Abstract
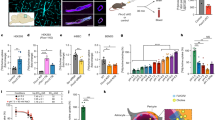
Choline is an essential micronutrient critical for cellular and organismal homeostasis. As a core component of phospholipids and sphingolipids, it is indispensable for membrane architecture and function. Additionally, choline is a precursor for acetylcholine, a key neurotransmitter, and betaine, a methyl donor important for epigenetic regulation. Consistent with its pleiotropic role in cellular physiology, choline metabolism contributes to numerous developmental and physiological processes in the brain, liver, kidney, lung and immune system, and both choline deficiency and excess are implicated in human disease. Mutations in the genes encoding choline metabolism proteins lead to inborn errors of metabolism, which manifest in diverse clinical pathologies. While the identities of many enzymes involved in choline metabolism were identified decades ago, only recently has the field begun to understand the diverse mechanisms by which choline availability is regulated and fuelled via metabolite transport/recycling and nutrient acquisition. This review provides a comprehensive overview of choline metabolism, emphasizing emerging concepts and their implications for human health and disease.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Strecker, A. Ueber einige neue Bestandtheile der Schweinegalle. Justus Liebigs Ann. Chem. 123, 353–360 (1862).
Zeisel, S. H. A brief history of choline. Ann. Nutr. Metab. 61, 254–258 (2012).
Li, Z. & Vance, D. E. Phosphatidylcholine and choline homeostasis. J. Lipid Res. 49, 1187–1194 (2008).
Gobley, T. Recherches Chimiques Sur Les Oeufs de Carpe, Lues à l’Académie Nationale de Médecine (Imprimé par E. Thunot, 1850).
Gobley, T. Sur La Lécithine et La Cérébrine (1874).
Hensing, J. T. The discovery of lecithin, the first phospholipid. Bull. Hist. Chem. 29, 9–15 (2004).
Kennedy, E. P. & Weiss, S. B. The function of cytidine coenzymes in the biosynthesis of phospholipides. J. Biol. Chem. 222, 193–214 (1956).
Hershey, J. M. & Soskin, S. Substitution of ‘lecithin’ for raw pancreas in the diet of the depancreatized dog. Am. J. Physiol. 98, 74–85 (1931).
Best, C. H. & Huntsman, M. E. The effects of the components of lecithine upon deposition of fat in the liver. J. Physiol. 75, 405–412 (1932).
Best, C. H. & Huntsman, M. E. The effect of choline on the liver fat of rats in various states of nutrition. J. Physiol. 83, 255–274 (1935).
Buchman, A. L. et al. Choline deficiency: a cause of hepatic steatosis during parenteral nutrition that can be reversed with intravenous choline supplementation. Hepatology 22, 1399–1403 (1995).
Fischer, L. M. et al. Sex and menopausal status influence human dietary requirements for the nutrient choline. Am. J. Clin. Nutr. 85, 1275–1285 (2007).
Resseguie, M. E. et al. Aberrant estrogen regulation of PEMT results in choline deficiency-associated liver dysfunction. J. Biol. Chem. 286, 1649–1658 (2011).
Zeisel, S. H. et al. Choline, an essential nutrient for humans. FASEB J. 5, 2093–2098 (1991).
Tayek, J. A., Bistrian, B., Sheard, N. F., Zeisel, S. H. & Blackburn, G. L. Abnormal liver function in malnourished patients receiving total parenteral nutrition: a prospective randomized study. J. Am. Coll. Nutr. 9, 76–83 (1990).
Chawla, R. K., Berry, C. J., Kutner, M. H. & Rudman, D. Plasma concentrations of transsulfuration pathway products during nasoenteral and intravenous hyperalimentation of malnourished patients. Am. J. Clin. Nutr. 42, 577–584 (1985).
Burt, M. E., Hanin, I. & Brennan, M. F. Choline deficiency associated with total parenteral nutrition. Lancet 2, 638–639 (1980).
Sheard, N. F., Tayek, J. A., Bistrian, B. R., Blackburn, G. L. & Zeisel, S. H. Plasma choline concentration in humans fed parenterally. Am. J. Clin. Nutr. 43, 219–224 (1986).
Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes and its Panel on Folate, Other B Vitamins, and Choline. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline (National Academies Press, 1998); https://doi.org/10.17226/6015
European Food Safety Authority. Dietary reference values for choline. EFSA J.14, 4484 (2016).
Tavasoli, M., Lahire, S., Reid, T., Brodovsky, M. & McMaster, C. R. Genetic diseases of the Kennedy pathways for membrane synthesis. J. Biol. Chem. 295, 17877–17886 (2020).
Harayama, T. & Riezman, H. Understanding the diversity of membrane lipid composition. Nat. Rev. Mol. Cell Biol. 19, 281–296 (2018).
Kennedy, E. P. Sailing to Byzantium. Annu. Rev. Biochem. 61, 1–28 (1992).
Gallego-Ortega, D. et al. Differential role of human choline kinase alpha and beta enzymes in lipid metabolism: implications in cancer onset and treatment. PLoS ONE 4, e7819 (2009).
Fagone, P. & Jackowski, S. Phosphatidylcholine and the CDP–choline cycle. Biochim. Biophys. Acta 1831, 523–532 (2013).
Chen, W. W., Freinkman, E., Wang, T., Birsoy, K. & Sabatini, D. M. Absolute quantification of matrix metabolites reveals the dynamics of mitochondrial metabolism. Cell 166, 1324–1337 (2016).
Uhlén, M. et al. Tissue-based map of the human proteome. Science 347, 1260419 (2015).
Wu, G., Aoyama, C., Young, S. G. & Vance, D. E. Early embryonic lethality caused by disruption of the gene for choline kinase α, the first enzyme in phosphatidylcholine biosynthesis. J. Biol. Chem. 283, 1456–1462 (2008).
Haider, A. et al. PCYT1A regulates phosphatidylcholine homeostasis from the inner nuclear membrane in response to membrane stored curvature elastic stress. Dev. Cell 45, 481–495 (2018).
Krahmer, N. et al. Phosphatidylcholine synthesis for lipid droplet expansion is mediated by localized activation of CTP:phosphocholine cytidylyltransferase. Cell Metab. 14, 504–515 (2011).
Wang, L., Magdaleno, S., Tabas, I. & Jackowski, S. Early embryonic lethality in mice with targeted deletion of the CTP:phosphocholine cytidylyltransferase α gene (Pcyt1a). Mol. Cell. Biol. 25, 3357–3363 (2005).
