Abstract
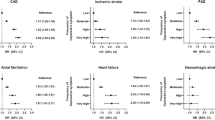
Loneliness and social isolation are crucial triggers in the development of cardiovascular disease (CVD) and depression. This study aimed to explore the associations of loneliness and social isolation with the transition from incident CVD to subsequent depression. Multistate models were constructed to investigate the effects of loneliness and social isolation on the transitions from a healthy state to incident CVD, further to subsequent depression and to death in the UK Biobank cohort (N = 265,794). Participants in the loneliness group had a greater risk for the transition from incident CVD to subsequent depression (hazard ratio = 2.008; 95% confidence interval 1.751–2.351). The hazard ratios of the transition from incident CVD to subsequent depression were 1.148 (1.036–1.274) in the moderately isolated group and 1.173 (1.020–1.348) in the most isolated group. These findings highlight the need for interventions targeting loneliness and social isolation to mitigate the risk of CVD and depression.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$79.00 per year
only $6.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
This project corresponds to UK Biobank application ID 46478. The UKB data are available through the UK Biobank Access Management System (https://www.ukbiobank.ac.uk/). The variables utilized in this study are detailed in Supplementary Table 17.
Code availability
The code used for multistate analyses is available via the GitHub repository at https://github.com/xinqi0702/mstate.
References
GBD 2021 Causes of Death Collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2100–2132 (2024).
Piao, J. et al. Alarming changes in the global burden of mental disorders in children and adolescents from 1990 to 2019: a systematic analysis for the Global Burden of Disease study. Eur. Child Adolesc. Psychiatry 31, 1827–1845 (2022).
Djärv, T., Wikman, A. & Lagergren, P. Number and burden of cardiovascular diseases in relation to health-related quality of life in a cross-sectional population-based cohort study. BMJ Open 2, e001554 (2012).
Yamabe, K., Liebert, R., Flores, N. & Pashos, C. L. Health-related quality of life outcomes, economic burden, and associated costs among diagnosed and undiagnosed depression patients in Japan. Clinicoeconon. Outcomes Res. 11, 233–243 (2019).
Correll, C. U. et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry 16, 163–180 (2017).
Kendler, K. S., Gardner, C. O., Fiske, A. & Gatz, M. Major depression and coronary artery disease in the Swedish twin registry: phenotypic, genetic, and environmental sources of comorbidity. Arch. Gen. Psychiatry 66, 857–863 (2009).
Jha, M. K., Qamar, A., Vaduganathan, M., Charney, D. S. & Murrough, J. W. Screening and management of depression in patients with cardiovascular disease: JACC state-of-the-art review. J. Am. Coll. Cardiol. 73, 1827–1845 (2019).
Moradi, M., Doostkami, M., Behnamfar, N., Rafiemanesh, H. & Behzadmehr, R. Global prevalence of depression among heart failure patients: a systematic review and meta-analysis. Curr. Probl. Cardiol. 47, 100848 (2022).
Golaszewski, N. M. et al. Evaluation of social isolation, loneliness, and cardiovascular disease among older women in the US. JAMA Netw. Open 5, e2146461 (2022).
Zhang, Y. et al. Loneliness, social isolation, depression and anxiety among the elderly in Shanghai: findings from a longitudinal study. Arch. Gerontol. Geriatr. 110, 104980 (2023).
Matthews, T. et al. Social isolation, loneliness and depression in young adulthood: a behavioural genetic analysis. Soc. Psychiatry Psychiatr. Epidemiol. 51, 339–348 (2016).
Cacioppo, S., Grippo, A. J., London, S., Goossens, L. & Cacioppo, J. T. Loneliness: clinical import and interventions. Perspect. Psychol. Sci. 10, 238–249 (2015).
Escalante, E., Golden, R. L. & Mason, D. J. Social isolation and loneliness: imperatives for health care in a post-COVID world. JAMA 325, 520–521 (2021).
Freedman, A. & Nicolle, J. Social isolation and loneliness: the new geriatric giants: approach for primary care. Can. Fam. Physician 66, 176–182 (2020).
Weeks, M. S. & Asher, S. R. Loneliness in childhood: toward the next generation of assessment and research. Adv. Child Dev. Behav. 42, 1–39 (2012).
Paul, E., Bu, F. & Fancourt, D. Loneliness and risk for cardiovascular disease: mechanisms and future directions. Curr. Cardiol. Rep. 23, 68 (2021).
Bowirrat, A. & Elman, I. Neurogenetics and epigenetics of loneliness. Psychol. Res. Behav. Manage. 16, 4839–4857 (2023).
Valtorta, N. K., Kanaan, M., Gilbody, S., Ronzi, S. & Hanratty, B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart 102, 1009–1016 (2016).
Christiansen, J. et al. Loneliness, social isolation, and chronic disease outcomes. Ann. Behav. Med. 55, 203–215 (2021).
Bae, S. M. The association between adverse childhood and adulthood experiences, social isolation, loneliness, and depression among young adults in South Korea. Int. J. Environ. Res. Public Health 20, 6900 (2023).
Díaz-Mardomingo, M. D. C. et al. Sex-related differences in the associations between diurnal cortisol pattern and social and emotional loneliness in older adults. Front. Psychol. 14, 1199405 (2023).
Xia, N. & Li, H. Loneliness, social isolation, and cardiovascular health. Antioxid. Redox Signal. 28, 837–851 (2018).
