups, finding that 75 genes were up-regulated (log2FC > 1 and adj. p value < 0.05) in aged compared to young mice (Fig. 1c). Among those, 13 genes were related to immunoglobulin production, including Igkv8-19, Ighm, Igkc, Igkj5, and Igkj1 (Supplementary Data 4). In overrepresentation analysis, the genes up-regulated in aged mice were associated with two pathways, “PPAR signaling” (Pck1, Angptl4, Plin5, Cyp4a32, Cyp4a14) and “IL-17 signaling” (Cebpb, S100a9, Nfkbia, S100a8, Cxcl1) (Fig. 1d, Supplementary Data 7). There were only 20 down-regulated genes (log2FC < −1 and adj. p value < 0.05) compared to the aged vs. young mice after sham treatment. No pathway was statistically over-represented among down-regulated genes (Supplementary Data 8).
Hepatic transcriptomics, shared response to burn injury by young and aged mice
Furthermore, we identified a common hepatic transcriptomic profile of burn-injury response in both young and aged animals. We identified genes responding to burn stimulus from the differential expression analysis in young (Fig. 2a) and aged (Fig. 2b) groups and selected the ones shared between the age groups. In the up-regulated genes after burn injury, 157 genes overlapped between young and aged groups (Fig. 2c). Those genes were associated within the 11 KEGG pathways like “protein processing in the endoplasmic reticulum” (30 genes, e.g., Derl3, Hyou1, Pdia3, Pdia4, Pdia6), “protein export’ (8 genes identified, e.g., Hspa5, Sec61a1, Sec61b, Sec61g, Spcs2),” fructose and mannose metabolism” (5 genes: Tkfc, Gmppb, Gmppa, Pfkfb1, Akr1b7) and “IL-17 signaling” (6 genes: Lcn2, Hsp90b1, Cxcl1, Hsp90aa1, S100a9, S100a8) (Fig. 2e, Supplementary Data 5). In the down-regulated genes, there were 114 genes that overlapped in both young and aged groups (Fig. 2d). These down-regulated genes were significantly overrepresented in 18 KEGG pathways, including “chemical carcinogenesis – DNA adducts” (18 genes, e.g., Sult2a3, Gsta4, Cyp3a25, Ugt2b1, Gsta3), “steroid hormone biosynthesis” (13 genes, e.g., Akr1d1, Hsd17b6, Ugt2a3, Cyp2c38, Cyp2c37) and “metabolism of xenobiotics by cytochrome P450” (12 genes, e.g., Gsta2, Cyp1a2, Sult2a8, Cyp2f2, Sult2a1) (Fig. 2f, Supplementary Data 6).
a Volcano plot showing genes responding to burn stimuli in young mice. b Volcano plot showing genes responding to burn stimuli in aged mice. c Venn diagram showing overlap of genes with up-regulated expression by burn stimuli in both aged and young mice. d Venn diagram showing overlap of genes with down-regulated expression by burn stimuli in both aged and young mice. e Sankey diagram of KEGG pathway from overrepresentation analysis based on overlapping up-regulated genes (panel C). f Sankey diagram of KEGG pathway from overrepresentation analysis based on overlapping down-regulated genes (panel D). g Volcano plot showing differential liver gene expression between aged and young mice after burn stimuli. h KEGG pathway overrepresentation analysis of genes down-regulated in aged burn mice vs young burn mice. For panels e, f and h, only pathways meeting the following criteria were shown. Size term < 200, intersection > 3, Benjamini–Hochberg adj. p-value < 0.05. N = 3 per group.
Hepatic transcriptomics, differences in response to burn injury by young and aged mice
After burn, there were 46 up-regulated genes and 89 downregulated genes in the livers of aged mice compared to their younger counterparts (Fig. 2g). No pathway was significantly overrepresented among the up-regulated genes (Supplementary Data 9). However, among down-regulated genes, we found eleven overrepresented pathways, including: “chemical carcinogenesis” (11 genes, e.g., Gsta3, Gsta4, Sult1a1, Cyp2c54, Cyp2c38),” steroid hormone biosynthesis” (10 genes, e.g., Akr1d1, Hsd3b3, Cyp2c40, Cyp2b10, Cyp2c29), “bile secretion” (8 genes, e.g., Abcb11, Nr0b2, Hmgcr, Atp1b1, Sult2a5), metabolism of linoleic acid, arachidonic acid and retinol metabolism (5 common genes - Cyp2c54, Cyp2c38, Cyp2c40, Cyp2c29, Cyp2c50), “arginine biosynthesis” (Gpt, Gls2, Ass1), and” metabolism of xenobiotics by cytochrome P450” (Cyp2f2, Gsta3, Gsta4, Sult2a5, Sult2a8) (Fig. 2h, Supplementary Data 10). We observed that the abovementioned pathways included many elements of the cytochrome P450 Cyp2 family (Cyp2c54, Cyp2c38, Cyp2c40, Cyp2c29, Cyp2c50, Cyp2f2, Cyp2b10, Cyp2a1) and glutathione metabolism genes (Gsta3, Gsta4).