Lykidis, A., Baburina, I. & Jackowski, S. Distribution of CTP:phosphocholine cytidylyltransferase (CCT) isoforms. J. Biol. Chem. 274, 26992–27001 (1999).
Henneberry, A. L. & McMaster, C. R. Cloning and expression of a human choline/ethanolaminephosphotransferase: synthesis of phosphatidylcholine and phosphatidylethanolamine. Biochem. J. 339, 291–298 (1999).
Henneberry, A. L., Wistow, G. & McMaster, C. R. Cloning, genomic organization, and characterization of a human cholinephosphotransferase. J. Biol. Chem. 275, 29808–29815 (2000).
Wang, Z., Yang, M., Yang, Y., He, Y. & Qian, H. Structural basis for catalysis of human choline/ethanolamine phosphotransferase 1. Nat. Commun. 14, 2529 (2023).
Wang, L. & Zhou, M. Structure of a eukaryotic cholinephosphotransferase-1 reveals mechanisms of substrate recognition and catalysis. Nat. Commun. 14, 2753 (2023).
Mödinger, Y., Schön, C., Wilhelm, M. & Hals, P. A. Plasma kinetics of choline and choline metabolites after a single dose of SuperbaBoost krill oil or choline bitartrate in healthy volunteers. Nutrients 11, 2548 (2019).
Garguilo, M. G. & Michael, A. C. Amperometric microsensors for monitoring choline in the extracellular fluid of brain. J. Neurosci. Methods 70, 73–82 (1996).
Brehm, R., Lindmar, R. & Löffelholz, K. Muscarinic mobilization of choline in rat brain in vivo as shown by the cerebral arterio‐venous difference of choline. J. Neurochem. 48, 1480–1485 (1987).
Bianchi, L. et al. Extracellular levels of amino acids and choline in human high grade gliomas: an intraoperative microdialysis study. Neurochem. Res. 29, 325–334 (2004).
Mulder, A. H., Yamamura, H. I., Kuhar, M. J. & Snyder, S. H. Release of acetylcholine from hippocampal slices by potassium depolarization: dependence on high affinity choline uptake. Brain Res. 70, 372–376 (1974).
Perry, W. L. M. Acetylcholine release in the cat’s superior cervical ganglion. J. Physiol. 119, 439–454 (1953).
Ennis, E. A. & Blakely, R. D. Choline on the move: perspectives on the molecular physiology and pharmacology of the presynaptic choline transporter. Adv. Pharm. 76, 175–213 (2016).
Hodgkin, A. L. & Martin, K. Choline uptake by giant axons of Loligo. J. Physiol. 179, 26P–27P (1965).
Martin, K. Concentrative accumulation of choline by human erythrocytes. J. Gen. Physiol. 51, 497–516 (1968).
Okuda, T. et al. Identification and characterization of the high-affinity choline transporter. Nat. Neurosci. 3, 120–125 (2000).
Apparsundaram, S., Ferguson, S. M., George, A. L. & Blakely, R. D. Molecular cloning of a human, hemicholinium-3-sensitive choline transporter. Biochem. Biophys. Res. Commun. 276, 862–867 (2000).
Apparsundaram, S., Ferguson, S. M. & Blakely, R. D. Molecular cloning and characterization of a murine hemicholinium-3-sensitive choline transporter. Biochem. Soc. Trans. 29, 711–716 (2001).
Inazu, M. Functional expression of choline transporters in the blood–brain barrier. Nutrients 10.3390/nu11102265 (2019).
Qiu, Y., Gao, Y., Huang, B., Bai, Q. & Zhao, Y. Transport mechanism of presynaptic high-affinity choline uptake by CHT1. Nat. Struct. Mol. Biol. 31, 701–709 (2024).
Ferguson, S. M. et al. Vesicular localization and activity-dependent trafficking of presynaptic choline transporters. J. Neurosci. 23, 9697–9709 (2003).
Nakata, K., Okuda, T. & Misawa, H. Ultrastructural localization of high‐affinity choline transporter in the rat neuromuscular junction: enrichment on synaptic vesicles. Synapse 53, 53–56 (2004).
Holmstrand, E. C., Asafu‐Adjei, J., Sampson, A. R., Blakely, R. D. & Sesack, S. R. Ultrastructural localization of high‐affinity choline transporter in the rat anteroventral thalamus and ventral tegmental area: differences in axon morphology and transporter distribution. J. Comp. Neurol. 518, 1908–1924 (2010).
Ferguson, S. M. et al. Lethal impairment of cholinergic neurotransmission in hemicholinium-3-sensitive choline transporter knockout mice. Proc. Natl Acad. Sci. USA 101, 8762–8767 (2004).
O’Regan, S. et al. An electric lobe suppressor for a yeast choline transport mutation belongs to a new family of transporter-like proteins. Proc. Natl Acad. Sci. USA 97, 1835–1840 (2000).
Yuan, Z., Wagner, L., Poloumienko, A. & Bakovic, M. Identification and expression of a mouse muscle-specific CTL1 gene. Gene 341, 305–312 (2004).
Wille, S. et al. Characterization of CDw92 as a member of the choline transporter-like protein family regulated specifically on dendritic cells. J. Immunol. 167, 5795–5804 (2001).
Fullerton, M. D., Wagner, L., Yuan, Z. & Bakovic, M. Impaired trafficking of choline transporter-like protein-1 at plasma membrane and inhibition of choline transport in THP-1 monocyte-derived macrophages. Am. J. Physiol. Cell Physiol. 290, C1230–C1238 (2006).
Inazu, M., Takeda, H. & Matsumiya, T. Molecular and functional characterization of an Na+-independent choline transporter in rat astrocytes. J. Neurochem. 94, 1427–1437 (2005).
Fagerberg, C. R. et al. Choline transporter-like 1 deficiency causes a new type of childhood-onset neurodegeneration. Brain 143, 94–111 (2020).
Sanchez-Lopez, E. et al. Choline uptake and metabolism modulate macrophage IL-1β and IL-18 production. Cell Metab. 29, 1350–1362 (2019).
Snider, S. A. et al. Choline transport links macrophage phospholipid metabolism and inflammation. J. Biol. Chem. 293, 11600–11611 (2018).
Inazu, M. Choline transporter-like proteins CTLs/SLC44 family as a novel molecular target for cancer therapy. Biopharm. Drug Dispos. 35, 431–449 (2014).
Hedtke, V. & Bakovic, M. Choline transport for phospholipid synthesis: an emerging role of choline transporter-like protein 1. Exp. Biol. Med 244, 655–662 (2019).
Michel, V., Yuan, Z., Ramsubir, S. & Bakovic, M. Choline transport for phospholipid synthesis. Exp. Biol. Med. 231, 490–504 (2006).
