Abstract
Background
Degenerative cervical myelopathy (DCM) represents a prevalent etiology of neurological dysfunction, for which cervical decompression surgery (CDS) constitutes the principal therapeutic intervention. Advanced magnetic resonance imaging (MRI) techniques are crucial in elucidating the cerebral alterations associated with neuroinjury resulting from DCM.
Methods
In this prospective cohort study, we conducted an analysis of data from 54 patients with DCM both before and after surgery, as well as 57 healthy controls (HC), using functional MRI in combination with high-resolution structural MRI. The primary metrics included the z score transformation amplitude of low-frequency fluctuations (zALFF), functional connectivity (FC), and gray matter volume (GMV). Neurological function was evaluated through standardized clinical scores. Statistical analyses were employed to compare preoperative and postoperative changes, as well as to examine correlations with patient recovery outcome.
Results
Here we show that DCM patients exhibit significant preoperative alterations in zALFF, FC, and GMV within critical brain regions associated with sensory processing, motor control, and cognitive integration. Postoperatively, an increase in zALFF within Postcentral_R region, along with increased FC with motor-related areas, which correlates positively with neurological recovery. Moreover, GMV shows a widespread reduction before and after surgery.
Conclusions
Our study reveals functional alterations within the brain are closely associated with effective surgical recovery, especially concerning the remodeling of the ascending and descending pathways along the brain–spinal cord axis. Moreover, macrostructural changes manifest more gradually, with the recovery of brain function depending more on compensation and remodeling within neural networks than solely on structural restoration.
Plain language summary
The spinal cord directly connects to the brain, and compression of the part of the spinal cord located within the neck can cause widespread brain changes. Surgery can alleviate this compression, but its impacts on brain function are not well understood. This study employed advanced imaging techniques to examine brain functional and structural changes pre- and post-surgery in people with a disease called Degenerative cervical myelopathy (DCM), which compresses the spine. Results indicated that brain regions associated with movement and how our bodies receive and interpret information about the body’s surroundings exhibited functional improvements shortly after surgery, whereas structural changes were slower and less noticeable. These findings suggest that brain function can improve even without significant structural changes. This study enhances understanding of brain adaptation following spinal surgery and may guide better rehabilitation strategies for DCM patients.
Similar content being viewed by others
Introduction
Degenerative cervical myelopathy (DCM) is a chronic degenerative disorder characterized by spinal cord compression and is the predominant cause of spinal cord injury among individuals over 50 years of age1. With advancing age, cervical anatomical structures undergo progressive degeneration, manifesting as intervertebral disc herniation, spinal canal stenosis, and osteophyte formation, which collectively contribute to myelopathy. This compression triggers a cascade of pathological events, including Wallerian degeneration of nerve axons2, demyelination3, and subsequent neuronal dysfunction4, manifesting clinically as gait disturbances, limb coordination difficulties, and sensory abnormalities, which substantially affect patients’ quality of life5. Recent research has highlighted that DCM is linked to modifications in the sensory and motor cortices, frequently ascribed to damage in the cervical neurons that extend projections to these cerebral regions6. Furthermore, cortical neural plasticity may serve a compensatory role, potentially mitigating functional deficits by modifying synaptic connections or developing new neural circuits7.
While neural plasticity has been proposed as a compensatory mechanism to maintain function in DCM patients, alterations in and remodeling of the brain following cervical decompression surgery (CDS) have not been extensively investigated. A review of the literature reveals both consensus and contradictions concerning the effects of CDS on the brain. Several studies have concentrated on postoperative neurological recovery, emphasizing sensory and motor improvements at the clinical level, often overlooking the potential role of brain remodeling in this process8,9. These studies predominantly attribute recovery to direct spinal cord decompression, without considering remote brain changes in response to spinal cord injury. However, emerging research highlights the intricate interactions between the brain and spinal cord, suggesting that cervical neuronal damage can induce changes in brain function via ascending and descending pathways along the brain–spinal cord axis10. In this context, DCM not only impacts spinal cord integrity but may also trigger upstream brain remodeling through neuronal damage and subsequent neural plasticity. The brain’s protective mechanisms, therefore, may aid functional preservation in DCM patients, although the precise contributions of these mechanisms to long-term recovery remain unclear.
Recent studies have begun to explore the structural and functional brain changes in DCM patient, revealing reductions in functional connectivity (FC) within motor and sensory regions11, as well as decrease in gray matter volume (GMV) in areas such as the posterior cingulate cortex and the sensorimotor cortex12. However, there is a paucity of research examining the intricate interactions between brain function and structure throughout the progression of the disease and during recovery, particularly following CDS. In addition, previous research often relied on small sample sizes (typically fewer than 50 participants)12,13 and focused on a single imaging modalities11,14, limiting the ability to understand the broader patterns of brain remodeling. Thus, comprehensive multimodal analysis of brain function and structure, both before and after CDS, are limited in the current literature. This gap underscores the necessity for studies that offers a holistic understanding of brain remodeling in response to DCM and surgery intervention.
This study aims to comprehensively investigate the remodeling of brain function and macrostructural changes (large-scale alterations in brain anatomy, such as in GMV and the overall volume of specific brain regions) in patients with DCM subsequent to CDS. Utilizing resting-state functional magnetic resonance imaging (rs-fMRI) and high-resolution T1-weighted structural MRI, we assess brain remodeling across all participants. We identify differences between patients with DCM and healthy controls (HC) both before and after surgery, as well as intra-group changes in DCM patients across time points. Neurological function is evaluated using the modified Japanese Orthopaedic Association (mJOA) score, which enables us to examine the association between brain remodeling and clinical recovery. Specifically, we find that DCM patients exhibit reduced functional activity in brain regions associated with sensory processing, motor control, and cognitive integration before surgery. After decompression, functional activity in these regions increases and positively correlates with neurological improvement. In contrast, reductions in GMV persist postoperatively. These findings suggest that functional brain reorganization precedes structural recovery and may serve a compensatory role in postoperative improvement.
Methods
Patient population
Between 2022 and 2024, 100 patients with DCM prospectively participated in an observational cohort study that involved MRI imaging and clinical assessments. Neurological function was evaluated using the mJOA score, where lower scores indicate greater neurological impairment. In addition, we recruited 60 HC, matched for age, sex, and education, from the patients’ relatives and friends. These controls had no neurological, psychiatric, or other illnesses and underwent baseline MRI assessments. All MRI and clinical evaluations were conducted by two experienced spinal surgeons, as illustrated in Fig. 1. Ultimately, the study included 54 DCM patients and 57 HC. Specifically, DCM patients received cervical and brain MRIs, as well as neurological assessments preoperatively and three months postoperatively, whereas HC underwent baseline MRI evaluations. Detailed inclusion and exclusion criteria are available in the Supplementary Methods.
