Abstract
Background
Complications arising from acute traumatic spinal cord injury (SCI) are routinely managed by various pharmacological interventions. Despite decades of clinical application, the potential impact on neurological recovery has been largely overlooked. This study aims to highlight commonly administered drugs with potential disease-modifying effects.
Methods
This systematic literature review included studies referenced in PubMed, Scopus and Web of Science from inception to March 31st, 2021, which assess disease-modifying properties on neurological and/or functional recovery of drugs routinely administered following spinal cord injury. Drug effects were classified as positive, negative, mixed, no effect, or not (statistically) reported. Risk of bias was assessed separately for animal, randomized clinical trials, and observational human studies.
Results
We analyzed 394 studies conducting 486 experiments that evaluated 144 unique or combinations of drugs. 195 of the 464 experiments conducted on animals (42%) and one study in humans demonstrate positive disease-modifying properties on neurological and/or functional outcomes. Methylprednisolone, melatonin, estradiol, and atorvastatin are the most common drugs associated with positive effects. Two studies on morphine and ethanol report negative effects on recovery.
Conclusion
Despite a large heterogeneity observed in study protocols, research from bed to bench and back to bedside provides an alternative approach to identify new candidate drugs in the context of SCI. Future research in human populations is warranted to determine if introducing drugs like melatonin, estradiol, or atorvastatin would contribute to enhancing neurological outcomes after acute SCI.
Plain language summary
Patients with spinal cord injury (SCI) are exposed to a wide range of medications treating health conditions arising as a consequence of the initial injury. The effect of providing patients with a large number of medications in the early period after injury, that is in the first days to weeks, on recovery from SCI, however, is typically not considered. This extensive and structured review of evidence from pre-clinical (animal) and clinical (human) studies quantifies these effects for the first time. 144 unique drugs or combinations of drugs previously reported to be administered in animal models or to patients with SCI have been studied for their effect on recovery across 486 distinct experiments. A small subset of drugs are associated with positive effects, and provide potential targets for further study to determine if they can be used to treat SCI.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a devastating condition that often leads to severe and permanent neurological and functional impairments. Despite recent advancements, effective treatments promoting neurological and functional recovery are urgently needed1, 2. Over the last decades, interest in exploring the disease-modifying effects of commonly administered drugs in this context has grown3,4,5,6. Nearly every individual sustaining a traumatic SCI receives multiple types and classes of drugs to manage a wide range of secondary complications associated with the neurotrauma7,8,9. These range from drugs to manage blood pressure, to analgesics for concomitant traumatic injuries, to anticholinergics for spasms. A recent study showed that patients receive up to 60 unique drugs within the first 2 months, often in combinatorial fashion7. Despite extensive polypharmacy, little is known to what degree drugs commonly used in the management of acute SCI have downstream, unintended, beneficial or detrimental, effects on neurological and functional outcomes.
The acute phase of SCI represents a crucial window of opportunity for therapeutic intervention. Consequently, understanding the potential therapeutic benefits or possible harm of routinely administered drugs on neurological and functional recovery is paramount in the development of effective treatment strategies for SCI. The detrimental effects of SCI extend beyond the initial damage, as a cascade of secondary injury processes like inflammation, oxidative stress, excitotoxicity, and apoptosis is triggered further compromising neural tissue and impeding recovery. Identifying drugs that can modify these secondary injury mechanisms while promoting neural repair and regeneration presents a promising avenue of research. Commonly administered drugs, already approved for various medical conditions, offer the advantage of established safety profiles and known pharmacokinetics. These drugs have been extensively studied in their primary therapeutic indications, but emerging evidence suggests that some possess additional neuroprotective, neuroregenerative, or anti-inflammatory properties potentially promoting recovery after SCI6, 10. Disease-modifying effects of these drugs can be multifaceted. Some drugs may act directly on the injured spinal cord by reducing inflammation11, inhibiting cell death pathways12, or promoting axonal regeneration13. Others may exert their effects indirectly by modulating the surrounding environment, such as promoting angiogenesis or altering the immune response14, 15 to create a more conducive environment for neural repair. Simultaneously, potential harmful effects of commonly administered drugs on neurological recovery are rarely considered but their identification could allow for crucial changes in treatment strategies.
To bridge this knowledge gap, we conducted a comprehensive systematic review of preclinical and clinical studies examining the effects of commonly administered drugs on functional and neurological recovery following SCI. We found extensive heterogeneity across study parameters, which could potentially complicate translation of promising findings from preclinical studies but also highlights opportunities for further investigation of promising candidates for drug repurposing.
Methods
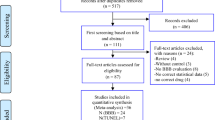
The study protocol was registered with and approved by the international prospective register of systematic reviews (PROSPERO) (registration number: CRD42021231851). This review conforms to the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines16.
Selection of drugs
The list of all drugs administered in the first 60 days after injury to treat secondary complications in the Sygen17 and SCIRehab18 cohorts were extracted from our recent publication7. We will refer to those as drugs of interest. The subset of drugs for which studies could be retrieved and were included in this review is provided in Supplementary Data S1.
Search methods for identification of studies
Using Publish or Perish (version 7.23.2852.7498)19, PubMed, SCOPUS, and Web of Science were searched using the time range from their individual inception dates (1977, 1960, and 1945 respectively) to March 31st, 2021. Search terms were spinal cord injury, recovery, and name of a drug of interest (Section “Selection of drugs”), joined with AND. A manual search was also performed to include matching references of relevant trials.
Selection of studies
Articles were independently screened in two stages: initial screening of titles and abstracts (MW, CRJ), and full-text assessments (LB, LPL, MW, CRJ) using criteria described in the following section. In case multiple articles reported on a single cohort, the article providing the most data or detail was selected for further synthesis. Disagreements were discussed and resolved at multiple consensus meetings.
Inclusion and exclusion criteria
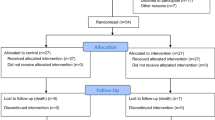
All full-text, peer-reviewed studies investigating the disease-modifying effect of a drug of interest on relevant neurological or functional outcomes after acute SCI were included. Where original articles were not published in English, screening and data extraction were performed by native speakers. We excluded duplicates, non peer-reviewed articles, reviews, meta-analyses, abstracts, editorials, commentaries, perspectives, patents, letters with insufficient data reporting, studies exclusively on children/neonates, or out-of-scope studies (see Fig. 1 for full definition). In particular, out-of-scope studies included publications investigating drugs outside of the drugs of interest as defined in Selection of Drugs. We only included studies comparing the treatment group to a placebo control group, and excluded experiments using active compounds as the only control as it is impossible to compare drug effects between studies using different comparators (i.e., different active controls in studies A and B instead of placebo). Authors of articles that were indexed but not accessible either through institutional library access (ETH Zurich) or open source publishing, were contacted to obtain a copy of the full article. In case no copy was provided, the article was excluded (see not accessible in Fig. 1). Subsequent data extraction was performed by six investigators (LB, LPL, BT, JL, TG, and CRJ).