Michel, V. & Bakovic, M. The solute carrier 44A1 is a mitochondrial protein and mediates choline transport. FASEB J. 23, 2749–2758 (2009).
Taylor, A., Grapentine, S., Ichhpuniani, J. & Bakovic, M. Choline transporter-like proteins 1 and 2 are newly identified plasma membrane and mitochondrial ethanolamine transporters. J. Biol. Chem. 296, 100604 (2021).
Nakata, T., Matsui, T., Kobayashi, K., Kobayashi, Y. & Anzai, N. Organic cation transporter 2 (SLC22A2), a low-affinity and high-capacity choline transporter, is preferentially enriched on synaptic vesicles in cholinergic neurons. Neuroscience 252, 212–221 (2013).
Sinclair, C. J., Chi, K. D., Subramanian, V., Ward, K. L. & Green, R. M. Functional expression of a high affinity mammalian hepatic choline/organic cation transporter. J. Lipid Res. 41, 1841–1848 (2000).
Kenny, T. C. et al. Integrative genetic analysis identifies FLVCR1 as a plasma-membrane choline transporter in mammals. Cell Metab. 35, 1057–1071 (2023).
Quigley, J. G. et al. Identification of a human heme exporter that is essential for erythropoiesis. Cell 118, 757–766 (2004).
Keel, S. B. et al. A heme export protein is required for red blood cell differentiation and iron homeostasis. Science 319, 825–828 (2008).
Fiorito, V. & Tolosano, E. Unearthing FLVCR1a: tracing the path to a vital cellular transporter. Cell. Mol. Life Sci. 81, 166 (2024).
Xu, Q. et al. Metagenomic and metabolomic remodeling in nonagenarians and centenarians and its association with genetic and socioeconomic factors. Nat. Aging 2, 438–452 (2022).
Moore, A. et al. Genome-wide metabolite quantitative trait loci analysis (mQTL) in red blood cells from volunteer blood donors. J. Biol. Chem. 298, 102706–102707 (2022).
Tsuchiya, M., Tachibana, N., Nagao, K., Tamura, T. & Hamachi, I. Organelle-selective click labeling coupled with flow cytometry allows pooled CRISPR screening of genes involved in phosphatidylcholine metabolism. Cell Metab. 35, 1072–1083 (2023).
Scharenberg, S. G. et al. An SPNS1-dependent lysosomal lipid transport pathway that enables cell survival under choline limitation. Sci. Adv. 9, eadf8966 (2023).
He, M. et al. Spns1 is a lysophospholipid transporter mediating lysosomal phospholipid salvage. Proc. Natl Acad. Sci. USA 119, e2210353119 (2022).
Ha, H. T. et al. Lack of SPNS1 results in accumulation of lysolipids and lysosomal storage disease in mouse models. JCI Insight 9, e175462 (2024).
Rajadhyaksha, A. M. et al. Mutations in FLVCR1 cause posterior column ataxia and retinitis pigmentosa. Am. J. Hum. Genet. 87, 643–654 (2010).
Yanatori, I., Yasui, Y., Miura, K. & Kishi, F. Mutations of FLVCR1 in posterior column ataxia and retinitis pigmentosa result in the loss of heme export activity. Blood Cells Mol. Dis. 49, 60–66 (2012).
Vaughan, D. P., Costello, D. J. & David Vaughan, C. P. Extending the phenotype of posterior column ataxia with retinitis pigmentosa caused by variants in FLVCR1. Am. J. Med. Genet. A https://doi.org/10.1002/AJMG.A.62612 (2021).
Calame, D. G. et al. Biallelic variation in the choline and ethanolamine transporter FLVCR1 underlies a severe developmental disorder spectrum. Genet. Med. https://doi.org/10.1016/J.GIM.2024.101273 (2024).
Grudzinska Pechhacker, M. K. et al. FLVCR1-related disease as a rare cause of retinitis pigmentosa and hereditary sensory autonomic neuropathy. Eur. J. Med. Genet. 63, 104037 (2020).
Kuk, A. C. Y. & Silver, D. L. The cellular supply-side economics for phospholipids. Cell Metab. 35, 909–911 (2023).
Ha, H. T. T. et al. Mfsd7b facilitates choline transport and missense mutations affect choline transport function. Cell. Mol. Life Sci. 81, 3 (2024).
Nguyen, X. T. A. et al. MFSD7c functions as a transporter of choline at the blood–brain barrier. Cell Res. 34, 245–257 (2024).
Kalailingam, P. et al. Deficiency of MFSD7c results in microcephaly-associated vasculopathy in Fowler syndrome. J. Clin. Invest. 130, 4081–4093 (2020).
Cater, R. J. et al. Structural and molecular basis of choline uptake into the brain by FLVCR2. Nature 629, 704–709 (2024).
Son, Y., Kenny, T. C., Khan, A., Birsoy, K. & Hite, R. K. Structural basis of lipid head group entry to the Kennedy pathway by FLVCR1. Nature https://doi.org/10.1038/s41586-024-07374-4 (2024).
Ri, K. et al. Molecular mechanism of choline and ethanolamine transport in humans. Nature 630, 501–508 (2024).
Nguyen, L. N. et al. Mfsd2a is a transporter for the essential omega-3 fatty acid docosahexaenoic acid. Nature 509, 503–506 (2014).
Wong, B. H. et al. Mfsd2a is a transporter for the essential ω-3 fatty acid docosahexaenoic acid (DHA) in eye and is important for photoreceptor cell development. J. Biol. Chem. 291, 10501–10514 (2016).
Chua, G. -L. et al. Mfsd2a utilizes a flippase mechanism to mediate omega-3 fatty acid lysolipid transport. Proc. Natl Acad. Sci. USA 120, e2215290120 (2023).
Walter, J. D., Remm, S. & Seeger, M. A. Fatty acid transporter MFSD2A is a multifunctional gatekeeper in brain and placenta. Nat. Struct. Mol. Biol. 29, 504–506 (2022).
Wood, C. A. P. et al. Structure and mechanism of blood-brain-barrier lipid transporter MFSD2A. Nature 596, 444–448 (2021).
Quek, D. Q. Y., Nguyen, L. N., Fan, H. & Silver, D. L. Structural insights into the transport mechanism of the human sodium-dependent lysophosphatidylcholine transporter MFSD2A. J. Biol. Chem. 291, 9383–9394 (2016).
Cater, R. J. et al. Structural basis of omega-3 fatty acid transport across the blood–brain barrier. Nature 595, 315–319 (2021).
