Abstract
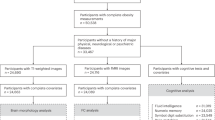
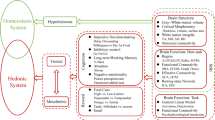
Obesity is often associated with a chronic, low-grade inflammatory state affecting the entire body. This sustained inflammatory state disrupts the coordinated communication between the periphery and the brain, which has a crucial role in maintaining homeostasis through humoural, nutrient-mediated, immune and nervous signalling pathways. The inflammatory changes induced by obesity specifically affect communication interfaces, including the blood–brain barrier, glymphatic system and meninges. Consequently, brain areas near the third ventricle, including the hypothalamus and other cognition-relevant regions, become susceptible to impairments, resulting in energy homeostasis dysregulation and an elevated risk of cognitive impairments such as Alzheimer’s disease and dementia. This Review explores the intricate communication between the brain and the periphery, highlighting the effect of obesity-induced inflammation on brain function.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Ellulu, M. S., Patimah, I., Khaza’ai, H., Rahmat, A. & Abed, Y. Obesity and inflammation: the linking mechanism and the complications. Arch. Med Sci. 13, 851–863 (2017).
Ugalde-Muniz, P., Fetter-Pruneda, I., Navarro, L., Garcia, E. & Chavarria, A. Chronic systemic inflammation exacerbates neurotoxicity in a Parkinson’s disease model. Oxid. Med. Cell Longev. 2020, 4807179 (2020).
Guillemot-Legris, O. & Muccioli, G. G. Obesity-induced neuroinflammation: beyond the hypothalamus. Trends Neurosci. 40, 237–253 (2017).
Jais, A. & Bruning, J. C. Hypothalamic inflammation in obesity and metabolic disease. J. Clin. Invest. 127, 24–32 (2017).
Gomez-Apo, E., Mondragon-Maya, A., Ferrari-Diaz, M. & Silva-Pereyra, J. Structural brain changes associated with overweight and obesity. J. Obes. 2021, 6613385 (2021).
Xie, J., Van Hoecke, L. & Vandenbroucke, R. E. The impact of systemic inflammation on Alzheimer’s disease pathology. Front. Immunol. 12, 796867 (2021).
de Oliveira, J. et al. Inflammatory cascade in Alzheimer’s disease pathogenesis: a review of experimental findings. Cells 10, 2581 (2021).
Banks, W. A. The blood–brain barrier as an endocrine tissue. Nat. Rev. Endocrinol. 15, 444–455 (2019).
Rhea, E. M. et al. Blood–brain barriers in obesity. AAPS J. 19, 921–930 (2017).
Dror, E. et al. Postprandial macrophage-derived IL-1beta stimulates insulin, and both synergistically promote glucose disposal and inflammation. Nat. Immunol. 18, 283–292 (2017).
Zhang, Y. et al. Positional cloning of the mouse obese gene and its human homologue. Nature 372, 425–432 (1994).
Halaas, J. L. et al. Weight-reducing effects of the plasma protein encoded by the obese gene. Science 269, 543–546 (1995).
Friedman, J. M. Leptin and the endocrine control of energy balance. Nat. Metab. 1, 754–764 (2019).
Li, M. et al. Trends in insulin resistance: insights into mechanisms and therapeutic strategy. Signal Transduct. Target. Ther. 7, 216 (2022).
Butterworth, R. F. The liver–brain axis in liver failure: neuroinflammation and encephalopathy. Nat. Rev. Gastroenterol. Hepatol. 10, 522–528, (2013).
Zhou, B. et al. Central FGF21 production regulates memory but not peripheral metabolism. Cell Rep. 40, 111239 (2022).
Fisher, F. M. et al. Obesity is a fibroblast growth factor 21 (FGF21)-resistant state. Diabetes 59, 2781–2789 (2010).
Owen, B. M. et al. FGF21 acts centrally to induce sympathetic nerve activity, energy expenditure, and weight loss. Cell Metab. 20, 670–677 (2014).
Pena-Leon, V. et al. Prolonged breastfeeding protects from obesity by hypothalamic action of hepatic FGF21. Nat. Metab. 4, 901–917 (2022).
