Abstract
Cognitive impairment after stroke is heterogeneous: there is no strict correspondence between brain damage and magnitude of deficit or recovery. Protective factors such as cognitive or brain reserve have been invoked to explain the mismatch. Here, we consider the opposite point of view: the instances in which this protection is overturned. We leveraged on multitasking to stress the brain’s processing limits and unveil deficits that may be missed by standard testing in a sample of 46 patients with unilateral subacute to chronic stroke and no sign of lateralized spatial-attentional disorders at neuropsychological paper-and-pencil tests. Multivariate analyses identified a phenotype of patients with high susceptibility to multitasking, showing stark contralesional spatial awareness deficit only when multitasking. Multivariate brain-behavior mapping based on lesions location and structural disconnections pointed to the Multiple-Demand System, a network of frontal and fronto-parietal areas subserving domain-general processes. Damage in this network may critically interact with domain-specific processes, resulting in subtle and yet invalidating deficits. Indeed, these patients (one-third of the sample) presented worse performance in tests evaluating activities of daily living and domain-general abilities. We conclude that the theoretical construct of susceptibility to multitasking helps understanding what marks the passage to clinically visible deficits after brain damage.

Similar content being viewed by others
Introduction
Stroke is one of the leading causes of death and morbidity worldwide1, with an estimated 50% of stroke survivors presenting significant sequelae. Neuropsychological research has typically focused on the characterization of (stark) behavioral impairments and the associated lesions to cortical and subcortical structures2, which is also very important for the study of recovery and rehabilitation3,4. The statistics imply, however, that a significant proportion of stroke survivors may, in fact, have minor consequences. Another positive news is that—despite the aging population, and a prevalence of stroke that is forecasted to sensibly increase in the western world5,6—the advances in primary prevention strategies are gradually shifting the burden of stroke from mortality to disability. The widespread adoption of early treatments (e.g., thrombolysis) further contributes to containing this burden6. As a result, the line separating relatively spared patients and patients with some degree of impairment is shifting but also becoming more blurred and uncertain. Therefore, it will be increasingly important, in the future, to study what marks the passage to stroke sequelae with enhanced resolution, as patients near this frontier will increase and may jeopardize the available clinical resources. The aim of this study is to better characterize where we should be drawing the thin, blurred line which, if crossed, determines the onset of cognitive deficits, with a special focus on disorders of spatial awareness.
The main path to a finer resolution in our assessment of patients’ deficits is developing tools that are sufficiently sensitive to a given construct (that is, a deficit). The most obvious way to achieve that is through technological advances. For example, when compared to clinical inspection, or tools that are designed for a coarse, quick clinical evaluation (for example, paper-and-pencil neuropsychological tests), computerized assessment offers a more sensitive and nuanced quantification of the impairment and the outcome of rehabilitation7,8,9,10,11. A second, less obvious way is informed by theory and is based on our state-of-the-art knowledge of brain functions and their inherent limitations.
Humans have, indeed, a limited capacity to process information12. Our performance typically declines when concurrent demands increase and/or serial information processing is required. For example, when a sequence of stimuli is rapidly presented in foveal13 or peripheral14 vision, the perception of a relevant target might be hampered if presented soon after the detection of a previous one, a phenomenon known as attentional blink. Concurrent task demands modulate the degree of interference by peripheral distracters, suggesting that visuospatial abilities might be particularly hampered by multitasking15. These well-known phenomena are comprehensively framed by the classic psychological literature that, since Broadbent’s seminal filter theory of attention, pinpoints the existence of bottlenecks in the flow of information in the brain16. The most evident obstacle is the case of multiple demands tapping onto the same sensory modality (e.g., visual tasks hampering visual perception). Multiple neuroimaging studies highlight, in the case of visual stimuli, functional deactivation of occipital cortex with increasing task demands17,18, which in turn suggests the existence of early peripheral processing bottlenecks that result in significant performance limitations. The behavioral impact of multitasking, however, can extend well beyond unimodal sensory effects to become domain-general or multisensory when higher-order processes are required. Working memory load, for example, similarly hampers visual search (to the point of inducing attentional blindness) and deactivates the temporo-parietal areas devoted to this main task19,20,21. These limitations are structural and computational in nature and, as such, can be consistently detected in the healthy brain. However, their impact is particularly profound in the presence of a disturbance to said architecture, as in the case of a brain lesion affecting the optimal integration between brain networks.
Unsurprisingly, multitasking has been reported to exacerbate symptoms across behavioral domains, from more basic motor (e.g., balance and walking22, finger tapping23) or sensory functions (e.g., vestibular24), to higher level functions such as visual awareness9,10,11,25,26,27. In principle, multitasking can be added to any test, and it would presumably unveil even subtle deficits, if present, by creating a condition in which the available cognitive and attentional resources are diverted away and thus made unable to compensate for these difficulties28. Conversely, an increased susceptibility to multitasking caused by brain damage can be regarded as a major determinant of the emergence of frank deficits in a given behavioral domain whenever the context is more taxing due to concurrent task demands. Hence, susceptibility to multitasking may provide a crucial signature of stroke outcome. Besides being transversal in nature (i.e., affecting diverse behavioral domains alike), multitasking conditions are also arguably ubiquitous in daily life situations, which also hints at their better generalizability.
This notion bears a striking resemblance with the concept of “strategy application disorder”, which has been applied to patients showing deficits restricted to conditions of multitasking following lesions of the right dorsolateral prefrontal cortex29,30. Action planning and task-switching have been classically considered a hallmark of executive functions, and their malfunctioning may very well subtend the emergence of multitasking deficits. However, a recent meta-analytic review suggests that multitasking and task-switching also present distinctive brain activation profiles31. While both dual-tasking and task-switching activate the bilateral intraparietal sulcus (IPS), left dorsal premotor cortex (dPMC), and right anterior insula, dual-tasking more specifically engages the bilateral frontal operculum, bilateral dPMC, bilateral anterior IPS, left inferior frontal sulcus, and left inferior frontal gyrus31. That said, the inconsistent use of labels and the different behavioral paradigms led to numerous discrepancies in the neurophysiological literature, pointing to the need of a unified framework to study dual-tasking32. The concept of multiple-demand system33—describing a network of frontal and parietal areas associated with diverse cognitive tasks, as well as fluid intelligence—by stressing the commonality between different tasks and domains, is one potential candidate for this role34,35,36,37,38,39,40. Susceptibility to multitasking might also be related to the notion of cognitive/brain reserve, which is typically invoked to explain the mismatch between the objective quantification of brain damage and the resulting clinical outcome41,42,43. In this regard, cognitive reserve is a major protective factor, shielding from cognitive deficits after brain disease, while susceptibility to multitasking might be regarded as the potential for this protective action to be overturned by unspecific demands. Therefore, quantifying susceptibility to multitasking, under these assumptions, enables the identification of the gray area in which brain damage can or cannot result in overt behavioral symptoms.
In this study, we capitalize on a dual-task paradigm originally proposed by Bonato and colleagues11. The task requires patients to report the side of appearance of one or two briefly presented dots that are displayed on the left, right, or on both sides of the screen, hence mimicking the classic diagnostic test for visual neglect and extinction44. Crucially, this primary, spatial monitoring task is administered alone (Single Task, ST) or in dual tasking conditions, both visual (Visual Dual Task, VDT) or auditory (Auditory Dual Task, ADT), though in absence of low-level, perceptual changes (see Fig. 1). Previous small-scale studies have confirmed the emergence of subtle lateralized biases in these latter conditions9,10,11 making this paradigm an excellent candidate to highlight and quantify susceptibility to multitasking. We thus administered the multitask paradigm to a sample of 46 patients with unilateral subacute or chronic stroke and no sign of lateralized attentional disorders according to established paper-and-pencil diagnostic tests (i.e., the Behavioral Inattention Test, BIT45). Our goals were: i) to identify a phenotype characterized by high susceptibility to multitasking; ii) to study its neuroanatomical (lesion) correlates; and iii) to study (indirect) structural disconnections46, since behavioral deficits in stroke reflect both structural damage at the site of injury and more widespread network dysfunction caused by lesions to white-matter tracts. In this regard, one outstanding question was whether the multitasking-induced spatial awareness deficit is primarily related to damage affecting a domain-specific visuospatial mechanism, such as the right-hemisphere network associated to neglect47,48, or a domain-general mechanism such as the Multiple-Demand (MD) system33, involving the frontal regions that subtend dual-tasking (e.g., bilateral frontal operculum, dorsal premotor cortex, inferior frontal gyrus)31.
The task consisted in a primary spatial monitoring task, in which the location of small dot(s) flashing briefly on the screen had to be reported (i.e., left, right, both sides). In the Single Task (ST), this was the only requirement. In the Auditory Dual Task (ADT), patients also had to report the object corresponding to the sound that they previously heard through headphones, whereas in the Visual Dual Task (VDT) they had to report the shape previously presented at fixation. The condition was made explicit in the instructions, which were given before each block. Note that conditions only differed for their task demands, but not for sensory properties. Thus, the difference in performance between single and dual-tasks is particularly suited to evaluate susceptibility to multitasking. The visual stimuli are not depicted in scale, see main text for an extended description.
