Abstract
FLASH radiotherapy holds promise for treating solid tumors given the potential lower toxicity in normal tissues but its therapeutic effects on tumor immunity remain largely unknown. Using a genetically engineered mouse model of medulloblastoma, we show that FLASH radiation stimulates proinflammatory polarization in tumor macrophages. Single-cell transcriptome analysis shows that FLASH proton beam radiation skews macrophages toward proinflammatory phenotypes and increases T cell infiltration. Furthermore, FLASH radiation reduces peroxisome proliferator-activated receptor-γ (PPARγ) and arginase 1 expression and inhibits immunosuppressive macrophage polarization under stimulus-inducible conditions. Mechanistically, FLASH radiation abrogates lipid oxidase expression and oxidized low-density lipid generation to reduce PPARγ activity, while standard radiation induces reactive oxygen species-dependent PPARγ activation in macrophages. Notably, FLASH radiotherapy improves infiltration and activation of chimeric antigen receptor (CAR) T cells and sensitizes medulloblastoma to GD2 CAR-T cell therapy. Thus, FLASH radiotherapy reprograms macrophage lipid metabolism to reverse tumor immunosuppression. Combination FLASH–CAR radioimmunotherapy may offer exciting opportunities for solid tumor treatment.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
Single-cell and bulk RNAseq data were deposited to the National Center for Biotechnology Information’s Gene Expression Omnibus under accession numbers GSE246970 and GSE246969, respectively. All remaining data are available within the article and the Supplementary Information or available from the authors upon request. Source data are provided with this paper.
References
Gajjar, A. J. & Robinson, G. W. Medulloblastoma—translating discoveries from the bench to the bedside. Nat. Rev. Clin. Oncol. 11, 714–722 (2014).
Northcott, P. A. et al. Medulloblastoma. Nat. Rev. Dis. Primers 5, 11 (2019).
Zhao, J. et al. Immune and genomic correlates of response to anti-PD-1 immunotherapy in glioblastoma. Nat. Med. 25, 462–469 (2019).
O’Rourke, D. M. et al. A single dose of peripherally infused EGFRvIII-directed CAR-T cells mediates antigen loss and induces adaptive resistance in patients with recurrent glioblastoma. Sci. Transl. Med. 9, eaaa0984 (2017).
Xie, Y. J. et al. Nanobody-based CAR-T cells that target the tumor microenvironment inhibit the growth of solid tumors in immunocompetent mice. Proc. Natl Acad. Sci. USA 116, 7624–7631 (2019).
Datta, M., Coussens, L. M., Nishikawa, H., Hodi, F. S. & Jain, R. K. Reprogramming the tumor microenvironment to improve immunotherapy: emerging strategies and combination therapies. Am. Soc. Clin. Oncol. Educ. Book 39, 165–174 (2019).
Morantz, R. A., Wood, G. W., Foster, M., Clark, M. & Gollahon, K. Macrophages in experimental and human brain tumors. Part 2: studies of the macrophage content of human brain tumors. J. Neurosurg. 50, 305–311 (1979).
Hambardzumyan, D., Gutmann, D. H. & Kettenmann, H. The role of microglia and macrophages in glioma maintenance and progression. Nat. Neurosci. 19, 20–27 (2016).
Pollard, J. W. Tumour-educated macrophages promote tumour progression and metastasis. Nat. Rev. Cancer 4, 71–78 (2004).
Ruffell, B. & Coussens, L. M. Macrophages and therapeutic resistance in cancer. Cancer Cell 27, 462–472 (2015).
Ostuni, R., Kratochvill, F., Murray, P. J. & Natoli, G. Macrophages and cancer: from mechanisms to therapeutic implications. Trends Immunol. 36, 229–239 (2015).
Sica, A. & Mantovani, A. Macrophage plasticity and polarization: in vivo veritas. J. Clin. Invest. 122, 787–795 (2012).
Murray, P. J. & Wynn, T. A. Protective and pathogenic functions of macrophage subsets. Nat. Rev. Immunol. 11, 723–737 (2011).
Stein, M., Keshav, S., Harris, N. & Gordon, S. Interleukin 4 potently enhances murine macrophage mannose receptor activity: a marker of alternative immunologic macrophage activation. J. Exp. Med. 176, 287–292 (1992).