Harel, T. et al. Homozygous mutation in MFSD2A, encoding a lysolipid transporter for docosahexanoic acid, is associated with microcephaly and hypomyelination. Neurogenetics 19, 227–235 (2018).
Guemez-Gamboa, A. et al. Inactivating mutations in MFSD2A, required for omega-3 fatty acid transport in brain, cause a lethal microcephaly syndrome. Nat. Genet. 47, 809–813 (2015).
Alakbarzade, V. et al. A partially inactivating mutation in the sodium-dependent lysophosphatidylcholine transporter MFSD2A causes a non-lethal microcephaly syndrome. Nat. Genet. 47, 814–817 (2015).
Scala, M. et al. Biallelic MFSD2A variants associated with congenital microcephaly, developmental delay, and recognizable neuroimaging features. Eur. J. Hum. Genet. 28, 1509–1519 (2020).
Zhou, J. et al. Zika virus degrades the ω-3 fatty acid transporter Mfsd2a in brain microvascular endothelial cells and impairs lipid homeostasis. Sci. Adv. 5, eaax7142 (2019).
Abe, A., Kelly, R. & Shayman, J. A. The measurement of lysosomal phospholipase A2 activity in plasma. J. Lipid Res. 51, 2464–2470 (2010).
Hiraoka, M., Abe, A. & Shayman, J. A. Cloning and characterization of a lysosomal phospholipase A2, 1-O-acylceramide synthase. J. Biol. Chem. 277, 10090–10099 (2002).
Hinkovska-Galcheva, V. et al. Determinants of pH profile and acyl chain selectivity in lysosomal phospholipase A2. J. Lipid Res. 59, 1205–1218 (2018).
Glukhova, A. et al. Structure and function of lysosomal phospholipase A2 and lecithin:cholesterol acyltransferase. Nat. Commun. 6, 6250 (2015).
Hiraoka, M. et al. Lysosomal phospholipase A2 and phospholipidosis. Mol. Cell. Biol. 26, 6139–6148 (2006).
Hostetler, K. Y., Yazaki, P. J. & van den Bosch, H. Purification of lysosomal phospholipase A. Evidence for multiple isoenzymes in rat liver. J. Biol. Chem. 257, 13367–13373 (1982).
Franson, R., Waite, M. & LaVia, M. Identification of phospholipase A1 and A2 in the soluble fraction of rat liver lysosomes. Biochemistry 10, 1942–1946 (1971).
Nyame, K. et al. PLA2G15 is a lysosomal BMP hydrolase with ester position specificity and its targeting ameliorates lysosomal disease. Preprint at bioRxiv https://doi.org/10.1101/2024.06.07.597919 (2024).
Kretzschmar, D. PNPLA6/NTE, an evolutionary conserved phospholipase linked to a group of complex human diseases. Metabolites 12, 284 (2022).
Van Tienhoven, M., Atkins, J., Li, Y. & Glynn, P. Human neuropathy target esterase catalyzes hydrolysis of membrane lipids. J. Biol. Chem. 277, 20942–20948 (2002).
Lush, M. J., Li, Y., Read, D. J., Willis, A. C. & Glynn, P. Neuropathy target esterase and a homologous Drosophila neurodegeneration-associated mutant protein contain a novel domain conserved from bacteria to man. Biochem. J. 332, 1–4 (1998).
Glynn, P. Neuronal phospholipid deacylation is essential for axonal and synaptic integrity. Biochim. Biophys. Acta 1831, 633–641 (2013).
Nyame, K. et al. Glycerophosphodiesters inhibit lysosomal phospholipid catabolism in Batten disease. Mol. Cell 84, 1354–1364 (2024).
Laqtom, N. N. et al. CLN3 is required for the clearance of glycerophosphodiesters from lysosomes. Nature 609, 1005–1011 (2022).
Ridgway, N. D. & Vance, D. E. Purification of phosphatidylethanolamine N-methyltransferase from rat liver. J. Biol. Chem. 262, 17231–17239 (1987).
Huitema, K., van den Dikkenberg, J., Brouwers, J. F. H. M. & Holthuis, J. C. M. Identification of a family of animal sphingomyelin synthases. EMBO J. 23, 33–44 (2004).
Tafesse, F. G. et al. Both sphingomyelin synthases SMS1 and SMS2 are required for sphingomyelin homeostasis and growth in human HeLa cells. J. Biol. Chem. 282, 17537–17547 (2007).
Okazaki, Y. et al. A novel glycerophosphodiester phosphodiesterase, GDE5, controls skeletal muscle development via a non-enzymatic mechanism. J. Biol. Chem. 285, 27652–27663 (2010).
Gallazzini, M., Ferraris, J. D. & Burg, M. B. GDPD5 is a glycerophosphocholine phosphodiesterase that osmotically regulates the osmoprotective organic osmolyte GPC. Proc. Natl Acad. Sci. USA 105, 11026–11031 (2008).
Hammond, S. M. et al. Human ADP-ribosylation factor-activated phosphatidylcholine-specific phospholipase D defines a new and highly conserved gene family. J. Biol. Chem. 270, 29640–29643 (1995).
Lopez, I., Arnold, R. S. & Lambeth, J. D. Cloning and initial characterization of a human phospholipase D2 (hPLD2). ADP-ribosylation factor regulates hPLD2. J. Biol. Chem. 273, 12846–12852 (1998).
Saito de, R. F., Andrade de, L. N. S., Bustos, S. O. & Chammas, R. Phosphatidylcholine-derived lipid mediators: the crosstalk between cancer cells and immune cells. Front. Immunol. 13, 768606 (2022).
Blusztajn, J. K., Lopez Gonzalez-Coviella, I., Logue, M., Growdon, J. H. & Wurtman, R. J. Levels of phospholipid catabolic intermediates, glycerophosphocholine and glycerophosphoethanolamine, are elevated in brains of Alzheimer’s disease but not of Down’s syndrome patients. Brain Res. 536, 240–244 (1990).
Pahud, G. et al. Study of subcellular localization of membrane-bound choline acetyltransferase in Drosophila central nervous system and its association with membranes. Eur. J. Neurosci. 10, 1644–1653 (1998).
Tandon, A., Bachoo, M., Weldon, P., Polosa, C. & Collier, B. Effects of colchicine application to preganglionic axons on choline acetyltransferase activity and acetylcholine content and release in the superior cervical ganglion. J. Neurochem. 66, 1033–1041 (1996).
Lever, M. & Slow, S. The clinical significance of betaine, an osmolyte with a key role in methyl group metabolism. Clin. Biochem. 43, 732–744 (2010).
