Abstract
The prevalence and burden of mental disorders have worsened despite increased community awareness. Enhanced access to treatments alone is unlikely to deliver improvements in population mental health, so more attention needs to be paid to social and environmental influences. Here we estimate the health benefits and economic value of improving the social determinants of mental health within Brisbane South, a diverse population of 1.2 million people, in Australia. The incremental net monetary benefit (combining costs and monetized health outcomes) derived from 5% improvements in the average yearly change of social cohesion, childhood difficulties, substance misuse and unemployment over 11 years from 2024 to 2034 was projected to be AUD$146.64 million, AUD$234.50 million, AUD$281.67 million and AUD$100.43 million, respectively. Quality-adjusted life years, suicide deaths, emergency department presentations and self-harm hospitalizations were also improved. This study demonstrates the health and economic value of investing in the social determinants of mental health.
Similar content being viewed by others
Main
Despite greater community awareness about mental health, the prevalence and burden associated with mental disorders are deteriorating1,2,3,4. Depressive disorders were the second-highest cause of nonfatal health burden globally in 2021, an increase in years lived with disability of 36.5% from 20105. Anxiety disorders were the sixth-highest cause of nonfatal burden5. Young people, in particular, have experienced a serious deterioration in mental health in the past 14 years. For example, a longitudinal survey found that the prevalence of depression and anxiety more than doubled between 2009 and 2021 in Australian young people aged 15–34 years (from 6.1% to 14.4% for males and from 12.7% to 29.3% for females)6. The prevalence of psychological distress also more than doubled between 2011 and 2021 in young people in Australia aged 15–24 years (from 18.4% to 42.3%)6. Suicide was the leading cause of death among people aged 15–44 in 2022 in Australia7. Although the decline in the mental health of younger age groups has been underway for more than a decade, the coronavirus disease 2019 pandemic and associated lockdowns have influenced these estimates in recent years8. Increases in the provision of mental health care have been outweighed by a concurrent increase in the incidence of high to very high levels of distress, as demonstrated by simulation modeling9. The Australian experience is replicated across most high-income countries10,11 and is also an emerging threat in developing nations12.
There are long-term consequences of young people experiencing mental disorders, for individuals and their families, for communities and for the whole economy. These disorders are a risk factor for a wide range of chronic physical illnesses13 and affect their ability to participate in the labor force later in life14. Some of this burden could be averted if young people had full access to optimal treatment15. However, expanding access to mental health treatments alone is insufficient to reduce the burden of poor mental health due to the rising incidence of disorders9,16, which occur in—and interact with—the context of wider social, economic, commercial and environmental factors. More meaningful, long-term, intergenerational reductions in mental illness are thus likely to be achieved by ‘moving upstream’, targeting the ‘causes of the causes’ and preventing mental ill health before it develops17,18. This could be achieved by a more intentional approach to choosing mental health and well-being as a key policy objective (which can be formally conceptualized as Mental Wealth19) and designing and implementing evidence-based economic and social systems and environments that foster this objective as the norm17,20.
Economic implications are interwoven through the causes and consequences of mental disorders. The global economic burden of mental disorders was estimated to be between US$2.5 trillion and US$8.5 trillion in 2010 depending on the methodological approach used to monetize health impacts21. The more conservative approach is expected to reach annual costs of US$6 trillion by 203021. In the USA, more health expenditure is dedicated to treating mental health disorders than any other disease area22. The persistent nature of mental health and substance use disorders in the USA, and other countries, suggests this expenditure is not currently allocated efficiently. Furthermore, most of the economic burden of poor mental health is incurred outside the health care system23. For example, the Australian Productivity Commission estimated there were AUD$39 billion in productivity costs associated with poor mental health and suicide in 2018–2019 compared with AUD$16 billion of mental health-related healthcare expenditure24. Estimates of the economic burden of mental illness are a part of the prioritization problem facing decision-makers (that is ‘How big is the problem?’); another is economic evidence supporting interventions (that is, ‘What can be done about it?’). Although much evidence exists on the cost-effectiveness of treatments25,26 and the prevention of mental ill health and promotion of mental health27,28, many gaps still exist29,30,31, including strategies that target the social determinants of mental health. Evidence on the economic credentials of current expenditure is also lacking32, and accountability in mental health decision-making and planning is poor33. Generating more and better economic evidence is critical for guiding better investment decisions and helping decision-makers prioritize the areas and strategies that can have the biggest impact for improving mental health34.
