Abstract
Childhood respiratory diseases remain a major global health concern, with school-centered exposures to air pollution and extreme temperatures posing significant risks. We conducted a spatiotemporal stratified multi-city, school-based design to evaluate underexplored risk patterns of fine particulate matter with an aerodynamic diameter ≤1 µm, nitrate, sulfate, ammonium, chloride, black carbon, and temperature exposures including daily mean, extremes, and short-term variability. The analysis included 265,076 pneumonia and/or tracheitis cases among schoolchildren in Jiangsu Province, China. We observed significant urban–rural disparities and spatial clustering in air pollution and temperature variation. Cumulative exposure to all pollutants was positively associated with increased risk of illness-related absences, with stronger effects observed in urban schools and during low-temperature conditions overall. Boys showed higher initial sensitivity to air pollution, while girls exhibited greater vulnerability after 10–14 days. Notably, urban children were most affected by combined exposures to low temperature-high pollution, whereas rural children experienced greater combined risks under high-temperature conditions. In contrast, short-term temperature variability contributed minimally to the observed health effects. These findings support the development of early warning systems for composite exposures, informed by exposure–risk profiles, to enable timely school intervention and protect schoolchildren’s respiratory health.
Similar content being viewed by others
Introduction
Protecting children’s respiratory health is a critical global public health priority, as respiratory diseases significantly contribute to morbidity and mortality in early childhood1. Among these, pneumonia and tracheitis represent major health burdens, with childhood pneumonia alone causing approximately 740,180 deaths annually among children under the age of five, accounting for 14% of all deaths in this age group2. This burden is especially severe in low- and middle-income countries, where environmental pollution, inadequate sanitation, and limited healthcare access to exacerbate the risks of pneumonia and other respiratory diseases3,4.
Children’s immature immune and respiratory systems heighten their susceptibility to environmental exposures5. Non-optimal temperature, defined as a deviation from the theoretical minimum risk exposure level6, encompassing both cold and heat exposures, has been shown to contribute to childhood respiratory distress7,8,9. Cold reduces mucociliary clearance and immune defenses8, while heat triggers airway inflammation and oxidative stress, worsening respiratory conditions10,11. O3 exposure induces oxidative stress, epithelial injury, and bronchial hyperreactivity12, and PM exposure exacerbates airway inflammation, causes oxidative DNA damage, and alters gene expression13,14,15. For instance, emerging evidence links air pollution exposures (e.g., PM2.5 and PM10) to childhood respiratory illnesses across multiple developmental stages, with effects potentially amplified during susceptibility windows under non-optimal temperatures through synergistic interactions15,16,17,18. Pneumonia primarily affects the alveoli and lung interstitium, causing fever and productive cough, and tracheitis inflames the tracheal mucosa, leading to dry cough, sore throat, and airway obstruction, both of which may result in respiratory distress19.
While the health effects of certain environmental exposures are well established based on clinical and mortality records4,20,21,22, risks linked to chemical composition and finer particles remain underexplored among children. Due to smaller size and larger surface area, PM1 could absorb toxic substances, penetrate deep into lung tissue, and enter the bloodstream, potentially amplifying health risks23,24. Moreover, the increasing frequency of extreme temperatures and fluctuations, combined with air pollution, may heighten respiratory risks25,26, yet evidence specific to children’s respiratory health remains insufficient, particularly regarding the role of chemical composition.
Given that children spend over 30% of their waking hours in school, school environment serves as a critical nexus between health, learning, and overall well-being, thus a more comprehensive framework is needed to assess broader health response and developmental consequences for schoolchildren27. Illness-related absences driven by environmental stressors not only impose health burdens but also lead to learning disruptions, with chronic absenteeism increasingly recognized as a risk factor for long-term socioeconomic disparities28. We hypothesize that air pollution and temperature independently and jointly contribute to school absenteeism due to childhood pneumonia and/or tracheitis, warranting investigation within school-based environmental contexts.
This study aims to evaluate the combined effects of extreme temperatures-including daily mean, max and min, inter-day change, and intra-day fluctuation-and air pollutants, including fine particulate matter with a diameter ≤1 µm (PM1), black carbon (BC), nitrate (NO3−), sulfate (SO42−), chloride (Cl−), and ammonium (NH4+), on schoolchildren’s respiratory health in Jiangsu Province, China. The multi-city, school-based study will provide essential evidence on the combined health impacts of temperature extremes and particulate matter pollution on schoolchildren’s illness-related absence due to pneumonia and/or tracheitis across urban and rural settings.
Results
Characteristics of school environment and cases
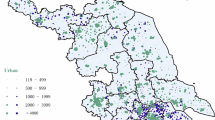
The average age of children with pneumonia and/or tracheitis was 7.34 ± 3.31 years, with boys constituting 52.95%. Notably, 44.64% of these cases occurred during winter, and 82.16% originated from urban schools (Supplementary Notes). Spatial analysis revealed that, rural cases were predominantly clustered in the northwest and southeast regions (Figs. 1 and S20); in particular, the northwest exhibited significantly higher overall particulate matter levels (Moran’s I 0.67–0.92, p < 0.001). Although the global spatial clustering of school average annual average temperature was very weak (Moran’s I −0.001 to 0.07, p < 0.05), we found the with higher temperature fluctuations detected in the northwest and central regions (p < 0.05, Fig. S21). In contrast, the spatial patterns for school green space coverage (Moran’s I = 0.85, p < 0.001) and road density (Moran’s I = 0.89, p < 0.001) were strongly clustered, particularly in the southeast where lower green space and higher road density coincided with higher counts of pneumonia and/or tracheitis. Additionally, strong associations emerged between pollutant concentrations and temperature conditions; higher pollution levels were generally linked to lower ambient temperatures and greater intra-day as well as diurnal temperature variations (p < 0.05, Fig. 1). Schools with larger student bodies also demonstrated weak positive correlations with increased pollution and temperature fluctuations (correlation coefficients 0.03–0.11, p < 0.05). Inter-group comparisons indicated that BC exposure and road density was significantly higher in urban schools (p < 0.001), whereas rural schools have higher green space coverage, but are more adjacent to factories and have serious PM1, NH4+, Cl−, and SO42− pollution (p < 0.001) (Figs. S22, 23).
a Urban (blue point) and rural (red point) school distribution and size characteristics, where the point size represent the schoolchildren number. b Spearman correlation between air pollution and temperature indicators, where T2m_var and T2m_sd represent the variance and standard deviation of the average daily temperature over the past period. c–e Spatial distribution of daily air pollution, ambient temperature environment, and land use characteristics, with annual global Moran’s index as well as mean and standard deviation provided.