Craig, S. A. Betaine in human nutrition. Am. J. Clin. Nutr. 80, 539–549 (2004).
Alvarenga, L., Ferreira, M. S., Kemp, J. A. & Mafra, D. The role of betaine in patients with chronic kidney disease: a narrative review. Curr. Nutr. Rep. 11, 395–406 (2022).
Ducker, G. S. & Rabinowitz, J. D. One-carbon metabolism in health and disease. Cell Metab. 25, 27–42 (2017).
Wang, Z. et al. Non-lethal inhibition of gut microbial trimethylamine production for the treatment of atherosclerosis. Cell 163, 1585–1595 (2015).
Baker, J. R. & Chaykin, S. The biosynthesis of trimethylamine-N-oxide. J. Biol. Chem. 237, 1309–1313 (1962).
Wang, H. et al. The microbial metabolite trimethylamine N-oxide promotes antitumor immunity in triple-negative breast cancer. Cell Metab. 34, 581–594 (2022).
Chen, S. et al. Trimethylamine N-oxide binds and activates PERK to promote metabolic dysfunction. Cell Metab. 30, 1141–1151 (2019).
Yoo, W. et al. High-fat diet-induced colonocyte dysfunction escalates microbiota-derived trimethylamine N-oxide. Science 373, 813–818 (2021).
Vance, J. E. Phospholipid synthesis and transport in mammalian cells. Traffic 16, 1–18 (2015).
van Meer, G., Voelker, D. R. & Feigenson, G. W. Membrane lipids: where they are and how they behave. Nat. Rev. Mol. Cell Biol. 9, 112–124 (2008).
Horibata, Y. & Sugimoto, H. StarD7 mediates the intracellular trafficking of phosphatidylcholine to mitochondria. J. Biol. Chem. 285, 7358–7365 (2010).
Khan, A. et al. Metabolic gene function discovery platform GeneMAP identifies SLC25A48 as necessary for mitochondrial choline import. Nat. Genet. 56, 1614–1623 (2024).
Schlosser, P. et al. Genetic studies of paired metabolomes reveal enzymatic and transport processes at the interface of plasma and urine. Nat. Genet. 55, 995–1008 (2023).
Patil, S. et al. The membrane transporter SLC25A48 enables transport of choline into human mitochondria. Kidney Int. https://doi.org/10.1016/j.kint.2024.06.022 (2024).
Verkerke, A. R. P. et al. SLC25A48 controls mitochondrial choline import and metabolism. Cell Metab. 36, 2156–2166 (2024).
Hollenbeck, C. B. An introduction to the nutrition and metabolism of choline. Cent. Nerv. Syst. Agents Med. Chem. 12, 100–113 (2012).
Li, J., Xin, Y., Li, J., Chen, H. & Li, H. Phosphatidylethanolamine N-methyltransferase: from functions to diseases. Aging Dis. 14, 879–891 (2023).
Zeisel, S. H. & da Costa, K. -A. Choline: an essential nutrient for public health. Nutr. Rev. 67, 615–623 (2009).
Wallace, T. C. et al. Choline: the underconsumed and underappreciated essential nutrient. Nutr. Today 53, 240–253 (2018).
Sanders, L. M. & Zeisel, S. H. Choline: dietary requirements and role in brain development. Nutr. Today 42, 181–186 (2007).
Leermakers, E. T. et al. Effects of choline on health across the life course: a systematic review. Nutr. Rev. 73, 500–522 (2015).
Wiedeman, A. M. et al. Dietary choline intake: current state of knowledge across the life cycle. Nutrients 10, 1513 (2018).
Zeisel, S. H. Dietary choline: biochemistry, physiology, and pharmacology. Annu. Rev. Nutr. 1, 95–121 (1981).
Zeisel, S. H., Growdon, J. H., Wurtman, R. J., Magil, S. G. & Logue, M. Normal plasma choline responses to ingested lecithin. Neurology 30, 1226–1229 (1980).
Horie, A., Ishida, K., Watanabe, Y., Shibata, K. & Hashimoto, Y. Membrane transport mechanisms of choline in human intestinal epithelial LS180 cells. Biopharm. Drug Dispos. 35, 532–542 (2014).
Lee, N. Y., Choi, H. M. & Kang, Y. S. Choline transport via choline transporter-like protein 1 in conditionally immortalized rat syncytiotrophoblast cell lines TR-TBT. Placenta 30, 368–374 (2009).
Zeisel, S. H. Choline: critical role during fetal development and dietary requirements in adults. Annu. Rev. Nutr. 26, 229–250 (2006).
Ensminger, M. E., Bowland, J. P. & Cunha, T. J. Observations on the thiamine, riboflavin, and choline needs of sows for reproduction. J. Anim. Sci. 6, 409–423 (1947).
Meader, R. D. Livers of choline-deficient pregnant and fetal rats. Anat. Rec. 153, 407–419 (1965).
da Costa, K. A. et al. Common genetic polymorphisms affect the human requirement for the nutrient choline. FASEB J. 20, 1336–1344 (2006).
Kohlmeier, M., da Costa, K. A., Fischer, L. M. & Zeisel, S. H. Genetic variation of folate-mediated one-carbon transfer pathway predicts susceptibility to choline deficiency in humans. Proc. Natl Acad. Sci. USA 102, 16025–16030 (2005).
Vance, D. E. & Vance, J. E. Physiological consequences of disruption of mammalian phospholipid biosynthetic genes. J. Lipid Res. 50, S132–S137 (2009).
Brody, L. C. et al. A polymorphism, R653Q, in the trifunctional enzyme methylenetetrahydrofolate dehydrogenase/methenyltetrahydrofolate cyclohydrolase/formyltetrahydrofolate synthetase is a maternal genetic risk factor for neural tube defects: report of the Birth Defects Research Group. Am. J. Hum. Genet. 71, 1207–1215 (2002).
Jacob, R. A., Jenden, D. J., Allman-Farinelli, M. A. & Swendseid, M. E. Folate nutriture alters choline status of women and men fed low choline diets. J. Nutr. 129, 712–717 (1999).
Kim, Y. I. et al. Severe folate deficiency causes secondary depletion of choline and phosphocholine in rat liver. J. Nutr. 124, 2197–2203 (1994).
Ananth, M. R., Rajebhosale, P., Kim, R., Talmage, D. A. & Role, L. W. Basal forebrain cholinergic signalling: development, connectivity and roles in cognition. Nat. Rev. Neurosci. 24, 233–251 (2023).
Picciotto, M. R., Higley, M. J. & Mineur, Y. S. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron 76, 116–129 (2012).