The Lancet Commission on Global Mental Health and Sustainable Development recognized that treatments alone are unlikely to achieve sufficient improvements in population mental health and that more attention needs to be paid to social and environmental influences, particularly during important developmental periods in the early life course, childhood and adolescence12. The social determinants of mental health refer to the social, economic and physical environments that directly influence the incidence, prevalence and severity of mental illness35,36. Examples of the structural risk factors that influence mental health include low educational attainment, unemployment and underemployment, poverty, food insecurity, unstable housing, social isolation and loneliness, discrimination, early life and childhood adversity and trauma, neighborhood social and physical conditions, and access to best practice and affordable health care37,38. These determinants can play out in regionally specific ways to impact population mental health and well-being. They often have a bidirectional relationship with mental health and are interlinked and dynamic, interacting with each other in a complex causal web, highlighting the importance of systems thinking when developing strategies to overcome them17. Most of these risk factors are associated with a social gradient based on socioeconomic disadvantage and inequality, whereby “the greater the inequality the higher the inequality in risk”35. There is also increasing awareness of the role of ‘global megatrends’ in harming the mental health of young people11 as well as the ongoing shadow cast by the coronavirus disease pandemic. These megatrends are broader concepts than social determinants, referring to long-lasting societal upheaval in environmental, social, economic, political or technological domains. Nevertheless, they overlap with the social determinants discussed here.
Evidence exists supporting the causal link between social determinants and later mental health outcomes37. The importance of different social determinants varies across the life course37. An umbrella review of 46 meta-analyses found that numerous social determinants, such as midlife unemployment, homelessness and interaction with the criminal justice system, had consistent associations with suicide-related outcomes39. Another umbrella review included 289 systematic reviews on the evidence for potential mechanisms by which social determinants affect mental health conditions16. This evidence was mapped to the United Nations Sustainable Development Goals using five domains: demographic, economic, neighborhood, environmental events, and social and cultural domains16. The World Health Organization recently issued new guidance on mental health policy and strategic action plans that has a strong emphasis on social and structural determinants40. Despite this evidence, social determinants of mental health are rarely addressed within child and youth health policies and services planning41, and the social determinants of mental health are either not improving or getting worse over time11,32. Investing in child and youth mental health has the potential to optimize the return on investment of scarce healthcare resources, given the potential for major intergenerational impacts that stretch into adulthood and beyond.
The Lancet Psychiatry Commission on Youth Mental Health specify enhancing awareness and advocacy of the social and economic determinants of mental ill health as the first key element of optimal youth mental health care11. However, in the context of scarcity and budgetary constraint, decision-makers require guidance on which social determinants should be prioritized, and what specific interventions can be implemented to improve them. This is one of the reasons why prominent reviews of the social determinants of mental health call for the generation of more economic evidence in this area36,42.
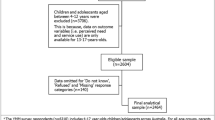
The objective of this Analysis was to estimate the health benefits and economic value of improving the social determinants of mental health for the Brisbane South region in Australia using system dynamics simulation modeling. To enhance the validity, transparency and usability of the Analysis, participatory model-building processes were followed, including meaningful participation of young people with lived experience of mental health conditions. This makes the Analysis relevant to the multifaceted nature of the problem, which involves diverse stakeholders engaging with the issue in real-world contexts. Results were reported for a variety of health outcomes and economic summary measures, and the cost impacts were disaggregated by payer. Only a selection of social determinants have been included in this Analysis. These were priority determinants identified by stakeholders of the region as key drivers of youth mental health outcomes and where sufficient data could be obtained.
Results
All costs are reported in 2020–2021 Australian dollars. All estimates relate to all ages of the Brisbane South Primary Health Network region, a population of 1.2 million people (4% of the Australian population), and are cumulative over the 11-year time horizon of the model (2024–2034) unless otherwise specified. Estimates are incremental compared with business as usual. Costs and quality-adjusted life years (QALYs) were discounted at 5%. Table 1 contains a definition of each social determinant and the specific changes that were applied for each scenario of improvement. ‘Improvement’ in this context could mean a reduction in the rate at which people develop substance misuse disorder or an increase in social cohesion, for example (Table 1).