Weber, M. S. et al. Type II monocytes modulate T cell-mediated central nervous system autoimmune disease. Nat. Med. 13, 935–943 (2007).
Golden, E. B., Marciscano, A. E. & Formenti, S. C. Radiation therapy and the in situ vaccination approach. Int. J. Radiat. Oncol. Biol. Phys. 108, 891–898 (2020).
Ibuki, Y. & Goto, R. Contribution of inflammatory cytokine release to activation of resident peritoneal macrophages after in vivo low-dose γ-irradiation. J. Radiat. Res. 40, 253–262 (1999).
Hosoi, Y. et al. Induction of interleukin-1β and interleukin-6 mRNA by low doses of ionizing radiation in macrophages. Int. J. Cancer 96, 270–276 (2001).
Klug, F. et al. Low-dose irradiation programs macrophage differentiation to an iNOS+/M1 phenotype that orchestrates effective T cell immunotherapy. Cancer Cell 24, 589–602 (2013).
O’Brien-Ladner, A., Nelson, M. E., Kimler, B. F. & Wesselius, L. J. Release of interleukin-1 by human alveolar macrophages after in vitro irradiation. Radiat. Res. 136, 37–41 (1993).
Russell, J. S. & Brown, J. M. The irradiated tumor microenvironment: role of tumor-associated macrophages in vascular recovery. Front. Physiol. 4, 157 (2013).
Shao, J., Welch, W. J., Diprospero, N. A. & Diamond, M. I. Phosphorylation of profilin by ROCK1 regulates polyglutamine aggregation. Mol. Cell. Biol. 28, 5196–5208 (2008).
Tsai, C. S. et al. Macrophages from irradiated tumors express higher levels of iNOS, arginase-I and COX-2, and promote tumor growth. Int. J. Radiat. Oncol. Biol. Phys. 68, 499–507 (2007).
Vozenin, M. C., Hendry, J. H. & Limoli, C. L. Biological benefits of Ultra-high Dose Rate FLASH radiotherapy: sleeping beauty awoken. Clin. Oncol. (R. Coll. Radiol.) 31, 407–415 (2019).
Favaudon, V. et al. Ultrahigh dose-rate FLASH irradiation increases the differential response between normal and tumor tissue in mice. Sci. Transl. Med. 6, 245ra293 (2014).
de Kruijff, R. M. FLASH radiotherapy: ultra-high dose rates to spare healthy tissue. Int. J. Radiat. Biol. 96, 419–423 (2020).
Velalopoulou, A. et al. FLASH proton radiotherapy spares normal epithelial and mesenchymal tissues while preserving sarcoma response. Cancer Res. 81, 4808–4821 (2021).
Mascia, A. E. et al. Proton FLASH radiotherapy for the treatment of symptomatic bone metastases: the FAST-01 nonrandomized trial. JAMA Oncol. 9, 62–69 (2023).
Montay-Gruel, P. et al. Long-term neurocognitive benefits of FLASH radiotherapy driven by reduced reactive oxygen species. Proc. Natl Acad. Sci. USA 116, 10943–10951 (2019).
Menjivar, R. E. et al. Arginase 1 is a key driver of immune suppression in pancreatic cancer. eLife 12, e80721 (2023).
Wang, Q. et al. Vascular niche IL-6 induces alternative macrophage activation in glioblastoma through HIF-2α. Nat. Commun. 9, 559 (2018).
Itoh, T. et al. Structural basis for the activation of PPARγ by oxidized fatty acids. Nat. Struct. Mol. Biol. 15, 924–931 (2008).
Reaven, P. et al. Effects of oleate-rich and linoleate-rich diets on the susceptibility of low density lipoprotein to oxidative modification in mildly hypercholesterolemic subjects. J. Clin. Invest. 91, 668–676 (1993).
Paret, C. et al. GD2 expression in medulloblastoma and neuroblastoma for personalized immunotherapy: a matter of subtype. Cancers (Basel) 14, 6051 (2022).