Materials and methods
Participants
Forty-six stroke patients (age: mean = 61.5 y, SD = 12.62, M = 33, F = 13) in the subacute or chronic phase were included in this prospective study. The sample consisted of all eligible patients admitted to IRCCS San Camillo Hospital (Venice, Italy) for stroke rehabilitation over a period of ~5 years (from March 2016 to September 2021). The enrollment of patients had the following inclusion criteria: adult age, first-ever unilateral stroke, right-handedness as assessed by a standard questionnaire49, and spared performance in the conventional part of the Behavioral Inattention Test (BIT), which is a standard paper-and-pencil battery for the assessment of spatial neglect45. Exclusion criteria were the presence of a history of other neurological or psychiatric disorders, primary hearing, sight, or clinically evaluated visual field deficits, as well as the inability to understand and provide informed consent. The final sample included 29 patients with right hemisphere damage (RHD) and 17 patients with left hemisphere damage (LHD). All patients underwent comprehensive neuropsychological assessment and were administered the computerized task assessing susceptibility to multitasking. Structural brain scans were also collected for lesion analysis upon admission to the hospital. We acquired 37 MRI and 8 CT scans (one patient did not consent to the scan). CT scans can lead to underestimate white matter damage, but we retained them to increase the statistical power of the lesion-symptom mapping. The sample was also heterogeneous in terms of time from stroke (Supplementary Table 1), reflecting the fact that only subacute and chronic patients are admitted to the rehabilitation hospital but with no specific constraint on timing. Variability in time from stroke is a potential confound, so we considered this variable both in the behavioral and neuroimaging analyses. Note, however, that all data considered in the present study (neuroimaging, neuropsychological, and computerized task) were acquired within a short time window of 2–3 weeks upon patient’s recruitment. All participants gave their informed written consent, in accordance with the Declaration of Helsinki. The study protocol was approved by the regional Ethics Committee (Comitato Etico per la Sperimentazione Clinica della Provincia di Venezia e IRCCS San Camillo; protocol n. 2015.09 and n. 2018.04).
Neuropsychological assessment
The neuropsychological assessment explored general cognitive functioning with the Mini-Mental State Examination—MMSE50, which evaluates very superficially areas including memory, attention, and language through a series of questions. Non-verbal, abstract reasoning and logic problem solving were assessed via the Raven’s progressive matrices51: the matrices require choosing, among different geometrical patterns, the one that fits with the three given panels considering any specific feature. The Attentional Matrices test52 was administered to evaluate attentional processes, particularly selective attention: the test requires to locate target stimuli that are scattered along a grid composed of both targets and distractors. Executive functions were evaluated via the Modified Card Sorting Test—MCST53, which assesses cognitive flexibility and task switching by requiring patients to sort cards according to different abstract rules. For this test, two sub-scales are given: one that indexes the capability to find and adapt to the hidden rules, and one that reflects perseverations and deficits in set-shifting; both can be sensitive measures of frontal dysfunctions. Next, long-term memory was assessed via different tests, depending on the side of hemispheric damage and thus (on average) the linguistic or visuo-spatial components that are more likely affected. Patients with RHD were administered the Rey’s auditory verbal learning test51; patients with LHD were administered the Rey’s figure54. These tests require delayed recalling of a list of words or of a complex drawing, respectively. To evaluate visuo-spatial attention, we administered the BIT45 (conventional part), which provides a set of standard paper and pencil tasks to evaluate spatial attentional biases and hemispatial neglect (i.e., cancellation, line bisection, copy, and drawing tasks). According to our patients’ inclusion criteria, the overall BIT score had to be higher than the conventional cutoff point of 129 (scale range 0–140, with higher values indexing better performance) to exclude a clinical deficit. We also administered the Kessler Foundation Neglect Assessment Process55 (KF-NAP), which provides instead a functional examination of daily living autonomy (e.g., moving, having lunch, washing one’s own face) as impacted by spatial awareness deficits, and as assessed by specifically-trained personnel. The KF-NAP is a structured scale built upon the Catherine Bergego Scale (CBS56); accordingly, few missing patients’ data for the KF-NAP were replaced by CBS scores to increase statistical power for this particular test, given its importance (values were adapted to the appropriate range, i.e. 0–10, with increasing values indexing more impaired performance). Finally, a language comprehension test was additionally administered to LHD patients to quantify the degree of linguistic impairments (Token test in the Aachener Aphasie Test—AAT57). Due to constraints of the clinical setting, it was not always possible to acquire complete data for all the tests presented here. We decided, whenever warranted, to analyze the results as such, that is without imputation of the missing scores. Accordingly, these analyses may present various degrees of statistical power.
Computerized task
We administered a computerized multitasking paradigm previously optimized for patients suffering from either left or right hemisphere stroke9. Patients sat in a quiet room, at about 60 cm from the computer screen (38 × 30.5 cm). The task ran through E-Prime 2.0 (Psychology Software Tools, Pennsylvania, USA, http://www.pstnet.com). Each trial started with a black screen (1000 ms), followed by a centrally-presented white fixation cross (about 1 cm wide, 1000 ms). The fixation cross flickered for 200 ms before target presentation, as to direct attention to the screen center. The target was a white dot (~8 mm in diameter), which appeared for about 100 ms in three different locations: unilaterally, on the left or right side of the screen, or bilaterally at both sides of the screen (in all cases 170 mm away from fixation). Additional “catch” trials were administered and did not involve any lateralized target. All trials were equiprobable (i.e., 25% of frequency). Simultaneously to the primary target(s), and for a duration of 100 ms, a visual shape (i.e., square, circle or triangle) replaced the central fixation cross, and a sound (i.e., one of three ecological sounds, i.e. train whistle, hammer or doorbell) was binaurally delivered through headphones. Finally, a white-noise mask was presented until response to minimize the retinal after-effects induced by the dot(s) (Fig. 1).
The paradigm consists of three conditions: single task (ST), visual-dual task (VDT), and auditory dual-task (ADT). Task demands differed across conditions whereas sensory stimulation remained identical throughout the experiment. Patients were always asked to detect the position of the lateralized dots, i.e., a spatial monitoring task. This enables the assessment of both spatial neglect and visual extinction by measuring accuracy in reporting contralesional vs. double stimuli. In dual-task conditions, however, patients had to additionally report the central shape (VDT) or the sound (ADT). In the multitasking conditions, patients always had to report their response to the spatial monitoring task first, followed by the response about the shape (VDT) or sound (ADT). The majority of patients responded verbally to both requests. In case of difficulties in naming, patients could respond by pointing to flashcards with drawings of the possible options placed in front of them. These drawings depicted lateralized dots (spatial monitoring task) or objects (secondary tasks), which patients could indicate with their fingers. The experimenter coded the responses on a keyboard and monitored the patient’s gaze in order to discard trials in which fixation was not maintained. This check was performed manually by the clinician in charge of testing, and it was thus only intended to spot prominent lapses of attention (e.g., the head visibly turned away from the screen). Reaction times were not considered given that the responses were imputed by the experimenter.
The experimental paradigm consisted of a first ST practice block with 21 trials, followed by six experimental blocks, 36 trials each, administered in a fixed order (i.e., ST, VDT, ADT, VDT, ADT, ST), for a total duration of about 40 min and 216 trials (minimum number of trials per cell: 18).
Behavioral data analysis
Data preprocessing
Practice trials, used for familiarization, were discarded. Catch trials, which were included to rule out guessing strategies or the presence of productive symptoms (e.g., perseverations), were also excluded based on the low proportion of false alarms (less than 6% on average) across both RHD and LHD patients. All trials in which the dot-target was presented (i.e., left, right, or both sides) were coded as ipsilesional, contralesional, and bilateral, in order to make the responses of LHD and RHD patients directly comparable. Accuracy of target detection for each patient was therefore computed as a function of Location (i.e., Ipsilesional, Contralesional, and Bilateral) and Load (i.e., ST, ADT, VDT).
Patients’ clustering
In order to identify potentially distinct phenotypes based on performance in the computerized task, we used a purely data-driven (unsupervised) k-means clustering algorithm on the multivariate pattern of accuracy across the 9 variables given by the 3 × 3 combination of Location (Ipsilesional, Contralesional, and Bilateral) and Load (ST, VDT, ADT). The procedure has the objective of delineating k groups with the constraint that differences must be maximized between groups and minimized within groups—i.e. groups must be homogeneous internally but also clearly separated, such that the performance of patients belonging to the same cluster is similar whereas patients belonging to different clusters present substantial qualitative and/or quantitative differences. We choose k = 2 for classification based on inspection of the scree plot depicting within-groups variance by k (see Supplementary Fig. 1). The internal consistency of this parameter was also probed by repeating the clustering procedure with two subsets of the data. The two subsets represented “short” versions of the computerized task, in which only the first block of multitasking trials (i.e., either ADT or VDT) was assessed in conjunction with the first block of baseline trials (ST). Besides checking the internal reliability of the task and algorithm, these analyses also assessed the feasibility of a more time-efficient, brief version of the task which includes only one third of the trials. Note that, however, for all subsequent analyses we used the data obtained from the extended behavioral task, for enhanced precision. Finally, the data-driven clustering procedure dispenses from the problem of establishing a somewhat arbitrary performance cut-off to assign patients to subgroups. It is worth noting that healthy elderly and even patients with Mild Cognitive Impairment tend to perform very close to the ceiling in our computerized task9, suggesting that it is not sensitive to unspecific, global cognitive impairments. Thus, k-means clustering allows us to detect patients with deviant performance within the overall sample of stroke patients.