Meex, R. C. R. & Watt, M. J. Hepatokines: linking nonalcoholic fatty liver disease and insulin resistance. Nat. Rev. Endocrinol. 13, 509–520 (2017).
Godoy-Matos, A. F., Silva Junior, W. S. & Valerio, C. M. NAFLD as a continuum: from obesity to metabolic syndrome and diabetes. Diabetol. Metab. Syndr. 12, 60 (2020).
Nakagami, H. Mechanisms underlying the bidirectional association between nonalcoholic fatty liver disease and hypertension. Hypertens. Res. 46, 539–541 (2023).
Weinstein, G. et al. Association of nonalcoholic fatty liver disease with lower brain volume in healthy middle-aged adults in the Framingham study. JAMA Neurol. 75, 97–104 (2018).
Fabbrini, E. et al. Metabolically normal obese people are protected from adverse effects following weight gain. J. Clin. Invest. 125, 787–795 (2015).
Richards, P., Thornberry, N. A. & Pinto, S. The gut–brain axis: identifying new therapeutic approaches for type 2 diabetes, obesity, and related disorders. Mol. Metab. 46, 101175 (2021).
Clemmensen, C. et al. Gut–brain cross-talk in metabolic control. Cell 168, 758–774 (2017).
Gruber, T. et al. High-calorie diets uncouple hypothalamic oxytocin neurons from a gut-to-brain satiation pathway via kappa-opioid signaling. Cell Rep. 42, 113305 (2023).
Cani, P. D. et al. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 57, 1470–1481 (2008).
Febbraio, M. A. & Karin, M. Sweet death: fructose as a metabolic toxin that targets the gut–liver axis. Cell Metab. 33, 2316–2328 (2021).
Rohm, T. V. et al. Targeting colonic macrophages improves glycemic control in high-fat diet-induced obesity. Commun. Biol. 5, 370 (2022).
Pavlov, V. A. & Tracey, K. J. The vagus nerve and the inflammatory reflex–linking immunity and metabolism. Nat. Rev. Endocrinol. 8, 743–754, (2012).
Tracey, K. J. The inflammatory reflex. Nature 420, 853–859 (2002).
Pavlov, V. A. The evolving obesity challenge: targeting the vagus nerve and the inflammatory reflex in the response. Pharmacol. Ther. 222, 107794 (2021).
Chang, E. H., Chavan, S. S. & Pavlov, V. A. Cholinergic control of inflammation, metabolic dysfunction, and cognitive impairment in obesity-associated disorders: mechanisms and novel therapeutic opportunities. Front. Neurosci. 13, 263 (2019).
Schaeffer, S. & Iadecola, C. Revisiting the neurovascular unit. Nat. Neurosci. 24, 1198–1209 (2021).
Banks, W. A. Brain meets body: the blood–brain barrier as an endocrine interface. Endocrinology 153, 4111–4119, (2012).
Van Dyken, P. & Lacoste, B. Impact of metabolic syndrome on neuroinflammation and the blood–brain barrier. Front. Neurosci. 12, 930 (2018).
Jais, A. et al. Myeloid-cell-derived VEGF maintains brain glucose uptake and limits cognitive impairment in obesity. Cell 165, 882–895 (2016).
Peng, W. et al. Suppression of glymphatic fluid transport in a mouse model of Alzheimer’s disease. Neurobiol. Dis. 93, 215–225 (2016).
Mollgard, K. et al. A mesothelium divides the subarachnoid space into functional compartments. Science 379, 84–88 (2023).
Hablitz, L. M. & Nedergaard, M. The glymphatic system: a novel component of fundamental neurobiology. J. Neurosci. 41, 7698–7711 (2021).
Shechter, R. et al. Recruitment of beneficial M2 macrophages to injured spinal cord is orchestrated by remote brain choroid plexus. Immunity 38, 555–569 (2013).
Baruch, K. et al. Aging. Aging-induced type I interferon response at the choroid plexus negatively affects brain function. Science 346, 89–93 (2014).
Schwartz, M. & Baruch, K. The resolution of neuroinflammation in neurodegeneration: leukocyte recruitment via the choroid plexus. EMBO J. 33, 7–22 (2014).