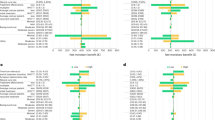
The greatest increase in health outcomes in terms of QALYs was attained by a 5% improvement in childhood difficulties (2,621 QALYs), followed by social cohesion (1,309 QALYs) and substance misuse (82 QALYs) (Fig. 1; Supplementary Table 3 in Supplementary Information part B). A 5% improvement in the other determinants was also associated with an increase in QALYs but to a lesser extent. Reducing substance misuse and improving social cohesion individually resulted in the greatest number of suicide deaths avoided (Supplementary Table 3 in Supplementary Information part B). Reducing substance misuse, improving social cohesion and reducing childhood difficulties individually realized the greatest number of avoided self-harm hospitalizations. Improving childhood difficulties and social cohesion avoided the greatest number of mental health-related emergency department presentations.
Improving the social determinants of mental health substantially reduced downstream costs. For the health care perspective, the greatest reduction in costs was achieved by a 5% improvement in homelessness ($16.4 million), followed by social cohesion ($16.3 million) and childhood difficulties ($11.7 million) (Fig. 2; Supplementary Table 1 in Supplementary Information part B). A 5% improvement in substance misuse resulted in $1 million of downstream cost savings. Improvements in unemployment, underemployment and discontinuation of secondary or tertiary education resulted in cost reductions less than this.
For the societal perspective, the greatest reductions in costs were seen by 5% improvements in substance misuse ($274.8 million), unemployment ($97.3 million), social cohesion ($38 million) and homelessness ($38 million) (Fig. 3; Supplementary Table 1 in Supplementary Information part B). The downstream cost savings were attributed largely to a reduction in lost productivity. These productivity savings amounted to $157.3 million for substance misuse, $95 million for unemployment, and $20.6 million for social cohesion, for the societal perspective.
When analyzing cost impacts by payer for the societal perspective, homelessness ($13.6 million), substance misuse ($10.4 million) and social cohesion ($7.3 million) were the most important determinants for the Australian (National) Government. Five percent improvements in substance misuse ($107.8 million), homelessness ($19.1 million), social cohesion ($16.3 million) and childhood difficulties ($11.5 million) achieved the greatest reductions in costs for the Queensland (State) Government. Homelessness was the only determinant that reduced costs for nongovernment payers, which predominantly consists of individuals in the form of out-of-pocket costs. Improvements in all other determinants increased costs for nongovernment payers. (This was mainly due to a reduction in welfare payments received by this group. Changes in these transfer payments result in a decrease in costs to government and zero net impact on total costs. We have not included employment income, nor income tax, in this Analysis, which would be expected to more than offset the reduced welfare payments for individuals.) For reductions in the cost of lost productivity incurred by the general economy, improvements in substance misuse ($157.3 million), unemployment ($95 million), social cohesion ($20.6 million) and underemployment ($10.8 million) achieved the greatest changes.
For all social determinants except social cohesion, the estimated incremental total costs that flowed from a 10% improvement in social determinants were slightly greater than simply doubling the estimates for a 5% improvement (Supplementary Table 1 in Supplementary Information part B).
When costs and QALYs were combined with a willingness to pay per QALY of $83,004 to derive incremental net monetary benefit (INMB) compared with business as usual (a full explanation of these terms and methodology is available in the Methods), a 5% improvement in substance misuse resulted in an INMB of $281.67 million, childhood difficulties $234.50 million, social cohesion $146.64 million and homelessness $38.75 million (Fig. 4; Supplementary Table 2 in Supplementary Information part B). A comparison between 3-year and 11-year time horizons reveals that taking a long-term view would enable decision-makers to exponentially capitalize on the full extent of the net benefit anticipated from improving the social determinants of mental health. For example, for the societal perspective, the INMB for a 5% improvement in social cohesion was $3.99 million at 3 years and $146.64 million at the end of 11 years. Similar findings reinforcing the importance of a long-term view were found for health outcomes (Supplementary Table 3 in Supplementary Information part B). For example, a 5% improvement in social cohesion achieved a reduction of 648 mental health-related emergency department presentations over 11 years, but this was only 12 by the end of 3 years.
Univariate sensitivity analysis found that varying utility values, homelessness costs and substance misuse costs did not change the rank ordering of social determinants based on INMB for the societal perspective (Supplementary Information part B).
Discussion
System dynamics modeling (SDM), including a participatory model-building process, was used to demonstrate the health and economic benefits of improving eight social determinants of mental health. We observe from the model that even modest improvements in determinants resulted in material increases in health outcomes and reductions in costs for both the health care and societal perspectives. This simulation model was developed in collaboration with a diverse group of local stakeholders for a region of 1.2 million people, a process that could be replicated and customized for other regions.