Pollution exposure risk assessment
Figure 2 showed the associations between independent exposure to air pollutants and and the daily absences of childhood pneumonia and/or tracheitis. For cumulative 0–14 day exposures, the six particulate matter pollutants demonstrated consistent upward risk trends, with relative risks ranging from 1.014 to 1.119 and SO42- posing the highest threats of 1.119 [95% CI, 1.101-1.137] to school attendance. We found that urban school children faced higher absence risks associated with various exposure (urban RR 1.010-1.023, rural RR 1.007–1.020). There was almost no significant risk associated with pollution exposure in spring except BC, which showed robust risk associations in all seasons (RR 1.031–1.214, p < 0.05) and the highest threats occurred in summer Cl− exposure (RR 1.353 [1.158, 1.581]) (Fig. S4). Lag effect analysis indicated that boys experienced higher risks within the initial seven days, whereas after a 10-14 day lag, risks for girls exceeded those for boys (Fig. S15).
Health threats from non-optimal temperatures
We found that both low and high ambient temperatures were associated with elevated relative risks of pneumonia and/or tracheitis related absences among children (Fig. 3). It was noted that low temperature exposures are consistantly significantly associated with elevated risk. In the low temperature segment ranging from the 5th percentile at 2.12 °C to the 25th percentile at 7.17 °C, the relative risk estimates span 1.020 to 1.079, with the highest risk observed under cumulative 7-days’ exposure at the 5th percentile (RR 1.079 [95% CI: 1.057, 1.103], p < 0.01). In contrast, the risk association of high temperature exposure was less robust, with consistent positive associations observed only in the 20th (21.85 °C) to 25th (20.71 °C) percentile temperature range (RR 1.016–1.059).
a Various temperature-stratified risk trends with comfort temperature range as reference. b Seasonal patterns of cumulative 14-days’ exposure-response. c Gender differences in cumulative 14-days’ high and low temperature conditions (25% stratification). d Relative risks of lag_0 exposure to each unit increase in pollution concentration under different temperature ranges (25% stratification).
The exposure–response curves consistently reveal a superlinear risk trend in the low temperature range across seasons, with an overall risk threshold below 12.5 °C (Fig. 3). Moreover, gender stratification indicates that boys are more susceptible in low temperature conditions (RR 1.100 [1.070, 1.131]) compared to girls (RR 1.053 [1.024, 1.083]), while high temperature effects are not statistically significant (p > 0.05).
The 0–14 days lag analysis revealed distinct risk trends associated with DAT between urban and rural schools (Fig. S12). In urban schools, risk persisted with a stable trend during low-temperature periods, while rural schools showed a weaker association. Sensitivity analyses confirm that daily maximum temperatures below 15 °C and minimum temperatures below 5 °C exhibit consistent exposure–response patterns, while IDF was weakly associated with increased risk in a few lagged days and showed regional and gender differences, and IDC always showed no significant impacts (Figs. S7–S10).
Elevated respiratory health risks among combined exposures
Subgroup analyses reveal that the adverse effects posed by the six pollutants were consistently higher in low temperature environments than in the comfortable and high temperature intervals, with RR estimates ranging from 1.059 to 1.087 (p < 0.001, Fig. 3d). Figure 4 illustrates that the joint exposure to six particulate matter pollutants and non-optimal temperature conditions substantially elevates the risk of school absences due to pneumonia and/or tracheitis, with pronounced urban–rural exposure risk heterogeneity. Under low temperature scenarios, relative risks ranged from 1.018 to 1.095, compared with 0.999–1.131 under high temperature conditions. Notably, based on comfortable temperature-low pollution baseline, rural children faced significantly higher risks (except BC) under high temperature and high pollution conditions (RR 1.067–1.134, p < 0.05), whereas urban children were more adversely affected by the combined exposure to low temperature and high pollution (RR 1.075–1.095, p < 0.001). Overall, the combined exposure risk in low temperature settings (RR 1.065–1.086, p < 0.001) consistently exceeded that of pollution alone (RR 1.035–1.055, p < 0.001), underscoring the amplified risks of non-optimal environments (Fig. 4).
We stratified by the 25th percentile of daily average temperature, The 0–0 (comfortable temperature–low pollution) is set as the reference, with the remaining groups defined as 0–1 (comfortable temperature–high pollution), 1–0 (low temperature–low pollution), 1–1 (low temperature–high pollution), 2–0 (high temperature–low pollution), and 2–1 (high temperature–high pollution).
Discussion
Through a multi-city, school-based spatiotemporal stratified design, this study provides critical evidence on the burden of illness-related absence driven by the combined effects of typical air pollutants and extreme temperature. By examining 14-day cumulative exposures to PM1, BC, NO₃−, SO₄2−, Cl−, and NH₄+, alongside extreme temperatures in both urban and rural schools, we found consistent associations between particulate matter pollution and increased absenteeism due to pneumonia and/or tracheitis with rising cumulative risks, particularly under low-temperature conditions. Combined exposure scenarios, especially low temperature-high pollution, posed greater health risks across all schools. The findings reveal seasonal, gender-based, and healthcare-related variations in relative risks and exposure-response trends, underscoring the need for targeted school health interventions to protect schoolchildren’s respiratory health.
