Abstract
Background
A skeletal muscle strength (SMS) decline is associated with metabolic diseases, but whether SMS also declines with chronic kidney disease (CKD) in individuals with metabolic dysfunction-associated steatotic liver disease (MASLD) is uncertain. This study examined the associations between SMS and the risk of CKD in MASLD population.
Method
We performed a large-scale study with four cohorts: PERSONS and NHANES 2011–2014 cohorts for the cross-sectional investigation, and TCLSIH and UK Biobank cohorts for the longitudinal investigation. A handgrip dynamometer measured handgrip strength as a proxy for overall SMS. Participants were stratified according to CKD status [non-CKD vs. CKD (stages 1–5) groups].
Results
In the PERSONS cohort, the CKD group has a lower handgrip strength than the non-CKD group (27.14 ± 9.19 vs. 33.59 ± 11.92 kg, P < 0.001). Higher handgrip strength is associated with lower odds of abnormal albuminuria or CKD (OR: 0.96, 95%CI:0.92-0.99 and OR:0.95, 95%CI: 0.91-0.99 respectively). The highest handgrip strength tertile is associated with the lowest risk of having abnormal albuminuria or CKD (compared with the lowest or middle tertile). Results are similar in NHANES cohort. Furthermore, the highest handgrip strength is independently associated with the lowest risk of incident CKD in MASLD (HR: 0.95, 95%CI: 0.92-0.99 and HR:0.99, 95%CI: 0.98-0.99 in TCLSIH and UK Biobank cohorts). In Kaplan-Meier curve analysis, the cumulative incidence of CKD is lowest in the highest handgrip strength tertile compared to the lowest or the middle tertile.
Conclusions
Higher handgrip/muscle strength is independently associated with a lower risk of CKD and abnormal albuminuria in MASLD population.
Plain language summary
Metabolic dysfunction-associated steatotic liver disease (MASLD) occurs when there is too much fat in the liver. People with MASLD have an increased risk of developing chronic kidney disease (CKD). Skeletal muscles are responsible for voluntary movements and are crucial for movement and health. We investigated whether skeletal muscle strength (SMS), assessed using handgrip strength, was associated with the risk of CKD in individuals with MASLD. Based on data from over 14,000 participants we found that higher SMS was associated with a lower risk of CKD. These findings suggest that preserving skeletal muscle strength may help prevent people with MASLD developing kidney disease.
Similar content being viewed by others
Introduction
Metabolic dysfunction-associated steatotic liver disease (MASLD), also known as metabolic dysfunction-associated fatty liver disease (MAFLD), affects up to a third of the world’s adult population and has become a major global public health challenge1,2,3,4. MASLD not only increases liver-related morbidity and mortality but is also a multisystem disease, affecting multiple extra-hepatic organs and regulatory pathways5,6,7. It has been reported that MASLD is strongly associated with abnormal albuminuria and chronic kidney disease (CKD), regardless of the presence of obesity, type 2 diabetes mellitus (T2DM) or hypertension8,9. In a recent Delphi consensus study, international experts have developed and endorsed consensus statements guiding the epidemiology, management, and treatment of MASLD with CKD8. Recently, there has been controversy over pathological tissue/organ crosstalk, and skeletal muscle dysfunction may be a novel risk factor for CKD in the MASLD population10
It is known that there is a substantial decline in skeletal muscle strength (SMS) and mass in the aging population11. Skeletal muscle loss is associated with functional disability, greater bone fracture risk, cardiometabolic disorders, poor quality of life, and even death12,13. Studies have also reported that reduced handgrip strength, as a proxy for overall SMS, is associated with the development and progression of MASLD10,14,15. To our knowledge, however, no studies have extensively assessed the association between handgrip strength and the risk of CKD in people with MASLD.
Therefore, the primary aim of this study, which included four independent cohorts from various countries, was to evaluate the magnitude of the association between SMS and the risk of prevalent and incident CKD in individuals with MASLD. Identifying any potential association could offer valuable insights into the contributing role of SMS in the development of kidney dysfunction and potentially inform treatment strategies to prevent CKD in individuals with MASLD. The findings of our study indicate that higher handgrip strength is significantly associated with a lower prevalence and incidence of CKD in the MASLD population.
Materials and methods
Study design
This is a large-scale multinational study, which included 14,079 Asian and non-Asian adult individuals with MASLD. We first performed a cross-sectional investigation to assess the association between handgrip strength and the prevalence of CKD or abnormal albuminuria in the MASLD population. Subsequently, we performed a longitudinal investigation to examine the association between handgrip strength and the incidence of CKD.