Once k was chosen, we assessed whether RHD and LHD patients were equally represented in the clusters through a chi-squared test. Performance in the computerized task was assessed using analysis of variance (ANOVA) with Location and Load as within-subjects factors and cluster as between-subjects factor. Then, we assessed whether the newly defined clusters differed in terms of clinical variables (lesion volume, time from stroke onset, etiology), demographic variables (age, education), and performance in conventional neuropsychological tests; Welch’s correction for unequal groups’ variances was used for t-tests when appropriate (this correction leads to degrees of freedom with decimal points), and the resulting p-values are reported both uncorrected and corrected for multiple comparisons using the False Discovery Rate (FDR)58.
Data reduction: principal component analysis
The patients’ multivariate patterns defined by nine accuracy variables (3 × 3 combination of Location and Load conditions) were also submitted to rotated Principal Component Analysis (rPCA) to summarize the behavioral performance with few latent factors. We used an oblique rotation (promax59) because, for behavioral data, we favored interpretability of the components as psychological constructs, and we did not want to force them to be orthogonal, as clinical factors may often correlate. Promax has been used before for neuropsychological tests60,61 as well as psychophysiological data62. We interpreted rPCs against overall performance and spatial biases in the computerized task. Moreover, we exploited the rPC(s) continuous values to explore the correlation with neuropsychological tests (the resulting p-values are reported both uncorrected and FDR-corrected for multiple correlations), as well as for the neuroimaging data analyses.
Neuroimaging data analysis
Lesion analysis
Individual brain lesions were reconstructed from the patients’ MRI T1-weighted images (N = 37) or CT scans (N = 8). One (RHD) patient did not give consent to be scanned. Each patient’s lesion was reconstructed from the original data and spatially registered on a common coordinate template provided by the Montreal Neurological Institute (MNI152 space, 91 × 109 × 91 with isovoxel resolution of 2 mm) for further processing. For MRI scans, an automated segmentation of brain lesions was performed first using the Lesion Identification with Neighborhood Data Analysis software (LINDA63) and then, after visual inspection, manually corrected with the ITK-snap software64 by two experts (DD and ZR). Normalization into MNI152 space was performed using the pipeline of the BCBToolkit software65 (http://toolkit.bcblab.com), which is based on an enantiomorphic approach66 and uses affine and diffeomorphic deformations for image registration67. Data from five patients had to be excluded from the analyses due to normalization failure (two LHD and three RHD patients). The patients without a usable scan were still included in the behavioral analyses to enhance the precision by which we can identify and describe the clinical phenotype of high susceptibility to multitasking. For CT scans, the lesion maps were manually segmented (DD and ZR) and then normalized using the RegLSM software, running on Matlab68. This method consists of two steps: firstly, native segmented CT is registered to an intermediated template, specific for elderly brains69, and then to the MNI152 template (the same space of MRI scans). Note that normalization to MNI152 is mandatory for computing structural disconnections (see below, also see Salvalaggio et al.46, for discussion).
Structural disconnection
Structural disconnections were computed through the BCBToolkit software65 from each MNI-registered lesion map using 176 healthy controls from the “Human Connectome Project” 7T diffusion-weighted imaging dataset to track fibers passing through each lesioned voxel. The resulting structural disconnection (SDC) maps show only disconnected tracts and indicate the probable location of disconnections70, with each voxel reflecting the probability of disconnection (from 0.5 to 1 if above the conventional threshold of 0.5 and 0 otherwise70).
Multivariate lesion and structural disconnection symptom mapping
Multivariate brain-behavior mapping from lesions and disconnection maps was performed using the established approach of dimensionality reduction of the maps (each consisting of 9,022,292-mm3 voxels) through PCA followed by multiple regression onto a target behavioral score46,71,72. We retained from PCA the components that explained 95% of the variance (that is, 22 components for lesion and 23 components for SDC maps) and used them as input for the regression model. Regression modeling exploited a Best Subset Regression (BSR) strategy using, as dependent variable, the first component obtained from the rPCA on the computerized task scores (rPC1); rPC1 was multiplied by −1 prior to modeling in order to ease data interpretation, so that positive values indicated the presence of a deficit. BSR is a model selection procedure that consists in iteratively testing all possible combinations of predictor variables (with simultaneous inclusion of up to ten predictors at each iteration). We selected the best model using the Bayesian Information Criterion (BIC), which is a stringent selection criterion that strongly penalizes model complexity (thereby minimizing the number of predictors in the final model). We thus obtained the best linear regression model for both lesion and disconnectome maps and then assessed its cross-validated accuracy in terms of R-squared. Our cross-validation setup iteratively left one patient out of the sample and used the model trained on the remaining patients to predict her/his behavioral score, from which the cv-R-squared was calculated. Note that the cross-validated R-squared is only given to gauge the predictive performance of the selected model, but the selection criterion itself remains the BIC. To control for the possible influence of age, lesion volume, and time from stroke onset, these variables were among the possible predictors in the BSR analysis. All covariates were scaled beforehand as to have unit-variance (e.g., direct total lesion volume control, dTLVC73).
Finally, the models’ regression weights were back-projected onto the original space using the transpose matrix of the PC coefficients46. The back-projected values were Z-normalized, smoothed with a Gaussian kernel (sigma = 1 mm), and thresholded at Z = 3 to display the voxels that are most predictive of the behavioral deficit. Predictive maps were visualized in a glass brain (using the niilearn Python library) and the positive Z-scores (which are associated to deficit) were also rendered as a mosaic of 2D slices using MRIcroGL74 (http://www.nitrc.org/). An atlas-based approach75 was used to label the clusters of predictive voxels. For the lesion map we used the Automated Anatomical Labeling (AAL) atlas (version 3) of gray matter structures76. Furthermore, white matter voxels were matched to a tract atlas65,77 for identification.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Demographic, neurological and behavioral data for the whole patients’ sample are reported in Supplementary Table 1. Other information about the complete neuropsychological patients’ profiles are reported in Supplementary Table 2. For the grand means, and the patients’ assignments to the clinical phenotype we refer the reader to Table 1.
Identification of clusters from the computerized task
We assessed patients’ assignments to clusters with k = 2. The first cluster (C1, N = 31) included 13 LHD and 18 RHD patients, that is 67% of the sample; the second cluster (C2, N = 15) included 33% of the patients’ sample, with 4 LHD and 11 RHD. The distribution of RHD and LHD patients did not differ between clusters (X2(1, N = 46) = 0.46, p = 0.496). We repeated the clustering procedure twice using only one block of ST and one block of dual tasking (either ADT or VDT), and checked the new predictions against the original clusters. Because the two clusters were unbalanced (67.4% of patients were in C1), we did not evaluate the new classifications against chance level (50% accuracy) but rather against the more stringent No-Information Rate (NIR) of 67.4%. Both brief versions yielded excellent consistency despite having only one third of the trials compared to the full task. In the brief-visual version (ST + VDT), three patients were misclassified. The balanced accuracy was 91.7%, significantly superior to the NIR (binomial test: p < 0.001, 95% CI [82.1%, 98.6%]). In the brief-auditory version (ST + ADT), only two patients were misclassified. The balanced accuracy was therefore 93.3%, significantly superior to the NIR (binomial test: p < 0.001, 95% CI [85.2%, 99.5%]).
Overall, patients were accurate in reporting the central shape in the VDT (88.59% ± 13.05) or the sound in the ADT (92.12% ± 12) (i.e., the secondary task). The performance of patients in the primary visuospatial task is depicted in Fig. 2 as a function of cluster (Supplementary Fig. 2 and Supplementary Fig. 3 include additional graphs depicting the performance of individual patients and divided by lesioned hemisphere). Patients in C1 consistently achieved near-ceiling performance across all conditions. Patients in C2, however, showed a distinctive pattern of awareness deficit for contralesional targets (i.e., a neglect-like performance), though particularly so during multitasking. In Fig. 3 the same data depicted in Fig. 2 is summarized, and the two multitasking conditions have been averaged together. The 3 (Location) × 3 (Load) × 2 (Cluster) ANOVA on accuracy showed a significant three-way interaction, (F(4,176) = 4.07, p = 0.0035, pes = 0.085). The interaction further indicates that the two clusters differ indeed for the interaction between Load and Location. In other words, the key feature that guided the clustering was not (or not only) a main effect (e.g., lateralized conditions being more difficult) but the emergence of stronger lateralized biases during multitasking.
Accuracy in the computerized task is depicted as a function of dot location (i.e., Ipsi-, Contra-, or Bi-lateral presentation) and load condition (i.e., Single Task - ST, Auditory Dual Task - ADT, and Visual Dual Task - VDT). An automated k-means clustering algorithm identified two clusters of patients within the entire sample (N = 46). Cluster 1 (C1, N = 31) achieved near-ceiling performance, whereas Cluster 2 (C2, N = 15) was characterized by clear lateralized biases which mainly emerged under multitasking conditions. The plot depicts the data distribution through boxplots: here, the boxes extend from the first to the third quartile of the distribution; the black line inside the box depicts the median; whiskers illustrate the variability in the tails of the distribution, and extend to either the minimum/maximum values or 1.5 times the height of the boxes (in which case more extreme values may be present, and are represented as dots). In Supplementary Fig. 2 and Supplementary Fig. 3 further images are available, depicting the performance of individual patients and divided by lesioned hemisphere.
The figure depicts the mean (±SEM) accuracy to the primary (spatial monitoring) task separately for Cluster (1: spared; 2: susceptible to multitasking), side of appearance of the dots, and condition. To define conditions, here we collapsed the auditory and visual dual tasks, since they induced similar detrimental effects.