Transcriptomics validation by qPCR and by functional studies of cytochrome P450
As Cyp2c genes are associated with multiple essential liver functions, from drug metabolism to inflammatory mediators’ production15, we decided to validate those changes and evaluate their dynamics at 4-time points after burn injury. From the differentially expressed genes in Fig. 2, we selected representatives of the cytochrome P450 Cyp2c family, namely Cyp2c29, Cyp2c38, Cyp2c40, and Cyp2c54. We measured their expression in the 4 study groups at 4 different time points – 6 h, 9 h, 12 h, and 24 h after burn injury (Supplemental Fig. 1). We confirmed the downregulation of their expression at the 24 h time point after burn in both age groups. The transcriptomics validation of multiple P450 cytochrome genes in a time course study confirms that the downregulation is initially mild and becomes more severe as time progresses postburn (Supplementary Fig. 1).
Common metabolomic response to burn injury in young and aged mice
Cytochrome P450 genes are closely associated with many metabolic pathways16. Thus, we analyzed liver samples’ metabolite in young and aged mice. Metabolomic profiling of liver samples indicated that mice, irrespective of age, responded to burn injury by lowering their levels of many amino acids, including valine, methionine, tyrosine, phenylalanine, and leucine as well as cis-p-coumarate and protein 5-hydroxylysine. We also observed increased levels of glucosamine, UMP (uridine monophosphate), UDP-glucose (uridine diphosphate glucose), thymidine, putrescine, and N-acetylneuraminate (Fig. 3a, Supplementary Data 11).
a A heatmap of differentially expressed metabolites in both aged burn versus aged sham and young burn mice versus young sham ones (p < 0.05 for each comparison). The blue cluster shows metabolites with a lower level in aged burn mice, and the red cluster shows metabolites with a higher level in aged burn mice. b Network of differentially expressed genes and metabolites in both young and aged mice after burn injury (only nodes having any connections were shown). c Upstream regulators of metabolic and transcriptomic changes after the burn injury are common for both aged and young mice. Only experimentally proven data for hepatocytes and/or liver was used for the prediction. d A heatmap of differentially expressed metabolites between aged burn and young burn mice (p < 0.05). In network, red and green colors mark up- and down-regulated nodes found in either metabolomic or transcriptomic data. N = 5 per group.
Next, we connected the observed dysregulated metabolites with previously selected commonly differentially expressed genes in both aged and young mice after burn injury (Fig. 2). In our network analysis, we looked for a connection between two datasets via the Ingenuity Pathway Analysis tool. The created network showed many associations between differentially expressed metabolites and genes that were commonly dysregulated by burn injury in both aged and young mice (Fig. 3b). Interestingly, Egfr (epidermal growth factor receptor), a membrane receptor, was found to be highly associated with many disturbed metabolites suggesting its crucial role in the development of post-injury metabolomic disturbances17,18. Additionally, we looked for upstream regulators of all commonly observed changes in metabolites and genes (Fig. 3c). We found 9 upstream regulators predicted to be activated. Among them, we found two kinases: Eif2ak3 (Eukaryotic Translation Initiation Factor 2 Alpha Kinase 3), Ern1 (Endoplasmic Reticulum to Nucleus Signaling 1); two transcription regulators: Atf6 (Activating Transcription Factor 6), Stat5b (Signal Transducer And Activator Of Transcription 5B); two enzymes associated with glutathione metabolism: Txnrd1 (Thioredoxin Reductase 1), Gsr (Glutathione-Disulfide Reductase); two cytokines: IL1b, IL6, and one hypoxia-inducible gene: S100a4 (S100 calcium binding protein A4). Inhibition of six upstream regulators was also predicted: two transcription regulators: Zbtb20 (Zinc Finger and BTB Domain Containing 20), Ncoa2 (Nuclear Receptor Coactivator 2); one transporter (Atp7b - ATPase Copper Transporting Beta), one cytokine - visfatin (Nampt), one growth factor - leptin (Lep), and one ligand-dependent nuclear receptor (Ahr - Aryl Hydrocarbon Receptor). The molecular targets of those master regulators found to be dysregulated in our transcriptomic data are shown in Supplementary Data 12. Interestingly, inhibition of Zbtb20 could be responsible for observed Cyp2 downregulation (by targeting molecules like Cyp1a2, Cyp2c54, Cyp2c8, Cyp2f1) and inhibition of leptin (by targeting: Cyp2c54, Cyp2c8, Cyp2f1, Cyp7a1)19.
Metabolomic differences in response to burn injury between young and aged mice
Having looked at common metabolomic changes after burn injury in both aged and young mice, next, we also looked for the differences. Firstly, we found that among some of the commonly burn-dysregulated metabolites, three had more pronounced changes in aged mice, including deeper downregulation of phenylalanine and methionine levels and higher up-regulation of UMP levels in aged vs. young mice (Fig. 3d). Additional disturbances, not present in young mice, were identified in aged burn mice, and included: downregulation of phosphate, S-adenosyl-L-homocysteine, L-proline, glutathione disulfide and 9(10)-EpOME (epoxyoctadecenoic acid); and up-regulation of guanosine, ADP (adenosine diphosphate), ethanolamine phosphate, acyl-C6-DC (methylglutarylcarnitine) and ectione.
In silico drug predictions
Finally, we searched for drugs that could modify the liver burn injury response. Thus, we performed an in silico analysis of drugs that could cause similar or opposite effects to the transcriptomic differences observed in burn response among aged and young mice. To do so, we used the Connectivity map tool - Cmap. Providing the list of commonly dysregulated genes from Fig. 2, we predicted which drugs could cause a similar effect to burn injury (Fig. 4a right panel). The predicted drug list included commonly used drugs like albendazole, dextromethorphan, and valsartan. Assuming that observed expression changes after burn injury are harmful, the abovementioned drugs could exacerbate them. We also looked at drugs that have opposite expression effects. We found widely used drugs like enalapril, atorvastatin, and cilostazol. Those drugs could cause the opposite transcriptional effect, potentially reversing transcriptomic changes observed in mice liver after burn injury (Fig. 4a left panel).
a Predictions of drugs able to cause similar (right panel, red columns) or reverse effect (left panel, blue columns) in HepG2 cell line as common transcriptional changes observed after burn injury in the liver in both aged and young mice. b Predictions of drugs performed for the transcriptional difference observed after burn injury between aged and young mice. Only drugs with HepG2 tau score > |95| are shown.