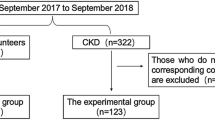
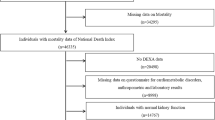
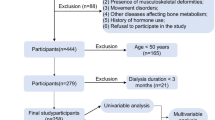
Participants
This study included individuals with MASLD from four independent cohorts (as shown in Fig. 1). Specifically, we included the PERSONS (Prospective Epidemic Research Specially Of NASH) cohort, which enrolled 460 Chinese adults admitted to the Hepatology Center of the First Affiliated Hospital of Wenzhou Medical University for liver biopsy examination (from 2017 to 2022) and approved by the Ethics Committees of the First Affiliated Hospital of Wenzhou Medical University (2016–246); the NHANES (National Health and Nutrition Examination Survey) 2011–2014 cohort (obtained from URL: http://www.cdc.gov/nchs/nhanes.htm), which involved 1,414 participants with hepatic steatosis index (HSI)-detected MASLD (annotated from 2011 to 2014) and approved by the National Center for Health Statistics (NCHS) Ethics Review Board; the TCLSIH (Tianjin Chronic Low-grade Systemic Inflammation and Health) cohort, which was a large prospective dynamic population cohort study of adults living in Tianjin (China) with 6,358 subjects with ultrasound-detected MASLD (recruited from 2013 to 2016) and approved by the Institutional Review Board of Tianjin Medical University (TMUhMEC 201430); and the UK Biobank cohort (obtained from URL: https://www.ukbiobank.ac.uk/enable-your-research/register with UKB permission), which was a large population-based prospective cohort with 5,847 UK participants with MASLD diagnosed by ultrasonography (recruited from 2006 to 2010) and approved by the National Health Service (NHS) North West Centre for Research Ethics Committee (11/NW/0382). All participants signed a written informed consent to participate in the study.
Patients from the four independent cohorts were identified with a single etiology to their MASLD, and MASLD was defined by the presence of hepatic steatosis in combination with at least one cardiometabolic risk factor, including overweight/obesity, T2DM, or evidence of metabolic dysregulation16,17,18. The exclusion criteria for our study were as follows: (1) hepatocyte steatosis <5% on liver histology in the PERSONS cohort; (2) other liver diseases, such as alcoholic liver disease, viral hepatitis or autoimmune hepatitis; (3) missing data on kidney function, including estimated glomerular filtration rate (eGFR) and albuminuria; (4) other known kidney diseases in the cross-sectional cohorts and pre-existing kidney conditions in the longitudinal cohorts; and (5) missing data on skeletal muscle strength measurements.
Liver biopsy examination
All participants in the PERSONS cohort underwent percutaneous liver biopsy guided by ultrasound. An expert liver pathologist blinded to the data collection analyzed all liver histology specimens in detail, including quantification of steatosis, hepatocyte ballooning and lobular inflammation16,19. Fibrosis stages were graded based on Brunt’s histology criteria, and significant fibrosis was defined as a histologic stage F ≥ 2 16.
Skeletal muscle strength measurement
Handgrip strength, as a proxy for overall SMS, was measured using a handgrip dynamometer (the Camry Digital EH101 dynamometer in the PERSONS and TCLSIH cohorts, the Takei Digital Grip Strength dynamometer in the NHANES cohort, and the Jamar J00105 hydraulic hand dynamometer in the UK Biobank cohort). According to the guidance, all participants were instructed to set their elbows at a 90° angle flexion while standing or sitting. They kept a neutral wrist position and had their upper arms vertically set against the trunk20. Participants performed maximum-force squeezes three times for each hand with professional instruction, and the mean of the three readings was recorded for analysis. Handgrip strength measurements did not apply to participants with prior surgical operations, arthritis, injury, or other defects in the last 6 months21 and these subjects were excluded from the study. Handgrip strength was reported in absolute terms since it has previously been demonstrated that the association between handgrip strength and health outcomes did not differ according to whether handgrip strength was expressed in absolute or relative terms22. In addition, we categorized handgrip strength (expressed in kg) into the highest, middle, and lowest groups according to tertiles in the four cohorts. The mean handgrip strength in the lowest, middle, and highest groups for the PERSONS cohort were: 20.6 ± 4.8 vs. 32.6 ± 2.8 vs. 45.7 ± 8.6 kg; for the NHANES 2011–2014 cohort: 21.6 ± 3.3 vs. 29.3 ± 2.1 vs. 42.5 ± 7.6 kg; for the TCLSIH cohort: 32.2 ± 7.2 vs. 39.2 ± 7.2 vs. 46.6 ± 9.1 kg; and for the UK Biobank cohort: 23.2 ± 8.6 vs. 31.8 ± 8.6 vs. 39.0 ± 10.8 kg, respectively.