A finer-grain assessment is described below, in terms of different latent factors defining the two clusters. Overall, the results of the clustering procedure are very clear in pointing to the following conclusions:
-
1.
Two distinct behavioral phenotypes are found when assessing performance under multitasking. One cluster (C1) presents an overall spared, and near-perfect performance, whereas a second cluster (C2) shows markedly compromised performance during multitasking.
-
2.
The difficulties encountered by C2 patients are neither generalized nor unspecific. Indeed, their performance in Ipsilesional trials was largely spared, with more than 83% of correct responses across Load conditions, and thus was not driving the assignment to a distinct cluster. The sharpest performance drops occurred in Contralesional and Bilateral trials, which is a marker of spatial awareness deficit for the contralesional side of space.
-
3.
Crucially, a marked spatial awareness deficit emerged in C2 only when concurrent task-demands were introduced, irrespective of whether the concurrent task engaged the same or a different sensory modality (i.e., VDT vs. ADT). In these conditions, performance of C2 was as low as 22% of correctly-reported targets, whereas in the baseline (i.e., ST) condition the average accuracy remained above 62%. Thus, a context in which attentional resources are limited is particularly prone to unveil any underlying attentional bias, whereas standard conditions may not present sufficient sensitivity and may allow patients to fully compensate for this bias. The fact that the visual and auditory dual tasks similarly affected performance suggests the involvement of a higher order, amodal system, rather than low-level, sensory competition between stimuli.
Control for lesion volume, time from stroke, age, and education
The two clusters did not differ in terms of overall lesion volume (t(19.43) = 1.09, p = 0.29; C1: 49.47 ± 69.56 cm3, C2: 79.79 ± 88.38 cm3), neither for etiology of lesions (X2(1, N= 46) = 0.72, p = 0.395). Time from stroke onset was also comparable in the two clusters (t(29.47) = 0.38, p = 0.70), as all patients were tested in the subacute or chronic stage (C1: 10.79 ± 19.76 months; C2: 9.06 ± 18.52 months). The time from stroke did not correlate with lesion volume (r = −0.14, t(38)= −0.86, p = 0.39). However, patients in C1 were significantly younger (57.3 ± 12.63 years) than patients in C2 (70.1 ± 7.31 years), t(42.37) = 4.31, p < 0.001, while there was no difference in terms of years of formal education (t(26.82) = 0.29, p = 0.77).
To control for the potential confound of age in the clustering solution, we iteratively removed the younger patients from C1 until reaching evidence that the two clusters were comparable in terms of age (using a Bayes Factor <1 for the contrast as criterion; the size of the samples did not allow probing an even stricter threshold of, e.g., Bayes Factor <1/3). This occurred after the exclusion of the 12 youngest patients in C1, yielding a subgroup of N = 19 patients with mean age of 65.68 years (SD = 7.79) that did not differ from the C2 patients’ mean age (t(30.98) = 1.69, p = 0.1; BF = 0.95). We therefore repeated the 3X3X2 ANOVA (Load X Type X Cluster) with this new, age-matched, control group (Supplementary Fig. 4) and found that the three-way interaction remained significant (F(4,128) = 2.62, p = 0.038, pes = 0.076) and with a similar effect size. Crucially, we also repeated the clustering procedure above without the 12 youngest (C1) patients and observed 100% concordance between the new cluster assignment and the one previously obtained on the full sample. Overall, these findings show that impaired contralesional performance under multitasking (and therefore assignment to the C2 cluster) is not entirely driven by age, education, or clinical variables such as lesion volume and time from stroke.
Finally, we highlight that only 3 out of 13 females in our sample (against 12 out of 33 males) were included in C2 (see Supplementary Table 1). We refrained from performing inferential statistics on this result considering the stark unbalance, but we note that this apparent asymmetry might warrant further exploration in future studies.
A continuous index of susceptibility to multitasking from rPCA
Three components in the rPCA solution accounted for 87.9% of the cumulative variance of the data (see components’ loadings in Supplementary Table 3). The first component (rPC1), in particular, explained 41.9% of the variance and loaded especially onto lateralized conditions (i.e., Contra- and Bi-lateral) but only under multitasking. The loadings for both dual tasks, ADT and VDT, were again very similar, further corroborating the amodal nature of multitasking-induced effects. We compared the values of this component between C1 (M = 0.65) and C2 (M = −1.34) to find that the two clusters significantly differed along this dimension (t(16.93) = 15.43, p < 0.001). We therefore retained this component for all analyses warranting the use of continuous measures alongside the information about the clustering.
The second (rPC2) and third (rPC3) components also accounted for an additional 23% of the variance each, and mostly loaded onto ipsilesional trials (rPC2) and trials belonging to the ST (rPC3). Thus, these last two components appeared to represent the “baseline” performance for the (main) effects of Type and Load. The three components were positively correlated, with values ranging from r = 0.32 to r = 0.58. Of these scores, only those of rPC3 significantly differed between C1 (mean = 0.40) and C2 (mean = −0.83) (t(14.39) = 3.38, p = 0.0043); note, however, that the correlation between rPC1 and rPC3 was r = 0.58, which indicates that the two constructs are somehow collinear and thus redundant. There was no difference between clusters in terms of rPC2 (t(15.87) = 1.59, p = 0.131).
Relationship between susceptibility to multitasking and neuropsychological assessment
The differences between clusters (t-tests), as well as the correlation between each variable and rPC1, are reported in detail in Table 1. The two clusters did not differ in terms of MMSE scores (N = 41, t(20.32) = 0.965, p = 0.346). They differed, instead, in their average performance at the neuropsychological tests assessing attention: C2 presented marginally lower scores with respect to C1 in the BIT (C2: 138.1 ± 4.27, C1: 141.9 ± 2.75) as well as in the Attentional Matrices test (C2: 37.13 ± 9.8, C1: 44.2 ± 10.1) that specifically assesses selective attention (although the effect did not survive FDR correction, see Table 1). However, all patients had scores within normal range in both tests; thus, multitasking revealed an otherwise undetected spatial attentional deficit. Most importantly, the susceptibility to multitasking shown by C2 patients is not a mere subtlety because the two clusters significantly differed in terms of functional evaluation of daily living activities. Indeed, C2 patients presented significantly higher scores (indicative of more severe deficits) in the KF-NAP55, assessing spatial neglect-like biases and difficulties in ecological situations, compared to C1 patients (C1: 2.15 ± 2.88, C2: 5.54 ± 4.8; N = 40, t(16.28) = 2.35, p = 0.032, pFDR = 0.06). All these neuropsychological tests were also significantly correlated with the first component obtained from the rPCA (though to a lesser extent for attentional matrices). Notably, the rPC1 showed a correlation of −0.54 with the KF-NAP score (t(38) = 3.93, p < 0.001, pFDR = 0.003). Finally, although cluster differences were comparatively smaller in this case, we found that rPC1 correlated with the scores of two tests evaluating reasoning and executive functions, i.e. the Raven’s progressive matrices, and the Modified Card Sorting Test, the latter for both category scores and, marginally, for perseveration errors.
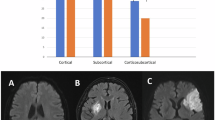
Multivariate analyses of lesion—and disconnection—symptom mapping
The majority of lesions, for both LHD and RHD patients, affected the insula, central opercular cortex, and putamen. The most affected tracts were the superior longitudinal fasciculus III (SLFIII), fronto-striatal fasciculus, cortico-pontine tract and corpus callosum for both LHD and RHD patients. In addition, the corticospinal tract appeared frequently disconnected by the right hemisphere lesions (see Fig. 4).
Multivariate brain-behavior mapping was carried out both on lesion and SDC maps (N = 40 patients, 27 for C1 and 13 for C2). We first assessed the potential role of covariates such as lesion volume, time from stroke onset, and age. Neither lesion volume (r = −0.2, t(38) = 1.26, p = 0.22) nor time from stroke onset (r = −0.11, t(38) = −0.66, p = 0.52) were significantly correlated with rPC1, and did not differ between clusters (t(19.43) = 1.09, p = 0.29 for lesion volume; t(29.47) = 0.38, p = 0.70 for time from stroke). This is remarkable in that lesion size has been classically considered a proxy for stroke severity and has been often found to correlate with behavioral deficits, though in interaction with mediator variables43,78. Age, on the other hand, was significantly associated with rPC1 (r = −0.46, t(38) = −3.48, p = 0.001) and did differ between clusters, as outlined in the paragraph above. Thus, these three variables were included in the BSR approach as predictors alongside the features obtained from the neuroimaging data (22 for lesion maps, 23 for SDC).
Lesion location
For lesion maps, the BSR approach selected a model including k = 5 predictors (PCs 3, 5, 7, 8 and 9), in addition to age and lesion volume as covariates (BIC = 104.4). This model was far superior to the null model (intercept-only: BIC = 119.3). Note that smaller values index better fit and a BIC difference of ten corresponds to posterior odds of about 150:179. When assessed using leave-one-out cross-validation, the model’s accuracy on left-out patients in terms of explained variance was R2 = 0.39, which is well aligned with state-of-the-art multivariate lesion-symptom mapping across behavioral domains46. When age and lesion volume were not in the pool of possible predictors, the modeling approach still selected k = 5 predictors (components 1, 5, 8, 9, and 14) and obtained a better fit than the null model (BIC = 109.6). Importantly, the cross-validated performance was very similar to that obtained with additional covariates (R2 = 0.36), showing that age alone was not driving the good model fit and performance.