Del Bufalo, F. et al. GD2-CART01 for relapsed or refractory high-risk neuroblastoma. N. Engl. J. Med. 388, 1284–1295 (2023).
Sampson, J. H. et al. EGFRvIII mCAR-modified T-cell therapy cures mice with established intracerebral glioma and generates host immunity against tumor-antigen loss. Clin. Cancer Res. 20, 972–984 (2014).
Ma, W. et al. Targeting PAK4 to reprogram vascular microenvironment and improve CAR-T immunotherapy for glioblastoma. Nat. Cancer 2, 83–97 (2021).
Hornsey, S. & Alper, T. Unexpected dose-rate effect in the killing of mice by radiation. Nature 210, 212–213 (1966).
Town, C. D. Effect of high dose rates on survival of mammalian cells. Nature 215, 847–848 (1967).
Wisdom, A. J. et al. Single cell analysis reveals distinct immune landscapes in transplant and primary sarcomas that determine response or resistance to immunotherapy. Nat. Commun. 11, 6410 (2020).
Shukla, S. et al. Ultra-high dose-rate proton FLASH improves tumor control. Radiother. Oncol. 186, 109741 (2023).
Montay-Gruel, P. et al. Hypofractionated FLASH-RT as an effective treatment against glioblastoma that reduces neurocognitive side effects in mice. Clin. Cancer Res. 27, 775–784 (2021).
Ricote, M., Huang, J. T., Welch, J. S. & Glass, C. K. The peroxisome proliferator-activated receptor (PPARγ) as a regulator of monocyte/macrophage function. J. Leukoc. Biol. 66, 733–739 (1999).
Peters, J. M., Shah, Y. M. & Gonzalez, F. J. The role of peroxisome proliferator-activated receptors in carcinogenesis and chemoprevention. Nat. Rev. Cancer 12, 181–195 (2012).
Nagy, L., Tontonoz, P., Alvarez, J. G., Chen, H. & Evans, R. M. Oxidized LDL regulates macrophage gene expression through ligand activation of PPARγ. Cell 93, 229–240 (1998).
Marx, N., Bourcier, T., Sukhova, G. K., Libby, P. & Plutzky, J. PPARγ activation in human endothelial cells increases plasminogen activator inhibitor type-1 expression: PPARγ as a potential mediator in vascular disease. Arterioscler. Thromb. Vasc. Biol. 19, 546–551 (1999).
Schild, R. L. et al. The activity of PPARγ in primary human trophoblasts is enhanced by oxidized lipids. J. Clin. Endocrinol. Metab. 87, 1105–1110 (2002).
Spitz, D. R. et al. An integrated physico-chemical approach for explaining the differential impact of FLASH versus conventional dose rate irradiation on cancer and normal tissue responses. Radiother. Oncol. 139, 23–27 (2019).
Epp, E. R., Weiss, H., Djordjevic, B. & Santomasso, A. The radiosensitivity of cultured mammalian cells exposed to single high intensity pulses of electrons in various concentrations of oxygen. Radiat. Res. 52, 324–332 (1972).
Ling, C. C., Michaels, H. B., Epp, E. R. & Peterson, E. C. Oxygen diffusion into mammalian cells following ultrahigh dose rate irradiation and lifetime estimates of oxygen-sensitive species. Radiat. Res. 76, 522–532 (1978).
Adrian, G. et al. The FLASH effect depends on oxygen concentration. Br. J. Radiol. 93, 20190702 (2020).
Buonanno, M., Grilj, V. & Brenner, D. J. Biological effects in normal cells exposed to FLASH dose rate protons. Radiother. Oncol. 139, 51–55 (2019).
Fouillade, C. et al. FLASH irradiation spares lung progenitor cells and limits the incidence of radio-induced senescence. Clin. Cancer Res. 26, 1497–1506 (2020).
Ciccone, R. et al. GD2-targeting CAR-T-cell therapy for patients with GD2+ medulloblastoma. Clin. Cancer Res. 30, 2545–2557 (2024).
Majzner, R. G. et al. GD2-CAR T cell therapy for H3K27M-mutated diffuse midline gliomas. Nature 603, 934–941 (2022).
Thomas, B. C. et al. CAR-T cell therapies for diffuse midline glioma. Trends Cancer 9, 791–804 (2023).