Delle, C. et al. Long-term high-fat diet increases glymphatic activity in the hypothalamus in mice. Sci. Rep. 13, 4137 (2023).
Andica, C. et al. Neuroimaging findings related to glymphatic system alterations in older adults with metabolic syndrome. Neurobiol. Dis. 177, 105990 (2023).
Banks, W. A. et al. Triglycerides cross the blood-brain barrier and induce central leptin and insulin receptor resistance. Int J. Obes. 42, 391–397 (2018).
Yi, C. X. et al. High calorie diet triggers hypothalamic angiopathy. Mol. Metab. 1, 95–100 (2012).
Gruber, T. et al. Obesity-associated hyperleptinemia alters the gliovascular interface of the hypothalamus to promote hypertension. Cell Metab. 33, 1155–1170 (2021).
Yulyaningsih, E. et al. Acute lesioning and rapid repair of hypothalamic neurons outside the blood–brain barrier. Cell Rep. 19, 2257–2271 (2017).
Cai, D. & Khor, S. "Hypothalamic microinflammation" paradigm in aging and metabolic diseases. Cell Metab. 30, 19–35 (2019).
Meng, Q. & Cai, D. Defective hypothalamic autophagy directs the central pathogenesis of obesity via the IkappaB kinase beta (IKKβ)/NF-κB pathway. J. Biol. Chem. 286, 32324–32332 (2011).
Kaushik, S. et al. Autophagy in hypothalamic AgRP neurons regulates food intake and energy balance. Cell Metab. 14, 173–183 (2011).
Moraes, J. C. et al. High-fat diet induces apoptosis of hypothalamic neurons. PLoS ONE 4, e5045 (2009).
Li, J., Tang, Y. & Cai, D. IKKβ/NF-κB disrupts adult hypothalamic neural stem cells to mediate a neurodegenerative mechanism of dietary obesity and pre-diabetes. Nat. Cell Biol. 14, 999–1012 (2012).
Thaler, J. P. et al. Obesity is associated with hypothalamic injury in rodents and humans. J. Clin. Invest. 122, 153–162 (2012).
Yi, C. X. et al. TNFα drives mitochondrial stress in POMC neurons in obesity. Nat. Commun. 8, 15143 (2017).
Quarta, C. et al. POMC neuronal heterogeneity in energy balance and beyond: an integrated view. Nat. Metab. 3, 299–308 (2021).
Saucisse, N. et al. Functional heterogeneity of POMC neurons relies on mTORC1 signaling. Cell Rep. 37, 109800 (2021).
Lutomska, L. M. et al. Diet triggers specific responses of hypothalamic astrocytes in time and region dependent manner. Glia 70, 2062–2078 (2022).
Garcia-Caceres, C. et al. Role of astrocytes, microglia, and tanycytes in brain control of systemic metabolism. Nat. Neurosci. 22, 7–14 (2019).
Gonzalez-Garcia, I. & Garcia-Caceres, C. Hypothalamic astrocytes as a specialized and responsive cell population in obesity. Int. J. Mol. Sci. 22, 6176 (2021).
Douglass, J. D., Dorfman, M. D., Fasnacht, R., Shaffer, L. D. & Thaler, J. P. Astrocyte IKKβ/NF-κB signaling is required for diet-induced obesity and hypothalamic inflammation. Mol. Metab. 6, 366–373 (2017).
Kwon, Y. H. et al. Hypothalamic lipid-laden astrocytes induce microglia migration and activation. FEBS Lett. 591, 1742–1751 (2017).
Liddelow, S. A. et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature 541, 481–487 (2017).
Patani, R., Hardingham, G. E. & Liddelow, S. A. Functional roles of reactive astrocytes in neuroinflammation and neurodegeneration. Nat. Rev. Neurol. 19, 395–409 (2023).
Kim, J. G. et al. Leptin signaling in astrocytes regulates hypothalamic neuronal circuits and feeding. Nat. Neurosci. 17, 908–910 (2014).
Garcia-Caceres, C. et al. Astrocytic insulin signaling couples brain glucose uptake with nutrient availability. Cell 166, 867–880 (2016).