Back-projection of the model coefficients to the atlas space for visualization (see Fig. 5) revealed that the right hemisphere voxels most predictive of susceptibility to multitasking corresponded to the frontal white matter (Z peak at [30, −4, 34]). Predictive locations extended then into the inferior frontal operculum, the insula, and precentral gyrus. This region included the most predictive voxels overall and had a symmetric counterpart (though with much smaller coefficients) in the left hemisphere ([−26, −6, 3]). Secondary clusters, associated with much smaller coefficients, were located in the thalamus (ventral lateral thalamus, [16, −12, 0]), and the medial aspect of the right superior frontal gyrus ([10, 28, 56]).
The figure depicts a glass brain projection, where red-yellow represents voxels predicting deficits while blue-green represents voxels predicting no deficit. To optimize the visualization, Z-normalized values in the range (−3, 3) are not displayed. Back-projected values associated with the deficit (Z > 3 for better visualization) are also rendered on a mosaic of 2D slices. The coordinates of axial [Z: 0 10 20 30 40 50 60] and coronal [Y: −30 −20 −15 −5 0 5 15] slices have been selected to highlight peaks in the Z-values.
While neglect following damage to frontal areas has been described before80,81,82, predictive voxels were generally more anterior with respect to the brain areas more often associated with stark symptoms, such as the inferior parietal lobule48,83,84. Here, the locations of predictive voxels were rather more in line with the involvement of a domain-general mechanism. In particular, the MD system has been previously associated with areas in the posterior part of the inferior frontal sulcus, in particular the frontal operculum and anterior insula33,85. Brain activations in the MD system have been associated with diverse cognitive demands and the assembly of many distinct subtasks33,86. Thus, one possibility is that impairments in this domain-general network may interact with or affect distant areas, among which those devoted to domain-specific (e.g., visuospatial) processes. This is in large agreement with recent evidence87 suggesting that disrupted anatomical connectivity of the MD system (as measured, for example, through indirect disconnections and as opposed to functional connectivity, measured with resting-state fMRI) predicted very well deficits in a range of diverse neuropsychological tests (e.g., the Trail-Making Test or the Stroop test), measuring different constructs but yet joined in their requiring a certain degree of cognitive control. Here, the most predictive location ([30, −4, 34]) corresponded very well to a recently described “white matter crossroad” ([28, −2, 26]) whose lesion jointly impacts distinct cognitive domains (e.g., attention, alertness, inhibition)35. Note that these frontal white matter voxels are intersected by many tracts, which further motivates the use of disconnectome-based analyses presented in the next section to properly assess their contribution to the deficit. However, we binarized the peak values (z > 12) in the map and fed the mask to the Tractotron software (part of the BCBtoolkit65) to identify the underlying white matter tracts. Six tracts were associated with a disconnection probability ≥0.95: the right Corticospinal tract, the right Superior Longitudinal Fasciculus (SLF, segments II and III), the right Frontal Aslant tract (FAT), the right Anterior Arcuate Fasciculus (AAF), and the Corpus Callosum. Of these tracts, four (SLFII, SLFIII, FAT, AAF) have been previously identified as white matter tracts connecting brain regions in the MD system40,88.
Structural disconnections
For SDC maps, the BSR approach selected a model with k = 3 predictors (PCs 2, 3 and 20) and age as a covariate (BIC = 104.7), which was superior to the null model (intercept-only; BIC = 119.3). The cross-validated accuracy on left-out patients was R2 = 0.39. When age was not in the pool, performance in cross-validation was slightly worse (R2 = 0.24), although in face of a relatively good model fit with k = 3 predictors (PCs 1, 2, and 20; BIC = 112.4).
The predictive map obtained by back-projecting the model coefficients is displayed in Fig. 6. Susceptibility to multitasking was associated with widespread damage to the right and left anterior thalamic radiation (ATR) and right SLF II. The analysis also highlighted an important role of interhemispheric disconnection, in that predictive voxels extended to the opposite hemisphere through substantial involvement of the corpus callosum and frontal commissure. Note that the ATR has been previously linked to individual differences in multitasking ability in healthy individuals86. SLF II has been implicated in spatial awareness before89,90 as, if damaged, it predicts well the presence of spatial neglect. The latter disconnection seems to reconcile with the fact that lesion location does not suggest the involvement of domain-specific areas such as those subserving visuo-spatial attention, which might nonetheless become dysfunctional due to their connectivity with regions in frontal areas subserving domain general processes that are relevant for multitasking or cognitive control87.
The figure depicts a glass brain projection, where red-yellow represents tracts predicting deficits while blue-green represents tracts predicting no deficit. To optimize the visualization, Z-normalized values in the range (−3, 3) are not displayed. Back-projected values associated with the deficit (Z > 3 for better visualization) are also rendered on a mosaic of 2D slices. The coordinates of axial [Z: −12 −8 5 15 20 30 35] and coronal [Y: −45 −35 −25 −10 −3 2 10] slices have been selected to highlight peaks in the Z-values.
Discussion
In this study, we enrolled patients with first-ever subacute or chronic stroke who performed well within normal limits in a widely used paper-and-pencil neuropsychological battery for the assessment of visuospatial neglect45. When administered with a computerized task tapping onto spatial monitoring performance, both in isolation and under conditions of concurrent task demands (i.e., multitasking), patients split into two very distinct behavioral phenotypes. Two-thirds of the patients (67%) performed the spatial monitoring task with near-ceiling accuracy, irrespective of target side (ipsilesional vs contralesional) and of the increasing attentional load in the multitasking condition. The remaining third of the patients (33%), however, deviated from the latter pattern to such an extent that they were assigned to a separate group by a multivariate clustering algorithm. This second cluster of patients (C2) was indeed impaired in the spatial monitoring task, but not in a generalized and unspecific way. In this group, performance in ipsilesional trials was always near-ceiling and even the detection of contralesional targets (for contralesional and bilateral trials) was relatively spared when spatial monitoring was the only task (i.e., the baseline, single task condition). This indicates relative absence of lateralized deficits (either neglect or extinction) in a condition of low attentional load, which fits well with the neuropsychological assessment. Performance deteriorated sharply, however, when concurrent task demands were introduced, irrespective of whether the second task loaded onto the same (i.e., VDT) or a different sensory modality (i.e., ADT).
The current study has some limitations that are worth stressing. First, the sample was extremely heterogeneous with respect to time from stroke, which is due to the characteristics of the hospital in which patients were admitted for stroke rehabilitation. As an important reassurance in this regard, we note that this variable did not differ between the clusters and did not correlate with rPC1. Second, while the sample was relatively large, the results should nonetheless be interpreted with caution, especially for what concerns the correlations with clinical tests and neuroimaging data. All things considered, however, the finding of a behavioral phenotype characterized by high susceptibility to multitasking substantiates and qualifies previous small-scale studies suggesting that computerized tasks, especially when involving dual-tasking, can unveil subtle lateralized deficits of visuospatial attention9,11. A context in which attentional resources are limited is particularly prone to reveal any underlying bias, if present, whereas standard conditions may not have sufficient sensitivity and may allow patients to fully compensate for it7,8. Successful compensation for a deficit is a clinically-relevant, desirable feature, and may indicate that sufficient cognitive resources can be recruited when needed to overcome everyday life challenges and difficulties. However, this condition may be fragile, as for a substantial share of patients these resources may be limited and rigidly capped. Hence, assessing susceptibility to multitasking allows one to objectively quantify the extent by which these patients would struggle in more taxing conditions, thereby enhancing our understanding of their needs. In other words, it enables us to better characterize what marks the passage to stark stroke’s sequelae, namely the buffer zone in which brain damage can or cannot result in significant deficits, depending on a wealth of contextual factors. Finally, it may inform treatment, in that patients within this gray area may benefit the most from cognitive training aimed at fostering general cognitive resources.
Our main task leverages on a classic visual detection paradigm for visual extinction and spatial neglect44, i.e. the inability to orient attention toward or respond to stimuli presented in the contralesional hemisphere83,91. However, it would be questionable to classify C2 patients as having spatial neglect, first and foremost because they all performed well above the clinical cut-off in established diagnostic tests (i.e., the BIT). It is true that, on average, C2 patients performed worse in tests that measure neglect in everyday life situations (i.e., the KF-NAP), which are regarded as particularly sensitive to neglect35,55,92. However, there is no strict correspondence between cluster assignment and neglect at the KF-NAP, as revealed by the fact that 12 out of 22 patients showing deficit at the KF-NAP (score >0) were included in C1 by the clustering procedure. It is also true, however, that C2 presents many core features of spatial neglect, though on a different scale. For example, spatial neglect is considered a rather heterogeneous syndrome in which core lateralized (i.e., spatial) biases coexist and interact with non-lateralized deficits75. This picture is very well captured by patients in C2: they show a marked lateralized bias (i.e., the difference in performance between Ipsilesional and Contralesional/Bilateral trials) when concurrently engaged by non-spatial demands. This suggests that the difference between C2 and patients with clinically-confirmed spatial neglect may be quantitative rather than qualitative in nature: in other words, a subtle lateralized bias is a distinctive feature of this group, and part of the equation delineated by susceptibility to multitasking. This has, in turn, important consequences. First, based on the results of paper-and-pencil clinical tests, all patients (both C1 and C2) would be considered as a control group (i.e., N−) for patients with overt lateralized spatial deficits (i.e., N+). Equating the two clusters as both “spared” control groups may lead to a loss of potentially relevant information. Specifically, neuropsychological and neuroimaging studies may overlook the clinical picture and neural correlates of patients in C2, thus failing to capture the full extent of spatial neglect manifestations. Second, an in-depth description of C2 may provide hints about the clinical characteristics of patients who are at the prodromal boundary of spatial awareness disorders, and possibly any other deficit, given that attentional load similarly affects several diverse domains23,24. This is not trivial because, as a matter of fact, patients in C2 may experience higher than normal functional difficulties in everyday life situations, as mentioned before and as suggested by the higher scores (i.e., worse performance) of this group in the test evaluating activities of daily living (i.e., KF-NAP). Thus, susceptibility to multitasking better captures the difficulties that may arise in everyday life, ecological situations. Ecological tests are indeed regarded as more sensitive to the presence of neglect, though their administration is not always feasible. Therefore, introducing multitasking to computer-based tests may provide an effective compromise.