This Analysis provides quantitative support for ‘moving upstream’ to target the underlying causes of a large portion of distress and mental health challenges17,43,44. A decision-maker contemplating how to prioritize the allocation of scarce resources towards improving mental health via social determinants could utilize these estimates by first identifying what their most important objectives are. If their main objective is to maximize the improvement of mental health outcomes in terms of QALYs, then social cohesion and childhood difficulties would be the primary determinants to target. If their main objective is to reduce suicide deaths, targeting substance misuse and social cohesion would maximize this outcome. If their objective is reducing pressure on health care services, improving social cohesion and childhood difficulties achieves the greatest reductions in mental health-related emergency department (ED) presentations, and reducing substance misuse attains the greatest reduction in self-harm hospitalizations.
The greatest reductions in costs for the health care perspective were attained by reductions in childhood difficulties and homelessness. When this perspective was expanded to account for costs incurred outside the health care sector and lost productivity for the societal perspective, reductions in substance misuse and unemployment realized the greatest downstream cost savings.
Ideally, a decision-maker would seek to maximize allocative efficiency through consideration of both health benefits (in this case, in terms of QALYs) and costs by using the INMB, which also accounts for the willingness to pay for a QALY. The ranking based on the highest INMB over 11 years for the societal perspective was (1) substance misuse, (2) childhood difficulties, (3) social cohesion and (4) unemployment. Caution should be applied when interpreting the INMB estimates in this Analysis, as these exclude the cost of interventions normally included in the calculation of INMB .
Overall, social cohesion, childhood difficulties, substance misuse and unemployment are a group of social determinants that could be prioritized on the basis that they were forecast to improve a variety of final (QALYs and suicide deaths) and intermediate (hospitalizations and ED presentations) health outcomes and/or reduce costs for the societal perspective. This adds to, and is consistent with, existing literature on the link between unemployment and suicide45,46, the influence of early life circumstances on mental disorders in later life47,48,49, the importance of social connection for mental health and well-being39,50,51,52,53, and the association between substance misuse and mental health challenges54,55. Given the limitations of universal prevention in mental health4, this Analysis provides quantitative support for targeting more specific, underlying causes. Box 3 provides a summary of systematic review-level evidence of interventions targeting the social determinants of mental health.
The findings of this study highlight the importance of taking a long-term view when considering whether the social determinants of mental health warrant the investment of scarce resources. When comparing the estimates produced here between 3 years and 11 years, much more value, in terms of both health benefits and costs, became apparent by 11 years. The choice of 11 years as the maximum time horizon is itself arbitrary, and the model timeframe could be extended to multiple decades. This would allow a more comprehensive capture of health benefits accrued by people who are younger at the start of the simulation as they age, as well as the potential for intergenerational prevention effects. The ranking of social determinants based on total cost reductions for both the health care and societal perspectives changed over the 11-year timeframe (Figs. 2 and 3) and may change beyond this time horizon.
Taking a societal perspective was useful for analyzing the economic impact of improving the social determinants of mental health, with cost estimates much larger for the societal perspective than for the health care perspective. This was due to the inclusion of additional cost categories, such as lost productivity, the criminal justice system, and non-health care social services for homelessness and substance misuse. There have been calls for greater use of the societal perspective56, or at least reporting both the health care and societal perspectives in economic evaluations57. Perspective can alter the conclusions in economic evaluations for mental health. For example, a systematic review of economic evaluations for depression found that the results in 24% of studies changed quadrant of the cost-effectiveness plane (representing positive or negative differences in costs or health outcomes) when the societal perspective was taken and 5% of studies changed conclusions of whether the intervention was cost-effective or not58. In the case of this Analysis, a societal perspective helps to highlight a more comprehensive picture of benefits available from targeting the social determinants of mental health.