Assessments and outcomes
The review focused on studies reporting drug effects on recovery as assessed by locomotor function, skilled fore- or upper limb function, sensory function as well as electrophysiology. Details about the assessments included in the analysis are reported in Supplementary Data S2 and Supplementary Table S1. Assessments used to track recovery outcomes in animals with SCI were grouped into categories based on the deficits measured. Tasks that assess spontaneous and voluntary motor function were differentiated between quadrupedal locomotion or skilled reaching or forelimb usage. Sensory assessments were grouped, including sensory reflex arcs, regardless of the type of sensory input eliciting the reflex. Assessments of electrical activity of muscle fibers or circuits were grouped under electrophysiology assessments to mirror comparable assessments in humans and reflect neural excitability. Too few papers assessed reflexes or utilized electrophysiology to warrant distinguishing between proprioceptive or pain/withdrawal reflexes, or between assessments of single units vs. monosynaptic or polysynaptic potentials or motor vs. sensory circuits. Assessments spanning multiple categories (e.g., Gale scale) or used in only a few studies were grouped together. In cases of ambiguity, the methods and results of the paper were closely reviewed to ascertain the feature of the deficit being assessed (e.g., toe spread as a measure of reflexes vs. weight bearing during locomotion).
Data extraction and synthesis
The following information was extracted from all studies: (1) study characteristics (first author’s last name, publication year, language), (2) study population (species, group sizes [total/control/treatment], sex, age, weight), (3) injury characteristics (level, severity, mechanism, duration), (4) drug administration (drug name, dose, route of administration, timing of start of treatment relative to injury, duration of treatment), and (5) neurological and functional assessment outcomes (name, time point(s), investigators blinded to treatment, drug effect). A full list of extracted variables is provided in Supplementary Data S3. Studies analyzing multiple drugs of interest (e.g., drug A, drug B, and control, with drugs A and B of interest) were separated into multiple experiments (e.g., experiment 1: drug A vs. control, experiment 2: drug B vs. control) and extracted individually. Clinical studies on human populations were assessed for risk of bias (RoB) according to their design, either using the RoB 2 tool for randomized clinical trials (RCTs)20 or the ROBINS-I tool for non-randomized interventions21. Animal experiments were assessed for risk of bias based on the SYstematic Review Centre for Laboratory animal Experimentation (SYRCLE) RoB tool22. Additionally, incomplete reporting of basic information relating to the study protocol was graded with a score from 0 (no selective reporting) to 20 (highest selective reporting) according to criteria listed in Supplementary Table S2. Visualizations for RoB assessments of RCTs and intervention studies were created using robvis23.
Statistical analysis
Drug effects were classified for each experiment in one of six categories (Table 1). Descriptive statistics (mean, standard deviations, median, min, max, percentage, and proportions) were used to provide summary information on the study characteristics, the studied drugs and their effect on recovery after SCI.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Initially 9338 studies were screened and 1140 qualified for full-text reading. 394 unique studies, reporting 486 experiments, met our inclusion criteria (Fig. 1). Sixty-four studies (16%) reported more than one experiment. Studies were published between June 1975 and March 2021, with the majority after 2010 (238 studies, 60%, Supplementary Fig. S1A). While most studies were published in English (n = 381, 96·7%), some were also written in Mandarin (n = 7, 1·8%), Turkish (n = 2, 0·5%), Portuguese (n = 2, 0·5%), Persian (n = 1, 0·3%), and Korean (n = 1, 0·3%). Most studies addressed the effect of medications in animal models (n = 377, 96%). Seventeen (4%) studies, reporting 22 experiments (5%), reported results in humans. 774 drugs are known to be administered in the acute phase of SCI7. 116 (15%) of those drugs were included in experiments identified in our review. 110 drugs were examined individually and 33 in combination (Supplementary Data S1). Six drugs were only tested as part of combinatorial treatments - aminocaproic acid24, rosuvastatin25, magnesium chloride26, 27, ketamine28, isoflurane28 and nitroprusside29.
Pre-clinical studies
Population studied Rat models were most extensively investigated (n = 382/464 experiments, 82%). Larger mammals (i.e., cats, dogs) were mainly used before 2001 (n = 19/22 experiments conducted on cats and dogs, 86%, Supplementary Fig. S1B). By contrast, all experiments performed on mice (n = 38) were published after 2000. Sample size, age, and sex were partly or fully missing in 77 (17%), 341 (73%), and 61 (13%) experiments, respectively. Partly missing entries included sample size bounded or expressed as ranges, age described as adult or young, and samples comprising both male and female in unknown proportions. Likewise, exclusion or death of animals was only reported for 51 (11%) experiments. Among experiments reporting sample size, cohorts included a mean of 63 animals (SD: 52, median: 48, Q1-Q3: 32-80). Studies using larger mammals exhibited smaller cohorts (Supplementary Table S3). When reported, age was commonly expressed in weeks (n = 87, 19%). Rats had a mean age of 10 weeks (10.69 weeks when mean age is reported [n = 31/77], 8.92 weeks for lower bound and 10.76 weeks for upper bound when ranges are reported [n = 57/77]). Mice were also 10 weeks of age (mean of 10.00 [n = 2/10], 8.25 [n = 8/10] and 10.13 [n = 8/10] weeks when mean, minimum and maximum are reported, respectively). A majority of studies included exclusively male or female animals (n = 387, 83%), with more experiments being performed on exclusively male populations (n = 206, 44%). Details on the use of male, female and mixed populations over time are reported in Supplementary Fig. S1C.
Injury characteristics SCI models have been previously categorized into contusion, compression, distraction, dislocation, transection and chemical models30. 278 (60%), 132 (28%), 27 (6%), 16 (3%), 7 (2%), 5 (1%) experiments reported a contusion, compression, transection, ischemia, multiple or other injury mechanisms (photochemical lesion31,32,33, irradiation34, electrolytic lesion35), respectively. Although protocols used to induce injuries were often described in detail, information about the corresponding severity of the injury was missing for most experiments (n = 257, 55%). Level of injury was typically reported either precisely (n = 262, 56%) or in ranges (n = 172, 37%). Most experiments studied injuries at the thoracic level, predominantly at or below T5 (n = 222, 85% and n = 151, 88%, of experiments reporting unique and range levels respectively, Fig. 2).