One of the intriguing results of this study is that high susceptibility to multitasking was not correlated with the size of the brain lesion. Lesion volume is an established proxy for stroke severity, and has been suggested to correlate with most deficits, although in interaction with mediator variables43,78. The lack of correlation with the main deficits of patients in C2 may question that they stem from a unitary construct. There was, on the other hand, an association between the latent factor indexing susceptibility to multitasking (rPC1) and patients’ age, which has been often taken, instead, as a proxy for brain reserve, chiefly because it is negatively associated with brain plasticity43. Older patients were more likely to present high susceptibility to multitasking, even in spite of similar lesion size. This is not entirely surprising considering that dual tasking performance (at least in terms of latency measures) declines in healthy ageing93. However, while patients’ difficulties may be graded and continuous in nature, this has not a continuous counterpart in terms of objective brain damage, at least in this study. While the volume of brain damage does not seem to play a substantial role, multivariate lesion-symptom mapping linked susceptibility to multitasking to specific lesion locations and structural disconnections. We start by noting, first, that we did not observe a significantly different prevalence of high susceptibility to multitasking in patients with LHD vs. RHD. This may be surprising, in that disorders of spatial awareness are thought to be more common following lesion of the right hemisphere94,95, on the one hand, and because cognitive reserve may also be lateralized in the right hemisphere41, on the other hand. Moreover, as pointed out by De Renzi94, studies in which LHD and RHD are compared typically suffer a common selection bias: if only LHD patients with sufficiently spared language abilities are enrolled, in order for them to properly understand the experimental tasks, these patients will necessarily present, on average, milder stroke sequelae, and will generally perform better. However, we did not observe differences in this direction in the current study. Part of the reason is that our computerized task can be administered also to a population of patients with variable degree of language impairments9. Another possible explanation for this finding may be insufficient statistical power due to the different size of the groups (17 LHD vs. 29 RHD). Besides hemispheric asymmetries, however, multivariate lesion-symptom mapping did highlight the neural correlates of high susceptibility to multitasking in both hemispheres, suggesting that this construct may not necessarily be strongly lateralized.
The areas most predictive of susceptibility to multitasking were located in the frontal white matter, both for RHD and LHD patients, and extended to the frontal operculum and insula. Thus, the lesions associated with visuospatial bias under multitasking (i.e., the pattern shown by C2 patients) did not fully match those typically associated with spatial neglect. This is not entirely surprising. While differences between C2 and clinically-confirmed spatial neglect may be only quantitative in nature, more extended lesions reaching, posteriorly, the inferior parietal lobe may be more likely to cause stark symptoms. There were no stark symptoms in our sample of patients, as per our selection criteria. Rather, C2-like patients are more likely to have been included in the control groups when assessing neglect, which may have led to overlook these frontal sites in most lesion-symptom mapping studies. The bilateral frontal operculum and anterior insula (together with bilateral dPMC, bilateral anterior IPS, left inferior frontal sulcus, and left inferior frontal gyrus) characterize the distinctive activation profile of dual tasking according to a recent meta-analysis31. These areas have been previously associated with several different tasks, spanning diverse cognitive functions, and may thus be regarded as an abstract, higher order, and multi-purpose system, known as the Multiple-Demand network33, subtending overall cognitive functioning. For example, this network may provide the basis for cognitive control87, or the assembly and timing of specific subtasks33,85, all aspects that are independent, but closely related to the concept of fluid intelligence86. The MD system has been previously described in subcortical and cortical parietal and frontal areas, including the frontal operculum and the anterior insula85, thereby closely mirroring what was predictive of susceptibility to multitasking in the present study. It is therefore possible that structural damage to these regions would affect multitasking conditions more notably, which is precisely the main behavioral feature of C2. While this can nicely explain pure multitasking deficits, however, it still does not account for the full picture consisting of both a multitasking deficit and a concurrent spatial one. In this regard, the analysis of structural disconnections provides complementary and crucial information. White matter damage involving the ATR, anterior commissure, as well as fronto-parietal disconnections along SLF II were the most predictive of behavioral deficits. The ATR joins cortical (prefrontal) and subcortical areas, most notably the hippocampal formation, thalamus, and striatum96, subserving thus multiple tasks and functions97,98. Few studies have implied a role of the ATR in strategic processes, overall processing speed, and/or executive functions98; Kievit et al. 86 found that the ATR integrity predicted age-related differences in multitasking ability. Overall, the ATR presents substantial connectivity with the prefrontal components of the MD system86, and thus its involvement is not entirely surprising given the most predictive lesions of susceptibility to multitasking, i.e., within the MD system itself. SLF II, on the other hand, is known to be implicated in spatial awareness89,90 as, if damaged, it predicts the presence of spatial neglect. SLF II originates from the posterolateral parietal lobe, including the angular gyrus, runs through the middle frontal gyrus, and ends within the dorsolateral prefrontal cortex99. Thus, the analysis of structural disconnections seems to reconcile the fact that the lesions of C2 were located in the frontal cortex, as opposed to areas more strongly tied to spatial processes such as those in the inferior parietal lobe: suboptimal communication between them caused by structural disconnection, which cannot be fully captured by lesion maps, may be ultimately responsible for the detrimental effects of multitasking on spatial attention. This would be in line with a recent study showing that lesions affecting the connectivity within the MD system, very similar to what described here, lead to impairments in multiple aspects of attention that are traditionally considered relatively independent (e.g., visuo-spatial attention vs. alertness or executive control), corroborating the notion that these aspects closely interact and that a higher order factor may be the joining link35. The study by Kaufmann et al.35 is particularly relevant since it additionally shows that lesions to this network are associated with difficulties in daily life activities. One important point to stress, however, is that damage to the MD system, albeit pervasive, should not be necessarily regarded as an alternative definition of “global impairment”. For example, the performance in ipsilesional trials of C2 patients was, even under multitasking, rather good, their deficits being limited to few critical conditions as defined by their underlying spatial awareness bias (contralesional or bilateral trials). Selective impairments, limited to specific domains or conditions, require a different explanation than a global deficit, and probably distinct lesion patterns. One possibility is that the presence of an underlying “dormant” deficit may be necessary, as the disruption of the communication between candidate areas (one domain-general, one domain-specific). For this, future studies should probe the generalizability of susceptibility to multitasking to different measures (i.e., beyond spatial awareness). Another thrilling perspective is to research alternative operationalizations of “susceptibility to multitasking”. While multitasking is an inherently dichotomous concept—one either performs one task at once, or more than one—the notion of cognitive load can be parametrized100,101.Thus, a range of psychophysical, adaptive, or machine-learning procedures can be exploited to define multitasking as an objective distraction threshold which, once surpassed, results in stark performance deficits on a given primary task.
In summary, computerized paradigms exploiting multitasking can detect subtle deficits even in seemingly spared, chronic stroke patients. These paradigms leverage on our state-of-the-art knowledge of the brain’s functions and limitations, and can be reliably administered even in very short, quick formats (e.g., 10 min). More importantly, they better capture the difficulties of patients in daily life activities, where multitasking is ubiquitous. Individual susceptibility to multitasking as a construct has the promising potential to provide us a better understanding of what marks the passage, after brain damage, to clinically visible deficits, hence advancing our knowledge of the impact of stroke and tailoring patient-specific options for treatment.
Data availability
The conditions of our ethics approval do not permit the public archiving of clinical and neuroimaging data of individual patients. Z-maps from multivariate lesion and disconnection analyses, lesion and disconnection overlays, and aggregated data from the computerized behavioral task are available at https://github.com/CCNL-UniPD/Multitasking.
Code availability
E-Prime code of the computerized task and MRIcroGL python scripts used to display the brain maps is available at https://github.com/CCNL-UniPD/Multitasking.
References
Donkor, E. S. Stroke in the 21st century: a snapshot of the burden, epidemiology, and quality of life. Stroke Res. Treat. 2018, 3238165 (2018).
Corbetta, M. et al. Common behavioral clusters and subcortical anatomy in stroke. Neuron 85, 927–941 (2015).
D’Imperio, D. et al. Sensorimotor, attentional, and neuroanatomical predictors of upper limb motor deficits and rehabilitation outcome after stroke. Neural Plast. 2021, e8845685 (2021).
Ramsey, L. E. et al. Behavioural clusters and predictors of performance during recovery from stroke. Nat. Hum. Behav. 1, 1–10 (2017).