This study is compliant with the “Guidance of the Ministry of Science and Technology (MOST) for the Review and Approval of Human Genetic Resources” and the approval of the Research Ethics Committee of the First Affiliated Hospital of Anhui Medical University (Approval No: PJ2022-01-12). All participants, including DCM patients and HC, provided written consent in line with the ethical principles of the Declaration of Helsinki by the World Medical Association15. We affirm that no human genetic materials or data were exported from China in the course of this study. All original brain MRI and phenotypic data were comprehensively collected, processed, and stored within the borders of China. Participant data has undergone de-identification, and rigorous anonymization protocols have been instituted to prevent any potential traceability to individual subjects. The storage of data adheres to the General Data Protection Regulation (GDPR) as well as the institution’s pertinent data protection policies, and is stored in an encrypted electronic database accessible only to members of the research team.
Power analysis
To assess the adequacy of the current sample size in providing sufficient statistical power, a power analysis was conducted utilizing G*Power 3.1 (https://www.gpower.hhu.de). Under standard statistical parameters (two-tailed test, α = 0.05, power = 0.8) and a medium effect size (Cohen’s d = 0.5), the analysis demonstrated that the study possessed adequate statistical power (power > 0.8) (see Supplementary Fig. S1).
Cervical radiographical imaging
Among the cohort of 54 patients, 25 demonstrated elevated T2-weighted signal intensity within the spinal cord parenchyma, while none exhibited evident spinal cord atrophy. The distribution of compression sites was as follows: 1 case at the C3-4 segment, 9 cases at the C4-5 segment, 18 cases at the C5-6 segment, 4 cases at the C6-7 segment, and 22 cases with compression across multiple segments (≥2). Based on the preoperative mJOA scores16, 6 patients were categorized as having mild impairment, 42 as moderate, and 6 as severe.
Operative treatment
Surgical intervention was conducted within a timeframe of 3 to 6 months subsequent to the onset of symptoms. All surgical procedures were performed by an experienced spine surgeon (F.L.D.). Among the patients, 41 underwent anterior cervical discectomy and fusion (ACDF), 8 received anterior cervical corpectomy and fusion (ACCF), 3 had a combined ACDF and ACCF procedure, and 2 underwent posterior open-door decompression of the cervical vertebral canal.
Brain image acquisition
To evaluate changes in brain function and GMV in our patients, we employed a 3.0 T MRI scanner (Discovery MR750w, General Electric, Milwaukee, WI, USA) equipped with a 24-channel head coil. All participants wore earplugs to mitigate scanner noise and had foam padding to stabilize their heads and reduce movement. They were instructed to keep their eyes closed while remaining awake and relaxed during the scanning process. The detailed acquisition parameters for the blood-oxygenation-level-dependent (BOLD) fMRI data and high-resolution three-dimensional T1-weighted structural images can be found in the Supplementary Methods.
Functional MRI data preprocessing and analysis
All fMRI image preprocessing was conducted using the MATLAB 2022a platform (Mathworks, Sherborn, MA, USA) along with the RESTplus Toolbox (http://www.restfmri.net/forum), which implements functions from the Statistical Parametric Mapping (SPM12, http://www.fil.ion.ucl.ac.uk/spm/software/spm12/) toolbox.
The data preprocessing steps are as follows: (1) The first 10 time points of the time series were removed to reduce the impact of magnetic field instability during the initial scanning period; (2) Slice timing correction was applied to the functional images to correct for temporal offsets between different slices; (3) Motion correction was performed to exclude subjects with head movement parameters exceeding 3 mm or 3° in the X, Y, or Z axis; (4) Images were registered to MNI standard space using DARTEL registration techniques17. Resampled to 3 × 3 × 3 mm; (5) Smoothing was applied using a Gaussian kernel with full-width half-maximum (FWHM) = 6 mm; (6) Confounding covariates (including head motion parameters, white matter signals, and cerebrospinal fluid signals) were removed from the regression calculations, and linear drift was also removed.
Calculation of ALFF
The ALFF was calculated using preprocessed data via the RESTplus toolbox. The Fast Fourier Transform was applied to analyze the voxel time series, computing the square root of the power spectrum of BOLD signals within the 0.01–0.08 Hz frequency range to derive the ALFF values. These values were subsequently transformed into z-scores, resulting in zALFF, which were utilized for further group-level analysis.
Seed-based FC calculation
Seed-to-voxel correlation was employed to calculate the FC values between seed regions and the whole brain. FC maps were generated by assessing the linear correlations between seed regions and other brain voxels, with Fisher’s z transformation applied to obtain zFC maps for further group-level analysis. Seeds were selected from zALFF clusters that demonstrated significant intergroup or intragroup differences, and the relevant computations were performed using the RESTplus toolbox for subsequent clinical analyses.
Additional details regarding the analysis can be found in the Supplementary Methods.
Calculation of voxel-based morphometry (VBM)
VBM was performed using the Computational Anatomy Toolbox (CAT12, http://dbm.neuro.uni-jena.de/cat/)18. Preoperative and postoperative T1-weighted scan data were preprocessed through CAT12’s longitudinal preprocessing pipeline. This tool is integrated within SPM12 and employs a projected thickness approach to automatically measure cortical thickness (CT) and the central surface of the cerebral hemispheres. Previous studies have demonstrated that CAT12 reliably and accurately estimates the GMV and CT19. The detailed preprocessing steps are outlined in the Supplementary Methods.
Statistics and reproducibility
Statistical analyses were conducted using GraphPad Prism 9.5 software (https://www.graphpad.com/). The Kolmogorov-Smirnov test was employed to assess the normality of the data. For normally distributed variables, a two-sample t-test was used, whereas nonnormally distributed variables were analyzed using the Mann–Whitney test. Following image preprocessing, a general linear model (GLM) was implemented to examine the changes in brain function and structure after CDS. A two-sample t-test assessed differences between DCM patients and HC, while a paired t-test evaluated pre- and post-operation differences within DCM patients. Age, sex, and education level were included as covariates in the analysis. The voxel-level p-value was set to p ≤ 0.001 and corrected at the cluster level with p < 0.05 using family-wise error (FWE) correction. Meanwhile, the false discovery rate (FDR) correction was applied to adjust the resulting P-values for multiple comparison correction (Q < 0.05). A two-tailed p-value < 0.05 was considered statistically significant.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Demographic data and clinical scale scores
This Study includes 54 patients with DCM (29 males, 25 females) and 57 HC (29 males, 28 females). Detailed demographic characteristics of both groups are presented in Table 1. There are no significant differences between the groups in demographic variables such as age, sex, education level, height, weight, and body mass index (BMI). The preoperative mean mJOA score in DCM patients is 12.96 ± 1.55, which significantly improves to 15.93 ± 1.18 postoperatively (p = 0.001, Table 1 and Fig. 2a). Cervical MRI conducted three months postoperatively confirms satisfactory surgical decompression for all patients, as evidenced by the reconstruction of cerebrospinal fluid around the spinal cord and the absence of residual bone or soft tissue in contact with the spinal cord (Fig. 2b, c).