Seguella, L., Capuano, R., Sarnelli, G. & Esposito, G. Play in advance against neurodegeneration: exploring enteric glial cells in gut–brain axis during neurodegenerative diseases. Expert Rev. Clin. Pharmacol. 12, 555–564 (2019).
Bush, T. G. et al. Fulminant jejuno-ileitis following ablation of enteric glia in adult transgenic mice. Cell 93, 189–201 (1998).
Nampoothiri, S., Nogueiras, R., Schwaninger, M. & Prevot, V. Glial cells as integrators of peripheral and central signals in the regulation of energy homeostasis. Nat. Metab. 4, 813–825 (2022).
Langlet, F. et al. Tanycytic VEGF-A boosts blood-hypothalamus barrier plasticity and access of metabolic signals to the arcuate nucleus in response to fasting. Cell Metab. 17, 607–617 (2013).
Balland, E. et al. Hypothalamic tanycytes are an ERK-gated conduit for leptin into the brain. Cell Metab. 19, 293–301 (2014).
Porniece Kumar, M. et al. Insulin signalling in tanycytes gates hypothalamic insulin uptake and regulation of AgRP neuron activity. Nat. Metab. 3, 1662–1679 (2021).
Bottcher, M. et al. NF-κB signaling in tanycytes mediates inflammation-induced anorexia. Mol. Metab. 39, 101022 (2020).
Gage, F. H. Mammalian neural stem cells. Science 287, 1433–1438 (2000).
Xu, Y. et al. Neurogenesis in the ependymal layer of the adult rat 3rd ventricle. Exp. Neurol. 192, 251–264 (2005).
Lee, D. A. et al. Tanycytes of the hypothalamic median eminence form a diet-responsive neurogenic niche. Nat. Neurosci. 15, 700–702 (2012).
Füger, P. et al. Microglia turnover with aging and in an Alzheimer’s model via long-term in vivo single-cell imaging. Nat. Neurosci. 20, 1371–1376 (2017).
Milanova, I. V., Correa-da-Silva, F., Kalsbeek, A. & Yi, C. X. Mapping of microglial brain region, sex and age heterogeneity in obesity. Int. J. Mol. Sci. 22, 3141 (2021).
Yi, C. X., Tschop, M. H., Woods, S. C. & Hofmann, S. M. High-fat-diet exposure induces IgG accumulation in hypothalamic microglia. Dis. Model Mech. 5, 686–690, (2012).
Gao, Y. et al. Hormones and diet, but not body weight, control hypothalamic microglial activity. Glia 62, 17–25 (2014).
Wang, Z. et al. Saturated fatty acids activate microglia via Toll-like receptor 4/NF-κB signalling. Br. J. Nutr. 107, 229–241 (2012).
Valdearcos, M. et al. Microglial inflammatory signaling orchestrates the hypothalamic immune response to dietary excess and mediates obesity susceptibility. Cell Metab. 26, 185–197 (2017).
Valdearcos, M. et al. Microglia dictate the impact of saturated fat consumption on hypothalamic inflammation and neuronal function. Cell Rep. 9, 2124–2138 (2014).
Douglass, J. D. et al. Obesity-associated microglial inflammatory activation paradoxically improves glucose tolerance. Cell Metab. 35, 1613–1629 (2023).
Delahanty, L. M. et al. Effects of weight loss, weight cycling, and weight loss maintenance on diabetes incidence and change in cardiometabolic traits in the Diabetes Prevention Program. Diabetes Care 37, 2738–2745 (2014).
Tschop, M. H. et al. Unimolecular polypharmacy for treatment of diabetes and obesity. Cell Metab. 24, 51–62 (2016).
Rosenstock, J. et al. Retatrutide, a GIP, GLP-1 and glucagon receptor agonist, for people with type 2 diabetes: a randomised, double-blind, placebo and active-controlled, parallel-group, phase 2 trial conducted in the USA. Lancet 402, 529–544 (2023).
Jastreboff, A. M. et al. Triple-hormone-receptor agonist retatrutide for obesity—a phase 2 trial. N. Engl. J. Med. 389, 514–526 (2023).
Sethi, J. K. & Hotamisligil, G. S. Metabolic messengers: tumour necrosis factor. Nat. Metab. 3, 1302–1312 (2021).