Kim, Y. E. et al. Effects of ultra-high doserate FLASH irradiation on the tumor microenvironment in Lewis lung carcinoma: role of myosin light chain. Int. J. Radiat. Oncol. Biol. Phys. 109, 1440–1453 (2021).
Allen, B. D. et al. Elucidating the neurological mechanism of the FLASH effect in juvenile mice exposed to hypofractionated radiotherapy. Neuro Oncol. 25, 927–939 (2023).
Zhang, D. et al. PHGDH-mediated endothelial metabolism drives glioblastoma resistance to chimeric antigen receptor T cell immunotherapy. Cell Metab. 35, 517–534 (2023).
Zhang, D. et al. Protocol to generate traceable CAR-T cells for syngeneic mouse cancer models. STAR Protoc. 5, 102898 (2024).
Liu, Y. et al. Somatic cell type specific gene transfer reveals a tumor-promoting function for p21(Waf1/Cip1). EMBO J. 26, 4683–4693 (2007).
Ciznadija, D., Liu, Y., Pyonteck, S. M., Holland, E. C. & Koff, A. Cyclin D1 and cdk4 mediate development of neurologically destructive oligodendroglioma. Cancer Res. 71, 6174–6183 (2011).
Fan, Y. et al. Profilin-1 phosphorylation directs angiocrine expression and glioblastoma progression through HIF-1α accumulation. Nat. Cell Biol. 16, 445–456 (2014).
Huang, M. et al. c-Met-mediated endothelial plasticity drives aberrant vascularization and chemoresistance in glioblastoma. J. Clin. Invest. 126, 1801–1814 (2016).
Diffenderfer, E. S. et al. Design, implementation, and in vivo validation of a novel proton FLASH radiation therapy system. Int. J. Radiat. Oncol. Biol. Phys. 106, 440–448 (2020).
International Atomic Energy Agency. Absorbed Dose Determination in External Beam Radiotherapy: An International Code of Practice for Dosimetry Based on Standards of Absorbed Dose to Water. Technical Reports Series no. 398 (IAEA, 2001).
Zou, W. et al. Framework for quality assurance of ultrahigh dose rate clinical trials investigating FLASH effects and current technology gaps. Int. J. Radiat. Oncol. Biol. Phys. 116, 1202–1217 (2023).
Hao, Y. et al. Integrated analysis of multimodal single-cell data. Cell 184, 3573–3587 (2021).
Hafemeister, C. & Satija, R. Normalization and variance stabilization of single-cell RNA-seq data using regularized negative binomial regression. Genome Biol. 20, 296 (2019).
Yang, F. et al. Synergistic immunotherapy of glioblastoma by dual targeting of IL-6 and CD40. Nat. Commun. 12, 3424 (2021).
Yang, F. et al. Small-molecule toosendanin reverses macrophage-mediated immunosuppression to overcome glioblastoma resistance to immunotherapy. Sci. Transl. Med. 15, eabq3558 (2023).
Acknowledgements
We are grateful to J. Billings for help with single-cell RNAseq analysis. This work was supported in part by the University of Pennsylvania Abramson Cancer Center Radiation Oncology Translational Center for Excellence (to Y.F.), National Institutes of Health grants R01NS094533 (to Y.F.), R01NS106108 (to Y.F.), R01CA241501 (to J.F.D. and Y.F.), R01HL106108 (to Y.F. and Y.G.), R35CA197616 (to D.G.K), P01CA257904 (to A.J.M., C.K. and D.G.K.) and K08CA256045 (to Z.J.R.) and developmental funds from P30CA014236 (to Z.J.R.) and P50CA190991 Duke SPORE in Brain Cancer (to Z.J.R. and D.G.K.), a Yosemite Award from the American Cancer Society (to Y.F.), a Mark Foundation grant (to A.J.M.), a Pediatric Brain Tumor Foundation grant (to Z.J.R.), a St. Baldrick’s Foundation grant (to Z.J.R.), a Chadtough Defeat DIPG grant (to Z.J.R.) and an Alex’s Lemonade Stand Foundation grant (to Z.J.R.).