a A statistically significant difference in neurological improvement was observed in patients with DCM following surgical intervention (p = 0.001). b Preoperative T2 sagittal MRI demonstrated spinal cord compression and signal change in a 51-year-old DCM patient with an mJOA score of 13. c Postoperative T2 sagittal MRI revealed spinal cord decompression and resolution of the signal change abnormality after C4–6 anterior cervical discectomy and fusion. His mJOA score improved to 18 after surgery. DCM degenerative cervical myelopathy, mJOA modified Japanese Orthopaedic Association, MRI magnetic resonance imaging.
zALFF differences among HC, preoperative patients, and postoperative patients
To assess changes in brain functional activity, we compare zALFF values between HC and DCM patients both pre- and postoperatively. Preoperative DCM patients exhibit significantly lower zALFF values in sensory and visual processing areas, including Occipital_Mid_L (MOG.L), Calcarine_R (CAL.R), Lingual_L/R (LING.L/R), and Temporal_Sup_L/R (STG.L/R) (p = 0.0001) (Fig. 3a and Table 2). In contrast, higher zALFF values are observed in regions like Supramarginal_R (SMG.R), Precuneus_R (PCUN.R), and Angular_R (ANG.R) compared to HC (p = 0.0001) (Fig. 3a and Table 2). Three months postoperatively, the zALFF values in MOG.L remains lower than HC (p = 0.0001), while SMG.R, PCUN.R, ANG.R, Parietal_Inf_R (IPL.R), and Supp_Motor_Area_L (SMA.L) show significantly higher zALFF values (p = 0.0001) (Fig. 3b and Table 2). Notably, Postcentral_R (PoCG.R) demonstrates a significant increase in zALFF values compared to preoperative levels (p = 0.0001) (Fig. 3c and Table 2).
a Comparison of zALFF values between HC and preoperative patients. b Comparison of zALFF values between HC and postoperative patients. c Comparison of zALFF values between preoperative and postoperative patients. The voxel-level P value was set to p ≤ 0.001 and was corrected at the cluster-level at p < 0.05 via FWE correction. The color bar indicates the contributions of different brain regions. zALFF z score transformation amplitude of low-frequency fluctuations, HC healthy controls, FWE family-wise error.
Seed-based FC differences among HC, preoperative patients, and postoperative patients
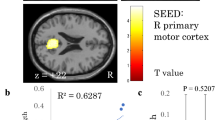
Seed-based voxel-wise FC analysis is performed using brain regions identified from the zALFF analysis. Preoperatively, patients show reduced FC with sensorimotor areas (e.g., Precentral_L/R (PreCG.L/R), PoCG.L/R, and SMA.L/R) when using STG.L as a seed, and reduced FC with regions such as Putamen_R (PUT.R), Insula_R (INS.R), Frontal_Inf_Tri_L/R (FGtriang.L/R), and Frontal_Inf_Orb_L/R (ORBinf.L/R) when using STG.R as a seed (Fig. 4a, Table 3). Using PCUN.R as a seed, FC with PoCG.R also shows a decrease (Fig. 4a and Table 3). Three months after surgery, no marked return to HC levels was observed in many brain regions. For example, using MOG.L as a seed, FC with Frontal_Mid_R (MFG.R) remains reduced. In addition, FC with ANG.L, Temporal_Mid_L (MTG.L), ORBinf.L, and PreCG.L remains weaker when SMG.R was used as a seed; using PCUN.R as a seed, the FC with Frontal_Inf_Oper_R (FGoperc.R), Cingulum_Mid_L/R (DCG.L/R), and Cingulum_Ant_L (ACG.L) remains lower (Fig. 4b and Table 3). Notably, compared with preoperative levels, FC with PreCG.L/R, PoCG.L, SMA.L, and Thalamus_L (THA.L) significantly increases postoperatively when using PCUN.R as a seed (Fig. 4c and Table 3).
a Comparison of zFC values between preoperative patients and HC. b Comparison of zFC values between postoperative patients and HC. c Comparison of zFC values between preoperative and postoperative patients. Each edge and connection in the chord diagram represents FC between distinct brain regions, establishing a one-to-one correspondence with the connections depicted in the brain region stick diagram. The different colored connections are used solely to distinguish FC between different brain regions and do not represent any specific significance. The voxel-level P value was set to p ≤ 0.001 and was corrected at cluster-level p < 0.05 via FWE correction. HC healthy controls, zFC z score transformation Functional connectivity, STG superior temporal gyrus, PoCG postcentral gyrus; PreCG precentral gyrus, SMA supplementary motor area, PUT lenticular nucleus, putamen, IFGtriang inferior frontal gyrus, triangular part, ORBinf inferior frontal gyrus, orbital part, PCUN precuneus, INS insula, MOG middle occipital gyrus, MFG middle frontal gyrus, SMG supramarginal gyrus, ANG angular gyrus, DCG median cingulate and paracingulate gyri, ACG anterior cingulate and paracingulate gyri, THA thalamus, FWE family-wise error.
GMV differences among HC, preoperative patients, and postoperative patients
We use VBM to compare GMV changes across groups. Preoperatively, DCM patients show significant GMV reductions in regions involved in sensory, motor, cognitive, visual, and emotional functions, including PreCG.R, PoCG.L/R, MTG.L/R, INS.L/R, ORBinf.L/R, MOG.L, PCUN.L/R, ANG.L/R, and Hippocampus_L/R (HIP.L/R) (Fig. 5a). Postoperatively, significant GMV reductions persist in these areas, including PreCG.R, PoCG.L/R, MTG.L/R, ORBinf.L/R, ACG, MOG.L, ANG.L/R, and PCUN.L/R, all remaining lower than HC level (Fig. 5b). In addition, THA.L/R show further GMV reduction compared to preoperative levels (Fig. 5c).
a Comparison of GMV between preoperative patients and HC. b Comparison of GMV between postoperative patients and HC. c Comparison of GMV between preoperative and postoperative patients. The left panel of the Fig highlights the brain regions that show significant differences in GMV among the HC, preoperative, and postoperative groups. The brain mapping presents the functional distribution of these regions, with font size reflecting the number of brain regions associated with each specific function. The color bar indicates the contribution of different brain regions. HC healthy controls, GMV gray matter volume.