Additionally, we searched for drugs able to cause similar and opposite expression changes to those observed between aged burn vs. young burn mice (Fig. 4b). Among drugs causing similar transcriptional effects to the one observed in aged vs. young mice after burn injury; we found such commonly used drugs as etomidate, probenecid, flumetazone and nadolol (Fig. 4b – right panel). Among drugs with opposite expressional effect to the one observed in aged burn mice (compared to young burn individuals) were clinically relevant drugs such as melperone, clozapine, dexamethasone, and sertraline (Fig. 4b – left panel).
Discussion
Burns are a significant cause of morbidity and mortality worldwide, with an estimated 11 million cases yearly and more than 300,000 fatalities20. Burns affect seemingly every age group2. However, the mortality rate is significantly higher in elderly burn patients21. Regardless of age, severe burns cause damage to multiple organs distant from the original burn wound, leading to severe clinical problems such as multiple organ dysfunction syndrome (MODS)3. The liver is particularly affected after burn injury exhibiting hepatomegaly and fatty infiltration5. BILD is characterized by edema and cellular damage leading to leakage of hepatic enzymes AST and ALT into the circulation4. Clinical studies have demonstrated that the mortality in burn victims is elevated in patients with persistently elevated AST and ALT8. Advanced age is associated with cellular derangements in the liver22. Several age-related hepatic changes include a decline in liver volume, an increase in the hepatic dense body compartment (lipofuscin), a reduction in drug metabolism, and diminished hepatobiliary functions21,22,23. Based on these correlations, it is not unreasonable to suggest that elderly patients are more susceptible to liver damage after suffering burns. With its metabolic, inflammatory, and immune functions, the liver is fundamental for patient survival and recovery following burn injury4. Therefore, it is logical to study the liver and attempt to elucidate modifiable factors that specific targeted interventions could improve the outcomes of burn victims.
We evaluated the liver omics at a base level, comparing young and aged sham animals. In this study, the transcriptomics analysis has demonstrated that while the livers from aged sham animals exhibit higher immunoglobulin gene expression and increased activity of IL-17 signaling pathways, they do not present significant downregulation of genes or signaling pathways compared to the livers of younger counterparts. These results match common age-related findings contributing to the characteristic chronic inflammatory state of aged individuals known as inflammaging24.
Following a significant trauma such as a burn, the liver physiology drastically redirects its protein synthesis favoring the production of acute phase reactants5. As the liver becomes hyper-functional in producing these essential proteins to survive a burn insult, it reduces the production of constitutional proteins, steroid hormones, bile, and numerous cytochrome p450 metabolic processes4,25. As such, in this study, the transcriptomics analysis showed that after burn, the foremost up-regulated pathways in the livers of young and aged mice involved protein processing in the endoplasmic reticulum, protein export, fructose, and mannose metabolism, and IL-17 signaling. The major hepatic pathways downregulated after a burn in young and aged mice were chemical carcinogenesis, steroid hormone biosynthesis, and metabolism of xenobiotics by cytochrome P450.
Additionally, our data demonstrate that after burn, the livers of aged differently from younger mice profoundly downregulate processes such as steroid hormone biosynthesis, bile secretion, linoleic acid, arachidonic acid, and retinol metabolism, arginine biosynthesis, and metabolism of xenobiotics by cytochrome P450. While prioritization of acute phase proteins benefits survival rate at an initial phase post-injury, a severe and prolonged downregulation of other hepatic functions, such as cytochrome metabolism, may be detrimental for burn victims, especially in the elderly26. There is a lack of understanding about the impact of these processes on the outcomes in young and aged burn victims, which can be an important focus of future research.
Particularly distinctive was the downregulation of cytochrome P450 Cyp2 family genes involved in multiple liver functions, including protein and lipid metabolism, oxidative stress buffers, and metabolism of drugs and toxins27. These differences can result in a toxin metabolism shift in the liver cells and destabilization of free radical scavenging and DNA replication, recombination, and repair processes in aged animals after burn injury28,29. The cytochrome P450 system may also be affected by inflammation and age30. Two cytochrome P450 enzyme families, Cyp2c and Cyp2j, are responsible for metabolizing proinflammatory metabolites (arachidonic acid) to anti-inflammatory compounds (epoxyeicosatrienoic acids)31. In the data presented herein, all 11 members of the Cyp2c family identified in our liver samples (Cyp2c54, Cyp2c38, Cyp2c40, Cyp2c29, Cyp2c50, Cyp2c68, Cyp2c70, Cyp2c39, Cyp2c67, Cyp2c37, Cyp2c69) and one detected CYP2J member - Cyp2j5 - were found to be downregulated among liver of aged burn mice compared to the young burn mice.