CKD assessment
Although glomerular filtration rate (GFR) is the best tool for diagnosing, staging, and managing CKD, its measurement is labor-intensive, costly, and not widely accessible23. In our analysis, we estimated GFR using the CKD-Epidemiology Collaboration (CKD-EPI) equation, a widely used first-line tool, which may be influenced by factors such as muscle mass, age, gender, diet, and hydration status24,25. CKD-EPI equation was as follows: eGFR = 141 × min (Scr/κ, 1)α × max (Scr/κ, 1)-1.209 × 0.993age × 1.018 [if female], where Scr is serum creatinine, κ is 0.7 for females and 0.9 for males, α is –0.329 for females and –0.411 for males, min indicates the minimum of Scr/κ or 1, and max indicates the maximum of Scr/κ or 1. CKD stages were defined according to the KDIGO guidelines as follows: stage 1, urinary albumin-to-creatinine ratio (ACR) ≥ 30 mg/g with eGFR ≥ 90 ml/min/1.73 m2; stage 2, ACR ≥ 30 mg/g with eGFR of 60–89 ml/min/1.73 m2; stage 3, eGFR of 30–59 ml/min/1.73 m2 (with or without abnormal ACR); stage 4, eGFR of 15–29 ml/min/1.73 m2; and stage 5, eGFR < 15 ml/min/1.73 m2. In the present study, all participants were stratified into the non-CKD and CKD (stages 1 to 5) groups, respectively.
Demographic, clinical and laboratory data
All participants’ related data were obtained by highly trained medical personnel and included biochemical parameters, anthropometric variables, and demographic data. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. The presence of hypertension was diagnosed by a blood pressure of ≥ 130/85 mmHg or the current use of any anti-hypertensive medication. T2DM was characterized by either self-reported physician diagnosis, the use of anti-diabetic medications, fasting glucose levels ≥ 7 mmol/L, or a hemoglobin A1c (HbA1c) level ≥ 6.5% (≥ 48 mmol/mol)16.
Statistics and reproducibility
Statistical analyses were conducted using the R statistical package (The R Foundation; http://www.r-project.org; version 3.4.3) and Empower (R) (www.empowerstats.com; X & Y Solution, Inc., Boston, MA, USA). Continuous variables were expressed as means ± SD or medians with interquartile ranges (IQR) and compared using the unpaired Student’s t-test or the Mann-Whitney test based on whether the data distribution was normal or skewed. Categorical variables were expressed as percentages and compared using the chi-square test or Fisher’s exact test for small numbers, as appropriate. Cross-sectional associations between handgrip strength and the risk of prevalent CKD or abnormal albuminuria (urinary ACR ≥ 30 mg/g) were first investigated using binary logistic regression analysis by tertiles of exposure. Participants in the lowest handgrip strength tertile were used as the reference group in each logistic regression model, and the results were reported as odds ratios (OR) and 95% confidence intervals (CIs). Analyses were adjusted for common risk factors for CKD, including age, sex, ethnicity, BMI, T2DM and hypertension. The overall diagnostic accuracy of this logistic regression model for discrimination between CKD and non-CKD status was evaluated by the receiver operator characteristic (ROC) curve analysis and was expressed as the area under the receiver operator characteristic curve (AUROC). We also calculated diagnostic indexes, including sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio, and negative likelihood ratio. Cox proportional hazards regression models were used to assess the longitudinal association between handgrip strength and the risk of developing incident CKD and expressed as hazard ratio (HR) and 95% CIs. Kaplan-Meier survival curves were also performed to study the cumulative incidence rates of CKD according to baseline handgrip strength tertiles.
Results
Characteristics of participants in the cross-sectional and longitudinal cohorts
In the two cross-sectional cohorts, 460 Chinese adults with biopsy-confirmed MASLD were enrolled in the PERSONS cohort, among which 44 (9.6%) individuals had CKD stages 1 to 5. A total of 1414 United States adults with MASLD (based on hepatic steatosis index) were enrolled in the NHANES 2011–2014 cohort, among which 271 (19.1%) individuals had CKD stages 1 to 5. As shown in Supplementary Table 1, in the PERSONS cohort, patients with CKD were more likely to be female and older and had lower eGFR and higher levels of urinary ACR, HbA1c and fasting glucose. Patients with CKD also had a higher prevalence of T2DM and hypertension. Furthermore, those with CKD were more likely to have significant liver fibrosis on liver histology than those without CKD. Notably, handgrip strength was conspicuously lower in the CKD group than in the non-CKD group (27.14 ± 9.19 vs. 33.59 ± 11.92 kg; P < 0.001). Similar results were observed in the NHANES cohort, with 27.39 ± 8.83 kg in the CKD group and 32.00 ± 10.00 kg in the non-CKD group, respectively. However, the ethnic composition of the NHANES cohort included Mexican Americans, non-Hispanic Whites and others, which differed from the Chinese PERSONS cohort, which was predominantly of a single ethnicity.