Leistner, C. & Menke, A. Hypothalamic–pituitary–adrenal axis and stress. Handb. Clin. Neurol. 175, 55–64 (2020).
Kovaleva, M., Spangler, S., Clevenger, C. & Hepburn, K. Chronic stress, social isolation, and perceived loneliness in dementia caregivers. J. Psychosoc. Nurs. Ment. Health Serv. 56, 36–43 (2018).
Gulyaeva, N. V. Stress-associated molecular and cellular hippocampal mechanisms common for epilepsy and comorbid depressive disorders.Biochemistry 86, 641–656 (2021).
Van Bogart, K. et al. The association between loneliness and inflammation: findings from an older adult sample. Front. Behav. Neurosci. 15, 801746 (2021).
Hackett, R. A., Hamer, M., Endrighi, R., Brydon, L. & Steptoe, A. Loneliness and stress-related inflammatory and neuroendocrine responses in older men and women. Psychoneuroendocrinology 37, 1801–1809 (2012).
Akçay, E. et al. Loneliness, internalizing symptoms, and inflammatory markers in adolescent COVID-19 survivors. Child Care Health Dev. 48, 1112–1121 (2022).
Li, H. & Xia, N. The role of oxidative stress in cardiovascular disease caused by social isolation and loneliness. Redox Biol. 37, 101585 (2020).
Matthews, T. et al. Social isolation, loneliness, and inflammation: a multi-cohort investigation in early and mid-adulthood. Brain Behav. Immun. 115, 727–736 (2024).
Shankar, A., McMunn, A., Banks, J. & Steptoe, A. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol. 30, 377–385 (2011).
Colaianna, M. et al. Neuroendocrine profile in a rat model of psychosocial stress: relation to oxidative stress. Antioxid. Redox Signal. 18, 1385–1399 (2013).
Chu, H. Y. & Chan, H. S. Loneliness and social support among the middle-aged and elderly people with visual impairment. Int. J. Environ. Res. Public Health 19, 14600 (2022).
Kotwal, A. A. et al. A peer intervention reduces loneliness and improves social well-being in low-income older adults: a mixed-methods study. J. Am. Geriatr. Soc. 69, 3365–3376 (2021).
Zaid, M. et al. Associations of high-density lipoprotein particle and high-density lipoprotein cholesterol with alcohol intake, smoking, and body mass index—the INTERLIPID Study. Circ. J. 82, 2557–2565 (2018).
Barua, R. S. & Ambrose, J. A. Mechanisms of coronary thrombosis in cigarette smoke exposure. Arterioscler. Thromb. Vasc. Biol. 33, 1460–1467 (2013).
Wang, X. et al. Joint association of loneliness and traditional risk factor control and incident cardiovascular disease in diabetes patients. Eur. Heart J. 44, 2583–2591 (2023).
Hackett, R. A., Hudson, J. L. & Chilcot, J. Loneliness and type 2 diabetes incidence: findings from the English Longitudinal Study of Ageing. Diabetologia 63, 2329–2338 (2020).
Sudlow, C. et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
Song, Y. et al. Social isolation, loneliness, and incident type 2 diabetes mellitus: results from two large prospective cohorts in Europe and East Asia and Mendelian randomization. EClinicalMedicine 64, 102236 (2023).
Wang, X. et al. Air pollution associated with incidence and progression trajectory of chronic lung diseases: a population-based cohort study. Thorax 78, 698–705 (2023).
Wang, X. et al. Ambient air pollution associated with incident asthma, subsequent cardiovascular disease and death: a trajectory analysis of a national cohort. J. Hazard. Mater. 460, 132372 (2023).
Bisquera, A. et al. Inequalities in developing multimorbidity over time: a population-based cohort study from an urban, multi-ethnic borough in the United Kingdom. Lancet Reg. Health. Eur. 12, 100247 (2022).
Han, Y., Hu, Y. & Yu, C. Lifestyle, cardiometabolic disease, and multimorbidity in a prospective Chinese study. Eur. Heart J. 42, 3374–3384 (2021).
Wang, X. et al. Population attributable fraction of lung cancer due to genetic variants, modifiable risk factors, and their interactions: a nationwide prospective cohort study. Chemosphere 301, 134773 (2022).
Acknowledgments
We thank the UK Biobank participants and the UK Biobank team for their work in collecting, processing and disseminating these data for analysis. This study was supported by the Natural Science Basic Research Plan in Shaanxi Province of China (2021JCW-08 to F.Z.). The funding body played no role in study design, data collection and analysis, decision to publish or preparation of the paper.
Author information
Authors and Affiliations
Contributions
F.Z. and X.Q. designed and conceptualized this study. F.Z., X.Q. and S.C. acquired the data. X.Q., W.W., C.P. and L.L. performed the data generation, processing and statistical analyses. J.Y., J.H., Y.W., M.K. and B.C. contributed to the interpretation of the significant results and scientific discussion. All of the authors wrote and revised the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Elisabeth Lambert and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Tables 1–17.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qi, X., Cheng, S., Yang, J. et al. The risk of social isolation and loneliness on progression from incident cardiovascular disease to subsequent depression. Nat. Mental Health 3, 558–566 (2025). https://doi.org/10.1038/s44220-025-00418-2
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44220-025-00418-2