Although emerging evidence has demonstrated the health effects of PM2.5 and PM1029,30, there is still a lack of understanding of the toxic impacts of exposure to related components and finer particles, especially for schoolchildren’s living environment. This study addresses this gap, demonstrating the significant adverse effects of PM1 and main chemical composition on schoolchildren’s respiratory system, as indicated by school attendance behavior. We identified increasing health risks linked to cumulative exposure than evidence from hospital records14, with gender-specific trends that boys faced higher risks initially, while girls experienced greater vulnerability with prolonged exposure (10–14 days). This difference may arise from differences in alveolar surface area development and particle deposition patterns, with boys potentially facing greater early exposure risk due to higher levels of physical activity, while girls may be more vulnerable to prolonged exposure effects due to cumulative oxidative stress, delayed inflammatory responses, and hormonal regulation31,32,33. Estrogen, for instance, has been implicated in modulating immune function, which may influence inflammatory trajectories34,35. Additionally, sociocultural factors36,37, such as differences in care-seeking behavior, symptom reports, and perceived severity, may also play a role in shaping the sex-specific pattern, warranting further investigation combined family-level health surveys.
Rural schools were located near more factories and had higher exposure levels to PM1, NH4+, Cl−, and SO42−; meanwhile, children in urban areas are more densely populated and may be more susceptible to toxic heavy metals and black carbon produced by motor vehicle exhaust emissions on high-density roads15,38. The assessment of exposure- response risk for urban and rural children should focus on differences in adjacent spatial characteristics and pollution sources. Attention should be given to ensuring adequate health resources and strictly controlling factory emissions for rural children, while also addressing the risks associated with dense population, high road density, and less green space faced by urban children. These findings highlight the need for urban-rural, gender and emission source specific strategies for particulate matter pollution mitigation and respiratory health interventions.
Studies from northern China, Qatar, Japan, and the United States consistently report associations between PM exposure and school absences due to illness39,40,41,42,43, although evidence comparing PM1 or chemical components in relation to childhood respiratory disease-related absenteeism remains limited. Even low air pollution levels may affect school attendance, with disproportionate impacts on schools in disadvantaged areas39. A nationwide case-crossover study in China found that particulate matter exposure is linked to distinct respiratory outcomes across age groups, with children showing heightened susceptibility44. PM2.5 was more closely associated with tracheitis, while PM2.5-10 was linked to pneumonia44, highlighting the importance of distinguishing particle size, their adsorbed components, and patterns of respiratory deposition.
Moreover, O3 has always been a focus of attention in respiratory health caused by air pollution45. Hence, we controlled O3 concentrations in PM pollution-focused models because we also found significantly higher absence risk from exposure to O3 and extreme temperatures (Fig. S2). O3 may affect respiratory health through different mechanisms, primarily causing oxidative stress, airway inflammation, and ciliary dysfunction, leading to bronchial irritation and increased susceptibility to infection45. This underscores the need to not only focus on PM pollution as highlighted in this study, but also more efforts are needed to control various air pollutants to better protect children from both acute and chronic respiratory diseases.
Non-optimal temperature exposures have been linked to increased respiratory hospitalizations and specific illness incidence among children in Ho Chi Minh City, Vietnam, and several Chinese cities11,16,46,47. Extending this evidence, our findings reveal similar robust associations between both low and high temperatures and reduced school attendance. Notably, low temperatures appear to exert a more persistent and pronounced impact on school attendance due to pneumonia and/or tracheitis. This may be attributed to low temperature-induced immune suppression, reduced alveolar macrophage activity, and increased pathogen transmission and colonization facilitated by prolonged indoor crowding48. Although our temperature-segmented model detected overall risks associated with high temperatures, these effects nearly disappeared in the exposure-response curve, suggesting that high temperatures may pose more subtle risks via indirect mechanisms such as heightened inflammatory responses, systemic heat stress, and synergistic interactions with air pollution, which together exacerbate airway inflammation and disease susceptibility12,48. In addition, urban children appear to experience heightened risks associated with inter-day temperature drops, potentially due to dense urban infrastructure and materials with high thermal conductivity that amplify respiratory stress49.
The seasonal pattern of childhood pneumonia and/or tracheitis further reinforces the findings of temperature stratification and season-stratified models, with approximately 45% of cases occurring in winter and 25% in summer (Supplementary Notes). In winter, cold weather compels children to spend more time in crowded classrooms with poor ventilation, promoting bacterial and viral proliferation and intensifying adverse effects of immune suppression and compromised lung function48. Conversely, in summer, increased outdoor activities expose children to indirect risks, including heat stress and the synergistic impact of air pollution12. Season-stratified exposure to air pollution also showed that the associated risks are considerably higher in summer and winter compared with other seasons, which may lead to increased cases (Fig. S4). Risk disparities in childhood respiratory outcomes arise from complex interactions among temperature regulation, air pollutants, and behavior-driven seasonal patterns, underscoring the need for regional and seasonal-specific interventions that address these risk trends in school environments.
Moreover, the combined health impacts of particulate matter and temperature extremes on children are expected to intensify25,26. While previous studies have examined the risks of PM2.5 and extreme temperatures50,51,52, research on the combined effects of PM1 and main chemical composition on schoolchildren’s respiratory health remains limited. We found that the joint exposure to six particulate matter pollutants and non-optimal temperature conditions substantially elevates the risk of school absences due to pneumonia and/or tracheitis, with urban–rural disparity. Low temperatures exacerbate the adverse effects of particulate matter pollution in both rural and urban schools. Additionally, high temperatures-high pollution still posed higher risks among rural children. Rural children may be more vulnerable to biomass burning and inadequate indoor cooling and ventilation, exacerbating the impacts of air pollution during extreme heat. A retrospective cohort study of preschool children across seven cities in China also revealed a positive interaction between particulate matter and high temperature on childhood asthma risk16. Consequently, early warnings for non-optimal temperatures and high-pollution days should be implemented to identify areas with frequent compound exposure hotspots, thereby protecting childhood respiratory health.
Growing evidence highlights early life as a critical window during which environmental exposures shape long-term respiratory health53. Studies have shown that prenatal and early postnatal exposure to air pollution, in conjunction with temperature extremes, increases childhood respiratory distress15,16,54. Intrauterine exposure during the second trimester and exposure during the first year of life have been identified as key susceptibility windows15. In vivo studies further confirm that combined heat and pollution exposure exacerbates airway inflammation via oxidative stress and TRPV1-mediated pathways55. Our study extends this evidence by demonstrating that school exposure to PM1, chemical composition and non-optimal temperatures continues to pose significant risks in later childhood, as reflected in increased school absences due to pneumonia and/or tracheitis. Comprehensive evidence highlights the importance of targeting both early-life and school-age periods in strategies to mitigate the respiratory burden associated with combined environmental exposures.