As for the two prospective cohorts, the attrition rates were 10.70% and 0.00% in the TCLSIH cohort and the UK Biobank cohort, respectively. In the TCLSIH cohort (a dynamic adult population cohort study of individuals living in Tianjin, China), at the baseline, subjects who developed incident CKD over the follow-up were more likely to be older and had higher proportions of metabolic syndrome traits, with 28.07% T2DM and 82.46% hypertension, compared to those who did not. Furthermore, subjects who developed incident CKD also had lower baseline handgrip strength than those who did not (36.01 ± 10.96 vs. 39.38 ± 9.86 kg, P = 0.004). Similar findings were observed in the UK Biobank cohort (including 5,847 participants with ultrasound-detected MASLD), with a baseline handgrip strength of 29.33 ± 11.69 kg in subjects who developed incident CKD over the follow-up and 31.66 ± 11.65 kg in those who did not.
Cross-sectional associations between handgrip strength and risk of abnormal albuminuria
As shown in Fig. 2a, b, in the PERSONS and NHANES cohorts, we found an inverse linear association between handgrip strength and the risk of having abnormal albuminuria in the MASLD group with CKD. In multivariable logistic regression modeling (Table 1) with the presence of abnormal albuminuria as the dependent variable, the inverse association between handgrip strength and the risk of abnormal albuminuria remained evident even after adjustment of sex, age, BMI, T2DM and hypertension (adjusted OR: 0.96, 95%CI: 0.92-0.99, P = 0.023 in the PERSONS cohort, and adjusted OR: 0.96, 95%CI: 0.93–0.98, P = 0.002 in the NHANES cohort). Figure 2c shows the risk of having abnormal albuminuria according to handgrip strength tertiles in the PERSONS cohort. Compared with those in the lowest tertile, individuals in the middle or the highest tertile of handgrip strength had an OR of 0.38 (95%CI: 0.15-0.97) and 0.29 (95% CI: 0.11-0.80) for having abnormal albuminuria, after adjusting for sex, age, BMI, T2DM and hypertension. Similar associations between handgrip strength tertiles and the risk of abnormal albuminuria were observed in the NHANES cohort (Fig. 2c).
a Risk of abnormal albuminuria according to handgrip strength in Chinese patients with biopsy-proven MASLD in the hospital-based cohort. b Risk of abnormal albuminuria according to handgrip strength in the NHANES cohort. c Logistic regression models showing the risk of abnormal albuminuria according to handgrip strength tertiles.
Cross-sectional associations between handgrip strength and risk of prevalent CKD
The smoothing spline curves show an inverse association between handgrip strength and the risk of prevalent CKD (stages 1 to 5) in the PERSONS and NHANES cohorts (Fig. 3a, b). As shown in Table 1, there was a significant inverse association between handgrip strength and the risk of prevalent CKD even after adjustment for common renal risk factors (adjusted OR: 0.95, 95%CI: 0.91–0.99, P = 0.008 in the PERSONS cohort and OR: 0.96, 95%CI: 0.94–0.99, P = 0.004 in the NHANES cohort). Also, we found that there were no significant interactions of potential confounders like T2DM or obesity on the association between handgrip strength and the risk of prevalent CKD (P-interaction > 0.05) (Supplementary Table 2). Figure 3c shows the associations between handgrip strength tertiles and the risk of prevalent CKD in the PERSONS cohort. Compared with those in the lowest tertile, individuals in the middle or the highest tertile of handgrip strength had an OR of 0.30 (95%CI: 0.12–0.77) and an OR of 0.23 (95%CI: 0.09–0.62) for CKD, respectively, after adjustment for potential confounders. Similar findings were observed in the NHANES cohort (Fig. 3c). Based on these findings, we established a non-invasive assessment model that combined handgrip strength, age, sex, BMI, hypertension, and T2DM status to test discrimination between high-risk CKD and non-CKD groups in the MASLD population. The AUROC of this non-invasive assessment model was 0.74 (95% CI: 0.66-0.80) in the PERSONS cohort and 0.72 (95% CI: 0.68–0.75) in the NHANES cohort, respectively (Fig. 4).
Longitudinal associations between handgrip strength and risk of incident CKD
The association between handgrip strength and the risk of developing CKD is shown in Supplementary Table 3, among which the multivariable HRs (95% CI) were 0.95 (0.92-0.99) and 0.99 (0.98-0.99) in the TCLHIS and UK Biobank cohorts, respectively. The inverse association between handgrip strength tertiles and the risk of developing CKD remained significant even after adjusting for sex, age, BMI, T2DM, and hypertension, and was not influenced by baseline eGFR. As for Kaplan-Meier survival analyses, we found that the cumulative incidence rates of CKD had an upward trend in the TCLSIH and UK Biobank cohorts. Figure 5a, b shows that the cumulative incidence rates of CKD were 0.008 and 0.003 per annum, respectively, in the sixth year of follow-up. Figure 5c, d shows the associations between handgrip strength tertiles and the risk of developing incident CKD. When compared with the lowest tertile, the risk of incident CKD was much lower in the middle and the highest handgrip strength tertiles, both in the TCLSIH and UK-Biobank cohorts.