Author information
Authors and Affiliations
Contributions
H.N. performed the experiments, analyzed the results and produced the figures. Z.J.R. designed the experiments. W.Z. and S.A.O.M. conducted the radiation dosimetry and delivery. M.N.A. and R.M. helped with the T cell assays. R.P. and M.H. contributed to the initial in vivo RT experiments. D.Z. and L.Z. contributed to the bioinformatic analysis. H.Z., R.Z. and G.N. helped with the experimental assays. J.B.F. contributed to the GD2 CAR-T treatment. E.S.D., M.M.K., A.M., J.F.D., J.M. and C.K. contributed to the FLASH physics and RT. D.G.K., Y.G. and Y.F. contributed to the experimental design and data interpretation. D.G.K., Y.G. and Y.F. supervised the project. Y.F. conceptualized the ideas and wrote the manuscript. All authors commented on the manuscript.
Corresponding authors
Ethics declarations
Competing interests
D.G.K. is a cofounder of and stockholder in XRAD Therapeutics, which is developing radiosensitizers. D.G.K. is a member of the scientific advisory board and owns stock in Lumicell, a company commercializing intraoperative imaging technology. None of these affiliations represent a conflict of interest with respect to the work of this manuscript. D.G.K. is a coinventor on a patent for a handheld imaging device and is a coinventor on a patent for radiosensitizers. None of these patents are relevant to this manuscript. XRAD Therapeutics, Merck, Bristol Myers Squibb and Varian Medical Systems have provided research support to D.G.K. but this did not support the research described in this manuscript. Z.J.R. is listed as an inventor for intellectual property related to genetic testing for brain tumors that is managed by Duke Office of Licensing and Ventures, which is not relevant to this manuscript. The other authors declase no competing interests.
Peer review
Peer review information
Nature Cancer thanks Niels Bovenschen, Aaron Diaz, Ping-Chih Ho and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Effects of RT on tumor-associated Mfs, microglia, and NK cells.
Medulloblastoma was genetically engineered in SmoM2 mice, followed by irradiation with FLASH or standard proton beam. Tumors were excised and subjected to flow cytometry analysis. a, Gating strategies for analysis of T cells and Mϕs, corresponding to Fig. 1i–o. b-e, Analysis for b, CD11b+F4/80+ total Mϕs (n = 5 mice), c, CD45LowCD11b+TMEM119+ total microglia (n = 12 mice for no RT group, and n = 11 mice for FLASH and standard RT groups), d, CD86+ M1-like (n = 5 mice) and CD206+ M2-like microglia (n = 6 mice), and e, NK1.1+ NK cells (n = 6 mice). Statistical analysis by one-way ANOVA (mean ± SEM).
Extended Data Fig. 2 Effects of RT on human Mf polarization in vitro.
Human PBMC-derived Mϕs were irradiated with FLASH or standard proton beam, followed by treatment with LPS or IL-4. a, Experimental procedure. b,c, After treatment with b, LPS or c, IL-4, cells were analyzed by flow cytometry. Left, representative cell sortings. Right, quantified results (n = 3 human participants, mean ± SEM). b, Statistical analysis by two-tailed Student’s t test. c, Statistical analysis by one-way ANOVA.
Extended Data Fig. 3 Effects of irradiated Mfs on T cell functions in vitro.
Human PBMC-derived Mϕs cells were irradiated by FLASH or standard proton beam and treated with IL-4 for 2 days. Human PBMC-derived CD3+ T cells were stimulated with CD3/CD28 beads for 3 days, and loaded with CFSE. Treated Mϕs and T cells were incubated for 2 days, followed by flow cytometry analysis. a, CFSE was analyzed in CD3+ T cells. Left, representative cell sortings. Right, quantified results (n = 3 human participants, mean ± SEM). Statistical analysis by one-way ANOVA. b, CD25 expression was analyzed in CD3+ T cells. Left, representative cell sortings. Right, quantified results (n = 3 human participants, mean ± SEM). Statistical analysis by one-way ANOVA.
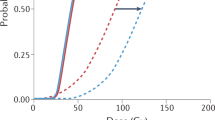
Extended Data Fig. 4 Effects of RT on ROS generation, PPARg activity and oxLDL production in human Mfs.
