Abstract
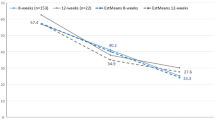
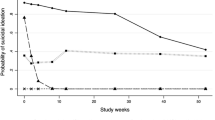
Non-invasive brain stimulation interventions for treating suicidal ideation in individuals with treatment-resistant depression offer the potential for new therapeutic options for patients with borderline personality disorder (BPD), a condition that responds poorly to antidepressant medications. Here we present a study to explore the application of magnetic seizure therapy (MST) in an open-label pilot trial of moderately to severely suicidal individuals with comorbid BPD and treatment-resistant depression conducted at the Centre for Addiction and Mental Health (Toronto, Canada). Using a non-randomized, case-control design, we investigated the feasibility and initial clinical effects of 5 weeks of conjoint MST and dialectical behaviour therapy (MST + DBT) compared with 5 weeks of DBT alone. Changes in primary symptom outcomes of suicidal ideation on the Modified Scale for Suicide Ideation and clinician-rated depression severity on the Hamilton Rating Scale for Depression – 24 were investigated using multilevel models. Additional outcomes included self-reported depression, BPD symptom severity and cognitive functioning. Out of 62 screened participants, n = 21 were enrolled, and N = 19 completed the intervention (n = 9 MST + DBT and n = 10 DBT only). The intervention was feasible to implement. Conjoint MST + DBT, but not DBT alone, led to a rapid, significant and clinically meaningful reduction in suicidal ideation at 5 weeks that was sustained at four-month follow-up. Conjoint MST + DBT was also associated with significant reductions in clinician-rated depression and BPD interpersonal symptom severity, but neither effect was sustained at four-month follow-up. There were no treatment-related effects on cognition. There were no treatment-related serious adverse events. These findings provide initial evidence to suggest that MST + DBT is a feasible intervention to reduce acute suicide risk in individuals with BPD and warrant further exploration in a sham-controlled randomized clinical trial.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$79.00 per year
only $6.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Study participants did not consent to have their data shared publicly. Deidentified participant data from all study timepoints, along with data dictionaries and the study protocol, can be made available, beginning 12 months and ending 3 years after publication of this paper, to researchers who provide a methodologically sound proposal that includes a protocol and a statistical analysis plan and is not in conflict with the investigators’ research plans. Proposals should be directed to the corresponding author and will need to be reviewed by the study’s principal investigators. To gain access, data requestors will need to sign a data access agreement.
Code availability
Data were analysed using custom scripts created in freely-available R Programming (v.4.1.2). All custom code used to analyse the data in this manuscript are available on Open Science Framework (OSF): https://osf.io/2hwcg/.
References
Brodsky, B. S., Groves, S. A., Oquendo, M. A., Mann, J. J. & Stanley, B. Interpersonal precipitants and suicide attempts in borderline personality disorder. Suicide Life Threat. Behav. 36, 313–322 (2006).
Paris, J. & Zweig-Frank, H. A twenty-seven year follow-up of borderline patients. Compr. Psychiatry 42, 482–487 (2001).
Söderholm, J. J., Socada, J. L., Rosenström, T., Ekelund, J. & Isometsä, E. T. Borderline personality disorder with depression confers significant risk of suicidal behavior in mood disorder patients—a comparative study. Front. Psychiatry 11, 290 (2020).
McMain, S. F. et al. Outcome trajectories and prognostic factors for suicide and self-harm behaviors in patients with borderline personality disorder following one year of outpatient psychotherapy. J. Pers. Disord. 32, 497–512 (2018).
Gartlehner, G. et al. Pharmacological treatments for borderline personality disorder: a systematic review and meta-analysis. CNS Drugs 35, 1053–1067 (2021).
Gunderson, J. G. Borderline Personality Disorder: A Clinical Guide 2nd edn (American Psychiatric Press, 2008).
Kellner, C. H. et al. ECT in treatment-resistant depression. Am. J. Psychiatry 169, 1238–1244 (2012).
Yip, A. G., Ressler, K. J., Rodriguez-Villa, F., Siddiqi, S. H. & Seiner, S. J. Treatment outcomes of electroconvulsive therapy for depressed patients with and without borderline personality disorder: a retrospective cohort study. J. Clin. Psychiatry 82, 19m13202 (2021).
Kaster, T. S., Goldbloom, D. S., Daskalakis, Z. J., Mulsant, B. H. & Blumberger, D. M. Electroconvulsive therapy for depression with comorbid borderline personality disorder or post-traumatic stress disorder: a matched retrospective cohort study. Brain Stimul. 11, 204–212 (2018).