While we emphasize the respiratory health risks of air pollution and extreme temperatures for children amid intensifying global climate change, this study doesn’t specifically focus on historical extreme weather events in the study area due to limited cases. Therefore, the study can’t explain the impact of climate change but should carefully assess extreme temperature indicators and related comprehensive exposure risks. Previous studies have varied definitions of extreme temperatures, and comfortable temperature ranges differ across regions and health outcomes6,56. Given the challenge of integrating historical data from past research with regional variations in individual lung function sensitivity, we adopt a comprehensive approach by assessing low and high temperatures with multi-layer, daily maximum and minimum temperatures, as well as intra-day and inter-day temperature fluctuations to represent extreme temperature exposure.
Several limitations existing in this study should be noted. First, the observational design precludes causal inference. Local spatial analysis without correction for multiple testing may lead to inflated false positives57, and should be interpreted alongside direct spatial distribution in our study. Second, confounding factors like indoor air pollution, socioeconomic status, and healthcare access were not fully accounted for, which may influence observed associations, especially between urban and rural schools, and need more detailed social survey about these aspects in the following research to reduce potential bias. Due to data limitations, we could only use the health records of children in Jiangsu province, China to take this exposure-response assessment. In the future, multi-country and multi-city center child health attendance studies are urgently needed. Moreover, reliance on ambient monitoring may not fully reflect individual-level exposures. We aggregated individual pneumonia and/or tracheitis absences into daily school counts and focused on school-level exposure, which may not adequately reflect children’s true exposure levels across multiple settings. The large-scale spatiotemporal environmental exposure data obtained by simulation may have systematic biases due to lack of high-resolution monitoring stations in the current field. It’s worth noting that the feature of this study is focusing on schoolchildren’s illness-related absence burden due to combined pneumonia and/or tracheitis conditions to reflect the comprehensive impacts of environmental exposure, but the pathological mechanisms, disease progression, and severity of pneumonia and tracheitis are different, and aggregated statistical analyses may mask their specific risk profiles. Therefore, the results need to be interpreted more cautiously compared with previous epidemiological studies based on hospital diagnosis.
Conclusions
This school-centered study highlights the respiratory health risks schoolchildren face from both independent and joint exposures to six major particulate matter pollutants and relatively non-optimal temperatures. We observed consistent increases in respiratory illness-related absenteeism associated with particulate matter exposure, as well as elevated risks linked to both low and high temperatures, while the impact of temperature variability appeared minimal. By analyzing 14-day cumulative exposure trends, the study reveals heterogeneity in risk across urban and rural areas, sex, seasons, and healthcare access. Notably, urban children were most susceptible to low temperatures, whereas rural children experienced heightened risks from air pollution under high-temperature conditions. These findings underscore schoolchildren’s heightened and heterogeneous vulnerability to complex environmental exposures, emphasizing the urgent need for targeted, school-based public health interventions. Addressing regional disparities in air quality and temperature-related risks could benefit from interventions such as air filtration systems, expanded green space, and early warning systems for extreme temperatures. These scalable, context-sensitive measures may help safeguard childhood respiratory health and reduce environmentally related school absenteeism across both urban and rural settings.
Methods
Study area
This study was conducted in Jiangsu Province, an industrialized coastal region in eastern China (30°45′–35°08′ N, 116°21′–121°56′ E, Fig. 5), comprising 95 county-level divisions and covering a land area of 107,200 km², with a population exceeding 80 million. As one of the country’s most economically developed and densely populated provinces, Jiangsu faces significant environmental challenges driven by industrial emissions, biomass burning, traffic-related pollution, and construction activities.
Childhood pneumonia and/or tracheitis surveillance
Absenteeism records of childhood pneumonia and/or tracheitis infections were systematically collected from the student health monitoring system of the Jiangsu Provincial Center for Disease Control and Prevention (JS CDC). Recognizing that children’s respiratory infections often present with overlapping clinical features58,59, where pneumonia and tracheitis share symptoms such as cough, fever, and respiratory distress, accurate, rapid differentiation is frequently challenging in public health practice. Consequently, the monitoring system aggregates these conditions to simplify surveillance and reduce potential biases from variable diagnostic criteria, thereby fully grasping the overall burden of respiratory diseases in schoolchildren and improving the operational stability of the system. Overall, this integrative approach enables public health authorities to promptly allocate resources, implement targeted preventive interventions, and orchestrate emergency responses.
The data collection protocol requires the class teachers or attendance officers to observe and record students’ daily attendance and health status, documenting absences, absence reasons, early symptoms, and suspected cases. If a child is found to have symptoms of pneumonia or tracheitis, or is absent from school due to this, the school will immediately report it to the designated school health staff. Subsequent verification through inquiries with the child or guardian and confirmed by school or hospital doctors to ensure accurate case identification, with relevant information entered into an online health monitoring system subject to routine quality control by regional CDC staff. Multi-step data cleaning was employed: (1) records pertaining to non-respiratory illnesses were omitted; (2) health records lacking key symptomatic information or misclassified as non-disease-related (e.g., accidental injuries, personal leave) were excluded based on cross-validation between original system classifications and text-recognized symptomatology; (3) consecutive illness-related absences were assumed to result from environmental exposures occurring on or before the first day of absence; and (4) refer to the suspension standards stipulated by the Ministry of Health and the Ministry of Education to exclude the following cases: 10 or more students absent on the same day, or more than 20 cases in the same class within 3 days (or more than 30% of the class population). After the above data screening and quality control, including excluding schools with missing key characteristics such as school size and absence dates, 1777 kindergartens, 2797 primary schools and 1468 secondary schools were covered. We ultimately retained 265,076 records of school-age children under 18 years old between September 1st, 2016, and June 30th, 2021, in 95 counties for analysis.