Zhang, Y. et al. TNF-alpha antagonizes the effect of leptin on insulin secretion through FOXO1-dependent transcriptional suppression of LepRb in INS-1 cells. Oxid. Med. Cell. Longev. 2022, 9142798 (2022).
Yang, J. et al. New insight into neurological degeneration: inflammatory cytokines and blood–brain barrier. Front. Mol. Neurosci. 15, 1013933 (2022).
Kwon, H. S. & Koh, S. H. Neuroinflammation in neurodegenerative disorders: the roles of microglia and astrocytes. Transl. Neurodegener. 9, 42 (2020).
Liu, X. & Quan, N. Microglia and CNS interleukin-1: beyond immunological concepts. Front. Neurol. 9, 8 (2018).
Romanatto, T. et al. TNF-alpha acts in the hypothalamus inhibiting food intake and increasing the respiratory quotient–effects on leptin and insulin signaling pathways. Peptides 28, 1050–1058 (2007).
Jager, J., Gremeaux, T., Cormont, M., Le Marchand-Brustel, Y. & Tanti, J. F. Interleukin-1beta-induced insulin resistance in adipocytes through down-regulation of insulin receptor substrate-1 expression. Endocrinology 148, 241–251 (2007).
Negrin, K. A. et al. IL-1 signaling in obesity-induced hepatic lipogenesis and steatosis. PLoS ONE 9, e107265 (2014).
Americo-Da-Silva, L. et al. Activation of the NLRP3 Inflammasome Increases the IL-1beta level and decreases GLUT4 translocation in skeletal muscle during insulin resistance. Int. J. Mol. Sci. 22, 10212 (2021).
Donath, M. Y. Targeting inflammation in the treatment of type 2 diabetes: time to start. Nat. Rev. Drug Discov. 13, 465–476 (2014).
Wang, Y. et al. Interleukin-1beta induces blood–brain barrier disruption by downregulating sonic hedgehog in astrocytes. PLoS ONE 9, e110024 (2014).
Mendiola, A. S. & Cardona, A. E. The IL-1β phenomena in neuroinflammatory diseases. J. Neural Transm. 125, 781–795 (2018).
Rizzo, F. R. et al. Tumor necrosis factor and interleukin-1β modulate synaptic plasticity during neuroinflammation. Neural Plast. 2018, 8430123 (2018).
El-Kadre, L. J. & Tinoco, A. C. Interleukin-6 and obesity: the crosstalk between intestine, pancreas and liver. Curr. Opin. Clin. Nutr. Metab. Care 16, 564–568 (2013).
Sun, B. & Karin, M. Obesity, inflammation, and liver cancer. J. Hepatol. 56, 704–713 (2012).
Mauer, J., Denson, J. L. & Bruning, J. C. Versatile functions for IL-6 in metabolism and cancer. Trends Immunol. 36, 92–101 (2015).
Bobbo, V. C. et al. Interleukin-6 actions in the hypothalamus protects against obesity and is involved in the regulation of neurogenesis. J. Neuroinflammation 18, 192 (2021).
Timper, K. et al. IL-6 improves energy and glucose homeostasis in obesity via enhanced central IL-6 trans-signaling. Cell Rep. 19, 267–280 (2017).
Balschun, D. et al. Interleukin-6: a cytokine to forget. FASEB J. 18, 1788–1790 (2004).
Sukoff Rizzo, S. J. et al. Evidence for sustained elevation of IL-6 in the CNS as a key contributor of depressive-like phenotypes. Transl. Psychiatry 2, e199 (2012).
Tan, C. K., Chong, H. C., Tan, E. H. & Tan, N. S. Getting ‘Smad’ about obesity and diabetes. Nutr. Diabetes 2, e29 (2012).
Makwana, M. et al. Endogenous transforming growth factor beta 1 suppresses inflammation and promotes survival in adult CNS. J. Neurosci. 27, 11201–11213 (2007).
Kanda, H. et al. MCP-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity. J. Clin. Invest. 116, 1494–1505 (2006).
Lee, Y. S. & Olefsky, J. Chronic tissue inflammation and metabolic disease. Genes Dev. 35, 307–328 (2021).