Daskalakis, Z. J. et al. Magnetic seizure therapy (MST) for major depressive disorder. Neuropsychopharmacology 45, 276–282 (2020).
Weissman, C. R. et al. Magnetic seizure therapy for suicidality in treatment-resistant depression. JAMA Netw. Open 3, e207434 (2020).
Fitzgerald, B. et al. A pilot study of the comparative efficacy of 100 Hz magnetic seizure therapy and electroconvulsive therapy in persistent depression. Depress. Anxiety 35, 393–401 (2018).
Cretaz, E., Brunoni, A. R. & Lafer, B. Magnetic seizure therapy for unipolar and bipolar depression: a systematic review. Neural Plast. https://doi.org/10.1155/2015/521398 (2015).
Chen, M. et al. Comparative efficacy and cognitive function of magnetic seizure therapy vs. electroconvulsive therapy for major depressive disorder: a systematic review and meta-analysis. Transl. Psychiatry 11, 437 (2021).
Unoka, Z. & Richman, M. J. Neuropsychological deficits in BPD patients and the moderator effects of co-occurring mental disorders: a meta-analysis. Clin. Psychol. Rev. 44, 1–12 (2016).
Reyes-López, J. et al. Clinical improvement in patients with borderline personality disorder after treatment with repetitive transcranial magnetic stimulation: preliminary results. Braz. J. Psychiatry. 40, 97–104 (2018).
Feffer, K. et al. Dorsomedial prefrontal rTMS for depression in borderline personality disorder: a pilot randomized crossover trial. J. Affect. Disord. 301, 273–280 (2022).
Calderón-Moctezuma, A. R. et al. Improvement in borderline personality disorder symptomatology after repetitive transcranial magnetic stimulation of the dorsomedial prefrontal cortex: preliminary results. Braz. J. Psychiatry 43, 65–69 (2021).
Cailhol, L. et al. Borderline personality disorder and rTMS: a pilot trial. Psychiatry Res. 216, 155–157 (2014).
Miller, I. W., Norman, W. H., Bishop, S. B. & Dow, M. G. The modified scale for suicidal ideation: reliability and validity. J. Consult. Clin. Psychol. 54, 724–725 (1986).
Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62 (1960).
Rush, A. J., Carmody, T. & Reimitz, P. E. The inventory of depressive symptomatology (IDS): clinician (IDS-C) and self-report (IDS-SR) ratings of depressive symptoms. Int. J. Methods Psychiatr. Res. 9, 45–59 (2000).
Zanarini, M. C. et al. Zanarini rating scale for borderline personality disorder (ZAN-BPD): a continuous measure of DSM-IV borderline psychopathology. J. Pers. Disord. 17, 233–242 (2003).
Harvey, P. D. Domains of cognition and their assessment. Dialogues Clin. Neurosci. 21, 227–237 (2019).
Markham, D. Attitudes towards patients with a diagnosis of borderline personality disorder: social rejection and dangerousness. J. Ment. Health 12, 595–612 (2003).
Soloff, P. H., Lynch, K. G. & Kelly, T. M. Childhood abuse as a risk factor for suicidal behavior in borderline personality disorder. J. Pers. Disord. 16, 201–214 (2002).
Storebø, O. J. et al. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst. Rev. 5, CD012955 (2020).
De Cou, C. R. & Comtois, K. A. Dialectical behavior therapy is effective for the treatment of suicidal behavior: a meta-analysis. Behav. Ther. https://doi.org/10.1016/j.beth.2018.03.009 (2019).
Loo, C. K., Katalinic, N., Martin, D., & Schweitzer, I. A review of ultrabrief pulse width electroconvulsive therapy. Ther. Adv. Chronic Dis. https://doi.org/10.1177/2040622311432493 (2012).
Daskalakis, Z. J. et al. Confirmatory Efficacy and Safety Trial of Magnetic Seizure Therapy for Depression (CREST-MST): study protocol for a randomized non-inferiority trial of magnetic seizure therapy versus electroconvulsive therapy. Trials 22, 786 (2021).
Deng, Z. D., Lisanby, S. H. & Peterchev, A. V. Electric field strength and focality in electroconvulsive therapy and magnetic seizure therapy: a finite element simulation study. J. Neural Eng. 8, 016007 (2011).
Lee, W. H., Lisanby, S. H., Laine, A. F. & Peterchev, A. V. Stimulation strength and focality of electroconvulsive therapy and magnetic seizure therapy in a realistic head model. In Proc. 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society 410–413 (ed. Brenan, C.) (IEEE, 2014); https://doi.org/10.1109/EMBC.2014.6943615
Newton-Howes, G. et al. Influence of personality on the outcome of treatment in depression: systematic review and meta-analysis. J. Pers. Disord. 28, 577–593 (2014).