Ambient PM pollution assessment
High-resolution daily estimates of the six particulate matter pollutants (NO3−, SO42-, Cl−, BC, NH4+, and PM1) between 2016 and 2021 were derived from our previous open-source datasets (China High Air Pollutants, CHAP)60,61. By integrating multisource datasets, including MODIS MAIAC aerosol optical depth, ground-based observations, atmospheric reanalysis, and detailed emission inventories, we developed a space-time extremely randomized trees, incorporating random forest and deep forest algorithms enhanced with multidimensional spatiotemporal information, to assess the six pollutants’ exposure at 1 km resolution. This approach combines aerosol optical depth (AOD) as a key predictor with measured information from ground monitoring stations to capture nonlinear, multiplicative relationships between AOD, meteorological variables, and pollution emissions, while downscaling coarse satellite data using geographically weighted regression and spatial interpolation techniques. Cross-validation was applied to ensure the robustness of the model. Subsequently, chemical transport models and statistical decomposition techniques are integrated to partition the predicted particulate matter mass into its primary components, including SO42-, NO3−, NH4+, Cl−, and BC. This approach provides a quantitative basis for linking environmental exposure to health outcomes and has been widely used in epidemiology and environmental health risk assessment62,63,64. More detailed information about model setup and dataset details are placed in the open access website (https://weijing-rs.github.io/product.html). Cross-validation results indicated strong model performance, with coefficients of determination (CV-R²) of 0.83 for PM1 and 0.74–0.75 for main chemical composition, and the root-mean-square errors (RMSEs) ranging from 2.3 to 9.5 µg/m³. Here, we used the nonparametric k-nearest neighbor (k-NN) algorithm to extract daily exposure levels of six pollutants for each school in the study area on the day of the case occurrence and in the past 14 days based on the collected school geographic information. The k-NN algorithm determines the particle grid point located to each school based on the Euclidean distance geographical proximity, thus accurately estimating local exposure, and the algorithm was implemented in the FNN package in R v3.6.165.
Extreme temperature assessment
We obtained hourly 2-meter temperature data at a 9-km resolution from the ERA5-Land reanalysis dataset, which integrates ground-based observations through data assimilation to provide observation-informed estimates of near-surface temperature66. Recognizing that the optimal temperature range varies by population and region20,56, and that the health risks associated with extreme temperatures differ among health outcomes6,67, we delineated temperature windows based on the 5th to 25th percentiles (in five-percentage point increments) from both the lower (cold) and upper (heat) tails of the temperature distribution to capture the relative risks of low and high temperatures. In addition, emerging evidence suggests that, beyond average temperature, both intra- and inter-day temperature variability may disrupt thermoregulation, trigger inflammatory responses, and impair respiratory defenses56,68. These effects may also exist in children, increasing vulnerability to infections such as pneumonia and/or tracheitis. Thus, we computed intra-day temperature change as the difference between the daily maximum and minimum temperatures on the event day and over the previous 14 days leveraging hourly simulation data, while inter-day fluctuation was estimated as the average temperature difference between consecutive exposure days. Based on these metrics, we derived a suite of temperature indicators for each school over a 14-day period, including daily average temperature (DAT), intra-day change (IDC), inter-day fluctuation (IDF), as well as daily maximum and minimum temperatures and standard deviation of daily average temperatures.
Spatial characteristic analysis
To assess spatial exposure disparities of associated pollutants and temperature variables as well as their potential impact on children’s health, we employed both global and local spatial analyses using R version 3.6.1. First, we collected data on all pollutants and temperature indices and converted these into spatial objects based on geographic coordinates. Next, we constructed spatial normalized weight matrix using a k-nearest neighbors approach (k = 8) to define the adjacency relationships between monitoring locations. Global spatial autocorrelation was quantified by computing Moran’s I for each pollutant. Significant positive or negative Moran’s I values indicate overall spatial clustering of high or low concentrations, whereas values near zero suggest spatial randomness. For localized analysis, we computed the Getis-Ord Gi* statistic to identify hot spots and cold spots. The resulting z-scores indicate areas of statistically significant clustering: high positive z-scores denote hot spots where pollutant levels are significantly elevated, while low negative z-scores indicate cold spots, with significance at levels of p < 0.05 and p < 0.01 according to previous research69. To further illustrate the spatial characteristics of the school environment, we applied these global and local tests to green space coverage, road density, and the number of nearby factories (Fig. S1). This dual-level spatial analysis framework not only quantifies overall spatial autocorrelation but also pinpoints local concentration patterns, thereby providing critical insights for subsequent risk assessment efforts and targeted public health interventions to mitigate adverse health impacts among children. Finally, independent sample t-tests were conducted on all school environment variables to compare urban and rural settings.
Statistical analysis
To examine the association between air pollution, extreme temperatures, and the daily counts of childhood pneumonia and/or tracheitis, we employed a spatiotemporal stratified case-crossover design using the gnm() function in R version 3.6.170. This approach is rooted in the self-matching principle using time-series, location-specific data. By comparing the aggregated cases within the set window, we could assess school-level exposure variations in different time periods, effectively controlling time-varying and location-specific confounders. Here, we applied school-based quasi-Poisson regression models, incorporating both linear and nonlinear exposure-response assumptions at school level while addressing overdispersion in count data. To further mitigate spatiotemporal confounding, we defined strata based on school code, year, season and day of the week (DOW), with each stratum defined by a unique combination of these four factors (e.g., school-year-season-DOW). Within each stratum, all days sharing the same temporal and spatial characteristics were compared, enabling each observation to be evaluated relative to others. This non-random, self-matched design helps control for unmeasured between-school differences, long-term trends, weekly effects, and spatial variation, thereby enhancing the robustness of our estimates.