Human PBMC-derived Mϕs were irradiated with FLASH or standard proton beam. a, Total ROS were analyzed at different time post-irradiation (mean ± SEM, n = 3 human participants). b, PPARγ activity was measured 24 h after irradiation (mean ± SEM, n = 5 human participants). Statistical analysis by one-way ANOVA. c, Human PBMC-derived Mϕs were irradiated with FLASH or standard proton beam, followed by treatment with or without IL-4. Cell lystes were subjected to oxLDL analysis (mean ± SEM, n = 6 human participants). Statistical analysis by one-way ANOVA.
Extended Data Fig. 5 Effects of RT on trancriptional factor activity in vitro.
Mouse BM-derived Mϕs (pooled from 3 mouse samples for each group) were irradiated with FLASH or standard proton beam, and subjected to analysis with a transcriptional factor profiling assay. The activity of 96 transcriptional factors was expressed as the fold of no RT group. a, Heatmap. b, Ranked activity.
Extended Data Fig. 6 Combination of RT with CAR T cell therapy in a syngeneic mouse glioma model.
Glioma was induced in mice by orthotopic transplantation with GL261 mouse glioma cells, followed by FLASH or standard RT and GD2 CAR-T cell therapy. a, Experimental procedures. b, Animal survival was monitored for 60 days (n = 10 mice). Statistical analysis by a two-tailed Log-rank Mantel-Cox test. c, Tumor volume was measured by bioluminescence imaging (n = 10 mice, mean ± SEM). Note: after standard RT plus CAR T cell treatment, one mouse developed neurological symptoms at late day 26 and was imaged at day 27. Statistical analysis by two-way ANOVA.
Extended Data Fig. 7 Effects of RT on CAR T infiltration and activity in vivo.
a-c, 5 days after irradiation, SmoM2 mice were treated with GD2 CAR-T cells. a, Experimental procedures. b,c, Tumors were excised 7 days after CAR-T cell therapy, followed by flow cytometry analysis. (b, Analysis of GFP+ CAR-T cells (n = 6 mice, mean ± SEM). Statistical analysis by one-way ANOVA. c, Analysis of IFN-g+, Ki-67+, Lag-3+, PD-1+ and Tim-3+ GFP+ CAR T cells (n = 4 mice, mean ± SEM). Statistical analysis by two-way ANOVA. d-e, 3 days after irradiation, SmoM2 mice were treated with GD2 CAR-T cells. d, Experimental procedures. e,f, Tumors were excised 3 days after CAR-T cell therapy, followed by flow cytometry analysis. e, Analysis of GFP+ CAR T cells (n = 3 mice, mean ± SEM). Statistical analysis by one-way ANOVA. f, Analysis of IFN-g+, Ki-67+, Lag-3+, PD-1+ and Tim-3+ GFP+ CAR T cells (n = 3 mice, mean ± SEM). Statistical analysis by two-way ANOVA.
Supplementary information
Source data
Source Data Fig. 1
Statistical source data.
Source Data Extended Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 3
Unprocessed western blots.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 4
Unprocessed western blots.
Source Data Extended Data Fig. 4
Statistical source data.
Source Data Fig. 5
Statistical source data.
Source Data Extended Data Fig. 5
Statistical source data.
Source Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 7
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ni, H., Reitman, Z.J., Zou, W. et al. FLASH radiation reprograms lipid metabolism and macrophage immunity and sensitizes medulloblastoma to CAR-T cell therapy. Nat Cancer 6, 460–473 (2025). https://doi.org/10.1038/s43018-025-00905-6
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s43018-025-00905-6
This article is cited by
-
Nuclear receptors as novel regulators that modulate cancer radiosensitivity and normal tissue radiotoxicity
Molecular Cancer (2025)
-
Strategies to overcome tumour relapse caused by antigen escape after CAR T therapy
Molecular Cancer (2025)
-
FLASH radiotherapy at a crossroads: a bibliometric perspective on progress and challenges
Discover Oncology (2025)
-
Tissue-specific iron levels modulate lipid peroxidation and the FLASH radiotherapy effect
Cell Death & Disease (2025)