UK ECT Review Group Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet 361, 799–808 (2003). 8.
Posner, K. et al. The Columbia–Suicide Severity Rating Scale (C-SSRS): initial validity and internal consistency findings from three multi-site studies with adolescents and adults. Am. J. Psychiatry 168, 266–1277 (2011).
Joiner, T. E., Rudd, M. D. & Rajab, M. H. The modified scale for suicidal ideation: factors of suicidality and their relation to clinical and diagnostic variables. J. Abnorm. Psychol. 106, 260–265 (1997).
Clum, G. A. & Yang, B. Additional support for the reliability and validity of the Modified Scale for Suicide Ideation. Psychol. Assess. 7, 122–125 (1995).
Office of Communications, Division of Drug Information, Center for Drug Evaluation and Research Guidance for Industry: Suicidal Ideation and Behavior: Prospective Assessment of Occurrence in Clinical Trials (Food and Drug Administration, 2012); https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-industry-suicidal-ideation-and-behavior-prospective-assessment-occurrence-clinical-trials
Sun, Y. et al. Magnetic seizure therapy reduces suicidal ideation and produces neuroplasticity in treatment-resistant depression. Transl. Psychiatry 8, 253 (2018).
Bani-Fatemi, A. et al. Structural and functional alterations of the suicidal brain: an updated review of neuroimaging studies. Psychiatry Res. Neuroimaging 278, 77–91 (2018).
Wise, T. et al. Instability of default mode network connectivity in major depression: a two-sample confirmation study. Transl. Psychiatry 7, e1105 (2017).
Adolphs, R. The social brain: neural basis of social knowledge. Annu. Rev. Psychol. 60, 693–716 (2009).
Wrege, J. S. et al. Negative affect moderates the effect of social rejection on frontal and anterior cingulate cortex activation in borderline personality disorder. Cogn. Affect. Behav. Neurosci. 19, 1273–1285 (2019).
Martin, A. K., Dzafic, I., Ramdave, S. & Meinzer, M. Causal evidence for task-specific involvement of the dorsomedial prefrontal cortex in human social cognition. Soc. Cogn. Affect. Neurosci. 12, 1209–1218 (2017). 1.
Soloff, P. H. & Chiapetta, L. Subtyping borderline personality disorder by suicidal behavior. J. Pers. Disord. 26, 468–480 (2012).
Kaurin, A., Dombrovski, A. Y., Hallquist, M. N. & Wright, A. G. C. Momentary interpersonal processes of suicidal surges in borderline personality disorder. Psychol. Med. 10, 1–11 (2020).
Lisoni, J. et al. Efficacy and tolerability of brain stimulation interventions in borderline personality disorder: state of the art and future perspectives—a systematic review. Prog. Neuropsychopharmacol. Biol. Psychiatry. 116, 110537 (2022).
Konstantinou, G. N. et al. Repetitive transcranial magnetic stimulation in patients with borderline personality disorder: a systematic review. Psychiatry Res. 304, 114145 (2021).
Cho, S. S. et al. Investing in the future: stimulation of the medial prefrontal cortex reduces discounting of delayed rewards. Neuropsychopharmacology 40, 546–553 (2015).
Giesen-Bloo, J. H., Wachters, L. M., Schouten, E. & Arntz, A. The Borderline Personality Disorder Severity Index-IV: psychometric evaluation and dimensional structure. Pers. Individ. Dif. 49, 136–141 (2010).
Deng, Z., Lisanby, S. H. & Peterchev, A. V. Electric field depth–focality tradeoff in transcranial magnetic stimulation: stimulation comparison of 50 coil designs. Brain Stimul. 6, 1–13 (2013).
Loranger, A. M. in Assessment and Diagnosis of Personality Disorders. The ICD-10 International Personality Disorder Examination (IPDE) (eds Loranger, A. M. & Sartorius, N.) 43–51 (Cambridge Univ. Press, 1997).
First, M. B., Spitzer, R. L., Gibbon, M. & Williams, J. B. W. Structured clinical interview for DSM-IV axis I disorders: SCID-I/P v.2.0 (Biometrics Research Dept, New York State Psychiatric Institute, 1995).
Sackeim, H. A. The definition and meaning of treatment-resistant depression. J. Clin. Psychiatry 62, 10–17 (2001).
Oquendo, M. A. et al. A computer algorithm for calculating the adequacy of antidepressant treatment in unipolar and bipolar depression. J. Clin. Psychiatry 64, 825–833 (2003).