Clinical evidence reveals that older patients have an attenuated inflammatory response to burn injury relative to younger injured subjects, followed by a hyper-inflammatory reaction21. Microsomal oxidation deceleration driven by cytochrome P450 was shown to play a critical role in developing MODS due partly to the accumulation of endogenous toxic compounds27. MODS was found to have increased incidence in the elderly after burn injury, but this was not accompanied by increased infection or sepsis rate21. Moreover, decreased cytochrome P450 Cyp2c activity could accumulate toxic metabolites from burn treatment medications as these cytochrome family members are mainly involved with drug metabolism32. Those observations suggest that inhibiting cytochrome P450 Cyp2 as a component of the hepatic post-burn inflammatory response may have detrimental effects and that increased expression of those enzymes could have a potentially beneficial effect. However, further studies need to establish whether the downregulation of Cyp2c after burn injury is responsible for less favorable clinical outcomes.
Given that the cytochrome p450 system is abundant in the liver playing the role of numerous functions33, we validated our transcriptomics findings by measuring the gene expression of central genes that operate in this system in 2 different mice strains (Balb/c and C57BL/6). In a time-course study, the transcriptomics validation of multiple P450 cytochrome genes demonstrates that the downregulation becomes more severe as time advances postburn. These findings raise a red flag in treating burn patients, indicating that drug metabolism may be severely affected in the first weeks after burns.
The metabolomic analysis exhibited a common and a different hepatic response pattern to burns between young and aged animals. The common response showed a decrease in amino acid levels, including valine, methionine, tyrosine, phenylalanine, leucine, cis-p-coumarate, and protein 5-hydroxylysine. Most of these metabolites are essential amino acids, and their decrease is commonly associated with a lack of nutritional intake34. Postburn metabolism not only consumes essential amino acids but also decreases appetite, which can result in an essential amino acid deficiency35. Liver injury can cause a decrease in several catabolic pathways resulting in the accumulation of several metabolites36. In the liver of mice postburn, we observed an increased level of glucosamine, UMP (uridine monophosphate), UDP-glucose (uridine diphosphate glucose), thymidine, putrescine, and N-acetylneuraminic, indicating that energy and proliferation catabolic pathways are affected in this pathology (Fig. 4a, Supplementary Data 11).
We used an Ingenuity Pathway Analysis tool to further evaluate the common hepatic response to burns to create a network connecting the metabolomic and transcriptomics changes among the four study groups. The network showed many connections between differentially expressed metabolites and genes that were commonly dysregulated by burn injury in both aged and young mice (Fig. 3b). Egfr was found to be highly associated with many disturbed metabolites suggesting its crucial role in the development of post-injury metabolomic disturbances. EGFR is pivotal in hepatocyte proliferation, liver regeneration, liver steatosis, oxidative stress, mitochondria dysfunction, and cell death in different animal models of liver injury18. EGFR activation is achieved ligand-based or ligand-independent, and the latter is mainly associated with liver injury. Given EGFR’s diverse involvement at many levels in hepatic pathophysiological processes, additional research is necessary to determine if EGFR may be used as a therapeutic target to treat liver disorders, including burn induce liver damage17. The IPA analysis of the common hepatic response to burn yield 6 deactivated master regulators: Zbtb20, Ncoa2, Atp7b, visfatin (Nampt), leptin (Lep), and Aryl Hydrocarbon Receptor (Ahr). Interestingly, inhibition of Zbtb20 could be responsible for observed Cyp2 downregulation (by targeting molecules like Cyp1a2, Cyp2c54, Cyp2c8, Cyp2f1) and inhibition of leptin (by targeting: Cyp2c54, Cyp2c8, Cyp2f1, Cyp7a1)19.
The significant differences in metabolic pathways noticed in the livers of young burn and aged burn mice involved a severe downregulation of glutathione metabolism and citrate cycle (TCA cycle) in the aged animal group. These metabolomics results match our previous findings that highlight the presence of a disrupted antioxidant glutathione system in the liver of aged animals, which can lead to increased susceptibility to hepatic damage following burns10.
In silico (computer-based) drug prediction and repurposing have become one of the most used methods to make drug discovery more accurate and economical37. This method seeks to recognize the relationship network between the target and the drug, which is attained through bioinformatics tools and public databases38. In this study, we used a Connectivity map tool – Cmap, to obtain drugs that can induce opposite and similar transcriptomics and metabolomics changes in hepatocytes as the ones caused by burn injury in our experiments. We hypothesize that harnessing side targets of clinically used drugs might help reprogram liver cells to handle better the stress of responding to a burn injury.
Some predicted drugs, like atorvastatin, enalapril, cetirizine, cilostazol, and venlafaxine, are widely used in clinical practice. Based on their mechanism of action, these drugs should not affect the immune system’s response to burn injury, as anti-inflammatory drugs are used to ameliorate organ damage, such as dexamethasone. They might be considered an additional treatment for elderly patients after burn injury. Interestingly, histamine receptor antagonist was found previously to accelerate skin barrier repair. Thus, using cetirizine could have another beneficial effect in treating burns39.
The list of drugs our in silico search identifies involves several FDA-approved compounds used to treat common conditions. Drugs that induce “similar changes” could harm the organ and may be avoided when treating burn injury patients. Drugs that cause “opposite changes” should be further evaluated in animal models of burn-induced liver injury to validate the calculated effect predicted by our analysis.
Our approach via the expression data analysis by Cmap was previously used to predict targeted combination treatment for pancreatic cancer successfully40,41. Thus, we expect that some of the predicted drugs will prove to be beneficial for burn victims. However, the recommendation of using any of the predicted medications in a clinical scenario needs to be supported by in-depth in vivo drug studies and clinical trials as our results have a preliminary character. More follow-up studies are needed to validate the concept and develop a new treatment for burn injury patients.