Correlations between neuroimaging metrics among DCM patients and their association with functional scores
We conduct correlation analyses between neuroimaging metrics and mJOA score to examine the relationship between brain changes and functional recovery. A positive correlation is found between mJOA scores and zALFF values for PoCG.R (Fig. 6a). The strength of FC between PoCG.R and PoCG.L, PreCG.R, and SMA.R is positively correlated with mJOA scores (Fig. 6b–d). However, no significant correlation is observed between FC strength of PoCG.R with PreCG.L or THA.L and mJOA scores (Supplementary Fig. S2a, b). Similarly, GMV in THA.L/R does not significantly correlate with mJOA scores (Supplementary Fig. S2c).
a The study revealed that the mJOA scores of DCM patients were positively correlated with the zALFF values in the PoCG.R. The 95% confidence interval ranges from 0.4668 to 0.7837. b–d The FC strength between the PoCG.R and several regions including PoCG.L, PreCG.R, and SMA.R was positively correlated with mJOA scores. The 95% confidence intervals for (b–d) are as follows: 0.02567 to 0.5187, 0.007765 to 0.5055, and 0.09874 to 0.5703. All P-values were corrected for multiple comparisons using the FDR method. The mJOA scores, zALFF and FC values represent the postoperative scores minus the preoperative scores. DCM degenerative cervical myelopathy, mJOA modified Japanese Orthopaedic Association, zALFF z score transformation amplitude of low-frequency fluctuations, FC functional connectivity, PoCG postcentral gyrus, PreCG precentral gyrus, SMA supplementary motor area, FDR, false discovery rate.
In addition, we further examine the relationships between functional and structural alterations in abnormal brain regions of patients with DCM before and after surgery. The FC strength between PoCG.R and both the PoCG.L and the PreCG.R is positively correlated with zALFF value of PoCG.R (Fig. 7b, c), while FC strength between PoCG.R and the THA.L is negatively correlated with zALFF value of PoCG.R (Fig. 7d). No significant correlations are detected between FC strength of PoCG.R and PreCG.L or SMA.R and zALFF values of PoCG.R (Supplementary Fig. S3b,c), nor do we observe any correlations among zALFF, FC, and GMV (Supplementary Fig. S3d–i).
a We assessed two functional indicators, zALFF and FC, alongside the structural indicator of GMV. b, c The FC strength between PoCG.R and both PoCG.L and PreCG.R was positively correlated with the zALFF value of PoCG.R. The 95% confidence intervals for (b, c) are as follows: 0.01797 to 0.5131 and 0.1032 to 0.5733. d The FC strength between PoCG.R and THA.L was negatively correlated with zALFF value of PoCG.R. The 95% confidence interval ranges from −0.5300 to −0.04120. All P-values were corrected for multiple comparisons using the FDR method. The zALFF and FC values represent the postoperative scores minus the preoperative scores. DCM degenerative cervical myelopathy, zALFF z-score transformation amplitude of low-frequency fluctuations, FC functional connectivity, PoCG postcentral gyrus, PreCG precentral gyrus, THA thalamus, FDR false discovery rate.
Discussion
In recent years, extensive research has been conducted on upstream morphological abnormalities resulting from spinal cord injury (SCI)7 and alterations in sensorimotor regions of the brain20,21. Consistent with previous studies, our investigation has characterized the functional and structural changes in the brains of patients with DCM both before and after surgery. Our findings corroborate that these patients experience substantial functional and structural remodeling, thereby supporting the hypothesis that CDS can reorganize brain activity. Following CDS, patients with DCM exhibited marked improvements in neurological function, suggesting that downstream morphological recovery may influence upstream pathways.
Prior to surgery, brain changes in DCM patients primarily involve cortical and subcortical regions related to ascending and descending pathways of the spinal cord. Compression of the spinal cord can induce localized ischemia and inflammation within nerve fibers, resulting in neuronal and glial cell damage22, which impairs signal transmission efficiency, ultimately disrupting sensory and motor transmission23. This damage is reflected in reduced zALFF values is key sensorimotor areas such as the CAL.R and STG.L/R, and diminished FC between the STG.L and motor areas like PreCG.L/R and PoCG.L/R. These findings corroborate prior work showing that SCI-induced disruptions in the corticospinal tract (CST) and dorsal column-medial lemniscus (DCML) pathway impact sensorimotor integration. The CST serves as a crucial pathway for the transmission of motor commands between the brain and the spinal cord24, and injury to the spinal cord can have a direct impact on CST transmission25. Persistent obstruction may induce neuroplastic changes within the motor areas of the brain, thereby diminishing input to the cortical motor regions26, and resulting in decreased activity in downstream motor and sensory regions. This phenomenon is consistent with clinical observations of motor dysfunction in patients with DCM, including gait disturbances and compromised fine motor skills. Concurrently, SCI may also modify the sensory feedback mechanism by impacting the DCML pathway. The DCML system is essential for conveying fine touch, proprioception, kinesthetic senses, and pressure information27. Impairment of this pathway disrupts the transmission of ascending sensory information, which not only affects cortical sensory processing but also may result in the degeneration of the sensory feedback system.
The reduced FC in motor regions, along with the overall decrease in GMV, suggests that DCM not only impairs spinal conduction but also induces widespread brain network dysfunction. Akin to the process of “secondary demyelination,” prolonged transmission disruptions may decrease the metabolic demand and neuronal activity within certain brain regions, ultimately precipitating plastic changes and a gradual reduction in brain volume28,29,30. To compensate for brain function changes caused by SCI, previous research has demonstrated that the visual cortex frequently exhibits increased ALFF and FC values31. Our study, however, revealed markedly reduced zALFF values in regions associated with the visual cortex, such as MOG.L and LING.L/R. One plausible explanation for this discrepancy lies in study design, patient populations, and disease stage. Unlike studies focusing on traumatic SCI or chronic states, our cohort consisted of patients with progressive degenerative cervical myelopathy, which may produce different patterns of cortical adaptation. Earlier studies reviewed evidence of plasticity and stability of the primary visual cortex in adults, confirming that functional abnormalities of the visual cortex are linked to a decline in perceptual function32. Thus, we guess the decline in visual function may be due to diminished efficiency in the transmission of ascending signals as a result of spinal cord encroachment, where persistent signal interruption leads to functional degradation and decreased neuronal activity in perceptual-related brain regions, ultimately affecting the processing and integration of visual information33. However, since our study did not include visual performance tests or neurophysiological measures, this interpretation remains hypothetical. Future research should incorporate such data to validate whether these imaging changes correspond to functional visual deficits in DCM patients.