Drugs investigated and assessments of their effects 109 individual drugs and 32 combinations were tested in SCI animal models. Methylprednisolone and methylprednisolone sodium succinate were most prevalent among experiments reported with 71 (15%) and 23 (5%) experiments, respectively (Fig. 3). A total of 60 (43%) unique drugs or combinations were tested in more than one experiment.
Drug effects were evaluated by a wide range of neurological and locomotor assessments. The most common choice was the Basso Beattie Bresnahan36 (BBB) scale, developed and employed for rats. Its original or modified versions (e.g., Basso mouse scale37, canine BBB locomotor scale38) were used in 275 (59%) of the experiments (Fig. 4). Overall, most tests performed (n = 620/848, 73%) evaluated locomotor function. One experiment or study could include more than one assessment, and 174 (46%) unique studies tested more than one category among locomotion, skilled forelimb function, sensory function, electrophysiology, and other functional assessments. While assessment protocols were mostly well described, timing, number of repeats, and follow-up period varied widely between experiments.
Individual assessments are grouped into locomotion, skilled forelimb function, sensory function, electrophysiology (EP) and other functional assessments. BBB Basso, Beattie, and Bresnahan locomotor scale, BMS Basso mouse scale, SEPs somatosensory evoked potentials, MEPs motor evoked potentials, SCEPs spinal cord evoked potentials, EP electrophysiology.
Figure 3 illustrates the drug effect reported for the most prevalent drugs in our review. One can notice that diverging findings were reported when testing the same drug in different experiments. Using methylprednisolone as an example, 31 experiments reported positive effects, while 28 experiments found no effect for methylprednisolone. Similarly, metformin, atorvastatin, lithium, valproic acid, melatonin, and estradiol were investigated in more than five independent experiments and the majority (>50%) of those experiments reported a positive effect of the treatment (80%, 78%, 63%, 60%, 57%, 56%, respectively). Interestingly, we identified two drugs with negative effects reported (morphine39, ethanol28). However, most of the experiments published and reviewed here found their respective drugs of interest to have a positive (n = 195, 42%) or no effect (n = 115, 25%) on neurological or functional recovery following SCI. Details of mixed effects reported are presented in Supplementary Fig. S2. A summary of compounds identified for further investigations is provided in Table 2.
Clinical studies
We extracted information from 17 studies reporting 22 experiments conducted on human cohorts with SCIs (Figs. 5, 6). Cohort sizes varied greatly (n = 1040 to n > 200041). Sex distributions were consistently skewed towards male population (from 53.4% to 100% male), in line with the sex distribution observed in the general SCI population42,43,44,45. While one study (two experiments) explicitly included pediatric participants46, most experiments considered only adult participants with mean age between 32.54 and 57.647 years, matching the age distribution reported in the literature44, 45, 48, 49.
Icons are used to indicate the route of administration (intravenous, oral, intramuscular) of the drug of interest, and central aspects of study design, where prospective and retrospective refer to how data collection and analysis were planned and completed, while cross-over refers to a study design in which measurements taken pre- and post-exposure to a drug of interest were compared, which deviates from a split of individuals into control and treatment otherwise used. *: 71 participants were recruited for this study, of which 19 did not meet the inclusion criteria; **: 410 patients were excluded from the analysis in this study, making up the difference between sizes reported for the no treatment and intervention groups. Vit D: Vitamin D. The figure includes the following icons obtained from thenounproject.com: “Direction” icon by Uswa KDT CC BY 3.0, “Pill” icon by Three Six Five CC BY 3.0, “Shuffle” icon by Gregor Cresnar CC BY 3.0, “Syringe” icon by arman maulana CC BY 3.0, “Vaccination” icon by WiStudio CC BY 3.0, and “Empty set” icon by Gregor Cresnar CC BY 3.0.
D only distributional information reported, NR information not reported, A participants recruited in acute phase after injury, C participants recruited in chronic phase after injury, h: hours, d days, m months, w weeks, y: year, yrs: years, A(H) acute phase hospital stay, A(R) acute phase rehabilitation stay, D(R) discharge from rehabilitation, *: Age (mean and standard deviation) reported for low and high dose groups separately; **: 1 y and 2 y reported if possible but not mandatory.
As expected and in contrast to animal studies, most human experiments were performed on heterogeneous groups with regards to their injury characteristics (neurological level of injury, severity, mechanism of injury). The majority of the studies (n = 15, 18 experiments) investigated patients with acute SCI. Only three studies (five experiments) specifically enrolled participants with subacute or chronic incomplete injuries40, 50, 51 comparing test performances pre- and post-exposure to the drugs of interest.
Drugs tested included naloxone46, 52, 53 (n = 3, 14%), cyproheptadine40, 50 (n = 2, 9%), escitalopram40, 50 (n = 2, 9%), baclofen4, minocycline54, levodopa51, testosterone55 and a combination of progesterone and vitamin D56 (n = 1, each, 5%). Methylprednisolone was the most studied drug (n = 10, 45%) with publications between 199046 and 201857.
All studies evaluated drug effects through neurological assessments. Additionally, functional outcomes such as mobility40, 50, 58 or spasticity40, 50 were tested in eight experiments, and one study (two experiments)40 reported electrophysiological outcomes. Lastly, recovery was assessed based on changes to injury severity in four experiments4, 47, 57, 59.
Results reported for the effects of methylprednisolone diverged from the animal studies with only one experiment recording positive results46, which was part of the oldest study of methylprednisolone in humans. Most of the experiments on methylprednisolone reported no effect (n = 6, 60%) and three observed mixed effects depending on subgroup60, assessment57 or timing of treatment52. A similar trend was observed when considering all drugs tested in human populations: a total of 12 experiments reported no effect (55%) and 9 described mixed results (41%), mainly due to differences between assessments (n = 7, 32%). Notably, most of the data from human populations were collected prospectively (n = 18/22, 82%), i.e., individuals were followed and data were collected over time, while they were most often analyzed retrospectively (n = 12/22, 55%), i.e., data analysis was planned and completed after the final outcome was known. This hints towards few clinical trials testing pharmacological treatments for SCI.