We accept the murine model’s shortcomings and recognize that these models do not always replicate clinical observations. The animals are genetically similar and live in a controlled environment. While burn patients are treated in a burn intensive care unit (ICU), which provides continuous intravenous fluids, antibiotics, nutrition, and monitoring, the absence of a rodent ICU creates a drastically different treatment environment, adding extra variables that can affect the outcomes of experiments. Rodent skin has a different structure and physiology than human skin, and the quantity and quality of the inflammatory mediators produced by the damaged skin may differ from human skin. Environmental factors originate from many vendors of mice and may have an impact on the outcomes of the research.
In this investigation, the weight difference between young and old mice was around 3–5 grams, which might affect the findings. This study was performed using female mice, given that publications demonstrate higher mortality rates in women who sustain burn injuries than men; however, sex differences can impact the results in murine models of burn injuries42,43,44.
Since this study used the whole liver for transcriptomics and metabolomics analysis, we recognize that other parenchymal and immune cells in the liver can greatly impact the liver transcriptome/metabolome, which should be considered when analyzing this data. However, other studies showed that one day after skin burn injury, there is no significant increase of neutrophils infiltration MPO activity in liver samples45.
In conclusion, we analyzed the gene expression and metabolic responses to burn injury in the livers of aged and young mice and found multiple similarities and differences between them. A significant difference in the livers of aged animals after a burn is a profound downregulation of essential enzymatic superfamily such as the cytochrome P450. By using in silico analysis, we predicted commonly used drugs that may rewire the burn-induced liver response to a more favorable one and thus increase the survival of burn victims. Further study is warranted to evaluate the effect of these drugs on alleviating the burn injury in the aged mice.
Methods
Mice
Young 3–4 months old (equivalent to 20–25 human years) BALB/c and C57BL/6 female mice were obtained from The Jackson Laboratory (Bar Harbor, ME). Aged 20–22 months old (equivalent to 65–70 human years) BALB/c and C57BL/6 female mice from the National Institute of Aging (NIA) Colony (Charles River Laboratories, Wilmington, MA). All omics experiments were performed on BALB/c mice, while both strains were used for qPCR validation. Before the experiments, all mice were housed at the University of Colorado Anschutz Campus’s vivarium for two weeks. Mice were maintained on a 12-hour light/dark cycle with lights on at 8:00 am. All animals were kept in cages with controlled temperature (23 °C–24 °C) and humidity (60% ± 10%). The mice were fed with certified standard chow and tap water ad libitum. The experiments were performed between 9 and 11 am to decrease variability caused by differences in circadian rhythms. All procedures were approved by The University of Colorado Institutional Animal Care and Use Committee.
The ARRIVE guidelines were used to ensure proper reporting of methods, results, and discussion.
Burn injury model
We distributed mice randomly into four experimental groups (young sham, young burn, aged sham, and aged burn). To create a controlled burn injury, we used the method described by Faunce et al.46. The mice were anesthetized with isoflurane, 55.5 mg/kg of ketamine Intra peritoneal (lP), and 2.6 mg/kg of xylazine IP (Webster Veterinary, Sterling, MA). While anesthetized, each mouse’s dorsum was shaved. Each mouse was then placed individually in a plastic template designed to expose 15% total body surface area (TBSA) of skin calculated as described47. Mice were then exposed to 94 degrees Celsius (for the burn groups) or room temperature water baths (for the sham groups) for 8 s as previously described46,48. Following this method, exposure of the mice’s dorsum to 94 degrees Celsius water induces a localized full-thickness skin burn46. After this procedure, each mouse received additional pain medication (0.13 mg/kg buprenorphine IP) and normal saline IP for resuscitative purposes according to the parkland formula (4 × body weight (kg) × TBSA(%)). The mice were assessed and monitored through the post-procedure recovery preserving normothermia using warm pads. Lastly, the mice were humanly euthanized using CO2 followed by cervical dislocation, 24 h (for transcriptomics and metabolomics data) and at multiple points 6-, 9-,12-, and 24 h in a time course experiment (for transcriptomics validation) after the burn injury procedure.
Tissue and sample processing
Following euthanasia, the livers of all mice were infused with ice-chilled saline via the portal vein. For consistency, the right hepatic lobe in each animal was snap frozen in liquid nitrogen and then stored at −80 °C for further analysis. Livers were maintained in tubes on dry ice when pieces were removed for homogenization, and homogenized tissue was kept in tubes on ice prior to analysis.
RNA preparation and gene expression analysis
RNA was extracted from liver using a RNeasy mini kit (Qiagen, Hilden, Germany) as previously described9,10,11, following the manufacturer’s recommended protocol. cDNA was then synthesized using an iScript kit according to manufacturer protocol (Bio-Rad, Hercules, CA). Quantitative RT-PCR was was performed using Universal SYBR Green Supermix (BioRad, #1725124). Standard desalted primers were purchased from Sigma. Cyp2c29 Forward Primer: 5′ GCTCTCCTACTCCTGCTGAAGT 3′ Reverse Primer: 5′ ATGTGGCTCCTGTCTTGCATGC 3′ Cyp2c38 Forward Primer: 5′ CCTTGTCCCTAACAACCTACCC 3′ Reverse Primer: 5′ GGAACTCCTTGCTGTCATGCAG 3′ Cyp2c40 Forward Primer: 5′ CAAGAGGAAGCACAGTGGCTCA 3′ Reverse Primer: 5′ GGAAAACAATGGAGCAGATGACAT 3′ Cyp2c54 Forward Primer: 5′ GGACATCTGCCAATCCTTCACC 3′ Reverse Primer: 5′ GGTCAACCAGAGCTTCCTTCAC 3′ run on a QuantStudio 3 Real-Time PCR System (Applied Biosystems, Foster City, CA). Gene expression was quantified using the ΔΔCt algorithm, with Gapdh as the endogenous control (Cat No. 4352339E, Applied Biosystems, Foster City, CA).