Interestingly, despite considerable functional deficits in motor and sensory processing, our study observed increased zALFF values in certain such as the PCUN.R, SMG.R, and ANG.R. We hypothesize that this phenomenon may represent compensatory mechanisms in response to diminished input from the spine cord. The PCUN is a central component of the default mode network (DMN), primarily associated with self-awareness, attention regulation, and cognitive functions34. Empirical evidence indicates that the functional activity of the PCUN is intricately connected to variations in somatosensory input. In instances of sensory loss or motor dysfunction, increased activity within the PCUN facilitates optimized connectivity with other brain regions, thereby compensating for functional deficits. For example, in patients with SCI, heightened activity in the PCUN and other DMN regions serves to mitigate sensory and motor dysfunction35. Conversely, the ANG is strongly linked to action-feedback monitoring and locomotion36. When SCI restricts sensory input and motor control, the ANG may compensate for these deficits by enhancing its functional activity. The enhanced activity in these regions likely reflects neuroplastic changes where brain areas attempt to take over the functions of damaged network to offset deficits in impaired areas, a phenomenon widely reported in patients with spinal cord or brain injuries37,38. However, future studies should incorporate more objective neuropsychological evaluations, such as attention tasks and the Montreal Cognitive Assessment (MoCA), to further substantiate the potential compensatory mechanisms underlying postoperative functional improvements in cognitive regions like the PCUN and ANG.
Following surgical intervention, the alleviation of spinal cord encroachment facilitates the gradual recovery of brain–spinal cord pathways. CDS is thought to mitigate further damage to the spinal cord in the form of demyelination, axonal injury, or ischemia39. Studies have demonstrated that within ~5.5 days post-decompression, the pressure induced by dural factors markedly reduces, aiding the reestablishment of signal transmission between the brain and spinal cord40. The recovery process, however, is complex and involves remodeling across various regions of both the brain and spinal cord, especially those involved in sensory and motor integration41,42. Our findings highlight key functional changes observed three months following surgery, including a notable increase in zALFF values in the PoCG.R, which suggests recovery in primary sensory cortex. This was accompanied by enhanced FC between PoCG.R and other regions, including PreCG.L/R, PoCG.L, SMA.L, and THA.L, which are involved in motor planning and sensory feedback integration43,44,45. The zALFF of PoCG.R and the FC strength between PoCG.R and PoCG.L, as well as PreCG.R and SMA.R, was positively correlated with mJOA scores. These findings suggest that CDS facilitates the restoration of connectivity between sensory and motor networks, thereby enhancing coordination between sensory input and motor output. This process involves neural remodeling, facilitating the reestablishment of FC in pathways such as CST and DCML. The CST, the principal descending motor pathway, plays a critical role in transmitting motor commands from the cerebral cortex to the spinal cord46,47. Following the release of spinal compression, the functionality of the CST can be augmented through mechanisms such as synaptic plasticity, axonal regeneration, and functional compensation within local neural networks4. Similarly, the DCML pathway, responsible for transmitting fine touch and proprioceptive information27, also benefits from CDS, with improved spinal conduction velocity and sensory data processing. These changes contribute to enhanced sensory experience and better integration of sensory feedback with motor planning, which is essential for motor recovery.
Moreover, the reestablishment of neural pathways between the spinal cord and the cerebral cortex has the potential to further augment motor coordination by enhancing perceptual accuracy and providing real-time feedback for motor planning48. At the cortical level, our findings suggest that the restoration of the cortico-spinal-cortical loop underpins postoperative recovery. Enhancing the interactions between the PoCG and PreCG regions is likely crucial for postoperative motor recovery. This feedback loop facilitates the brain’s ability to adjust motor actions in response to real-time sensory input, thereby optimizing motor control during recovery49. In addition, The THA, as a relay station for sensory information45, exhibited strengthened connectivity with the motor cortex, further indicating a partial restoration of sensory information transmission functions. Despite these improvements, certain regions, such as the visual cortex (e.g., MOG.L), showed reduced zALFF values, suggesting delayed functional recovery in the visual system. FC analysis revealed diminished connectivity between MOG.L and MFG.R compared to HC, which may indicate ongoing impairments in visual information processing and cognitive control. The complexity of the visual system, coupled with the prolonged nature of neural damage, suggests that the full recovery of visual pathways may require more time, particularly in the ascending and descending pathways that influence visual processing47,50. Interestingly, regions such as SMG.R, PCUN.R, and ANG.R exhibited increased activity following surgery, which may reflect compensatory mechanisms following chronic neural damage. PCUN and ANG are involved in multitasking integration and cognitive control51,52, and their increased activity could represent an adaptive response to the sensory and motor deficits caused by spinal cord compression. Although this compensatory activation may support functional recovery in the short term, prolonged hyperactivation could strain neural resources, potentially leading to energy depletion and further neuronal damage53,54. More research in needed to determine whether this overactivation is a temporary compensatory mechanism or a maladaptive response.
Despite improvements in brain function following CDS, patients with DCM continue to experience widespread reductions in GMV. Chronic SCI results in persistent damage to the spinal cord and related brain regions, potentially leading to extensive cortical atrophy. This condition is characterized by limited neural regeneration in the affected areas, even following decompression. The prolonged impairment of signal transmission may have induced irreversible neuronal damage, and these changes are frequently not reversible through short-term surgical interventions, thereby contributing to delayed recovery of GMV55. Meanwhile, we observed that postoperative neurological recovery in DCM patients does not progress linearly. Specifically, our study found no significant correlation between the FC of the PoCG.R and PreCG.L with the mJOA score. Although the PoCG and PreCG are primarily involved in sensory and motor regulation56,57, their FC may not directly correspond to overall motor recovery. The mJOA score assesses global motor function, whereas brain region remodeling occurs in a temporal sequence. During the early postoperative period, these brain regions may undergo excessive activation, which gradually transitions to an adaptive adjustment phase in later stages. The intensity and patterns of FC in sensory and motor control brain regions may exhibit distinct recovery trajectories at different postoperative time points. However, as this study only tracked data for three months postoperatively, longer longitudinal studies are needed to elucidate the recovery time window for these relevant brain regions.