Discussion
As far as we are aware, this is the first large-scale study investigating the cross-sectional and longitudinal associations between handgrip strength, as a proxy for overall SMS, and the risk of having or developing CKD in adults with MASLD. The main and novel findings of our large-scale study that involved four independent cohorts of adults with MASLD from different countries are as follows: (a) higher handgrip strength was significantly associated with a lower prevalence and incidence of CKD or abnormal albuminuria in adults with MASLD; (b) this association remained evident even after adjusting for common renal risk factors, such as sex, age, ethnicity, obesity, hypertension, and T2DM; and (c) these findings have been reported in both Asian and non-Asian adults, thus reducing the bias of differential metabolic features in distinct geographical areas.
Recent studies have reported a significant inverse association between SMS and MASLD14,15,21. SMS is a key component of sarcopenia that may be involved in the development and progression of MASLD26. Sunyoung et al. found that lower SMS (defined as the lowest quartile of relative handgrip strength) was significantly associated with a 3.6-fold increased risk of prevalent MASLD (OR 3.62, 95%CI 3.25–4.03) even after adjustment of potential confounding factors14. Evidence has also shown the patterns of the association between handgrip strength and risk of severe MASLD. For example, Fanny et al., who followed 333,295 participants from the UK Biobank study for a median of ~10 years, reported that the risk of developing severe MASLD was lower among participants in the middle (HR 0.82; 95%CI 0.76-0.90) and the highest tertile of SMS (HR 0.70; 95%CI 0.64-0.77) compared to those in the lowest tertile15. Also, lower SMS was independently associated with a higher long-term risk of overall mortality in patients with MASLD21. As for the complications of MASLD, evidence demonstrates that lower SMS is associated with a higher risk of reduced pulmonary function in individuals with MASLD27. Previous studies have also reported an inverse association between SMS and CKD in the general population28,29,30,31. CKD may decrease SMS, reducing the patient’s quality of life and increasing the risk of morbidity and mortality30. To our knowledge, there have been no clinical studies examining the relationship between SMS and the risk of having or developing CKD in people with MASLD until now. Our large-scale study found that handgrip strength was much lower in the MASLD population with CKD, and higher handgrip strength, a proxy for overall SMS, was significantly associated with a lower prevalence and incidence of CKD, even after adjustment for common renal risk factors, such as sex, age, ethnicity, obesity, hypertension, and T2DM.
The pathogenic mechanisms linking handgrip strength/SMS to the risk of CKD in MASLD have not been fully elucidated. Skeletal muscle is one of the most important tissues for insulin-mediated glucose metabolism. Skeletal muscle loss can reduce insulin-mediated glucose disposal and, in turn, increase whole-body insulin resistance, which is causally involved in the development of cardiometabolic diseases5,32,33. Thus, we speculate that a decrease in SMS may adversely affect the prevalence and incidence of CKD in people with MASLD, and insulin resistance is one of the most relevant mechanisms linking lower SMS to the risk of CKD in the MASLD population. Other mechanisms linking SMS to CKD in MASLD may involve endothelial dysfunction and altered adipokine production that further exacerbate CKD development in metabolic diseases12. The association between MASLD and CKD has been investigated in recent years, and it has been shown that MASLD is independently associated with an increased prevalence and incidence of CKD34. For example, it has also been reported that MASLD was significantly associated with an increased prevalence (OR 2.12, 95%CI 1.69-2.66) and incidence of CKD (HR 1.79, 95%CI 1.65-1.95), and the severity of MASLD was independently associated with CKD and abnormal albuminuria9,35. Consequently, we speculate that lower SMS may exert adverse effects on the development and progression of CKD as we observed such association in four independent large cohorts of subjects from different countries, all of whom had MASLD.
A sedentary lifestyle may also impair muscle regeneration by reducing satellite cell content, decreasing myogenic potential, and increasing fibrosis36. Conversely, physical activity and exercise are well-established counter-measures against muscle wasting and are also advocated as part of a lifestyle habit essential to decreasing the risk of CKD in patients with MASLD36,37,38. Exercise may help mitigate the decline in muscle regeneration by increasing the activation of satellite cells, improving the myogenic potential, and reducing fibrosis formation. Additionally, exercise improves whole-body insulin sensitivity and adipokine balance36,39. Furthermore, physical activity is also beneficial for CKD management. In a meta-analysis comparing exercise training with sham or no exercise found that aerobic capacity, Heiwe et al. found that cardiovascular function, low-grade inflammation, and health-related quality of life were associated with various exercise interventions in patients with CKD40. This suggests that individualized physical activity prescription in patients with CKD is the primary treatment strategy. In addition, exercise can also benefit the liver and improve MASLD severity to some extent by decreasing hepatic steatosis and inflammation. Current evidence shows that aerobic and resistance exercise may produce comparable therapeutic effects in MASLD with similar frequency, duration, and periods of exercise (40–45 min/session three times/week for 12 weeks)41. Increased physical activity may, therefore, be important in the MASLD population to decrease the long-term risk of developing CKD.