Risk of bias (RoB)
RoB was assessed for animal, RCTs, and observational human studies separately. Overall, the majority of animal studies presented with unclear RoB, due to limited reporting on the items targeted by the SYRCLE tool. In particular, items corresponding to selection (sequence generation and allocation concealment), performance (random housing and blinding), and attrition (incomplete outcome data) biases were rated as unclear for 59.2%, 92.2%, 99.6%, 91.8%, and 87.5% of the experiments included, respectively. An important other source of bias identified was the frequent use of additional drugs, including anesthetics, painkillers and antibiotics. The grading of incomplete reporting of basic information relating to the study protocol scored from zero to 12, with 36 experiments (7.8%) having a score greater or equal to six (Supplementary Data S4). Variables most affected by incomplete reporting were age and blinding of recovery assessments (Fig. 7a, b). Among observational human studies, only one showed critical RoB (Fig. 7c), while most RCTs showed high RoB in the selection of the reported results (Fig. 7d).
a Co-occurrence of potential bias (grading as low or high risk) within animal experiments. Risk of bias was most prevalent in reported age, followed by a combination of age and blinding status. Conversely, information on species, route of drug administration, and dose showed lower risk of bias. b Proportion of each risk of bias (low, unclear or high) by domain of bias studied. Age represents the domain with the most prevalent high risk of bias. c Risk of bias for human intervention studies (observational). Only one study showed a critical risk of bias (domain 5: bias due to missing data), whilst most studies (n = 6, 67%) did not provide sufficient information to assess the risk of bias due to deviations from intended interventions (domain 4). Additionally, the majority of the studies (n = 8, 89%) had a low risk of bias due to selection of participants (domain 2). D1 bias due to confounding, D2 bias due to selection of participants, D3 bias in classification of interventions, D4 bias due do deviations from intended interventions, D5 bias due to missing data, D6 bias in measurement of outcomes, D7 bias in selection of the reported result. d Risk of bias for randomized controlled trials (RCTs). High risk of bias was detected in 7 studies (88%) for bias in selection of the reported results. D1 bias arising from the randomization process, D2 bias due to deviations from intended interventions, D3 bias due to missing outcome data, D4 bias in measurement of outcome, D5 bias in selection of reported result.
Discussion
The current study aimed to systematically review existing literature assessing effects of drugs commonly administered in the acute phase of SCI. Encouragingly, several drugs have been investigated across multiple animal models and have consistently demonstrated positive effects10, 61,62,63,64. This convergence of evidence prompted the formulation of drug repositioning, also known as drug repurposing, as a novel translational approach in the field of acute SCI care. Repositioning has emerged as a successful strategy in other fields (e.g., amantadine in Parkinson’s disease65 and l intuzumab in Alzheimer’s disease66) to improve neurological outcomes in the absence of novel therapies. Drug repositioning aims at identifying new uses for approved or investigational drugs that are outside the scope of the original drug indication67. A clear advantage of this approach is the use of de-risked compounds with established safety and biological activity profiles, thereby reducing overall development costs and shortening timelines68, 69. While drug repositioning utilizes existing evidence to accelerate the development of new treatments, it is still affected by challenges of translational research.
We identified 377 studies considering the effects of drugs previously identified as administered to human patients with acute SCI. Evidence exists for 112 (77.8%) unique compounds or combinations to exert beneficial and/or detrimental effects. For example, metformin is routinely used in humans to manage high blood sugar levels caused by type 2 diabetes70. Preclinical studies have identified enhanced regeneration in the spinal cord related to metformin-induced autophagy via the mTOR signaling pathway10, 71, 72. These observations suggest that administering metformin early after injury could potentially improve long-term neurological outcomes.
Detrimental effects were also observed for some drugs, including opioids, which attenuated the recovery of locomotor function and exacerbated pathophysiological processes in rodent models of SCI73,74,75,76. A detrimental opioid effect is in line with beneficial effects of naloxone, an opioid antagonist77, 78, and highly concerning in light of the ubiquitous administration of opioids for pain management in the early stages of SCI. Completely removing or restricting opioids presents serious ethical concerns (i.e., weighing the management of acute pain with long-term neurological effects). However, minimizing the administration of opioids could potentially facilitate neurological recovery68, 69.
To allow for a comprehensive characterization of potential effects of commonly administered drugs on neurological recovery, we deliberately decided to include preclinical studies involving animal models and clinical studies in humans. Nonetheless, the high degree of heterogeneity across studies, even in a single species, was surprising. A large variability in population characteristics, exact administration parameters, and timing of assessment is observed. In combination with a wide range of spinal levels subjected to injury and different species being studied, comparisons between experiments are challenging or impossible. One exception is the study by Popovich et al.79 aiming to replicate findings, which noted a strong connection between initial injury characteristics and detectable drug effects. This highlights the need for varying as few parameters as possible to allow for meaningful comparisons. In human studies we suspect that the majority reporting mixed or no effects also reflects the heterogeneity in injury patterns included. This likely results in effects which vary widely between individuals and cannot be detected in a group-level analysis. This extensive heterogeneity means that, currently, meta-analyses are not feasible, even for the most commonly studied drugs (Fig. 8). This constitutes a notable limitation as the large fraction of positive effects reported might hint towards a publication bias (Section “Risk of bias (RoB)”). Methylprednisolone constitutes the most interesting example of this pattern, as it has been extensively studied in both pre-clinical and clinical environments with mostly positive results or no effect reported (Figs. 3, 5). While methylprednisolone is still used as an active control in some animal studies, it is no longer an accepted treatment for acute SCI in humans.
Numbers reported in the bars refer to the size of the respective subset of studies with the relevant characteristics. The figure includes the following icons obtained from thenounproject.com: “Average” icon by James Bickerton CC BY 3.0, “Less or equal” icon by Julia Holmberg CC BY 3.0, and “Pin” icon by Nice Design CC BY 3.0.