Howard, G. & Goff, D. C. Population shifts and the future of stroke: forecasts of the future burden of stroke. Ann. N.Y. Acad. Sci. 1268, 14–20 (2012).
Wafa, H. A. et al. Burden of stroke in Europe. Stroke 51, 2418–2427 (2020).
Bonato, M. & Deouell, L. Hemispatial neglect: computer-based testing allows more sensitive quantification of attentional disorders and recovery and might lead to better evaluation of rehabilitation. Front. Hum. Neurosci. 7, (2013).
Bonato, M., Priftis, K., Umiltà, C. & Zorzi, M. Computer-based testing unveils severe neglect in apparently intact patients. Behav. Neurol. https://doi.org/10.3233/BEN-2012-129005 (2012).
Blini, E. et al. Multi-tasking uncovers right spatial neglect and extinction in chronic left-hemisphere stroke patients. Neuropsychologia 92, 147–157 (2016).
Bonato, M. et al. Ipsilesional impairments of visual awareness after right-hemispheric stroke. Front. Psychol. 10 (2019).
Bonato, M., Priftis, K., Marenzi, R., Umiltà, C. & Zorzi, M. Increased attentional demands impair contralesional space awareness following stroke. Neuropsychologia 48, 3934–3940 (2010).
Marois, R. & Ivanoff, J. Capacity limits of information processing in the brain. Trends Cogn. Sci. 9, 296–305 (2005).
Shapiro, K. L. & Raymond, J. E. Temporal Allocation of Visual Attention: Inhibition or Interference? (Academic Press, 1994).
Webster, R. G. & Haslerud, G. M. Influence on extreme peripheral vision of attention to a visual or auditory task. J. Exp. Psychol. 68, 269 (1964).
Lavie, N., Hirst, A., de Fockert, J. W. & Viding, E. Load theory of selective attention and cognitive control. J. Exp. Psychol: Gen. 133, 339 (2004).
Driver, J. A selective review of selective attention research from the past century. Br. J. Psychol. 92, 53–78 (2001).
Rauss, K. S., Pourtois, G., Vuilleumier, P. & Schwartz, S. Attentional load modifies early activity in human primary visual cortex. Hum. Brain Mapp. 30, 1723–1733 (2009).
Vuilleumier, P. et al. Abnormal attentional modulation of retinotopic cortex in parietal patients with spatial neglect. Curr. Biol. 18, 1525–1529 (2008).
Emrich, S. M., Burianová, H. & Ferber, S. Transient perceptual neglect: Visual working memory load affects conscious object processing. J. Cogn. Neurosci. 23, 2968–2982 (2011).
Shulman, G. L. et al. Quantitative analysis of attention and detection signals during visual search. J. Neurophysiol. 90, 3384–3397 (2003).
Todd, J. J., Fougnie, D. & Marois, R. Visual short-term memory load suppresses temporo-parietal junction activity and induces inattentional blindness. Psychol. Sci. 16, 965–972 (2005).
Yang, L. et al. Psychometric properties of dual-task balance and walking assessments for individuals with neurological conditions: a systematic review. Gait Posture 52, 110–123 (2017).
Mancioppi, G. et al. Innovative motor and cognitive dual-task approaches combining upper and lower limbs may improve dementia early detection. Sci. Rep. 11, 7449 (2021).
Nascimbeni, A., Gaffuri, A., Penno, A. & Tavoni, M. Dual task interference during gait in patients with unilateral vestibular disorders. J. Neuroeng. Rehabil. 7, 47 (2010).
Andres, M. et al. Increased cognitive load reveals unilateral neglect and altitudinal extinction in chronic stroke. J. Int. Neuropsychol. Soc. 25, 644–653 (2019).
Ciricugno, A., Bartlett, M. L., Gwinn, O. S., Carragher, D. J. & Nicholls, M. E. R. The effect of cognitive load on horizontal and vertical spatial asymmetries. Laterality 26, 706–724 (2021).
Dodds, C. M. et al. The effects of time-on-task and concurrent cognitive load on normal visuospatial bias. Neuropsychology 22, 545–552 (2008).
Saccani, M. S., Contemori, G., Corolli, C. & Bonato, M. Transforming a concept in a tool: diagnostic and prognostic value of tasks depleting cognitive resources. Front. Psychol. 12, (2022).
Burgess, P. W., Veitch, E., de Lacy Costello, A. & Shallice, T. The cognitive and neuroanatomical correlates of multitasking. Neuropsychologia 38, 848–863 (2000).
Shallice, T. & Burgess, P. W. Deficits in strategy application following frontal lobe damage in man. Brain 114, 727–741 (1991).
Worringer, B. et al. Common and distinct neural correlates of dual-tasking and task-switching: a meta-analytic review and a neuro-cognitive processing model of human multitasking. Brain Struct. Funct. 224, 1845–1869 (2019).
Watanabe, K. & Funahashi, S. Toward an understanding of the neural mechanisms underlying dual-task performance: Contribution of comparative approaches using animal models. Neurosci. Biobehav. Rev. 84, 12–28 (2018).
Duncan, J. The multiple-demand (MD) system of the primate brain: mental programs for intelligent behaviour. Trends Cogn. Sci. 14, 172–179 (2010).
Adcock, R. A., Constable, R. T., Gore, J. C. & Goldman-Rakic, P. S. Functional neuroanatomy of executive processes involved in dual-task performance. Proc. Natl. Acad. Sci. USA 97, 3567–3572 (2000).
Kaufmann, B. C. et al. Joint impact on attention, alertness and inhibition of lesions at a frontal white matter crossroad. Brain 146, 1467–1482 (2023).
Deprez, S. et al. The functional neuroanatomy of multitasking: combining dual tasking with a short term memory task. Neuropsychologia 51, 2251–2260 (2013).
Leone, C. et al. Cognitive-motor dual-task interference: a systematic review of neural correlates. Neurosci. Biobehav. Rev. 75, 348–360 (2017).
Fedorenko, E., Duncan, J. & Kanwisher, N. Broad domain generality in focal regions of frontal and parietal cortex. Proc. Natl. Acad. Sci. USA 110, 16616–16621 (2013).
Woolgar, A., Duncan, J., Manes, F. & Fedorenko, E. The multiple-demand system but not the language system supports fluid intelligence. Nat. Hum. Behav. 2, 200–204 (2018).
Chen, P. Y., Chen, C. L., Hsu, Y. C. & Tseng, W. Y. I. Fluid intelligence is associated with cortical volume and white matter tract integrity within multiple-demand system across adult lifespan. Neuroimage 212, 116576 (2020).
Robertson, I. H. A right hemisphere role in cognitive reserve. Neurobiol. Aging 35, 1375–1385 (2014).
Stern, Y. What is cognitive reserve? Theory and research application of the reserve concept. J. Int. Neuropsychol. Soc. 8, 448–460 (2002).
Umarova, R. M. et al. Interaction between cognitive reserve and age moderates effect of lesion load on stroke outcome. Sci. Rep. 11, 4478 (2021).
Làdavas, E. Selective spatial attention in patients with visual extinction. Brain 113, 1527–1538 (1990).
Wilson, B., Cockburn, J. & Halligan, P. W. The Behavioural Inattention Test. Bury St. Edmunds, UK: Thames Valley Test Company. (1987).
Salvalaggio, A., De Filippo De Grazia, M., Zorzi, M., Thiebaut de Schotten, M. & Corbetta, M. Post-stroke deficit prediction from lesion and indirect structural and functional disconnection. Brain 143, 2173–2188 (2020).
Karnath, H.-O. & Rorden, C. The anatomy of spatial neglect. Neuropsychologia 50, 1010–1017 (2012).
Vallar, G. & Perani, D. The anatomy of unilateral neglect after right-hemisphere stroke lesions. A clinical/CT-scan correlation study in man. Neuropsychologia 24, 609–622 (1986).
Oldfield, R. C. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia 9, 97–113 (1971).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198 (1975).
Carlesimo, G. A., Caltagirone, C. & Gainotti, G. The Mental Deterioration Battery: normative data, diagnostic reliability and qualitative analyses of cognitive impairment. The group for the standardization of the mental deterioration battery. Eur. Neurol. 36, 378–384 (1996).
Spinnler, H. & Tognoni, G. Gruppo italiano per lo studio neuropsicologico dell’invecchiamento. Standardizzazione e taratura italiana di test neuropsicologici. Ital. J. Neurol. Sci. 6, 1–120 (1987).
Nelson, H. E. A modified card sorting test sensitive to frontal lobe defects. Cortex 12, 313–324 (1976).
Caffarra, P., Vezzadini, G., Dieci, F., Zonato, F. & Venneri, A. Rey-Osterrieth complex figure: normative values in an Italian population sample. Neurol. Sci. 22, 443–447 (2002).
Chen, P., Chen, C. C., Hreha, K., Goedert, K. M. & Barrett, A. M. Kessler foundation neglect assessment process uniquely measures spatial neglect during activities of daily living. Arch. Phys. Med. Rehabil. 96, 869–876.e1 (2015).
Chen, P., Hreha, K., Fortis, P., Goedert, K. M. & Barrett, A. M. Functional assessment of spatial neglect: a review of the catherine bergego scale and an introduction of the Kessler foundation neglect assessment process. Top. Stroke Rehabil. 19, 423–435 (2012).