Notably, our large-scale study included both Asian and non-Asian adult individuals from hospital-based and community-based cohorts, thus avoiding the bias of differential metabolic features in distinct geographical areas. However, our study also has some important limitations. First, our study contains four cohorts, among which some parameters are missing across cohorts, such as nutritional status, use of certain medications (such as renin-angiotensin system inhibitors and diuretics), electrolyte levels (e.g., hyperkalemia), inflammatory biomarkers, and socioeconomic status. Second, liver biopsy examination (used in the hospital-based cohort of Chinese patients with MASLD) is regarded as the gold standard method for diagnosing and staging MASLD, but this method is expensive and unethical to perform in community-based cohort studies. The blood-based scores (such as HSI) and liver ultrasonography are non-invasive diagnostic tests of hepatic steatosis that have acceptable sensitivity and specificity and were used to assess the presence of MASLD instead of liver biopsy in our community-based cohorts. Third, serum cystatin C concentration which cannot be affected by factors such as muscle mass, is a more accurate biomarker for assessing kidney function than serum creatinine concentration25. We considered including serum cystatin C level in our study but excluded it to maintain consistency, as serum cystatin C concentration was not measured in all four cohorts. Fourth, although the NHANES cohort data were based on a single eGFR/ ACR measurement, numerous studies over the years have utilized this cohort to investigate CKD-related issues9,42,43. Therefore, we have adopted this approach to expand the scope of our study across diverse populations. Another limitation of the study is the lack of data on physical activity, which may attenuate skeletal muscle strength decline. Evidence has shown that resistance training is the best non-pharmacological intervention to improve and offset the age-related decline in skeletal muscle function 44.
Conclusion
In this large-scale study that involved four independent cohorts from different countries, we found that higher handgrip strength (a reliable marker of overall SMS) was strongly associated with a lower prevalence and incidence of CKD (stages 1 to 5) in adults with MASLD, as detected by liver histology, imaging or blood-based scores. This association remained significant even after adjusting for common renal risk factors, such as age, sex, ethnicity, obesity, hypertension, and T2DM. These findings also suggest that MASLD patients with greater handgrip strength may be less likely to develop CKD.
Abbreviation list
MASLD, metabolic dysfunction-associated steatotic liver disease; MAFLD, metabolic dysfunction-associated fatty liver disease; CKD, chronic kidney disease; SMS, skeletal muscle strength; ACR, albumin to creatinine ratio; eGFR, estimated glomerular filtration rate; HSI, hepatic steatosis index; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; HbA1c, glycated hemoglobin; T2DM, type 2 diabetes mellitus; OR, odds ratio; HR, hazards ratio; CI, confidence interval.
Data availability
The PERSONS cohort was administrated by the team of Professor Ming-Hua Zheng and participants were recruited while they were in the outpatient clinic at the First Affiliated Hospital of Wenzhou Medical University. The TCLSIH Cohort Study was a large prospective dynamic cohort study, managed by the team of Professor Kaijun Niu. Participants were recruited, while having their annual health examinations at the Tianjin Medical University General Hospital-Health Management Center. The underlying data from the PERSONS and TCLSIH cohorts can only be accessed upon specific request due to the presence of potentially sensitive and politically related information. Interested researchers can contact the corresponding author for data access requests via email (zhengmh@wmu.edu.cn). Eligible researchers may access UK Biobank data on www.ukbiobank.ac.uk with UKB permission and NHANES data on www.cdc.gov/nchs/nhanes upon registration. The source data for Figs. 2, 3, 4 and 5 are in Supplementary Data 2 and 3.
References
Feng, G. et al. Recompensation in cirrhosis: unravelling the evolving natural history of nonalcoholic fatty liver disease. Nat. Rev. Gastroenterol. Hepatol. 21, 46–56 (2024).
Younossi, Z. et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 15, 11–20 (2018).
Rinella, M. E. et al. A multi-society Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol. 79, 1542–1556 (2023).
Byrne, C. D. & Targher, G. MASLD, MAFLD, or NAFLD criteria: have we re-created the confusion and acrimony surrounding metabolic syndrome? Metab. Target Organ Damage 4, 10 (2024).
Byrne, C. D. & Targher, G. NAFLD: a multisystem disease. J. Hepatol. 62, S47–S64 (2015).
Wang, T. Y. et al. Association of metabolic dysfunction-associated fatty liver disease with kidney disease. Nat. Rev. Nephrol. 18, 259–268 (2022).
Zhou, X. D. et al. An international multidisciplinary consensus statement on MAFLD and the risk of CVD. Hepatol. Int. 17, 773–791 (2023).