RNA sequencing
The Genomics Shared Resource performed RNA sequencing in the Cancer Center shared resource core at the University of Colorado Anschutz Medical Campus. 100 ng of total RNA was used to construct an Illumina-compatible mRNA library using Tecan Universal Plus mRNA-SEQ kit Cat No. 0520-A01. Sequencing was done on an Illumina NovaSEQ6000 Instrument using an S4 Flow Cell paired-end sequencing 2 × 150. FASTQ files were delivered after standard demultiplexing procedures were used, converting.bcl files to.seq files using CASAVA software as described49,50.
Metabolomic analysis
The Mass Spectrometry Metabolomics Shared Resource Facility at the University of Colorado Anschutz Medical Campus processed and analyzed the metabolomics data. Briefly, mass spectrometry-based metabolomics was performed on frozen liver samples. For polar metabolites, tissues were extracted at 15 mg per mL in ice-cold lysis/extraction buffer (methanol:acetonitrile:water 5:3:2), and 10 µL of supernatants were analyzed using a 5 min C18 gradient in positive and negative ion modes (separate runs)51,52. For polar lipids, tissues were extracted at 7.5 mg per mL in cold methanol containing stable isotope-labeled standards (see attached list), and 10 µL of supernatants were analyzed using a 17 min gradient in negative ion mode as previously described53. Data was acquired on a Thermo Vanquish UHPLC system coupled online to a Thermo Q Exactive mass spectrometer. Data analysis was performed in Maven against an in-house compound library as described52,53.
Statistics and data reproducibility
The NetworkAnalyst platform was used to perform differential expression analysis with EdgerR test after filtering out genes with variance lower than 15 and abundance lower than 4 and transforming data with upper quantile normalization (Supplementary Data 1–4). Data visualization for transcriptomic analysis was performed with volcano plots and principal component analysis54. For the transcriptomics analysis, statistical significance was considered with adj. p < 0.05 values with n = 3 per group. For transcriptomics validation, qPCR data were analyzed in 100 mice (20 Balb/c and 80 C57BL/6) at different time points (6-,9-12-, and 24 h after burn; n = 5 per study group). We used Graph Pad Prism 9.3.1. The D’Agostino-Pearson normality test was used to check the normal distribution of the variables. For the statistical analysis of variables with a normal distribution, the student t-test or ANOVA was used, whereas, for variables with a non-normal distribution, the Mann–Whitney U test was used. A p value < 0.05 was considered significant, and all tests were two-sided.
Heatmap from metabolomic data was performed with Multiple Experiment Viewer (MeV 4.8)55; a p value lower than 0.05 was considered statistically significant with n = 5 per group. Overrepresentation analysis was performed with the g:Profiler56 using the KEGG database.
The experimental design was presented with graphics designed with the BioRender platform.
In silico analysis
To perform a functional analysis, construct networks, and predict upstream regulators, we used QIAGEN’s Ingenuity® Pathway Analysis (IPA®, QIAGEN Redwood City, www.qiagen.com/ingenuity). Network of direct and indirect connections of differentially expressed genes and metabolites overlapping for both young and aged mice after burn injury were used to feed the IPA algorithm. Nodes without any connections were excluded from the analysis. Prediction of upstream regulators of metabolic and transcriptomic changes after the burn injury was performed only using experimentally proven data for hepatocytes and/or liver from Qiagen knowledge base.
In silico drug repurposing prediction was done using the Connectivity map platform (https://clue.io/)57. The platform correlates the observed gene set dysregulation with known effects of perturbations on multiple cell lines. We narrowed our analysis to drugs tested on HepG2 cell lines as the closest to our experimental setting. For our analysis threshold for tau score >95 was considered to select drugs with similarity signature to our query, and <−95 for selecting drugs with the opposing signature. Tau score is a standardized measure ranging from −100 to 100, corresponding to the fraction of reference gene sets with significant similarity to the drug than the current query.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data produced within this manuscript were attached as ‘Supplementary Materials’ file. Raw sequencing data are available in Sequence Read Archive (SRA) under following number: SUB13385022.
References
Rajha, E. et al. Epidemiology of burn patients presenting to a tertiary hospital emergency department in Lebanon. Burns 44, 218–225 (2018).
Crowe, C. S. et al. Trends of burn injury in the United States: 1990 to 2016. Ann. Surg. 270, 944–953 (2019).
Jeschke, M. G. et al. Burn injury. Nat. Rev. Dis. Prim. 6, 1–25 (2020).
Jeschke, M. G. The hepatic response to thermal injury: is the liver important for postburn outcomes? Mol. Med. 15, 337–351 (2009).
Jeschke, M. G., Lopez, O. N. & Finnerty, C. C. In Total Burn Care 259–267.e253 (Elsevier, 2018).
Jeschke, M. G., Micak, R. P., Finnerty, C. C. & Herndon, D. N. Changes in liver function and size after a severe thermal injury. Shock 28, 172–177 (2007).
Adiga, U. & Adiga, S. Biochemical changes in burns. IJRSB 3, 88–91 (2015).