Kawano, Y. et al. Colonic pro-inflammatory macrophages cause insulin resistance in an intestinal Ccl2/Ccr2-dependent manner. Cell Metab. 24, 295–310 (2016).
Rakotoarivelo, V., Variya, B., Langlois, M. F. & Ramanathan, S. Chemokines in human obesity. Cytokine 127, 154953 (2020).
Stamatovic, S. M. et al. Monocyte chemoattractant protein-1 regulation of blood–brain barrier permeability. J. Cereb. Blood Flow. Metab. 25, 593–606 (2005).
Wojcieszak, J., Kuczynska, K. & Zawilska, J. B. Role of chemokines in the development and progression of Alzheimer’s disease. J. Mol. Neurosci. 72, 1929–1951 (2022).
Roberts, T. K. et al. CCL2 disrupts the adherens junction: implications for neuroinflammation. Lab Invest. 92, 1213–1233 (2012).
Hotamisligil, G. S., Shargill, N. S. & Spiegelman, B. M. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science 259, 87–91 (1993).
Hotamisligil, G. S., Arner, P., Caro, J. F., Atkinson, R. L. & Spiegelman, B. M. Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J. Clin. Invest. 95, 2409–2415, (1995).
Hotamisligil, G. S. et al. IRS-1-mediated inhibition of insulin receptor tyrosine kinase activity in TNF-alpha- and obesity-induced insulin resistance. Science 271, 665–668, (1996).
Uysal, K. T., Wiesbrock, S. M., Marino, M. W. & Hotamisligil, G. S. Protection from obesity-induced insulin resistance in mice lacking TNF-alpha function. Nature 389, 610–614 (1997).
Fried, S. K., Bunkin, D. A. & Greenberg, A. S. Omental and subcutaneous adipose tissues of obese subjects release interleukin-6: depot difference and regulation by glucocorticoid. J. Clin. Endocrinol. Metab. 83, 847–850 (1998).
Visser, M., Bouter, L. M., McQuillan, G. M., Wener, M. H. & Harris, T. B. Elevated C-reactive protein levels in overweight and obese adults. JAMA 282, 2131–2135 (1999).
Zhang, X., Dong, F., Ren, J., Driscoll, M. J. & Culver, B. High dietary fat induces NADPH oxidase-associated oxidative stress and inflammation in rat cerebral cortex. Exp. Neurol. 191, 318–325 (2005).
De Souza, C. T. et al. Consumption of a fat-rich diet activates a proinflammatory response and induces insulin resistance in the hypothalamus. Endocrinology 146, 4192–4199 (2005).
Zhang, X. et al. Hypothalamic IKKβ/NF-κB and ER stress link overnutrition to energy imbalance and obesity. Cell 135, 61–73 (2008).
Posey, K. A. et al. Hypothalamic proinflammatory lipid accumulation, inflammation, and insulin resistance in rats fed a high-fat diet. Am. J. Physiol. Endocrinol. Metab. 296, E1003–E1012 (2009).
Milanski, M. et al. Saturated fatty acids produce an inflammatory response predominantly through the activation of TLR4 signaling in hypothalamus: implications for the pathogenesis of obesity. J. Neurosci. 29, 359–370 (2009).
Kleinridders, A. et al. MyD88 signaling in the CNS is required for development of fatty acid-induced leptin resistance and diet-induced obesity. Cell Metab. 10, 249–259 (2009).
Soukas, A., Cohen, P., Socci, N. D. & Friedman, J. M. Leptin-specific patterns of gene expression in white adipose tissue. Genes Dev. 14, 963–980 (2000).
Xu, H. et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J. Clin. Invest. 112, 1821–1830 (2003).
Weisberg, S. P. et al. Obesity is associated with macrophage accumulation in adipose tissue. J. Clin. Invest. 112, 1796–1808 (2003).
Clement, K. et al. Weight loss regulates inflammation-related genes in white adipose tissue of obese subjects. FASEB J. 18, 1657–1669 (2004).
Cancello, R. et al. Reduction of macrophage infiltration and chemoattractant gene expression changes in white adipose tissue of morbidly obese subjects after surgery-induced weight loss. Diabetes 54, 2277–2286 (2005).