Sun, D. Q. et al. An international Delphi consensus statement on metabolic dysfunction-associated fatty liver disease and risk of chronic kidney disease. Hepatobiliary Surg. Nutr. 12, 386–403 (2023).
Sun, D. Q. et al. MAFLD and risk of CKD. Metabolism 115, 154433 (2021).
Lonardo, A., Mantovani, A., Targher, G. & Baffy, G. Nonalcoholic fatty liver disease and chronic kidney disease: epidemiology, pathogenesis, and clinical and research implications. Int. J. Mol. Sci. 23, 13320 (2022).
Cruz-Jentoft, A. J. & Sayer, A. A. Sarcopenia. Lancet 393, 2636–2646 (2019).
Seo, D. H. et al. Effect of low skeletal muscle mass and sarcopenic obesity on chronic kidney disease in patients with type 2 diabetes. Obesity (Silver Spring) 30, 2034–2043 (2022).
Lopez-Lopez, J. P. et al. The prediction of Metabolic Syndrome alterations is improved by combining waist circumference and handgrip strength measurements compared to either alone. Cardiovasc. Diabetol. 20, 68 (2021).
Kang, S., Moon, M. K., Kim, W. & Koo, B. K. Association between muscle strength and advanced fibrosis in non-alcoholic fatty liver disease: a Korean nationwide survey. J. Cachexia Sarcopenia Muscle 11, 1232–1241 (2020).
Petermann-Rocha, F. et al. Associations of muscle mass and grip strength with severe NAFLD: a prospective study of 333,295 UK Biobank participants. J. Hepatol. 76, 1021–1029 (2022).
Tang, L. J. et al. N-terminal propeptide of type 3 collagen-based sequential algorithm can identify high-risk steatohepatitis and fibrosis in MAFLD. Hepatol. Int. 17, 190–201 (2023).
Ha, S., Wong, V. W., Zhang, X. & Yu, J. Interplay between gut microbiome, host genetic and epigenetic modifications in MASLD and MASLD-related hepatocellular carcinoma. Gut 74, 141–152 (2024).
Perazzo, H., Pacheco, A. G. & Griep, R. H. Changing from NAFLD through MAFLD to MASLD: Similar prevalence and risk factors in a large Brazilian cohort. J. Hepatol. 80, e72–e74 (2024).
Kleiner, D. E. et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 41, 1313–1321 (2005).
Mey, R. et al. Handgrip strength and respiratory disease mortality: Longitudinal analyses from SHARE. Pulmonology 30, 445–451 (2022).
Charatcharoenwitthaya, P., Karaketklang, K. & Aekplakorn, W. Muscle strength, but not body mass index, is associated with mortality in patients with non-alcoholic fatty liver disease. J. Cachexia Sarcopenia Muscle 13, 2393–2404 (2022).
Ho, F. K. W. et al. The association of grip strength with health outcomes does not differ if grip strength is used in absolute or relative terms: a prospective cohort study. Age Ageing 48, 684–691 (2019).
Inker, L. A. & Titan, S. Measurement and estimation of GFR for use in clinical practice: Core Curriculum 2021. Am. J. Kidney Dis. 78, 736–749 (2021).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150, 604–612 (2009).
Delgado, C., Powe, N. R., Chertow, G. M., Grimes, B. & Johansen, K. L. Muscle mass and serum creatinine concentration by race and ethnicity among hemodialysis patients. J. Am. Soc. Nephrol. 35, 66–73 (2024).
Peng, T. C. Role of Sarcopenia in nonalcoholic fatty liver disease: definition is crucially important. Hepatology 68, 788–789 (2018).
Cho, J., Johnson, B. D., Watt, K. D. & Kim, C. H. Greater muscular strength is associated with a lower risk of pulmonary dysfunction in individuals with non-alcoholic fatty liver disease. J. Clin. Med. 11 (2022).
Avin, K. G. & Moorthi, R. N. Bone is not alone: the effects of skeletal muscle dysfunction in chronic kidney disease. Curr. Osteoporos. Rep. 13, 173–179 (2015).
He, P. et al. Association of handgrip strength and/or walking pace with incident chronic kidney disease: A UK biobank observational study. J. Cachexia Sarcopenia Muscle 14, 805–814 (2023).
Wang, X. H., Mitch, W. E. & Price, S. R. Pathophysiological mechanisms leading to muscle loss in chronic kidney disease. Nat. Rev. Nephrol. 18, 138–152 (2022).
Hara, A. et al. Relationship between handgrip strength and albuminuria in community-dwelling elderly Japanese subjects: the Shika Study. Biomarkers 25, 587–593 (2020).
Ye, C. et al. Causal associations of sarcopenia-related traits with cardiometabolic disease and Alzheimer’s disease and the mediating role of insulin resistance: a Mendelian randomization study. Aging Cell 22, e13923 (2023).