Luzzatti, C., Willmes, K. & De Bleser, R. Aachener aphasie test. Versione Italiana (1996).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple hypothesis testing. J. R. Stat. Soc. B 57, 289–300 (1995).
Hendrickson, A. E. & White, P. O. Promax: a quick method for rotation to oblique simple structure. Br. J. Stat. Psychol. 17, 65–70 (1964).
Bisogno, A. L. et al. A low-dimensional structure of neurological impairment in stroke. Brain Commun. 3, fcab119 (2021).
Santos, N. C. et al. Exploring the factor structure of neurocognitive measures in older individuals. PLoS ONE 10, e0124229 (2015).
Blini, E., Arrighi, R. & Anobile, G. Pupillary manifolds: uncovering the latent geometrical structures behind phasic changes in pupil size. Sci. Rep. 14, 27306 (2024).
Pustina, D. et al. Automated segmentation of chronic stroke lesions using LINDA: lesion identification with neighborhood data analysis. Hum. Brain Mapp. 37, 1405–1421 (2016).
Yushkevich, P. A. et al. User-guided segmentation of multi-modality medical imaging datasets with ITK-SNAP. Neuroinformation 17, 83–102 (2019).
Foulon, C. et al. Advanced lesion symptom mapping analyses and implementation as BCBtoolkit. Gigascience 7, 1–17 (2018).
Nachev, P., Coulthard, E., Jäger, H. R., Kennard, C. & Husain, M. Enantiomorphic normalization of focally lesioned brains. NeuroImage 39, 1215–1226 (2008).
Tustison, N. J. et al. The ANTsX ecosystem for quantitative biological and medical imaging. Sci. Rep. 11, 9068 (2021).
Biesbroek, J. M. et al. Brain infarct segmentation and registration on MRI or CT for lesion-symptom mapping. J. Vis. Exp. e59653. https://doi.org/10.3791/59653 (2019).
Rorden, C., Bonilha, L., Fridriksson, J., Bender, B. & Karnath, H.-O. Age-specific CT and MRI templates for spatial normalization. Neuroimage 61, 957–965 (2012).
Thiebaut de Schotten, M., Foulon, C. & Nachev, P. Brain disconnections link structural connectivity with function and behaviour. Nat. Commun. 11, 5094 (2020).
Siegel, J. S. et al. Disruptions of network connectivity predict impairment in multiple behavioral domains after stroke. PNAS 113, E4367–E4376 (2016).
Zorzi, M., De Filippo De Grazia, M., Blini, E. & Testolin, A. Assessment of machine learning pipelines for prediction of behavioral deficits from brain disconnectomes. In Brain Informatics (eds. Mahmud, M., Kaiser, M. S., Vassanelli, S., Dai, Q. & Zhong, N.) 211–222. https://doi.org/10.1007/978-3-030-86993-9_20 (Springer International Publishing, 2021).
Wiesen, D., Sperber, C., Yourganov, G., Rorden, C. & Karnath, H.-O. Using machine learning-based lesion behavior mapping to identify anatomical networks of cognitive dysfunction: spatial neglect and attention. NeuroImage 201, 116000 (2019).
Rorden, C. & Brett, M. Stereotaxic display of brain lesions. Behav. Neurol. 12, 191–200 (2000).
Forkel, S. J. et al. Anatomical evidence of an indirect pathway for word repetition. Neurology 94, e594–e606 (2020).
Rolls, E. T., Huang, C.-C., Lin, C.-P., Feng, J. & Joliot, M. Automated anatomical labelling atlas 3. NeuroImage 206, 116189 (2020).
Rojkova, K. et al. Atlasing the frontal lobe connections and their variability due to age and education: a spherical deconvolution tractography study. Brain Struct. Funct. 221, 1751–1766 (2016).
Sperber, C. The strange role of brain lesion size in cognitive neuropsychology. Cortex 146, 216–226 (2022).
Raftery, A. E. Bayesian model selection in social research. Sociol. Methodol. 25, 111–163 (1995).
Husain, M. & Kennard, C. Distractor-dependent frontal neglect. Neuropsychologia 35, 829–841 (1997).
He, B. J. et al. Breakdown of functional connectivity in frontoparietal networks underlies behavioral deficits in spatial neglect. Neuron 53, 905–918 (2007).
Mesulam, M.-M. Spatial attention and neglect: parietal, frontal and cingulate contributions to the mental representation and attentional targeting of salient extrapersonal events. Philos. Trans. R. Soc. Lond. B 354, 1325–1346 (1999).
Vallar, G. Spatial hemineglect in humans. Trends Cogn. Sci. 2, 87–97 (1998).
Fierro, B. et al. Contralateral neglect induced by right posterior parietal rTMS in healthy subjects. NeuroReport 11, 1519–1521 (2000).
Assem, M., Glasser, M. F., Van Essen, D. C. & Duncan, J. A domain-general cognitive core defined in multimodally parcellated human cortex. Cereb. Cortex 30, 4361–4380 (2020).
Kievit, R. A. et al. Distinct aspects of frontal lobe structure mediate age-related differences in fluid intelligence and multitasking. Nat. Commun. 5, 5658 (2014).
Jiang, J., Bruss, J., Lee, W.-T., Tranel, D. & Boes, A. D. White matter disconnection of left multiple demand network is associated with post-lesion deficits in cognitive control. Nat. Commun. 14, 1740 (2023).
Karadachka, K. et al. Structural connectivity of the multiple demand network in humans and comparison to the macaque brain. Cereb. Cortex 33, 10959–10971 (2023).
Karnath, H.-O., Rorden, C. & Ticini, L. F. Damage to white matter fiber tracts in acute spatial neglect. Cereb. Cortex 19, 2331–2337 (2009).
Thiebaut de Schotten, M. et al. Damage to white matter pathways in subacute and chronic spatial neglect: a group study and 2 single-case studies with complete virtual “in vivo” tractography dissection. Cereb. Cortex 24, 691–706 (2014).
Rode, G., Pagliari, C., Huchon, L., Rossetti, Y. & Pisella, L. Semiology of neglect: an update. Ann. Phys. Rehabil. Med. 60, 177–185 (2017).
Pitteri, M. et al. Conventional and functional assessment of spatial neglect: clinical practice suggestions. Neuropsychology 32, 835–842 (2018).
Verhaeghen, P., Steitz, D. W., Sliwinski, M. J. & Cerella, J. Aging and dual-task performance: a meta-analysis. Psychol. Aging 18, 443–460 (2003).
De Renzi, E. Disorders of Space Exploration and Cognition (John Wiley & Sons, Inc., 1982).
Beis, J.-M. et al. Right spatial neglect after left hemisphere stroke: qualitative and quantitative study. Neurology 63, 1600–1605 (2004).
Behrens, T. E. J. et al. Non-invasive mapping of connections between human thalamus and cortex using diffusion imaging. Nat. Neurosci. 6, 750–757 (2003).
Jankowski, M. M. et al. The anterior thalamus provides a subcortical circuit supporting memory and spatial navigation. Front. Syst. Neurosci. 7, 45 (2013).
Duering, M. et al. Strategic role of frontal white matter tracts in vascular cognitive impairment: a voxel-based lesion-symptom mapping study in CADASIL. Brain 134, 2366–2375 (2011).
Chang, E. F., Raygor, K. P. & Berger, M. S. Contemporary model of language organization: an overview for neurosurgeons. J. Neurosurg. 122, 250–261 (2015).
Lisi, M., Bonato, M. & Zorzi, M. Pupil dilation reveals top–down attentional load during spatial monitoring. Biol. Psychol. 112, 39–45 (2015).
Bonato, M. Unveiling residual, spontaneous recovery from subtle hemispatial neglect three years after stroke. Front. Hum. Neurosci. 9, 413 (2015).
Acknowledgements
We are grateful to all the patients who took part in our study. We would also like to thank the clinical team at IRCCS San Camillo Hospital for assistance and support. This study was supported by grants from the Italian Ministry of Health (RF-2013-02359306 to M.Z. and Ricerca Corrente to IRCCS Ospedale San Camillo).
Author information
Authors and Affiliations
Contributions
Elvio Blini: Conceptualization, Methodology, Software, Formal Analysis, Data Curation, Writing – Original draft, Writing – Review and Editing, Visualization. Daniela d’Imperio: Conceptualization, Methodology, Investigation, Data Curation, Writing – Original draft, Writing – Review and Editing, Project Administration. Zaira Romeo: Conceptualization, Methodology, Investigation, Data Curation, Writing – Review and Editing, Project Administration. Michele de Filippo de Grazia: Software, Data Curation, Writing – Review and Editing. Laura Passarini: Resources, Writing – Review and Editing. Cristina Pilosio: Resources, Writing – Review and Editing. Francesca Meneghello: Resources, Writing – Review and Editing, Supervision, Project Administration. Mario Bonato: Conceptualization, Methodology, Writing – Review and Editing. Marco Zorzi: Conceptualization, Methodology, Formal Analysis, Resources, Data Curation, Writing – Review and Editing, Visualization, Supervision, Project Administration, Funding Acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors report no competing interests.
Peer review
Peer review information
Communications Biology thanks Chris Foulon and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Benjamin Bessieres. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Blini, E., D’Imperio, D., Romeo, Z. et al. Susceptibility to multitasking in stroke is associated to multiple-demand system damage and leads to lateralized visuospatial deficits. Commun Biol 8, 734 (2025). https://doi.org/10.1038/s42003-025-08074-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s42003-025-08074-z