Carlson, A. B. & Kraus, G. P. Physiology, Cholinergic Receptors (StatPearls Publishing, 2024).
Giocomo, L. M. & Hasselmo, M. E. Neuromodulation by glutamate and acetylcholine can change circuit dynamics by regulating the relative influence of afferent input and excitatory feedback. Mol. Neurobiol. 36, 184–200 (2007).
McKay, B. E., Placzek, A. N. & Dani, J. A. Regulation of synaptic transmission and plasticity by neuronal nicotinic acetylcholine receptors. Biochem. Pharmacol. 74, 1120–1133 (2007).
Yao, Z. M. & Vance, D. E. The active synthesis of phosphatidylcholine is required for very low density lipoprotein secretion from rat hepatocytes. J. Biol. Chem. 263, 2998–3004 (1988).
Cole, L. K., Vance, J. E. & Vance, D. E. Phosphatidylcholine biosynthesis and lipoprotein metabolism. Biochim. Biophys. Acta 1821, 754–761 (2012).
Kansakar, U. et al. Choline supplements: an update. Front. Endocrinol. 14, 1148166 (2023).
Barrios, J. M. & Lichtenberger, L. M. Role of biliary phosphatidylcholine in bile acid protection and NSAID injury of the ileal mucosa in rats. Gastroenterology 118, 1179–1186 (2000).
Boyer, J. L. Bile formation and secretion. Compr. Physiol. 3, 1035–1078 (2013).
Small, D. M. Role of ABC transporters in secretion of cholesterol from liver into bile. Proc. Natl Acad. Sci. USA 100, 4–6 (2003).
Li, Z., Agellon, L. B. & Vance, D. E. Phosphatidylcholine homeostasis and liver failure. J. Biol. Chem. 280, 37798–37802 (2005).
Phang-Lyn, S. & Llerena, V. A. Biochemistry, Biotransformation (StatPearls Publishing, 2024).
Goss, V., Hunt, A. N. & Postle, A. D. Regulation of lung surfactant phospholipid synthesis and metabolism. Biochim. Biophys. Acta 1831, 448–458 (2013).
Bernhard, W. et al. Phosphatidylcholine molecular species in lung surfactant: composition in relation to respiratory rate and lung development. Am. J. Respir. Cell Mol. Biol. 25, 725–731 (2001).
Hamm, H., Fabel, H. & Bartsch, W. The surfactant system of the adult lung: physiology and clinical perspectives. Clin. Investig. 70, 637–657 (1992).
Nakanishi, T., Turner, R. J. & Burg, M. B. Osmoregulation of betaine transport in mammalian renal medullary cells. Am. J. Physiol. 258, F1061–F1067 (1990).
Bagnasco, S., Balaban, R., Fales, H. M., Yang, Y. M. & Burg, M. Predominant osmotically active organic solutes in rat and rabbit renal medullas. J. Biol. Chem. 261, 5872–5877 (1986).
Kempson, S. A., Vovor-Dassu, K. & Day, C. Betaine transport in kidney and liver: use of betaine in liver injury. Cell. Physiol. Biochem. 32, 32–40 (2013).
Kempson, S. A., Zhou, Y. & Danbolt, N. C. The betaine/GABA transporter and betaine: roles in brain, kidney, and liver. Front Physiol. 5, 159 (2014).
Huang, Y. H., Schafer-Elinder, L., Wu, R., Claesson, H. E. & Frostegard, J. Lysophosphatidylcholine (LPC) induces proinflammatory cytokines by a platelet-activating factor (PAF) receptor-dependent mechanism. Clin. Exp. Immunol. 116, 326–331 (1999).
Carneiro, A. B. et al. Lysophosphatidylcholine triggers TLR2- and TLR4-mediated signaling pathways but counteracts LPS-induced NO synthesis in peritoneal macrophages by inhibiting NF-κB translocation and MAPK/ERK phosphorylation. PLoS ONE 8, e76233 (2013).
Ashraf, M. A. & Nookala, V. Biochemistry of Platelet Activating Factor (StatPearls Publishing, 2024).
Billipp, T. E. et al. Tuft cell-derived acetylcholine promotes epithelial chloride secretion and intestinal helminth clearance. Immunity 57, 1243–1259 (2024).
Ndjim, M. et al. Tuft cell acetylcholine is released into the gut lumen to promote anti-helminth immunity. Immunity 57, 1260–1273 (2024).
Wiedeman, A. M. et al. Concentrations of water-soluble forms of choline in human milk from lactating women in Canada and Cambodia. Nutrients 10, 381 (2018).
Zeisel, S. H., Epstein, M. F. & Wurtman, R. J. Elevated choline concentration in neonatal plasma. Life Sci. 26, 1827–1831 (1980).
Buchman, A. L. et al. Plasma choline in normal newborns, infants, toddlers, and in very-low-birth-weight neonates requiring total parenteral nutrition. Nutrition 17, 18–21 (2001).
Bragg, M. G., Prado, E. L. & Stewart, C. P. Choline and docosahexaenoic acid during the first 1000 days and children’s health and development in low- and middle-income countries. Nutr. Rev. 80, 656–676 (2022).
Albright, C. D., Tsai, A. Y., Friedrich, C. B., Mar, M. H. & Zeisel, S. H. Choline availability alters embryonic development of the hippocampus and septum in the rat. Brain Res. Dev. Brain Res. 113, 13–20 (1999).
Albright, C. D., Friedrich, C. B., Brown, E. C., Mar, M. H. & Zeisel, S. H. Maternal dietary choline availability alters mitosis, apoptosis and the localization of TOAD-64 protein in the developing fetal rat septum. Brain Res. Dev. Brain Res. 115, 123–129 (1999).
Pyapali, G. K., Turner, D. A., Williams, C. L., Meck, W. H. & Swartzwelder, H. S. Prenatal dietary choline supplementation decreases the threshold for induction of long-term potentiation in young adult rats. J. Neurophysiol. 79, 1790–1796 (1998).
Niculescu, M. D., Craciunescu, C. N. & Zeisel, S. H. Dietary choline deficiency alters global and gene-specific DNA methylation in the developing hippocampus of mouse fetal brains. FASEB J. 20, 43–49 (2006).
Fisher, M. C., Zeisel, S. H., Mar, M. H. & Sadler, T. W. Perturbations in choline metabolism cause neural tube defects in mouse embryos in vitro. FASEB J. 16, 619–621 (2002).
Lauder, J. M. & Schambra, U. B. Morphogenetic roles of acetylcholine. Environ. Health Perspect. 107, 65–69 (1999).