Gong, Y., Long, X., Xu, H., Yang, X. & Guo, Q. The changes and prognostic value of liver function in young adults with severe burn: a retrospective observational study. Medicine 97.e13721 (2018).
Idrovo, J.-P., Boe, D. M., Kaahui, S., Yang, W.-L. & Kovacs, E. J. Hepatic inflammation after burn injury is associated with necroptotic cell death signaling. J. Trauma Acute Care Surg. 89, 768 (2020).
Idrovo, J.-P. et al. Advanced age heightens hepatic damage in a murine model of scald burn injury. J. Trauma Acute Care Surg. 90, 731–737 (2021).
Abdullahi, A. et al. Activation of ER stress signalling increases mortality after a major trauma. J. Cell. Mol. Med. 24, 9764–9773 (2020).
Heidecker, B. & Hare, J. M. The use of transcriptomic biomarkers for personalized medicine. Heart Fail. Rev. 12, 1–11 (2007).
Cavalli, M. et al. A multi-omics approach to liver diseases: integration of single nuclei transcriptomics with proteomics and HiCap bulk data in human liver. OMICS: J. Integr. Biol. 24, 180–194 (2020).
Gomez, C. R., Nomellini, V., Baila, H., Oshima, K. & Kovacs, E. J. Comparison of the effects of aging and IL-6 on the hepatic inflammatory response in two models of systemic injury: scald injury versus ip LPS administration. Shock (Augusta, Ga.) 31, 178 (2009).
Hammer, H., Schmidt, F., Marx-Stoelting, P., Pötz, O. & Braeuning, A. Cross-species analysis of hepatic cytochrome P450 and transport protein expression. Arch. Toxicol. 95, 117–133 (2021).
Deng, J., Guo, L. & Wu, B. Circadian regulation of hepatic cytochrome P450 2a5 by peroxisome proliferator-activated receptor γ. Drug Metab. Dispos. 46, 1538–1545 (2018).
Bhushan, B. & Michalopoulos, G. K. Role of epidermal growth factor receptor in liver injury and lipid metabolism: emerging new roles for an old receptor. Chem. Biol. Interact. 324, 109090 (2020).
Komposch, K. & Sibilia, M. EGFR signaling in liver diseases. Int. J. Mol. Sci. 17, 30 (2015).
Lemaigre, F. P. Mechanisms of liver development: concepts for understanding liver disorders and design of novel therapies. Gastroenterology 137, 62–79 (2009).
Peck, M. D. Epidemiology of burns throughout the world. Part I: distribution and risk factors. Burns 37, 1087–1100 (2011).
Jeschke, M. G. et al. Pathophysiologic response to burns in the elderly. EBioMedicine 2, 1536–1548 (2015).
Hunt, N. J., Kang, S. W. S., Lockwood, G. P., Le Couteur, D. G. & Cogger, V. C. Hallmarks of aging in the liver. Comput. Struct. Biotechnol. J. 17, 1151–1161 (2019).
Kim, H., Kisseleva, T. & Brenner, D. A. Aging and liver disease. Curr. Opin. Gastroenterol. 31, 184 (2015).
Morsiani, C. et al. The peculiar aging of human liver: a geroscience perspective within transplant context. Ageing Res. Rev. 51, 24–34 (2019).
Plackett, T. P. et al. The early acute phase response after burn injury in mice. J. Burn Care Res. 28, 167–172 (2007).
Wu, K.-C. & Lin, C.-J. The regulation of drug-metabolizing enzymes and membrane transporters by inflammation: evidences in inflammatory diseases and age-related disorders. J. Food Drug Anal. 27, 48–59 (2019).
Nepomniashchikh, V., Lomivorotov, V., Deryagin, M., Lomivorotov, V. & Kniazkova, L. Cytochrome P450-endogenous substrates metabolism is reduced in patients with a multiple organ dysfunction after coronary artery bypass grafting. Inter. Med. Appl. Sci. 4, 9–14 (2012).
Renton, K. W. Cytochrome P450 regulation and drug biotransformation during inflammation and infection. Curr. Drug Metab. 5, 235–243 (2004).
Sasaki, E. & Yokoi, T. Role of cytochrome P450-mediated metabolism and involvement of reactive metabolite formations on antiepileptic drug-induced liver injuries. J. Toxicol. Sci. 43, 75–87 (2018).
Klomp, S. D., Manson, M. L., Guchelaar, H.-J. & Swen, J. J. Phenoconversion of cytochrome P450 metabolism: a systematic review. J. Clin. Med. 9, 2890 (2020).
Graves, J. P. et al. Expression of Cyp2c/Cyp2j subfamily members and oxylipin levels during LPS‐induced inflammation and resolution in mice. FASEB J. 33, 14784–14797 (2019).
Goldstein, J. A. & De Morais, S. Biochemistry and molecular biology of the human CYP2C subfamily. Pharmacogenetics 4, 285–299 (1994).
Esteves, F., Rueff, J. & Kranendonk, M. The central role of cytochrome P450 in xenobiotic metabolism—A brief review on a fascinating enzyme family. J. Xenobiot. 11, 94–114 (2021).
Aliu, E., Kanungo, S. & Arnold, G. L. Amino acid disorders. Ann. Transl. Med. 6, 471 (2018).
Sommerhalder, C. et al. Current problems in burn hypermetabolism. Curr. Probl. Surg. 57, 100709 (2020).