We applied a cross-basis function to transform particulate matter exposure and temperature variables. Specifically, for the six air pollutants, we assumed a linear dose-dependent characteristic and applied linear assumption in cross-basis function setting according to previous evidence71; for temperature variables (DAT, IDC, and IDF), we assumed that low or high temperatures would cause respiratory health threats, thus we applied a nonlinear cross-basis matrix embedded in natural cubic splines with 4 degrees of freedom to ensure flexible and robust representation of DAT and IDF impacts, and 3 degrees for IDC56. The lag period of all was set to 14 days. We used a natural cubic spline function with three degrees of freedom to control the confounding impacts of O3 and RH; a natural cubic spline with four degrees of freedom was also applied to control average temperature impacts in air pollution model, while coarse particulate matter was treated as an additional control for confounding effects in the non-optimal temperature model. The model equation is as follows:
where E(Y) represents the expected number of cases, α represents the model intercept, stratum refers to the location-specific time window defined by grouping the same day of the week within each season of each year for the school, exposure denotes air pollutants treated with linear assumptions or temperature variables treated with nonlinear assumptions, which are modeled using a cross-basis function with coefficient β0; covariates represent other variables that may affect absenteeism with coefficient βT.
To compare the independent exposure risks of urban and rural children to various types of pollution and temperature changes, we fitted the exposure-response risk cures over the past 14-days based on the urban-rural attributes of school locations. We also assessed seasonal and gender differences using stratified models. For the air pollution model based on the linear assumption, we estimated the relative risk (RR) and its 95% confidence interval (95% CI) of pneumonia and/or tracheitis related absence burden per unit increase or per quartile increase in pollution concentration. For the average daily temperature variable, we replaced the original nonlinear hypothesis variable with the low temperature-comfortable-high temperature segment variable defined by 5–25% stratification and used the comfortable temperature range as the baseline to evaluate the relative risk of children’s absence due to illness caused by the low or high temperature segment, enhancing the quantitative analysis of temperature risk.
In the composite exposure scenario, we first evaluated the relative risk trends of six pollutants in different temperature ranges through the stratified variables of daily average temperature based on the findings from above independent temperature exposure risk assessments (below 25% low temperature, 25–75% comfortable temperature, and over 75% high temperature). Then, we constructed 18 composite exposure models combined with regional stratification, taking comfortable temperature-low pollution exposure as the baseline, and comprehensively evaluated the relative risks and significance levels of comfortable temperature-high pollution, low temperature-comfortable temperature, low temperature-high pollution, high temperature-low pollution and high temperature-high pollution for all schools, urban and rural schools.
Covariates and sensitivity analysis
Daily relative humidity (RH) for the preceding 14 days was calculated using air pressure, dew point temperature, and surface temperature data from the ERA5-Land meteorological reanalysis dataset66,72. Additional covariates in the analysis included year, season, geographic region (urban or rural), day of the week, gender, and 14-day cumulative exposure to PM10 and O3, which was placed in the model or as a stratified setting. In particular, we assessed the composite exposure risk of O3 and various temperature variables to fully consider its potential health threat when discussing air pollution and children’s respiratory health (Figure S2). To assess the robustness of the combined health outcome measure and to profile the severity of childhood pneumonia and/or tracheitis illnesses as reflected by the choice of care, we performed exposure–response analyses separately by recorded mode of care, including home care, outpatient care, and hospitalization (Fig. S3, Table S1).
We have set up 20 types of models for robustness testing on the air pollution and temperature impacts, including changing covariates, data distribution assumptions, and replacing models. We considered the spatial location distribution of each school and constructed a generalized additive model based on spatial smoothing functions to further verify the robustness of the model results (Table S2, 3). We also examined effect modifications by season, gender and region through stratified analyses and related risk trends during the past 14-days’ exposure (Figs. S5–S19). The models consistently demonstrated overall robust risk estimates and no collinearity (Table S4). All analyses were conducted using R version 3.6.1, with statistical significance assessed using two-tailed tests at levels of *p < 0.05, **p < 0.01, ***p < 0.001.
Data availability
All air pollution data, including NO3−, SO42-, Cl−, BC, NH4+, and PM1, are publicly accessible in our public dataset CHAP (https://weijing-rs.github.io/product.html). Due to privacy regulations, child health records are not open source. This study includes the frequency of school-level absences due to pneumonia and/or tracheitis based on individual records (school code, date, gender) as well as aggregated information on age, region, and school type. If you want to access some or all of the data, please contact the corresponding authors directly by email and provide a brief research design. Limited access is allowed after obtaining approval from the Ethics Committee of Jiangsu Provincial Center for Disease Prevention and Control and signing an authorization and confidentiality agreement. We welcome academic inquiries and collaborations.
References
Zar, H. J. & Ferkol, T. W. The global burden of respiratory disease—impact on child health. Pediatric pulmonology 49, 430–434 (2014).
World Health Organization. Pneumonia in children. https://www.who.int/news-room/fact-sheets/detail/pneumonia (2020).
Troeger, C. et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet infectious diseases 18, 1191–1210 (2018).
Walker, C. L. F. et al. Global burden of childhood pneumonia and diarrhoea. The Lancet 381, 1405–1416 (2013).
Sheffield, P. E. & Landrigan, P. J. Global climate change and children’s health: threats and strategies for prevention. Environmental health perspectives 119, 291–298 (2011).
Burkart, K. G. et al. Estimating the cause-specific relative risks of non-optimal temperature on daily mortality: a two-part modelling approach applied to the Global Burden of Disease Study. The Lancet 398, 685–697 (2021).
Achebak, H., Devolder, D., Ingole, V. & Ballester, J. Reversal of the seasonality of temperature-attributable mortality from respiratory diseases in Spain. Nature communications 11, 2457 (2020).
D’Amato, M. et al. The impact of cold on the respiratory tract and its consequences to respiratory health. Clinical and translational allergy 8, 1–8 (2018).
Zhang, W., Ruan, Y., Ling, J. & Wang, L. A study of the correlation between meteorological factors and hospitalization for acute lower respiratory infections in children. BMC Public Health 24, 3135 (2024).
Konstantinoudis, G. et al. Ambient heat exposure and COPD hospitalisations in England: a nationwide case-crossover study during 2007–2018. Thorax 77, 1098–1104 (2022).
Wu, Y. et al. Short-term exposure to extreme temperature and outpatient visits for respiratory diseases among children in the northern city of China: a time-series study. BMC Public Health 24, 341 (2024).
Hansel, N. N., McCormack, M. C. & Kim, V. The effects of air pollution and temperature on COPD. COPD: Journal of Chronic Obstructive Pulmonary Disease 13, 372–379 (2016).