Cinti, S. et al. Adipocyte death defines macrophage localization and function in adipose tissue of obese mice and humans. J. Lipid Res. 46, 2347–2355 (2005).
Ozcan, U. et al. Endoplasmic reticulum stress links obesity, insulin action, and type 2 diabetes. Science 306, 457–461 (2004).
Arkan, M. C. et al. IKK-beta links inflammation to obesity-induced insulin resistance. Nat. Med. 11, 191–198 (2005).
Kamei, N. et al. Overexpression of monocyte chemoattractant protein-1 in adipose tissues causes macrophage recruitment and insulin resistance. J. Biol. Chem. 281, 26602–26614 (2006).
Ito, A. et al. Role of CC chemokine receptor 2 in bone marrow cells in the recruitment of macrophages into obese adipose tissue. J. Biol. Chem. 283, 35715–35723 (2008).
Cani, P. D. et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56, 1761–1772 (2007).
Liu, J. et al. Genetic deficiency and pharmacological stabilization of mast cells reduce diet-induced obesity and diabetes in mice. Nat. Med. 15, 940–945 (2009).
Nishimura, S. et al. CD8+ effector T cells contribute to macrophage recruitment and adipose tissue inflammation in obesity. Nat. Med. 15, 914–920 (2009).
Ohmura, K. et al. Natural killer T cells are involved in adipose tissues inflammation and glucose intolerance in diet-induced obese mice. Arterioscler Thromb. Vasc. Biol. 30, 193–199 (2010).
Horvath, T. L. et al. Synaptic input organization of the melanocortin system predicts diet-induced hypothalamic reactive gliosis and obesity. Proc. Natl Acad. Sci. USA 107, 14875–14880 (2010).
Kanoski, S. E., Zhang, Y., Zheng, W. & Davidson, T. L. The effects of a high-energy diet on hippocampal function and blood–brain barrier integrity in the rat. J. Alzheimers Dis. 21, 207–219 (2010).
Morselli, E. et al. Hypothalamic PGC-1α protects against high-fat diet exposure by regulating ERα. Cell Rep. 9, 633–645 (2014).
Quarta, C. et al. Molecular integration of incretin and glucocorticoid action reverses immunometabolic dysfunction and obesity. Cell Metab. 26, 620–632 (2017).
Kim, J. D., Yoon, N. A., Jin, S. & Diano, S. Microglial UCP2 mediates inflammation and obesity induced by high-fat feeding. Cell Metab. 30, 952–962 (2019).
Wong, C. K. et al. Central glucagon-like peptide 1 receptor activation inhibits Toll-like receptor agonist-induced inflammation. Cell Metab. 36, 130–143 (2024).
Lenharo, M. Obesity drugs have another superpower: taming inflammation. Nature 626, 246 (2024).
Belle, M. et al. Tridimensional visualization and analysis of early human development. Cell 169, 161–173 (2017).
Cai, R. et al. Panoptic imaging of transparent mice reveals whole-body neuronal projections and skull-meninges connections. Nat. Neurosci. 22, 317–327 (2019).
Cai, R. et al. Whole-mouse clearing and imaging at the cellular level with vDISCO. Nat. Protoc. 18, 1197–1242 (2023).
Mai, H. et al. Whole-body cellular mapping in mouse using standard IgG antibodies. Nat. Biotechnol. 42, 617–627 (2023).
Pan, C. et al. Deep learning reveals cancer metastasis and therapeutic antibody targeting in the entire body. Cell 179, 1661–1676 (2019).
Formozov, A., Dieter, A. & Wiegert, J. S. A flexible and versatile system for multi-color fiber photometry and optogenetic manipulation. Cell Rep. Methods 3, 100418 (2023).
Sahasrabudhe, A. et al. Multifunctional microelectronic fibers enable wireless modulation of gut and brain neural circuits. Nat. Biotechnol. 42, 892–904 (2023).
Nota, M. H. C. et al. Obesity affects brain structure and function—rescue by bariatric surgery? Neurosci. Biobehav. Rev. 108, 646–657 (2020).
Cheke, L. G., Bonnici, H. M., Clayton, N. S. & Simons, J. S. Obesity and insulin resistance are associated with reduced activity in core memory regions of the brain. Neuropsychologia 96, 137–149 (2017).