DeFronzo, R. A. & Tripathy, D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diab. Care 32, S157–S163 (2009).
Zhou, J. et al. Metabolic dysfunction-associated fatty liver disease increases risk of chronic kidney disease: a systematic review and meta-analysis. eGastroenterology 1, e100005 (2023).
Musso, G. et al. Association of non-alcoholic fatty liver disease with chronic kidney disease: a systematic review and meta-analysis. PLoS Med. 11, e1001680 (2014).
Distefano, G. & Goodpaster, B. H. Effects of exercise and aging on skeletal muscle. Cold Spring Harb. Perspect. Med. 8 (2018).
Berzigotti, A., Saran, U. & Dufour, J. F. Physical activity and liver diseases. Hepatology 63, 1026–1040 (2016).
Henry, A. et al. Vigorous physical activity provides protection against all-cause deaths among adults patients with nonalcoholic fatty liver disease (NAFLD). Aliment Pharm. Ther. 57, 709–722 (2023).
Noor, H., Reid, J. & Slee, A. Resistance exercise and nutritional interventions for augmenting sarcopenia outcomes in chronic kidney disease: a narrative review. J. Cachexia Sarcopenia Muscle 12, 1621–1640 (2021).
Heiwe, S. & Jacobson, S. H. Exercise training in adults with CKD: a systematic review and meta-analysis. Am. J. Kidney Dis. 64, 383–393 (2014).
Zhang, X. L., Wang, T. Y., Targher, G., Byrne, C. D. & Zheng, M. H. Lifestyle interventions for non-obese patients both with, and at risk, of non-alcoholic fatty liver disease. Diab. Metab. J. 46, 391–401 (2022).
Li, T., Hu, Z., Qiao, L., Wu, Y. & Ye, T. Chronic kidney disease and cognitive performance: NHANES 2011-2014. BMC Geriatr. 24, 351 (2024).
Cusick, M. M., Tisdale, R. L., Chertow, G. M., Owens, D. K. & Goldhaber-Fiebert, J. D. Population-wide screening for chronic kidney disease: a cost-effectiveness analysis. Ann. Intern. Med. 176, 788–797 (2023).
Fyfe, J. J., Hamilton, D. L. & Daly, R. M. Minimal-dose resistance training for improving muscle mass, strength, and function: a narrative review of current evidence and practical considerations. Sports Med. 52, 463–479 (2022).
Acknowledgements
This paper was funded by grants from the National Key R&D Program of China (2023YFA1800801), Noncommunicable Chronic Diseases-National Science and Technology Major Project (2023ZD0508700), National Natural Science Foundation of China (82070588, 82370577, 82000690), High Level Creative Talents from Department of Public Health in Zhejiang Province (S2032102600032) and China Postdoctoral Science Foundation (2023M732681). Dan-Qin Sun is supported in part by grants from Top Talent Support Program for young (BJ2023023), and scientific technological innovation and venture capital fund in Wuxi (Y20232011). GT is supported in part by grants from the School of Medicine, University of Verona, Verona, Italy. CDB is supported in part by the Southampton National Institute for Health and Care Research (NIHR) Biomedical Research Centre (NIHR203319), UK.
Author information
Authors and Affiliations
Contributions
Study concept and design: Xin-Lei Zhang, Yeqing Gu, Dan-Qin Sun, Kaijun Niu and Ming-Hua Zheng Acquisition of data: Xin-Lei Zhang, Yeqing Gu, Jing Zhao, Pei-Wu Zhu, Wen-Ying Chen, Gang Li, Wen-Yue Liu, Wen Zheng, Ni Zhang, Li-Li Chen Drafting of the manuscript: Xin-Lei Zhang, Yeqing Gu, Dan-Qin Sun, Kaijun Niu and Ming-Hua Zheng Critical revision and writing: Giovanni Targher and Christopher D. Byrne Statistical analysis: Xin-Lei Zhang and Yeqing Gu Study supervision: Dan-Qin Sun, Kaijun Niu and Ming-Hua Zheng All authors contributed to the manuscript for important intellectual content and approved the submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Medicine thanks Limy Wong and the other, anonymous, review(s) for their contribution to the peer review of this work. [Peer review reports are available].
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, XL., Gu, Y., Zhao, J. et al. Associations between skeletal muscle strength and chronic kidney disease in patients with MASLD. Commun Med 5, 118 (2025). https://doi.org/10.1038/s43856-025-00821-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s43856-025-00821-x
This article is cited by
-
Association of triglyceride-glucose related indices with cardiovascular diseases in individuals with low handgrip strength: a prospective cohort study of UK biobank
BMC Cardiovascular Disorders (2026)
-
Metabolic Dysfunction-Associated Steatotic Liver Disease and Chronic Kidney Disease: Unraveling Connections and Advancing Therapies
Bratislava Medical Journal (2025)