Li, Q. et al. Dietary prenatal choline supplementation alters postnatal hippocampal structure and function. J. Neurophysiol. 91, 1545–1555 (2004).
Williams, C. L., Meck, W. H., Heyer, D. D. & Loy, R. Hypertrophy of basal forebrain neurons and enhanced visuospatial memory in perinatally choline-supplemented rats. Brain Res. 794, 225–238 (1998).
Jones, J. P., Meck, W. H., Williams, C. L., Wilson, W. A. & Swartzwelder, H. S. Choline availability to the developing rat fetus alters adult hippocampal long-term potentiation. Brain Res. Dev. Brain Res. 118, 159–167 (1999).
Meck, W. H. & Williams, C. L. Characterization of the facilitative effects of perinatal choline supplementation on timing and temporal memory. Neuroreport 8, 2831–2835 (1997).
Meck, W. H. & Williams, C. L. Metabolic imprinting of choline by its availability during gestation: implications for memory and attentional processing across the lifespan. Neurosci. Biobehav. Rev. 27, 385–399 (2003).
Meck, W. H. & Williams, C. L. Perinatal choline supplementation increases the threshold for chunking in spatial memory. Neuroreport 8, 3053–3059 (1997).
Meck, W. H. & Williams, C. L. Simultaneous temporal processing is sensitive to prenatal choline availability in mature and aged rats. Neuroreport 8, 3045–3051 (1997).
Meck, W. H., Smith, R. A. & Williams, C. L. Pre- and postnatal choline supplementation produces long-term facilitation of spatial memory. Dev. Psychobiol. 21, 339–353 (1988).
Wortmann, S. B. & Mayr, J. A. Choline-related-inherited metabolic diseases—a mini review. J. Inherit. Metab. Dis. 42, 237–242 (2019).
Mitsuhashi, S. et al. A congenital muscular dystrophy with mitochondrial structural abnormalities caused by defective de novo phosphatidylcholine biosynthesis. Am. J. Hum. Genet. 88, 845–851 (2011).
Barwick, K. E. et al. Defective presynaptic choline transport underlies hereditary motor neuropathy. Am. J. Hum. Genet. 91, 1103–1107 (2012).
Ohno, K. et al. Choline acetyltransferase mutations cause myasthenic syndrome associated with episodic apnea in humans. Proc. Natl Acad. Sci. USA 98, 2017–2022 (2001).
Hoover-Fong, J. et al. Mutations in PCYT1A, encoding a key regulator of phosphatidylcholine metabolism, cause spondylometaphyseal dysplasia with cone-rod dystrophy. Am. J. Hum. Genet. 94, 105–112 (2014).
Yamamoto, G. L. et al. Mutations in PCYT1A cause spondylometaphyseal dysplasia with cone-rod dystrophy. Am. J. Hum. Genet. 94, 113–119 (2014).
Payne, F. et al. Mutations disrupting the Kennedy phosphatidylcholine pathway in humans with congenital lipodystrophy and fatty liver disease. Proc. Natl Acad. Sci. USA 111, 8901–8906 (2014).
Zeisel, S. H. et al. Choline deficiency selects for resistance to p53-independent apoptosis and causes tumorigenic transformation of rat hepatocytes. Carcinogenesis 18, 731–738 (1997).
Sha, W. et al. Metabolomic profiling can predict which humans will develop liver dysfunction when deprived of dietary choline. FASEB J. 24, 2962–2975 (2010).
Corbin, K. D. & Zeisel, S. H. Choline metabolism provides novel insights into nonalcoholic fatty liver disease and its progression. Curr. Opin. Gastroenterol. 28, 159–165 (2012).
Li, Z., Agellon, L. B. & Vance, D. E. Choline redistribution during adaptation to choline deprivation. J. Biol. Chem. 282, 10283–10289 (2007).
Corbin, K. D. et al. Genetic signatures in choline and 1-carbon metabolism are associated with the severity of hepatic steatosis. FASEB J. 27, 1674–1689 (2013).
Mehedint, M. G. & Zeisel, S. H. Choline’s role in maintaining liver function: new evidence for epigenetic mechanisms. Curr. Opin. Clin. Nutr. Metab. Care 16, 339–345 (2013).
Hensley, K. et al. Dietary choline restriction causes complex I dysfunction and increased H2O2 generation in liver mitochondria. Carcinogenesis 21, 983–989 (2000).
Zhan, X. et al. Choline supplementation regulates gut microbiome diversity, gut epithelial activity, and the cytokine gene expression in gilts. Front. Nutr. 10, 1101519 (2023).
Glunde, K., Jacobs, M. A. & Bhujwalla, Z. M. Choline metabolism in cancer: implications for diagnosis and therapy. Expert Rev. Mol. Diagn. 6, 821–829 (2006).
Glunde, K., Bhujwalla, Z. M. & Ronen, S. M. Choline metabolism in malignant transformation. Nat. Rev. Cancer 11, 835–848 (2011).
Lee, Z. [18F]-choline PET/CT as an imaging biomarker for primary liver cancers. Transl. Cancer Res. 5, S1489–S1492 (2016).
Murphy, R. C., Kawashima, A. & Peller, P. J. The utility of 11C-choline PET/CT for imaging prostate cancer: a pictorial guide. AJR Am. J. Roentgenol. 196, 1390–1398 (2011).
Guo, Y., Wang, L., Hu, J., Feng, D. & Xu, L. Diagnostic performance of choline PET/CT for the detection of bone metastasis in prostate cancer: a systematic review and meta-analysis. PLoS ONE 13, e0203400 (2018).
Zhang, R. R. et al. Next-generation cancer magnetic resonance imaging with tumor-targeted alkylphosphocholine metal analogs. Invest. Radio. 57, 655–663 (2022).
Weichert, J. P. et al. Alkylphosphocholine analogs for broad-spectrum cancer imaging and therapy. Sci. Transl. Med. 6, 240ra75 (2014).
Yuan, J. et al. Is dietary choline intake related to dementia and Alzheimer’s disease risks? Results from the Framingham Heart Study. Am. J. Clin. Nutr. 116, 1201–1207 (2022).
Chen, Z. R., Huang, J. B., Yang, S. L. & Hong, F. F. Role of cholinergic signaling in Alzheimer’s disease. Molecules 27, 1816 (2022).
Bertrand, D. & Wallace, T. L. A review of the cholinergic system and therapeutic approaches to treat brain disorders. Curr. Top. Behav. Neurosci. 45, 1–28 (2020).
Dave, N. et al. Dietary choline intake is necessary to prevent systems-wide organ pathology and reduce Alzheimer’s disease hallmarks. Aging Cell 22, e13775 (2023).