Altman, M. C. et al. Associations between outdoor air pollutants and non-viral asthma exacerbations and airway inflammatory responses in children and adolescents living in urban areas in the USA: a retrospective secondary analysis. The Lancet Planetary Health 7, e33–e44 (2023).
Wang, X. et al. Ambient particulate matter (PM1, PM2.5, PM10) and childhood pneumonia: the smaller particle, the greater short-term impact? Science of The Total Environment 772, 145509 (2021).
Lu, C. et al. Effects of intrauterine and post-natal exposure to air pollution on children’s pneumonia: key roles in different particulate matters exposure during critical time windows. Journal of Hazardous Materials 457, 131837 (2023).
Lu, C. et al. Interaction effect of prenatal and postnatal exposure to ambient air pollution and temperature on childhood asthma. Environment International 167, 107456 (2022).
Gouveia, N. et al. Effects of air pollution on infant and children respiratory mortality in four large Latin-American cities. Environmental Pollution 232, 385–391 (2018).
Leung, S. Y. et al. Short-term association among meteorological variation, outdoor air pollution and acute bronchiolitis in children in a subtropical setting. Thorax 76, 360–369 (2021).
Jadhav, S. P. et al. Introduction to lung diseases. Targeting cellular Signalling pathways in lung diseases 1–25 (2021).
Gasparrini, A. et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. The lancet 386, 369–375 (2015).
Habre, R. et al. The effects of PM2.5 and its components from indoor and outdoor sources on cough and wheeze symptoms in asthmatic children. Journal of exposure science environmental epidemiology 24, 380–387 (2014).
Li, Y. et al. Short-term PM2. 5 exposure induces transient lung injury and repair. Journal of Hazardous Materials 459, 132227 (2023).
Yang, M. et al. Is PM1 similar to PM2.5? A new insight into the association of PM1 and PM2.5 with children’s lung function. Environment international 145, 106092 (2020).
Schraufnagel, D. E. The health effects of ultrafine particles. Experimental molecular medicine 52, 311–317 (2020).
Perera, F. & Nadeau, K. Climate change, fossil-fuel pollution, and children’s health. New England Journal of Medicine 386, 2303–2314 (2022).
Helldén, D. et al. Climate change and child health: a scoping review and an expanded conceptual framework. The Lancet Planetary Health 5, e164–e175 (2021).
World Health Organization. How school systems can improve health and well-being. Topic brief: physical activity (2023).
Cattan, S., Kamhöfer, D. A., Karlsson, M. & Nilsson, T. The long-term effects of student absence: Evidence from Sweden. The Economic Journal 133, 888–903 (2023).
Mahapatra, B., Walia, M., Avis, W. R. & Saggurti, N. Effect of exposure to PM10 on child health: evidence based on a large-scale survey from 184 cities in India. BMJ Global Health 5, e002597 (2020).
Southerland, V. A. et al. Global urban temporal trends in fine particulate matter (PM2.5) and attributable health burdens: estimates from global datasets. The Lancet Planetary Health 6, e139–e146 (2022).
Reyes-Garcia, J., Montano, L. M., Carbajal-Garcia, A. & Wang, Y.-X. In Lung Inflammation in Health and Disease, Volume II 259-321 (Springer, 2021).
Ekpruke, C. D. & Silveyra, P. Sex differences in airway remodeling and inflammation: clinical and biological factors. Frontiers in Allergy 3, 875295 (2022).
Silveyra, P., Al Housseiny, H. & Rebuli, M. E. Sex and gender differences in the susceptibility to environmental exposures. Sex-based differences in lung physiology 251–290 (2021).
Verthelyi, D. Sex hormones as immunomodulators in health and disease. International immunopharmacology 1, 983–993 (2001).
Lang, T. J. Estrogen as an immunomodulator. Clinical immunology 113, 224–230 (2004).
Nair, H. et al. Common childhood infections and gender inequalities: a systematic review (2015).
Hesketh, T., Ding, Q. J. & Tomkins, A. M. Health and health care-seeking behavior of adolescents in urban and rural China. Journal of adolescent health 33, 271–274 (2003).
Liu, T. et al. Urban-rural disparity of the short-term association of PM2.5 with mortality and its attributable burden. The Innovation 2 (2021).
Mendoza, D. L. et al. Impact of low-level fine particulate matter and ozone exposure on absences in K-12 students and economic consequences. Environmental Research Letters 15, 114052 (2020).
Bener, A., Kamal, M. & Shanks, N. J. Impact of asthma and air pollution on school attendance of primary school children: are they at increased risk of school absenteeism? Journal of Asthma 44, 249–252 (2007).
Liu, H. & Salvo, A. Severe air pollution and child absences when schools and parents respond. Journal of Environmental Economics and Management 92, 300–330 (2018).
Watanabe, M., Noma, H., Kurai, J., Kato, K. & Sano, H. Association with ambient air pollutants and school absence due to sickness in schoolchildren: a case-crossover study in a provincial town of Japan. International Journal of Environmental Research and Public Health 18, 6631 (2021).
Morphew, T., Graham, J., Rubio, K., Anderson, N. & Gentile, D. Association Between Exposure to Outdoor Air Pollution and School Absenteeism Among Asthmatic Children. Journal of Allergy and Clinical Immunology 147, AB42 (2021).
Lei, J. et al. Fine and coarse particulate air pollution and hospital admissions for a wide range of respiratory diseases: a nationwide case-crossover study. International journal of epidemiology 52, 715–726 (2023).
Zhang, J., Wei, Y. & Fang, Z. Ozone pollution: a major health hazard worldwide. Frontiers in immunology 10, 2518 (2019).
Lu, C., Yang, W., Lan, M., Li, B. & Wang, F. Effects of intrauterine and postnatal exposure to meteorological factors on childhood pneumonia. Building and Environment 244, 110800 (2023).
Ngo, H. K. et al. Impact of temperature on hospital admission for acute lower respiratory infection (ALRI) among pre-school children in Ho Chi Minh City, Vietnam. International Journal of Biometeorology 65, 1205–1214 (2021).
He, Q. et al. Differentiating the impacts of ambient temperature on pneumonia mortality of various infectious causes: a nationwide, individual-level, case-crossover study. EBioMedicine 98 (2023).