The lack of an effective pharmacological treatment for SCI highlights the discrepancy between largely positive pre-clinical results and unsuccessful translation to human subjects. A number of hypotheses that could explain this divergence can be derived from this review. One noticeable difference concerns basic study parameters such as the age of the cohort studied or level of injury. While the age distribution in humans affected by SCI is moving towards a bimodal shape45, studies in animal models are typically performed on more homogeneous groups of younger individuals80,81,82,83,84. While the use of young animals might be a result of practical limitations or cost reduction, the mean age at time of injury (10.0 weeks) can be approximately projected to an 18 year old human85, which fails to capture the human population of SCI and potentially affects translatability. Further, SCI in humans occurs predominantly in the cervical segment of the spinal cord45, while animals are mostly injured in the thoracic region (Fig. 2), likely due to ethical requirements. Similarly, injury severity has been named as a critical parameter to control for in animal studies to ensure translatability of findings to the human population86. Unfortunately, we found that it was also one of the factors least frequently reported (45% of studies). Noticeable differences also exist in the administration of drugs. Animal studies typically follow a weight-based dosing regime while humans receive a standardized dose. Similarly, many animal studies initiate treatment immediately after injury64, 87, 88, which appears infeasible in the human population. Additionally, most pre-clinical studies would restrict their investigation to a single drug, while human populations are subject to a large polypharmacy, with up to 59 drugs prescribed in the acute phase7. Translatability of findings from preclinical studies might be hindered as most of the preclinical studies fail to account for interactions between the drug under investigation and other compounds (e.g., treatments for pain management or other complications). These issues in the transfer from animal to human studies might contribute to the majority of human studies reporting mixed effects. While beneficial effects might still exist in humans, they could go undetected due to the scarcity of RCTs (Section “Clinical Studies”). While RCTs require substantial resources and can be challenging to conduct in a rare and heterogeneous condition like SCI, advancements in the treatment of SCI will only be possible if efforts extend from preclinical studies to systematic prospective data collection and analysis in humans. Finally, only a small subset of studies in humans considers the effect of drugs in the chronic phase. While animal studies often include chronic injury models (for examples see89,90,91) no chronic animal studies were encountered in the scope of this systematic review. One explanation could be that the hypothesized effects of drugs of interest selected target mechanisms of repair which are active early after injury more than at the chronic stage. It would however be interesting to see more human and animal chronic SCI studies investigating the effects of these drugs on debilitating secondary long-term complications86.
A noteworthy limitation of the current review was that literature search was limited to articles listed in PubMed/Medline, Scopus, and Web of Science, or identified by hand searches. Considering the pace at which research in this area advances, it is likely that the findings of the publications described in this paper will be quickly complemented by further research. The literature search also excluded gray literature (e.g., preprints, reports, conference proceedings), the importance of which to this topic is unknown, and thus might have introduced another source of search bias. Publication bias is likely to result in studies with positive results being preferentially submitted and accepted for publication.
The present review provides an extensive summary of existing evidence on effects of drugs administered to individuals affected by SCI. In particular, results highlight melatonin, estradiol, and valproic acid as commonly investigated drugs with largely positive effects, indicating the inherent potential to advance treatment through drug repurposing. Simultaneously, we observed and extensively characterized sources of heterogeneity among the valuable resources provided by existing studies. In light of the current lack of an effective pharmacological treatment for SCI and failed attempts to develop new treatments, the field would benefit from further standardization in studying and reporting drug effects investigated in animal models.
Data availability
The data used in this study can be accessed at our GitLab repository (https://gitlab.ethz.ch/BMDSlab/publications/SCI-drug-review-publication). Supplementary Data S1 contains information on the number of studies reporting on individual drugs of interest or combinations thereof, which is summarized for the most frequently studied drugs in Fig. 3. Supplementary Data S2 contains information on the assessments used as part of animal studies and the grouping applied, which is presented in Fig. 4. Supplementary Data S4 contains information on the risk of bias assessment applied to animal studies, which is summarized in Fig. 7a, b.
Code availability
The source code for the analysis performed, including visualizations, can be accessed at our GitLab repository (https://gitlab.ethz.ch/BMDSlab/publications/SCI-drug-review-publication) and Zenodo92. R Statistical Software version 4.3.1 and Python version 3.10.10 were used for all analysis.
References
Tian, T., Zhang, S. & Yang, M. Recent progress and challenges in the treatment of spinal cord injury. Protein Cell. https://doi.org/10.1093/procel/pwad003 (2023).
Donovan, J. & Kirshblum, S. Clinical trials in traumatic spinal cord injury. Neurotherapeutics 15, 654–668 (2018).
Warner, F. M. et al. The effect of non-gabapentinoid anticonvulsants on sensorimotor recovery after human spinal cord injury. CNS Drugs 33, 503–511 (2019).
Cragg, J. J. et al. A longitudinal study of the neurologic safety of acute baclofen use after spinal cord injury. Neurotherapeutics 16, 858–867 (2019).
Cragg, J. J. et al. Effects of pain and pain management on motor recovery of spinal cord-injured patients: a longitudinal study. Neurorehabil. Neural Repair 30, 753–761 (2016).
Warner, F. M. et al. Early administration of gabapentinoids improves motor recovery after human spinal cord injury. Cell Rep. 18, 1614–1618 (2017).
Jutzeler, C. R. et al. Pharmacological management of acute spinal cord injury: a longitudinal multi-cohort observational study. Sci. Rep. 13, 5434 (2023).
Cadel, L. et al. Spinal cord injury and polypharmacy: a scoping review. Disabil. Rehabil. 42, 3858–3870 (2020).
Paker, N., Soluk Özdemir, Y., Buğdaycı, D., Çelik, B. & Bölükbaş Y. Prevalence and predictors of polypharmacy among community-based individuals with traumatic spinal cord injury. J. Spinal Cord Med. 46, 958–963 (2023).
Zhang, D. et al. Metformin improves functional recovery after spinal cord injury via autophagy flux stimulation. Mol. Neurobiol. 54, 3327–3341 (2017).
Lambrechts, M. J. & Cook, J. L. Nonsteroidal anti-inflammatory drugs and their neuroprotective role after an acute spinal cord injury: a systematic review of animal models. Glob. Spine J. 11, 365–377 (2021).
Wang, X. et al. Ibuprofen enhances recovery from spinal cord injury by limiting tissue loss and stimulating axonal growth. J. Neurotrauma 26, 81–95 (2009).
Wang, H. et al. Metformin promotes axon regeneration after spinal cord injury through inhibiting oxidative stress and stabilizing microtubule. Oxid. Med. Cell Longev. 2020, 9741369 (2020).
Bracken, M. B. et al. Methylprednisolone and neurological function 1 year after spinal cord injury. Results of the National Acute Spinal Cord Injury Study. J. Neurosurg. 63, 704–713 (1985).
Canseco, J. A. et al. Updated review: the steroid controversy for management of spinal cord injury. World Neurosurg. 150, 1–8 (2021).
Shamseer, L. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 349, g7647 (2015).
Geisler, F. H., Coleman, W. P., Grieco, G. & Poonian, D. Sygen Study Group. The Sygen multicenter acute spinal cord injury study. Spine 26, S87–S98 (2001).
Whiteneck, G., Gassaway, J., Dijkers, M. & Jha, A. New approach to study the contents and outcomes of spinal cord injury rehabilitation: the SCIRehab Project. J. Spinal Cord. Med. 32, 251–259 (2009).