There are a number of limitations to this Analysis. First, only a selection of the social determinants of mental health have been included in this Analysis. These were identified as priority determinants thought to be driving youth mental health outcomes in the region. Some important determinants were not modeled owing to a current lack of data. Examples of excluded determinants include level of income, measures of relative socioeconomic advantage/disadvantage, food security, loneliness, discrimination and inequalities experienced by marginalized groups (for example, First Nations peoples, LGBTQ+, migrants, and culturally and linguistically diverse people). Although all of these are captured to a degree by the composite measure of social cohesion included in this Analysis (Table 1), analyzing these individually would provide a more nuanced picture to a decision-maker to aid their prioritization of scarce resources to particular areas. Second, the choice of 5% and 10% improvements in the social determinants is arbitrary and hypothetical. Five percent was used as the focus for results as something that could be attainable and set as a target by a policymaker. Related to this, we cannot say whether these improvements in social determinants are cost-effective as the cost of the interventions or policy changes required to achieve them is unknown. The cost of implementation would need to be compared with the reported cost offsets and health benefits to determine cost-effectiveness through simulation modeling. Third, although we have estimated cost impacts by payer, the Australian funding system is complex, and no attempt has been made in this Analysis to account for the impacts on original funding sources. Fourth, the capacity for homelessness and substance misuse to have more of a dramatic impact on cost reductions than their increase in QALYs would suggest is because a large portion of their costs is linked directly with that determinant rather than being mediated through levels of distress (which determines QALYs). For example, criminal justice costs are incurred for both substance misuse and homelessness, and any proportional reduction in the prevalence of these determinants has an equivalent reduction in criminal justice costs, regardless of their association and effect on levels of distress or suicide deaths. The same consideration applies to unemployment and underemployment and the productivity impacts linked to employment status. Fifth, we have not included all costs that might be relevant for the societal perspective. One example of this is the increase in earnings that would be received by healthier or newly employed people (represented here by the payer category of ‘nongovernment including individuals’), offsetting the reduction in welfare payments to this group. This has been excluded due to our focus on productivity-related costs. Another example would be carbon emissions and other environmental impacts. These were excluded due to time and resource constraints on the model development process. Another limitation is that only limited univariate sensitivity analysis was carried out, including the two different levels of improvement to determinants (of 5% and 10%) and two different time horizons (3 years and 11 years) (Supplementary Information part B). The main reason for this was the exclusion of defined and costed interventions from the analysis (that is, cost-effectiveness analysis has not been performed). One-way and probabilistic sensitivity analyses are useful for cost-effectiveness analyses because they reveal the circumstances for which the conclusions about cost-effectiveness might change and deriving the uncertainty intervals around economic summary measures. For the present Analysis, decision rules based on the incremental cost-effectiveness ratio, for example, are irrelevant due to the exclusion of interventions. One-way sensitivity analysis of the discount rate, for example, would only serve to change the magnitude of estimates. The limited sensitivity analysis that was performed found that varying utility values, homelessness costs and substance misuse costs did not change the rank ordering of social determinants based on INMB for the societal perspective. Another limitation is that we have included some costs related to carers but not changes in quality of life of carers due to time and resource constraints. This will be included in a future iteration of the model. Adding QALYs to the model for carers would be expected to enhance the value of improving the social determinants of health.
Although specific interventions have not been included in this Analysis, the results reported here do provide some guidance for decision-makers considering investing in interventions that target the social determinants of mental health. For example, if an intervention is expected to achieve a 5% improvement in social cohesion (as defined in Table 1), it could cost up to approximately $16 million over 11 years (discounted) and still be considered cost saving for the health care perspective based on the figures provided in Supplementary Table 1 (Supplementary Information part B) as well as the health benefits specified in Supplementary Table 3 (Supplementary Information part B). For the societal perspective, as long as the intervention cost less than $38 million over 11 years (discounted), it would be considered cost saving. Specific strategies are likely to be context dependent, and policymakers, academics and local communities could work together to both identify contextually appropriate interventions and develop models that can accurately evaluate them to reduce implementation barriers.
Future research directions could include using a similar modeling approach to investigate the cost-effectiveness of interventions targeted at improving the social determinants of mental health based on those that are supported by evidence of effectiveness. This would enable more specific policy actions by estimating the cost of implementing the intervention in a particular region and using the best available evidence to inform its anticipated effectiveness. Future iterations of this modeling could also seek to include an expanded set of benefits and costs that fall in the societal perspective, such as measures of well-being or environmental impacts, as relevant to the intervention and decision context being analyzed. Future research could also investigate the value of improving several social determinants concurrently or combinations of interventions concurrently.
Planning to respond to mental health is often health focused, and typically bound by the realities of funding limitations. While these limitations persist, the modeling approach outlined here vastly expands our capacity to better identify opportunities to respond to community mental health priorities, transcending the health system to more fully account for other key areas of concern, such as employment and housing. This increases our understanding of the relative utility of different interventions and their material impact on people’s lives and on the broader community.