Tong, S., Prior, J., McGregor, G., Shi, X. & Kinney, P. Urban heat: an increasing threat to global health. bmj 375 (2021).
Zhou, L. et al. The interactive effects of extreme temperatures and PM2.5 pollution on mortalities in Jiangsu Province, China. Scientific Reports 13, 9479 (2023).
Huang, Y. et al. Exploring health effects under specific causes of mortality based on 90 definitions of PM2.5 and cold spell combined exposure in Shanghai, China. Environmental Science Technology 57, 2423–2434 (2023).
Mirabelli, M. C., Vaidyanathan, A., Flanders, W. D., Qin, X. & Garbe, P. Outdoor PM2.5, ambient air temperature, and asthma symptoms in the past 14 days among adults with active asthma. Environmental health perspectives 124, 1882–1890 (2016).
Stocks, J., Hislop, A. & Sonnappa, S. Early lung development: lifelong effect on respiratory health and disease. The lancet Respiratory medicine 1, 728–742 (2013).
Lu, C. et al. Interaction of exposure to outdoor air pollution and temperature during pregnancy on childhood asthma: Identifying specific windows of susceptibility. Building and Environment 225, 109676 (2022).
Lu, C. et al. Interaction of high temperature and NO2 exposure on asthma risk: in vivo experimental evidence of inflammation and oxidative stress. Science of The Total Environment 869, 161760 (2023).
Guo, Y. et al. Temperature variability and mortality: a multi-country study. Environmental health perspectives 124, 1554–1559 (2016).
Sun, W., Reich, B. J., Tony Cai, T., Guindani, M. & Schwartzman, A. False discovery control in large-scale spatial multiple testing. Journal of the Royal Statistical Society Series B: Statistical Methodology 77, 59–83 (2015).
McIntosh, K. Community-acquired pneumonia in children. New England Journal of Medicine 346, 429–437 (2002).
Paul, S. P., Wilkinson, R. & Routley, C. Management of respiratory tract infections in children. Nursing: Research and Reviews, 135-148 (2014).
Wei, J. et al. Separating daily 1 km PM2. 5 inorganic chemical composition in China since 2000 via deep learning integrating ground, satellite, and model data. Environmental science technology 57, 18282–18295 (2023).
Wei, J. et al. Satellite-derived 1-km-resolution PM1 concentrations from 2014 to 2018 across China. Environmental science technology 53, 13265–13274 (2019).
Lin, L. et al. The airway microbiome mediates the interaction between environmental exposure and respiratory health in humans. Nature Medicine 29, 1750–1759 (2023).
Tian, Y. et al. Ambient PM2. 5 Chemical Composition and Cardiovascular Disease Hospitalizations in China. Environmental Science Technology 58, 16327–16335 (2024).
Zhang, Y. et al. Long-term PM1 exposure and hypertension hospitalization: A causal inference study on a large community-based cohort in South China. Science Bulletin 69, 1313–1322 (2024).
Altman, N. S. An introduction to kernel and nearest-neighbor nonparametric regression. The American Statistician 46, 175–185 (1992).
Muñoz Sabater, J. ERA5-Land hourly data from 1981 to present. Copernicus climate change service (C3S) climate data store (CDS) 10 (2019).
Chen, R. et al. Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. Bmj 363 (2018).
Xu, R. et al. Socioeconomic inequality in vulnerability to all-cause and cause-specific hospitalisation associated with temperature variability: a time-series study in 1814 Brazilian cities. The Lancet Planetary Health 4, e566–e576 (2020).
Chen, H., Chen, Y., Sun, B., Wen, L. & An, X. Epidemiological study of scarlet fever in Shenyang, China. BMC Infectious Diseases 19, 1–7 (2019).
Wu, Y., Li, S. & Guo, Y. Space-time-stratified case-crossover design in environmental epidemiology study. Health Data Science 2021 (2021).
Mudway, I. S. et al. Impact of London’s low emission zone on air quality and children’s respiratory health: a sequential annual cross-sectional study. The Lancet Public Health 4, e28–e40 (2019).
Lawrence, M. G. The relationship between relative humidity and the dewpoint temperature in moist air: A simple conversion and applications. Bulletin of the American Meteorological Society 86, 225–234 (2005).
Acknowledgements
This study was supported by National Natural Science Foundation of China (Grant No. 72488101 & No. 42377420 & 42477499). We would like to thank Dr. Yidong Zhou from the Department of Statistics, University of California, Davis, and Mr. Fan Liu from School of Environment, Nanjing University for their help in checking the method design and robustness of the results.
Author information
Authors and Affiliations
Contributions
Y. WU, J. Y., and J. W. contributed equally to this work. Y. WU, B. C., and L. H. were responsible for conceptualization and study design. J. Y. and H. S. contributed to data collection and statistical analysis. Y. WU, J. W., C.L. Y. WANG, and P. W. conducted data curation and methodology development. Y. WU conducted the literature review and manuscript drafting. L. H. and H. S. supervised the project and provided critical revisions to the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study utilized de-identified public health data obtained through routine administrative surveillance by the Jiangsu Provincial Center for Disease Control and Prevention. The dataset involved in this research doesn’t contain any personal identifiable or sensitive individual data and has been aggregated to the school level for modeling. No human subjects were directly contacted, and no biological specimens were collected. The use of this dataset and this study has been reviewed and authorized by the Ethics Committee of Jiangsu Provincial Center for Disease Prevention and Control. Based on the study design, the Ethics Committee of Jiangsu Provincial Center for Disease Prevention and Control authorized a waiver of informed consent and complied with the ethical principles of the Declaration of Helsinki.
Peer review
Peer review information
Communications Earth & Environment thanks the anonymous reviewers for their contribution to the peer review of this work. Primary Handling Editors: Sagar Parajuli and Alice Drinkwater. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, Y., Yang, J., Wei, J. et al. Extreme temperatures amplify air pollution risks to childhood respiratory health in school environment in Jiangsu province, China. Commun Earth Environ 6, 429 (2025). https://doi.org/10.1038/s43247-025-02409-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s43247-025-02409-8