The relationship between structural and functional alterations in the brains of patients with DCM is complex and dynamic. The classical neuroscience theory, “structure determines function,” posits that modifications in neuroanatomical structures directly affect the functional activity of corresponding brain regions58. This framework has been extensively utilized to understand brain damage and neurodegenerative diseases, highlighting the critical role of structural integrity in maintaining normal function. Prior research has demonstrated that a decrease in gray matter volume or damage to white matter fiber tracts can result in alterations in functional connectivity, consequently impacting cognitive and motor functions59,60. Our findings confirm this relationship, as evidenced by reductions in GMV across several brain regions, including MTG.L/R and PoCG.L/R, in preoperative DCM patients. These structural changes were accompanied by decreases in the zALFF and FC in areas such as the STG.L/R, indicating that structural alterations may underlie the observed functional impairments.
However, the relationship between structure and function is not unidirectional. Recent theories of neuroplasticity emphasize the bidirectional nature of this relationship. Structural changes can influence functional activity, while functional abnormalities can, in turn, result in alterations to the structure of corresponding brain regions. This reciprocal interaction is supported by the concepts of “functional plasticity” (brain function changes as compensatory mechanisms to structural damage), and “structural plasticity” (the brain’s ability to reorganize its structure in response to functional demands)61. Notably, prolonged cord compression syndrome in DCM leads to both functional disruptions within the spinal cord and brain regions involved in sensory and motor processing, potentially inducing long-lasting structural modifications. This viewpoint is well-grounded in the concept of “neural plasticity,” which posits that the brain compensates for damage by modifying neuronal activation patterns, enhancing synaptic connections among existing neurons and adjusting neuronal firing patterns when functionality is impaired62.
Our findings also suggest that functional recovery may precede structural in DCM patients, as demonstrated by the increased zALFF and FC values in specific cerebral regions, such as PoCG.R and PreCG.L/R, three months after CDS. However, the GMV in these regions persisted at levels lower than those observed in HC, indicating that structural recovery lags behind functional recovery. Following CDS, initial functional recovery likely represents an early compensatory mechanism, driven by neural plasticity, whereas structural recovery is a more gradual process. One explanation for this discrepancy is the time required for structural changes, such as neurogenesis, axonal regeneration, and glial cell recovery, which collectively contribute to structural remodeling. These processes are intrinsically slower than functional recovery, which is primarily driven by the enhancement of synaptic connectivity and neuronal activation patterns. In fact, neural plasticity enables the brain to compensate for functional deficits long before structural recovery is evident63,64. A similar pattern has been documented in studies of stroke patients, where functional recovery, especially in sensory and motor functions, has been reported despite ongoing structural deficits in the affected brain regions65. In addition, in animal models of SCI, functional compensation frequently occurs through increased cortical activity, even in the presence of minimal structural regeneration66. These observations bolster our hypothesis that functional alterations, mediated by the plastic reorganization of neural circuits, precede structural restoration. This temporal sequence may elucidate why enhancements in sensory and motor functions can be detected in the absence of concomitant changes in GMV. Interestingly, this may explain why the restoration of FC in regions such as the THA observed in our study did not fully correspond with alterations in GMV, and why no significant correlation was found between zALFF, FC, and GMV. While the aforementioned findings provide valuable insights into short-term postoperative brain remodeling, comprehensive long-term follow-up studies are necessary to systematically characterize the dynamic trajectories of functional and structural reorganization along the brain–spinal axis.
However, this study has some limitations. Firstly, variations in surgical techniques or the preoperative severity of conditions may affect postoperative recovery outcomes. To minimize the interference of these confounding variables, we instituted rigorous control measures in both patient selection and surgical procedures. However, this selection criterion may restrict the generalizability of the findings, as differences in the severity and type of spinal cord injury could uniquely influence postoperative brain changes. Future studies should encompass a more diverse cohort of patients exhibiting a spectrum of SCI severities to examine the impact of varying injury types on cerebral function and structural recuperation. Secondly, while this study provides valuable longitudinal data, the three-month follow-up may be insufficient to fully reflect the long-term recovery of brain function and structure, especially given the slow nature of GMV changes. To achieve a more comprehensive understanding of the neurorecovery trajectory in patients with DCM and to support the development of subsequent treatment strategies and rehabilitation measures, we propose extending the follow-up period (e.g., spanning 6 months, 12 months, and beyond) in future studies, with a particular focus on the long-term neuroplastic recovery of postoperative patients. Thirdly, the study did not utilize advanced imaging techniques such as diffusion tensor imaging (DTI), which constrains the direct assessment of white matter pathways, including the corticospinal tract and the dorsal column-medial lemniscus system. While the data on functional and gray matter volume indicate potential neuroplastic changes, the mechanistic understanding of modifications in white matter connectivity remains inadequate. Future research should integrate multimodal imaging approaches, such as DTI, to enhance the understanding of brain–spinal cord pathways’ contributions to postoperative recovery. Fourthly, surgical decompression may not fully restore neurological function. Future research should prioritize the promotion of neuroprotection through pharmacological or physical interventions during the early postoperative period to mitigate degenerative brain changes and assess their effects on brain function and structural recovery. Finally, the variability in MRI acquisition protocols across different institutions or imaging platforms may introduce discrepancies in cross-sectional comparisons. Variations in spatial resolution, scanning sequences, and other technical parameters could impact the consistency and reliability of measurements across patients. Standardizing MRI protocols or conducting multi-center studies with harmonized imaging techniques could help mitigate this limitation. In summary, while our study offers valuable insights into brain function recovery following DCM surgery, addressing these limitations in future research will enhance our understanding of the long-term effects of myelopathy and surgical intervention on brain health.
In conclusion, alterations in brain function are intricately associated with successful postoperative recovery, particularly within brain regions responsible for motor regulation and the integration of sensory information. Although macrostructural changes occur relatively slowly, the restoration of brain function appears to depend more substantially on the compensation and reorganization of neural networks. These findings underscore the importance of early surgical intervention and long-term rehabilitation for patients with DCM. Future research should investigate non-invasive neuromodulation technologies (such as transcranial magnetic stimulation and brain-computer interfaces) and dynamic neural changes at various stages of recovery, with the goal of identifying predictive biomarkers and optimizing personalized rehabilitation strategies. Moreover, interdisciplinary collaboration between neurosurgery, neurorehabilitation, and neuropsychology is essential for enhancing postoperative recovery and facilitating brain function remodeling.
Data availability
The source data for Figs. 2a, 3–7, and Supplementary Figs. 2 and 3 can be found in Supplementary Data 1. Clinical features analysis results are provided in Supplementary Data 1. Certain raw data cannot be publicly disclosed due to concerns regarding participant confidentiality. However, controlled access may be granted for legitimate academic purposes upon request to the corresponding author and signing a data use agreement.
References
Davies, B. M., Mowforth, O. D., Smith, E. K. & Kotter, M. R. Degenerative cervical myelopathy. BMJ 360, k186 (2018).