Chuang, Y. F. et al. Midlife adiposity predicts earlier onset of Alzheimer’s dementia, neuropathology and presymptomatic cerebral amyloid accumulation. Mol. Psychiatry 21, 910–915 (2016).
Alford, S., Patel, D., Perakakis, N. & Mantzoros, C. S. Obesity as a risk factor for Alzheimer’s disease: weighing the evidence. Obes. Rev. 19, 269–280 (2018).
Li, J., Liu, C., Ang, T. F. A. & Au, R. BMI decline patterns and relation to dementia risk across four decades of follow-up in the Framingham Study. Alzheimers Dement. 19, 2520–2527 (2023).
Xu, L. et al. The effects of exercise for cognitive function in older adults: a systematic review and meta-analysis of randomized controlled trials. Int J. Environ. Res. Public Health 20, 1088 (2023).
Morys, F. et al. Obesity-associated neurodegeneration pattern mimics alzheimer’s disease in an observational cohort study. J. Alzheimers Dis. 91, 1059–1071 (2023).
Willette, A. A. et al. Insulin resistance, brain atrophy, and cognitive performance in late middle-aged adults. Diabetes Care 36, 443–449 (2013).
Sedzikowska, A. & Szablewski, L. Insulin and insulin resistance in Alzheimer’s disease. Int. J. Mol. Sci. 22, 9987 (2021).
Woo, A., Botta, A., Shi, S. S. W., Paus, T. & Pausova, Z. Obesity-related neuroinflammation: magnetic resonance and microscopy imaging of the brain. Int. J. Mol. Sci. 23, 8790 (2022).
Lloret, A., Monllor, P., Esteve, D., Cervera-Ferri, A. & Lloret, M. A. Obesity as a risk factor for Alzheimer’s disease: implication of leptin and glutamate. Front. Neurosci. 13, 508 (2019).
Yin, F. Lipid metabolism and Alzheimer’s disease: clinical evidence, mechanistic link and therapeutic promise. FEBS J. 290, 1420–1453 (2023).
Kellar, D. & Craft, S. Brain insulin resistance in Alzheimer’s disease and related disorders: mechanisms and therapeutic approaches. Lancet Neurol. 19, 758–766 (2020).
Cugurra, A. et al. Skull and vertebral bone marrow are myeloid cell reservoirs for the meninges and CNS parenchyma. Science 373, eabf7844 (2021).
Acknowledgements
We thank C. Holleman for comments. This research is supported by funding from the DZD, the German Research Foundation DFG under Germany’s Excellence Strategy within the framework of the Munich Cluster for Systems Neurology (EXC 2145 SyNergy – ID 390857198), and Helmholtz Association - Initiative and Networking Fund. The funders had no role in decision to publish or prepare this work.
Author information
Authors and Affiliations
Contributions
O.L.T. and C.G.-C. conceptualized the content, wrote, edited and revised the original draft. Both authors have reviewed and approved the final version of the manuscript for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Metabolism thanks Vincent Prevot and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Alfredo Giménez-Cassina, in collaboration with the Nature Metabolism team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Le Thuc, O., García-Cáceres, C. Obesity-induced inflammation: connecting the periphery to the brain. Nat Metab 6, 1237–1252 (2024). https://doi.org/10.1038/s42255-024-01079-8
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s42255-024-01079-8
This article is cited by
-
Single-cell RNA sequencing uncovers molecular features underlying microglial lipid accumulation and depression-related behaviors in high-fat diet mouse model of obesity
Neuropsychopharmacology (2026)
-
The autonomic nervous system in the regulation of glucose and lipid metabolism
Nature Reviews Endocrinology (2026)
-
Ethnicity-Based Personalized Clozapine Titration Strategies for Prevention of Clozapine-Induced Inflammation: Recommendations Based on Evidence from the Japanese Population
CNS Drugs (2026)
-
Hijacking homeostasis: the brain-body neural circuitry in tumor pathogenesis and emerging therapeutic frontiers
Molecular Cancer (2025)
-
Serum S100β and neuron-specific enolase correlate with obesity parameters in Mexican children
International Journal of Obesity (2025)