Velazquez, R. et al. Lifelong choline supplementation ameliorates Alzheimer’s disease pathology and associated cognitive deficits by attenuating microglia activation. Aging Cell 18, e13037 (2019).
Pepeu, G. & Grazia Giovannini, M. The fate of the brain cholinergic neurons in neurodegenerative diseases. Brain Res. 1670, 173–184 (2017).
Lorent, J. H. et al. Plasma membranes are asymmetric in lipid unsaturation, packing and protein shape. Nat. Chem. Biol. 16, 644–652 (2020).
Li, Z. et al. The ratio of phosphatidylcholine to phosphatidylethanolamine influences membrane integrity and steatohepatitis. Cell Metab. 3, 321–331 (2006).
Ma, D. W. L. et al. Plasma phospholipids and fatty acid composition differ between liver biopsy-proven nonalcoholic fatty liver disease and healthy subjects. Nutr. Diabetes 6, e220–e220 (2016).
Cornell, R. & Antonny, B. CCTα commands phospholipid homeostasis from the nucleus. Dev. Cell 45, 419–420 (2018).
Cornell, R. B. & Ridgway, N. D. CTP:phosphocholine cytidylyltransferase: function, regulation, and structure of an amphitropic enzyme required for membrane biogenesis. Prog. Lipid Res. 59, 147–171 (2015).
Kent, C. Regulatory enzymes of phosphatidylcholine biosynthesis: a personal perspective. Biochim. Biophys. Acta 1733, 53–66 (2005).
Infante, J. P. & Kinsella, J. E. Control of phosphatidylcholine synthesis and the regulatory role of choline kinase in rat liver. Evidence from essential-fatty acid-deficient rats. Biochem. J. 176, 631–633 (1978).
Yu, Y., Sreenivas, A., Ostrander, D. B. & Carman, G. M. Phosphorylation of Saccharomyces cerevisiae choline kinase on Ser30 and Ser85 by protein kinase A regulates phosphatidylcholine synthesis by the CDP–choline pathway. J. Biol. Chem. 277, 34978–34986 (2002).
Bi, J. et al. Oncogene amplification in growth factor signaling pathways renders cancers dependent on membrane lipid remodeling. Cell Metab. 30, 525–538 (2019).
Desai, A. J. & Miller, L. J. Changes in the plasma membrane in metabolic disease: impact of the membrane environment on G-protein-coupled receptor structure and function. Br. J. Pharmacol. 175, 4009–4025 (2018).
Arish, M. et al. Orchestration of membrane receptor signaling by membrane lipids. Biochimie 113, 111–124 (2015).
Volmer, R., van der Ploeg, K. & Ron, D. Membrane lipid saturation activates endoplasmic reticulum unfolded protein response transducers through their transmembrane domains. Proc. Natl Acad. Sci. USA 110, 4628–4633 (2013).
Wang, B. & Tontonoz, P. Phospholipid remodeling in physiology and disease. Annu. Rev. Physiol. 81, 165–188 (2019).
O’Donnell, V. B. New appreciation for an old pathway: the Lands cycle moves into new arenas in health and disease. Biochem. Soc. Trans. 50, 1–11 (2022).
Lands, W. E. Stories about acyl chains. Biochim. Biophys. Acta 1483, 1–14 (2000).
Shayman, J. A. & Tesmer, J. J. G. Lysosomal phospholipase A2. Biochim. Biophys. Acta Mol. Cell. Biol. Lipids 1864, 932–940 (2019).
Hornburg, D. et al. Dynamic lipidome alterations associated with human health, disease and ageing. Nat. Metab. 5, 1578–1594 (2023).
Broadfield, L. A., Pane, A. A., Talebi, A., Swinnen, J. V. & Fendt, S. M. Lipid metabolism in cancer: new perspectives and emerging mechanisms. Dev. Cell 56, 1363–1393 (2021).
Settembre, C. & Perera, R. M. Lysosomes as coordinators of cellular catabolism, metabolic signalling and organ physiology. Nat. Rev. Mol. Cell Biol. 25, 223–245 (2024).
Feingold, K. R. Introduction to lipids and lipoproteins. In Endotext (eds. Feingold, K. R. et al.) (MDText.com, 2000).
Thelen, A. M. & Zoncu, R. Emerging roles for the lysosome in lipid metabolism. Trends Cell Biol. 27, 833–850 (2017).
Hirabayashi, T. et al. Hepatic phosphatidylcholine catabolism driven by PNPLA7 and PNPLA8 supplies endogenous choline to replenish the methionine cycle with methyl groups. Cell Rep. 42, 111940 (2023).
Acknowledgements
We thank all members of the Birsoy and Abu-Remaileh laboratories for their feedback and discussions. T.C.K. is supported by NIH/National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) F32DK127836 and K99DK140517. S.S. is supported by NIH T32GM007365 and 5T32GM139791-03. M.A.-R. is supported by NIH DP-CA271386, Michael J. Fox Foundation ASAP-000463 and Beat Batten NCL Foundation NCL-Stiftung. K.B. is supported by NIH/NIDDK R01DK123323-01 and R01DK140337-01.
Author information
Authors and Affiliations
Contributions
T.C.K. and S.S. performed the literature review and drafted an outline of the manuscript with input from M.A.-R. and K.B. T.C.K. and S.S. wrote the first draft of the manuscript and generated all figures. M.A.-R. and K.B. provided critical feedback and assisted in editing of the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
M.A.-R. is a scientific advisory board member of Lycia Therapeutics. K.B. is a scientific advisor to Nanocare Pharmaceuticals and Atavistik Bio. T.C.K. and S.S. declare no interests.
Peer review
Peer review information
Nature Metabolism thanks the anonymous reviewers for their contribution to the peer review of this work. Primary Handling Editor: Alfredo Giménez-Cassina, in collaboration with the Nature Metabolism team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kenny, T.C., Scharenberg, S., Abu-Remaileh, M. et al. Cellular and organismal function of choline metabolism. Nat Metab 7, 35–52 (2025). https://doi.org/10.1038/s42255-024-01203-8
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s42255-024-01203-8
This article is cited by
-
Association between dietary choline intake and bone mineral density in adolescents: a NHANES-based study
BMC Pediatrics (2025)
-
Lethal toxicity of metformin on zebrafish during early embryonic development by multi-omics analysis
Scientific Reports (2025)
-
Effect of light-emitting diode photobiomodulation on rat liver metabolomics after streptozotocin-induced diabetes – an evidence from nuclear magnetic resonance spectroscopy
Lasers in Medical Science (2025)