Bohlman, H. H. & Emery, S. E. The pathophysiology of cervical spondylosis and myelopathy. Spine 13, 843–846 (1988).
Freund, P. et al. MRI in traumatic spinal cord injury: from clinical assessment to neuroimaging biomarkers. Lancet Neurol. 18, 1123–1135 (2019).
Badhiwala, J. H. et al. Degenerative cervical myelopathy—update and future directions. Nat. Rev. Neurol. 16, 108–124 (2020).
Witiw, C. D. & Fehlings, M. G. Degenerative cervical myelopathy. CMAJ 189, E116 (2017).
Holly, L. T., Dong, Y., Albistegui-DuBois, R., Marehbian, J. & Dobkin, B. Cortical reorganization in patients with cervical spondylotic myelopathy. J. Neurosurg. Spine 6, 544–551 (2007).
Bernabéu-Sanz, Á., Mollá-Torró, J. V., López-Celada, S., Moreno López, P. & Fernández-Jover, E. MRI evidence of brain atrophy, white matter damage, and functional adaptive changes in patients with cervical spondylosis and prolonged spinal cord compression. Eur. Radio. 30, 357–369 (2020).
Bartels, R. A new dimension in degenerative cervical myelopathy. Lancet Neurol. 20, 82–83 (2021).
Badhiwala, J. H. et al. Predicting outcomes after surgical decompression for mild degenerative cervical myelopathy: moving beyond the mJOA to identify surgical candidates. Neurosurgery 86, 565–573 (2020).
De Ridder, D., Adhia, D. & Vanneste, S. The anatomy of pain and suffering in the brain and its clinical implications. Neurosci. Biobehav. Rev. 130, 125–146 (2021).
Shao, Z., Tan, Y., Zhan, Y. & He, L. Modular organization of functional brain networks in patients with degenerative cervical myelopathy. Sci. Rep. 14, 8593 (2024).
Bhagavatula, I. D. et al. Functional cortical reorganization in cases of cervical spondylotic myelopathy and changes associated with surgery. Neurosurg. Focus 40, E2 (2016).
Fouda, M. A. et al. Predictors of progression in radiation-induced versus nonradiation-induced pediatric meningiomas: a large single-institution surgical experience. J. Neurosurg. Pediatr. 28, 160–166 (2021).
Takenaka, S. et al. Resting-state amplitude of low-frequency fluctuation is a potentially useful prognostic functional biomarker in cervical myelopathy. Clin. Orthop. Relat. Res. 478, 1667–1680 (2020).
World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Participants. JAMA. 333, 71–74 (2025).
Tetreault, L. et al. The modified Japanese Orthopaedic Association scale: establishing criteria for mild, moderate and severe impairment in patients with degenerative cervical myelopathy. Eur. Spine J. 26, 78–84 (2017).
Ashburner, J. A fast diffeomorphic image registration algorithm. NeuroImage 38, 95–113 (2007).
Gaser, C. et al. I. CAT: a computational anatomy toolbox for the analysis of structural MRI data. GigaScience 13, giae049 (2024).
André, C. et al. REM sleep is associated with the volume of the cholinergic basal forebrain in aMCI individuals. Alzheimer’s. Res. Ther. 15, 151 (2023).
Holly, L. T., Wang, C., Woodworth, D. C., Salamon, N. & Ellingson, B. M. Neck disability in patients with cervical spondylosis is associated with altered brain functional connectivity. J. Clin. Neurosci. 69, 149–154 (2019).
Wang, C., Laiwalla, A., Salamon, N., Ellingson, B. M. & Holly, L. T. Compensatory brainstem functional and structural connectivity in patients with degenerative cervical myelopathy by probabilistic tractography and functional MRI. Brain Res. 1749, 147129 (2020).
Gu, G. et al. Multiple mechanisms of curcumin targeting spinal cord injury. Biomed. Pharmacother. 159, 114224 (2023).
Kigerl, K. A., de Rivero Vaccari, J. P., Dietrich, W. D., Popovich, P. G. & Keane, R. W. Pattern recognition receptors and central nervous system repair. Exp. Neurol. 258, 5–16 (2014).
Karadimas, S. K. et al. Sensory cortical control of movement. Nat. Neurosci. 23, 75–84 (2020).
Quintá, H. R., Pasquini, L. A. & Pasquini, J. M. Three-dimensional reconstruction of corticospinal tract using one-photon confocal microscopy acquisition allows detection of axonal disruption in spinal cord injury. J. Neurochem 133, 113–124 (2015).
Moreno-Lopez, Y., Bichara, C., Delbecq, G., Isope, P. & Cordero-Erausquin, M. The corticospinal tract primarily modulates sensory inputs in the mouse lumbar cord. Elife 10, e65304 (2021).
Khoo, Y. H., Abdullah, J. M., Idris, Z., Ghani, A. R. I. & Halim, S. A. Dorsal column bedside examination test: tips for the neurosurgical resident. Malays. J. Med. Sci. 30, 172–179 (2023).
Li, H. et al. Regional cortical thinning, demyelination and iron loss in cerebral small vessel disease. Brain 146, 4659–4673 (2023).
Papastefanaki, F. & Matsas, R. From demyelination to remyelination: the road toward therapies for spinal cord injury. Glia 63, 1101–1125 (2015).
Hanemann, C. O. & Gabreels-Festen, A. A. Secondary axon atrophy and neurological dysfunction in demyelinating neuropathies. Curr. Opin. Neurol. 15, 611–615 (2002).
Chen, Z. et al. Visual cortex neural activity alteration in cervical spondylotic myelopathy patients: a resting-state fMRI study. Neuroradiology 60, 921–932 (2018).
Wandell, B. A. & Smirnakis, S. M. Plasticity and stability of visual field maps in adult primary visual cortex. Nat. Rev. Neurosci. 10, 873–884 (2009).
Zhou, F. Q. et al. Intrinsic functional plasticity of the sensory-motor network in patients with cervical spondylotic myelopathy. Sci. Rep. 5, 9975 (2015).
Dadario, N. B. & Sughrue, M. E. The functional role of the precuneus. Brain 146, 3598–3607 (2023).
Cui, L. et al. Association of precuneus Aβ burden with default mode network function. Alzheimer’s. Dement. 21, e14380 (2025).
Baarbé, J. et al. Interhemispheric interactions between the right angular gyrus and the left motor cortex: a transcranial magnetic stimulation study. J. Neurophysiol. 125, 1236–1250 (2021).