Harzing, A. -W. Publish or Perish. Available from https://harzing.com/resources/publish-or-perish (2007).
Sterne, J. A. C. et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366, l4898 (2019).
Sterne, J. A. et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355, i4919 (2016).
Hooijmans, C. R. et al. SYRCLE’s risk of bias tool for animal studies. BMC Med. Res. Methodol. 14, 43 (2014).
McGuinness, L. A. & Higgins, J. P. T. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 12, 55–61 (2021).
Naftchi, N. E. Treatment of mammalian spinal cord injury with antioxidants. Int. J. Dev. Neurosci. 9, 113–126 (1991).
Kahveci, R. et al. Neuroprotective effects of rosuvastatin against traumatic spinal cord injury in rats. Eur. J. Pharm. 741, 45–54 (2014).
Kwon, B. K. et al. Magnesium chloride in a polyethylene glycol formulation as a neuroprotective therapy for acute spinal cord injury: preclinical refinement and optimization. J. Neurotrauma 26, 1379–1393 (2009).
Streijger, F. et al. The evaluation of magnesium chloride within a polyethylene glycol formulation in a porcine model of acute spinal cord injury. J. Neurotrauma 33, 2202–2216 (2016).
Halt, P. S., Swanson, R. A. & Faden, A. I. Alcohol exacerbates behavioral and neurochemical effects of rat spinal cord trauma. Arch. Neurol. 49, 1178–1184 (1992).
Rivlin, A. S. & Tator, C. H. Effect of vasodilators and myelotomy on recovery after acute spinal cord injury in rats. J. Neurosurg. 50, 349–352 (1979).
Cheriyan, T. et al. Spinal cord injury models: a review. Spinal Cord. 52, 588–595 (2014).
Lopez, S. et al. Intrathecal bupivacaine protects against extension of lesions in an acute photochemical spinal cord injury model. Can. J. Anaesth. 51, 364–372 (2004).
Hao, J. X., Xu, X. J., Aldskogius, H., Seiger, A. & Wiesenfeld-Hallin, Z. Beneficial effect of the opioid receptor antagonist naltrexone on hyper-sensitivity induced by spinal cord ischemia in rats: disassociation with MK-801. Restor. Neurol. Neurosci. 3, 257–266 (1991).
Madsen, J. R. et al. Tacrolimus (FK506) increases neuronal expression of GAP-43 and improves functional recovery after spinal cord injury in rats. Exp. Neurol. 154, 673–683 (1998).
Piao, M.-S. et al. Melatonin improves functional outcome via inhibition of matrix metalloproteinases-9 after photothrombotic spinal cord injury in rats. Acta Neurochir. 156, 2173–2182 (2014).
Afhami, M. et al. The demyelination and altered motor performance following electrolytic lesion in the ventrolateral white matter of spinal cord in male rats: benefit of post-injury administration of estradiol. Life Sci. I 20, 157–171 (2016).
Basso, D. M., Beattie, M. S. & Bresnahan, J. C. A sensitive and reliable locomotor rating scale for open field testing in rats. J. Neurotrauma 12, 1–21 (1995).
Basso, D. M. et al. Basso Mouse Scale for locomotion detects differences in recovery after spinal cord injury in five common mouse strains. J. Neurotrauma 23, 635–659 (2006).
Song, R. B. et al. Adaptation of the Basso-Beattie-Bresnahan locomotor rating scale for use in a clinical model of spinal cord injury in dogs. J. Neurosci. Methods 268, 117–124 (2016).
Hook, M. A. et al. Neurobiological effects of morphine after spinal cord injury. J. Neurotrauma 34, 632–644 (2017).
Leech, K. A., Kinnaird, C. R. & Hornby, T. G. Effects of serotonergic medications on locomotor performance in humans with incomplete spinal cord injury. J. Neurotrauma 31, 1334–1342 (2014).
Evaniew, N. et al. Methylprednisolone for the treatment of patients with acute spinal cord injuries: a propensity score-matched cohort study from a Canadian multi-center spinal cord injury registry. J. Neurotrauma 32, 1674–1683 (2015).
Kim, H. S. et al. Epidemiology of spinal cord injury: changes to its cause amid aging population, a single center study. Ann. Rehabil. Med. 45, 7–15 (2021).
Kang, Y. et al. Epidemiology of worldwide spinal cord injury: a literature review. J. Neurorestoratol. 6, 1–9 (2017).
Devivo, M. J. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 50, 365–372 (2012).
Bourguignon, L. et al. International surveillance study in acute spinal cord injury confirms viability of multinational clinical trials. BMC Med. 20, 225 (2022).
Bracken, M. B. et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N. Engl. J. Med. 322, 1405–1411 (1990).
Ito, Y., Sugimoto, Y., Tomioka, M., Kai, N. & Tanaka, M. Does high dose methylprednisolone sodium succinate really improve neurological status in patient with acute cervical cord injury?: a prospective study about neurological recovery and early complications. Spine 34, 2121–2124 (2009).
Ning, G.-Z., Wu, Q., Li, Y.-L. & Feng, S.-Q. Epidemiology of traumatic spinal cord injury in Asia: a systematic review. J. Spinal Cord. Med 35, 229–239 (2012).
Rahimi-Movaghar, V. et al. Epidemiology of traumatic spinal cord injury in developing countries: a systematic review. Neuroepidemiology 41, 65–85 (2013).
Thompson, C. K. & Hornby, T. G. Divergent modulation of clinical measures of volitional and reflexive motor behaviors following serotonergic medications in human incomplete spinal cord injury. J. Neurotrauma 30, 498–502 (2013).
Maric, O., Zörner, B. & Dietz, V. Levodopa therapy in incomplete spinal cord injury. J. Neurotrauma 25, 1303–1307 (2008).
Bracken, M. B. et al. Methylprednisolone or naloxone treatment after acute spinal cord injury: 1-year follow-up data: results of the second National Acute Spinal Cord Injury Study. J. Neurosurg. 76, 23–31 (1992).
Bracken, M. B. & Holford, T. R. Effects of timing of methylprednisolone or naloxone administration on recovery of segmental and long-tract neurological function in NASCIS 2. J. Neurosurg. 79, 500–507 (1993).
Casha, S. et al. Results of a phase II placebo-controlled randomized trial of minocycline in acute spinal cord injury. Brain 135, 1224–1236 (2012).
Clark, M. J. et al. Testosterone replacement therapy and motor function in men with spinal cord injury: a retrospective analysis. Am. J. Phys. Med. Rehabil. 87, 281–284 (2008).