Young, R. C., Biggs, J. T., Ziegler, V. E. & Meyer, D. A. A rating scale for mania: reliability, validity and sensitivity. Br. J. Psychiatry 133, 429–435 (1978).
Delis, D. C., Kramer, J. H., Kaplan, E. & Ober, B. A. CVLT, California Verbal Learning Test: Adult Version: Manual (Psychological Corporation, 1987).
Williams, J. M. & Broadbent, K. Autobiographical memory in suicide attempters. J. Abnorm. Psychol. 95, 144–149 (1986).
Benedict, R. H. B., Schretlen, D., Groninger, L., Dobraski, M. & Shpritz, B. Revision of the brief visuospatial memory test: studies of normal performance, reliability, and validity. Psychol. Assess. 8, 145–153 (1996).
Wechsler, D. Wechsler Adult Intelligence Scale–Fourth Edition (WAIS-IV) (APA PsycTests, 2008).
Delis, D. C., Kaplan, E. & Kramer, J. H. Delis–Kaplan executive function system (D–KEFS) (APA PsycTests, 2001).
Arnett, J. A. & Labovitz, S. S. Effect of physical layout in performance of the trail making test. Psychol. Assess. 7, 220–221 (1995).
Holdnack, H. A. Wechsler Test of Adult Reading: WTAR (Psychological Corporation, 2001).
Zanarini, M. C., Weingeroff, J. L., Frankenburg, F. R. & Fitzmaurice, G. M. Development of the self-report version of the Zanarini Rating Scale for Borderline Personality Disorder. Personal. Ment. Health 9, 243–249 (2015).
Acknowledgements
First and foremost, we thank the participants in this study for their time and meaningful contribution to scientific research. This research was supported by a 2014 NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation (BBRF) awarded to A.C.R. and Z.D. (ID: 22376). J.M.T. was supported by a Canadian Institutes of Health Research (CIHR) Fellowship Award (2019–2021). Z.D.’s work has been supported by the CIHR, the National Institutes of Mental Health (NIMH), Brain Canada and the Temerty Family and Grant Family through the Centre for Addiction and Mental Health (CAMH) Foundation and the Campbell Institute. A.C.R. is a BBRF ‘Families for Borderline Personality Disorder Investigator’ and University of Toronto Scarborough Research Excellence Faculty Scholar and reports research grants from the Social Sciences and Humanities Research Council of Canada, American Foundation for Suicide Prevention, CAMH Foundation and the Ministry of Research & Innovation, Province of Ontario. S.F.M. has received research funding from the CIHR. D.M.B. has received research support from the CIHR, NIH, Brain Canada and the Temerty Family through the CAMH Foundation.
Author information
Authors and Affiliations
Contributions
A.C.R., S.F.M., D.M.B. and Z.D. designed the study and supervised the work. J.M.T., A.C.R., N.H., D.M.B. and Z.D. were involved in preparation and submission of regulatory approvals. J.M.T., S.F.M., N.H., R.C., D.M.B. and Z.D. were involved in data collection. J.M.T. analysed the data and drafted the manuscript. All co-authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare the following competing interests: Z.D. has received research and equipment in-kind support for an investigator-initiated study through Brainsway Inc and Magventure Inc. He is also on the scientific advisory board for Brainsway Inc. D.M.B. received research support and in-kind equipment support for an investigator-initiated study from Brainsway Ltd, and he has been the site principal investigator for sponsor-initiated studies for Brainsway Ltd. He also receives in-kind equipment support from Magventure for investigator-initiated studies. He received medication supplies for an investigator-initiated trial from Indivior. He has participated in advisory boards for Welcony Inc and for Janssen. None of these organizations played a role in the conceptualization, design, data collection, analysis, decision to publish or preparation of this manuscript.
Peer review
Peer review information
Nature Mental Health thanks Jacopo Lisoni and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Tables 1 and 2, Inclusion and Exclusion Criteria, MST Protocol and Anaesthesia, and references.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Traynor, J.M., Ruocco, A.C., McMain, S.F. et al. A feasibility trial of conjoint magnetic seizure therapy and dialectical behavior therapy for suicidal patients with borderline personality disorder and treatment-resistant depression. Nat. Mental Health 1, 45–54 (2023). https://doi.org/10.1038/s44220-022-00003-x
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s44220-022-00003-x
This article is cited by
-
Non-invasive Brain Stimulation in the Management of Suicidal Behavior
Current Behavioral Neuroscience Reports (2024)
-
Pre-clinical indications of brain stimulation treatments for non-affective psychiatric disorders, a status update
Translational Psychiatry (2023)