Bessone, F., Razori, M. V. & Roma, M. G. Molecular pathways of nonalcoholic fatty liver disease development and progression. Cell. Mol. Life Sci. 76, 99–128 (2019).
Rifaioglu, A. S. et al. Recent applications of deep learning and machine intelligence on in silico drug discovery: methods, tools and databases. Brief. Bioinform. 20, 1878–1912 (2019).
Shaker, B., Ahmad, S., Lee, J., Jung, C. & Na, D. In silico methods and tools for drug discovery. Comput. Biol. Med. 137, 104851 (2021).
Bacci, S. Fine regulation during wound healing by mast cells, a physiological role not yet clarified. Int. J. Mol. Sci. 23, 1820 (2022).
Biancur, D. E. et al. Compensatory metabolic networks in pancreatic cancers upon perturbation of glutamine metabolism. Nat. Commun. 8, 15965 (2017).
De Lellis, L. et al. Drug repurposing, an attractive strategy in pancreatic cancer treatment: preclinical and clinical updates. Cancers (Basel) 13, 3946 (2021).
Bazhan, N. et al. Sex differences in liver, adipose tissue, and muscle transcriptional response to fasting and refeeding in mice. Cells 8, 1529 (2019).
Gasparin, F. R. S. et al. Sex differences in the development of hepatic steatosis in cafeteria diet-induced obesity in young mice. Biochim. Biophys. Acta Mol. Basis Dis. 1864, 2495–2509 (2018).
Ullah, I. et al. Effect of sex-specific differences on function of induced hepatocyte-like cells generated from male and female mouse embryonic fibroblasts. Stem Cell. Res. Ther. 12, 1–14 (2021).
Li, X., Akhtar, S., Kovacs, E. J., Gamelli, R. L. & Choudhry, M. A. Inflammatory response in multiple organs in a mouse model of acute alcohol intoxication and burn injury. J. Burn Care Res. 32, 489–497 (2011).
Faunce, D. E., Gregory, M. S. & Kovacs, E. J. Effects of acute ethanol exposure on cellular immune responses in a murine model of thermal injury. J. Leukoc. Biol. 62, 733–740 (1997).
Gouma, E. et al. A simple procedure for estimation of total body surface area and determination of a new value of Meeh’s constant in rats. Lab. Anim. 46, 40–45 (2012).
Kovacs, E. J., Grabowski, K. A., Duffner, L. A., Plackett, T. P. & Gregory, M. S. Survival and cell mediated immunity after burn injury in aged mice. J. Am. Aging Assoc. 25, 3–9 (2002).
Ambardekar, A. V. et al. Matrix-degrading enzyme expression and aortic fibrosis during continuous-flow left ventricular mechanical support. J. Am. Coll. Cardiol. 78, 1782–1795 (2021).
Joshi, M. et al. CPT1A over-expression increases reactive oxygen species in the mitochondria and promotes antioxidant defenses in prostate cancer. Cancers (Basel) 12, 3431 (2020).
Gehrke, S. et al. Red blood cell metabolic responses to torpor and arousal in the hibernator arctic ground squirrel. J. Proteome Res. 18, 1827–1841 (2019).
Nemkov, T., Reisz, J. A., Gehrke, S., Hansen, K. C. & D’Alessandro, A. In High-throughput metabolomics 13–26 (Springer, 2019).
Reisz, J. A., Zheng, C., D’Alessandro, A. & Nemkov, T. In High-throughput metabolomics 121–135 (Springer, 2019).
Zhou, G. et al. NetworkAnalyst 3.0: a visual analytics platform for comprehensive gene expression profiling and meta-analysis. Nucleic Acids Res. 47, W234–W241 (2019).
Howe, E. et al. In Biomedical informatics for cancer research 267–277 (Springer, 2010).
Raudvere, U. et al. g: Profiler: a web server for functional enrichment analysis and conversions of gene lists (2019 update). Nucleic Acids Res. 47, W191–W198 (2019).
Subramanian, A. et al. A next generation connectivity map: L1000 platform and the first 1,000,000 profiles. Cell 171, 1437–1452.e1417 (2017).
Acknowledgements
The Genomics Shared Resource performed RNA sequencing in the Cancer Center shared resource core at the University of Colorado Anschutz Medical Campus. The Mass Spectrometry Metabolomics Shared Resource Facility at the University of Colorado Anschutz Medical Campus processed the metabolomics data. The research in this publication was supported by K08GM134185 (JPI) and R01AG018859, R01GM115257, R35GM131831, and 1 I01 BX004335 (EJK). The content in this report is the authors’ responsibility and does not primarily represent the formal National Institutes of Health opinion.
Author information
Authors and Affiliations
Contributions
B.M., I.M., W.-L.Y., E.J.K., and J.-P.I. conceived and planned the experiments. D.B., A.Q., and J.-P.I. performed the burn injury experiment and collected tissue samples. B.M. analyzed all transcriptomics and metabolomics data and generated the graphics and figures. B.M., I.M., W.-L.Y., E.J.K., J.N.L. and J.-P.I. contributed to the analysis and interpretation of the results. All authors provided critical comments and helped in the creation of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Biology thanks the anonymous reviewers for their contribution to the peer review of this work. Primary Handling Editor: Karli Montague-Cardoso. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Malachowska, B., Yang, WL., Qualman, A. et al. Transcriptomics, metabolomics, and in-silico drug predictions for liver damage in young and aged burn victims. Commun Biol 6, 597 (2023). https://doi.org/10.1038/s42003-023-04964-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s42003-023-04964-2