Aminmansour, B. et al. Effects of progesterone and vitamin D on outcome of patients with acute traumatic spinal cord injury; a randomized, double-blind, placebo controlled study. J. Spinal Cord. Med. 39, 272–280 (2016).
Wilson, J. R. et al. Natural history, predictors of outcome, and effects of treatment in thoracic spinal cord injury: a multi-center cohort study from the North American Clinical Trials Network. J. Neurotrauma 35, 2554–2560 (2018).
Sunshine, J. E. et al. Methylprednisolone therapy in acute traumatic spinal cord injury: analysis of a regional spinal cord model systems database. Anesth. Analg. 124, 1200–1205 (2017).
Felleiter, P., Müller, N., Schumann, F., Felix, O. & Lierz, P. Changes in the use of the methylprednisolone protocol for traumatic spinal cord injury in Switzerland. Spine 37, 953–956 (2012).
Tsutsumi, S., Ueta, T., Shiba, K., Yamamoto, S. & Takagishi, K. Effects of the second national acute spinal cord injury study of high-dose methylprednisolone therapy on acute cervical spinal cord injury-results in spinal injuries center. Spine 31, 2992–2996 (2006).
Nacar, O. A. et al. Systemic administration of atorvastatin improves locomotor functions and hyperacute-acute response after experimental spinal cord injury: an ultrastructural and biochemical analysis. Turk. Neurosurg. 24, 337–343 (2014).
Zhang, D., Wang, F., Zhai, X., Li, X.-H. & He, X.-J. Lithium promotes recovery of neurological function after spinal cord injury by inducing autophagy. Neural Regen. Res 13, 2191–2199 (2018).
Hao, H.-H. et al. Valproic acid reduces autophagy and promotes functional recovery after spinal cord injury in rats. Neurosci. Bull. 29, 484–492 (2013).
Zhang, Y. et al. Melatonin improves functional recovery in female rats after acute spinal cord injury by modulating polarization of spinal microglial/macrophages. J. Neurosci. Res. 97, 733–743 (2019).
Hubsher, G., Haider, M. & Okun, M. S. Amantadine: the journey from fighting flu to treating Parkinson disease. Neurology 78, 1096–1099 (2012).
Corbett, A. et al. Drug repositioning for Alzheimer’s disease. Nat. Rev. Drug Discov. 11, 833–846 (2012).
Ashburn, T. T. & Thor, K. B. Drug repositioning: identifying and developing new uses for existing drugs. Nat. Rev. Drug Discov. 3, 673–683 (2004).
Nosengo, N. Can you teach old drugs new tricks? Nature 534, 314–316 (2016).
Kwon, B. K. et al. Demonstrating efficacy in preclinical studies of cellular therapies for spinal cord injury - how much is enough? Exp. Neurol. 248, 30–44 (2013).
Rojas, L. B. A. & Gomes, M. B. Metformin: an old but still the best treatment for type 2 diabetes. Diabetol. Metab. Syndr. 5, 6 (2013).
Guo, Y. et al. Metformin protects against spinal cord injury by regulating autophagy via the mTOR signaling pathway. Neurochem. Res. 43, 1111–1117 (2018).
Zhang, T. et al. Therapeutic effect of metformin on inflammation and apoptosis after spinal cord injury in rats through the Wnt/β-catenin signaling pathway. Neurosci. Lett. 739, 135440 (2020).
Hook, M. A. et al. The impact of morphine after a spinal cord injury. Behav. Brain Res 179, 281–293 (2007).
Hook, M. A. et al. Intrathecal morphine attenuates recovery of function after a spinal cord injury. J. Neurotrauma 26, 741–752 (2009).
Hook, M. A. et al. An IL-1 receptor antagonist blocks a morphine-induced attenuation of locomotor recovery after spinal cord injury. Brain Behav. Immun. 25, 349–359 (2011).
Woller, S. A. Analgesia Or Addiction: Implications for Morphine Use After Spinal Cord Injury (Texas A & M University, 2012).
Faden, A. I., Jacobs, T. P. & Holaday, J. W. Opiate antagonist improves neurologic recovery after spinal injury. Science 211, 493–494 (1981).
Faden, A. I., Jacobs, T. P. & Holaday, J. W. Comparison of early and late naloxone treatment in experimental spinal injury. Neurology 32, 677–681 (1982).
Popovich, P. G., Lemeshow, S., Gensel, J. C. & Tovar, C. A. Independent evaluation of the effects of glibenclamide on reducing progressive hemorrhagic necrosis after cervical spinal cord injury. Exp. Neurol. 233, 615–622 (2012).
Andreollo, N. A., Santos, E. F., dos Araújo, M. R. & Lopes, L. R. Rat’s age versus human’s age: what is the relationship? Arq. Bras. Cir. Dig. 25, 49–51 (2012).
Dutta, S. & Sengupta, P. Men and mice: Relating their ages. Life Sci. 152, 244–248 (2016).
Cambridge, R. Modeling the age difference between humans and Felis catus biological cat age: the actual age of a cat. J. Anim. Res. Nutr. 02, https://doi.org/10.21767/2572-5459.100034 (2017).
Wang, T. et al. Quantitative translation of dog-to-human aging by conserved remodeling of the DNA methylome. Cell Syst. 11, 176–85.e6 (2020).
Sengupta, P. & Dutta, S. Mapping the age of laboratory rabbit strains to human. Int. J. Prev. Med. 11, 194 (2020).
Flurkey, K., Mcurrer, J. & Harrison, D. Mouse models in aging research. in The Mouse in Biomedical Research 637–672 (Elsevier, 2007).
Guest, J., Datta, N., Jimsheleishvili, G. & Gater, D. R. Jr. Pathophysiology, classification and comorbidities after traumatic spinal cord injury. J. Pers. Med. 12, https://doi.org/10.3390/jpm12071126 (2022).
Ueno, T. et al. Hyperphosphorylated neurofilament NF-H as a biomarker of the efficacy of minocycline therapy for spinal cord injury. Spinal Cord. 49, 333–336 (2011).
Lee, J. Y., Kim, H. S., Choi, H. Y., Oh, T. H. & Yune, T. Y. Fluoxetine inhibits matrix metalloprotease activation and prevents disruption of blood-spinal cord barrier after spinal cord injury. Brain 135, 2375–2389 (2012).
Assinck, P. et al. Transplantation of skin precursor-derived schwann cells yields better locomotor outcomes and reduces bladder pathology in rats with chronic spinal cord injury. Stem Cell Rep. 15, 140–155 (2020).