Hou, J. et al. Motor recovery at 6 months after admission is related to structural and functional reorganization of the spine and brain in patients with spinal cord injury. Hum. Brain Mapp. 37, 2195–2209 (2016).
Kazim, S. F. et al. Corticospinal motor circuit plasticity after spinal cord injury: harnessing neuroplasticity to improve functional outcomes. Mol. Neurobiol. 58, 5494–5516 (2021).
Karadimas, S. K., Gatzounis, G. & Fehlings, M. G. Pathobiology of cervical spondylotic myelopathy. Eur. Spine J. 24, 132–138 (2015).
Saadoun, S., Werndle, M. C., Lopez de Heredia, L. & Papadopoulos, M. C. The dura causes spinal cord compression after spinal cord injury. Br. J. Neurosurg. 30, 582–584 (2016).
Mao, Y. R. et al. Effects of cortical intermittent theta burst stimulation combined with precise root stimulation on motor function after spinal cord injury: a case series study. Neural Regen. Res. 17, 1821–1826 (2022).
Moreno-López, Y. & Hollis, E. R. Sensory circuit remodeling and movement recovery after spinal cord injury. Front Neurosci. 15, 787690 (2021).
Chen, S. et al. Degeneration of the sensorimotor tract in degenerative cervical myelopathy and compensatory structural changes in the brain. Front Aging Neurosci. 14, 784263 (2022).
Chang, J. et al. Dysregulated neural activity between the thalamus and cerebral cortex mediates cortical reorganization in cervical spondylotic myelopathy. Brain Res. Bull. 205, 110837 (2023).
Roy, D. S., Zhang, Y., Halassa, M. M. & Feng, G. Thalamic subnetworks as units of function. Nat. Neurosci. 25, 140–153 (2022).
Wolpaw, J. R. & Tennissen, A. M. Activity-dependent spinal cord plasticity in health and disease. Annu. Rev. Neurosci. 24, 807–843 (2001).
Lemon, R. N. Descending pathways in motor control. Annu. Rev. Neurosci. 31, 195–218 (2008).
Pearson, K. G. Neural adaptation in the generation of rhythmic behavior. Annu. Rev. Physiol. 62, 723–753 (2000).
Diers, M., Christmann, C., Koeppe, C., Ruf, M. & Flor, H. Mirrored, imagined and executed movements differentially activate sensorimotor cortex in amputees with and without phantom limb pain. Pain 149, 296–304 (2010).
Quadri, S. A. et al. Recent update on basic mechanisms of spinal cord injury. Neurosurg. Rev. 43, 425–441 (2020).
Lyu, D. et al. Causal evidence for the processing of bodily self in the anterior precuneus. Neuron 111, 2502–2512.e2504 (2023).
Humphreys, G. F., Lambon Ralph, M. A. & Simons, J. S. A unifying account of angular gyrus contributions to episodic and semantic cognition. Trends Neurosci. 44, 452–463 (2021).
Tomasi, D. & Volkow, N. D. Abnormal functional connectivity in children with attention-deficit/hyperactivity disorder. Biol. Psychiatry 71, 443–450 (2012).
Mosconi, L. et al. Menopause impacts human brain structure, connectivity, energy metabolism, and amyloid-beta deposition. Sci. Rep. 11, 10867 (2021).
Liu, S. et al. Cognitive control subprocess deficits and compensatory modulation mechanisms in patients with frontal lobe injury revealed by EEG markers: a basic study to guide brain stimulation. Gen. Psychiatr. 36, e101144 (2023).
Giampiccolo, D. & Duncan, J. S. High plasticity within the precentral gyrus and its relevance for resective neurosurgery. Brain 146, e98–e99 (2023).
Jutzeler, C. R. et al. Sensorimotor plasticity after spinal cord injury: a longitudinal and translational study. Ann. Clin. Transl. Neurol. 6, 68–82 (2019).
Toga, A. W. & Thompson, P. M. Mapping brain asymmetry. Nat. Rev. Neurosci. 4, 37–48 (2003).
Kinnunen, K. M. et al. White matter damage and cognitive impairment after traumatic brain injury. Brain 134, 449–463 (2011).
Lee, E. Y. et al. Early cortical gray matter loss and cognitive correlates in non-demented Parkinson’s patients. Parkinsonism Relat. Disord. 19, 1088–1093 (2013).
Kolb, B. & Whishaw, I. Q. Brain plasticity and behavior. Annu. Rev. Psychol. 49, 43–64 (1998).
Cramer, S. C. et al. Harnessing neuroplasticity for clinical applications. Brain 134, 1591–1609 (2011).
Khan, F., Amatya, B., Galea, M. P., Gonzenbach, R. & Kesselring, J. Neurorehabilitation: applied neuroplasticity. J. Neurol. 264, 603–615 (2017).
Sampaio-Baptista, C., Sanders, Z. B. & Johansen-Berg, H. Structural plasticity in adulthood with motor learning and stroke rehabilitation. Annu. Rev. Neurosci. 41, 25–40 (2018).
Schulz, R. et al. Parietofrontal motor pathways and their association with motor function after stroke. Brain 138, 1949–1960 (2015).
Courtine, G. & Sofroniew, M. V. Spinal cord repair: advances in biology and technology. Nat. Med. 25, 898–908 (2019).
Acknowledgements
We express our gratitude to the patients and their families for contributing brain data essential to this study. We also acknowledge the financial support provided by the following funding sources: the First Affiliated Hospital of Anhui Medical University Clinical Research Project (Grant No. LCYJ2021YB018), University Natural Science Research Key Project of Anhui Province (Grant No. 2022AH051158), and Health Research Project of Anhui Province (Grant No. AHWJ2023A20125).
Author information
Authors and Affiliations
Contributions
B.Y.X.: Conceptualization, data curation, formal analysis, investigation, methodology, project administration, writing-original draft, writing-review & editing. H.Y.N.: Data curation, formal analysis, software, methodology, visualization. J.Y.Y.: Data curation, software. Z.B.X.: Data curation, methodology. S.C.B.: Data curation, software. H.X.W.: Visualization. K.Z.: Data curation. X.Y.W.: Software. P.W.S.: Supervision. Y.Y.W.: Methodology, data curation. Y.Q.Y.: Validation, supervision. F.L.D.: Conceptualization, funding acquisition, investigation, visualization, software, resources, supervision, project administration, writing-original draft, writing-review & editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Medicine thanks Arzu C. Has Silemek, Elena Filimonova and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xie, B., Ni, H., Yao, J. et al. Functional and structural brain remodeling in patients with degenerative cervical myelopathy following cervical decompression surgery. Commun Med 5, 191 (2025). https://doi.org/10.1038/s43856-025-00909-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s43856-025-00909-4