Powers, B. E. et al. Remyelination reporter reveals prolonged refinement of spontaneously regenerated myelin. Proc. Natl. Acad. Sci. USA 110, 4075–4080 (2013).
Ghnenis, A. B. et al. Evaluation of the cardiometabolic disorders after spinal cord injury in mice. Biology 11, https://doi.org/10.3390/biology11040495 (2022).
Bourguignon, L., Lukas, L. P. & Jutzeler, C. Impact of commonly administered drugs on the progression of spinal cord injury: a systematic review (code and data). https://doi.org/10.5281/zenodo.13871856.
Apostolova, N. et al. Mechanisms of action of metformin in type 2 diabetes: effects on mitochondria and leukocyte-endothelium interactions. Redox Biol. 34, 101517 (2020).
Zhou, L.-Y. et al. The effect of metformin on ameliorating neurological function deficits and tissue damage in rats following spinal cord injury: a systematic review and network meta-analysis. Front Neurosci. 16, 946879 (2022).
Weitz-Schmidt, G. Statins as anti-inflammatory agents. Trends Pharm. Sci. 23, 482–486 (2002).
Holmberg, E. et al. Simvastatin promotes neurite outgrowth in the presence of inhibitory molecules found in central nervous system injury. J. Neurotrauma 23, 1366–1378 (2006).
Malfitano, A. M. et al. Statins in neurological disorders: an overview and update. Pharm. Res 88, 74–83 (2014).
Zhao, Y.-J. et al. Lithium promotes recovery after spinal cord injury. Neural Regen. Res 17, 1324–1333 (2022).
Li, B. et al. Lithium inhibits GSK3β activity via two different signaling pathways in neurons after spinal cord injury. Neurochem. Res. 43, 848–856 (2018).
Reavis, K., Abrams, M., Dimas, G., Meier, N. & Fusick, A. J. Lithium for pain management and suicidality in spinal cord injury patients: a case report and review of the literature. Psychiatry Res. Case Rep. 2, 100131 (2023).
Göttlicher, M. et al. Valproic acid defines a novel class of HDAC inhibitors inducing differentiation of transformed cells. EMBO J. 20, 6969–6978 (2001).
Dai, Y. et al. Classical HDACs in the regulation of neuroinflammation. Neurochem Int 150, 105182 (2021).
Yang, Q., Zhang, H., Jin, Z., Zhang, B. & Wang, Y. Effects of valproic acid therapy on rats with spinal cord injury: a systematic review and meta-analysis. World Neurosurg. 182, 12–28 (2024).
Zhang, Y. et al. Melatonin for the treatment of spinal cord injury. Neural Regen. Res 13, 1685–1692 (2018).
Shvetcov, A. et al. The neuroprotective effects of estrogen and estrogenic compounds in spinal cord injury. Neurosci. Biobehav. Rev. 146, 105074 (2023).
Elkabes, S. & Nicot, A. B. Sex steroids and neuroprotection in spinal cord injury: a review of preclinical investigations. Exp. Neurol. 259, 28–37 (2014).
Stampas, A. et al. The first 24 h: opioid administration in people with spinal cord injury and neurologic recovery. Spinal Cord. 58, 1080–1089 (2020).
Flamm, E. S. et al. Ethanol potentiation of central nervous system trauma. J. Neurosurg. 46, 328–335 (1977).
Furlan, J. C. & Fehlings, M. G. Blood alcohol concentration as a determinant of outcomes after traumatic spinal cord injury. Eur. J. Neurol. 20, 1101–1106 (2013).
Pollard, M. E. & Apple, D. F. Factors associated with improved neurologic outcomes in patients with incomplete tetraplegia. Spine 28, 33–39 (2003).
Acknowledgements
This study was supported by the Swiss National Science Foundation (Ambizione Grant, #PZ00P3_186101 and #IZLIZ3_200275, C.R.J.), Wings for Life Research Foundation (#2017_044, #ID 2020_118, C.R.J. and J.L.K.K.), the International Foundation for Research in Paraplegia (#P192, C.R.J.). L.B. was supported by an ICORD student exchange award provided by the Praxis Spinal Cord Injury Foundation. B.R.K. was supported by the Paralyzed Veterans of America Research Foundation (# 3195). The authors would like to thank Najmeh Kheram for her support in analyzing studies published in Persian. The following icons from thenounproject.com were used: “Average” icon by James Bickerton CC BY 3.0; “Less or equal” icon by Julia Holmberg CC BY 3.0; “Pin” icon by Nice Design CC BY 3.0; “Direction” icon by Uswa KDT CC BY 3.0; “Pill” icon by Three Six Five CC BY 3.0; “Shuffle” icon by Gregor Cresnar CC BY 3.0; “Syringe” icon by arman maulana CC BY 3.0; “Vaccination” icon by WiStudio CC BY 3.0; “Empty set” icon by Gregor Cresnar CC BY 3.0. Statistical Analyses completed by: L.B. and L.P.L. (Swiss Federal Institute of Technology, ETH Zurich).
Author information
Authors and Affiliations
Contributions
All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. L.B.: selection of studies, extraction of data, statistical analysis, visualization, interpretation of the data, drafting of the manuscript; L.P.L.: selection of studies, extraction of data, statistical analysis, visualization, interpretation of the data, drafting of the manuscript; B.R.K.: interpretation of data, revising the manuscript for intellectual content; B.T.: extraction of data, interpretation of data, revising the manuscript for intellectual content; J.J.L.: extraction of data, interpretation of data, revising the manuscript for intellectual content; T.G.: extraction of data, interpretation of data, revising the manuscript for intellectual content; W.T.: interpretation of data, revising the manuscript for intellectual content; J.L.K.K.: interpretation of data, revising the manuscript for intellectual content; M.W.: study design, selection of studies, interpretation of data, revising the manuscript for intellectual content; C.R.J.: study design, selection of studies, extraction of data, visualization, interpretation of the data, drafting of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
M.W. has received/is receiving funding from Michael Smith Foundation for Health Research in partnership with the Rick Hansen Foundation, University Hospital Basel, Wellspect, Coloplast, Stoke Mandeville Spinal Research, International Foundation for Research in Paraplegia, and Swiss Multiple Sclerosis Society. M.W. reports advisory board activity for Coloplast from 2022 to 2024.
Peer review
Peer review information
Communications Medicine thanks Michelle Hook and Andrew Stevens for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bourguignon, L., Lukas, L.P., Kondiles, B.R. et al. Impact of commonly administered drugs on the progression of spinal cord injury: a systematic review. Commun Med 4, 213 (2024). https://doi.org/10.1038/s43856-024-00638-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s43856-024-00638-0