Methods
The Consolidated Health Economic Evaluation Reporting Standards (CHEERS) 2022 were followed when reporting the results and methods of analysis59. The completed CHEERS checklist is available as Supplementary Information. Protocols related to this project have been published on the SDM approach60, economic analysis61 and participatory model-building process62. More detailed methods area available as Supplementary Information.
Model development process
A participatory systems modeling process was undertaken to develop a system dynamics simulation model to estimate the health and economic consequences of three types of system change aimed at improving mental health outcomes for young people: (1) increasing or decreasing the growth rates of health services capacity; (2) implementing or upscaling evidence-based interventions; and (3) changing various social determinants of mental health. The present Analysis was focused on the third group of system changes. The participatory systems modeling component of the project included three in-person workshops with attendance from a range of stakeholders including mental health professionals, primary care physicians, allied health service providers, young people with a lived experience of mental health conditions and their carers, and health agency representatives.
-
In workshop 1, participants identified outcomes of interest, mapped the youth mental health service system in the geographical catchment of Brisbane South Primary Health Network,and identified programs and initiatives of interest, as well as the social determinants that were most important to youth mental health in their region.
-
In workshop 2, the research team presented the basic structure of the model based on the workshop 1 systems mapping exercise to participants for feedback. Participants also provided detailed advice on what new interventions would look like if implemented in their region.
-
In workshop 3, a draft, interactive version of the model was provided to participants for user testing and exploration of key policy and planning insights. This process facilitated ‘sense-checking’ of the model output and identification of bugs or unanticipated findings.
Regular meetings were held with a model development advisory group between the workshops for more detailed components of the model development process. Where model inputs or development decisions were informed by expert advice, this could be informed through any of the workshops, model development group meetings or personal communication with subject matter experts from any of the following roles, noting that these categorizations are somewhat arbitrary and individual participants are likely to span multiple roles and identities:
-
Young people with a lived experience of mental health conditions and their carers.
-
Clinician subject experts such as psychiatrists, psychologists and general practitioners.
-
Academic researchers including health economists, systems modelers, data scientists and research support personnel.
-
Policy, health administration and management representatives, including those from the Primary Health Network and State Department of Health.
-
Representatives from nonhealth sectors such as education and housing.
Research evidence and data were used to parameterize the model, and historical time series data were used to calibrate the model. With regard to searching the literature for mechanisms of effectiveness, a rapid review approach was used, relying where possible on systematic reviews. Parameter values that could not be derived directly from these sources were estimated or calibrated via constrained optimization, using historical time series data for a wide range of sociodemographic and health-related outcomes, including participation and unemployment rates, the prevalence of moderate to very high psychological distress, intentional self-harm hospitalization and suicide mortality rates and rates of mental health service usage. Powell’s method was used to obtain the set of optimal parameter values minimizing the mean of the absolute differences between the observed time series values and the corresponding model outputs, where each difference was expressed as a percentage of the observed value63.
Model structure overview
SDM was chosen for this Analysis owing to its potential for capturing complexity, interactions, dynamics and broader systemic effects relevant to mental health planning34. The model is a logically consistent mathematical framework that integrates best available data and evidence sources with expert and local knowledge (including the expert knowledge of those with a lived experience of mental health conditions and their carers). The model captures population and demographic dynamics, pathways to youth mental health care, service interactions and workforce capacity, and the potentially nonadditive effects of intervention combinations. The model was validated through face validity among stakeholders and by observing its ability to reproduce historic trends across observed data in the region from 2011 to 2022.
The sectors included in the model are:
-
Population, which models the resident population divided into six age brackets (0–4-year-olds, 5–11, 12–14, 15–17, 18–24, and 25 and older),
-
Education, which models students enrolled in primary, secondary and post-secondary education, and people with different levels of highest qualifications,
-
Labor force, which models unemployment, underemployment and participation rates,
-
Not in education, employment nor training (NEET), which models the youth population aged 15–24 years not in education, employment nor training,
-
Homelessness, which models the population experiencing homelessness,
-
Substance misuse, which models the prevalence of 12-month substance misuse disorder and substance misuse closed treatment episodes,
-
Psychological distress/disorder, which models the prevalence of low psychological distress and the prevalence of moderate to very high psychological distress based on the Kessler Psychological Distress Scale (K10)64. The population with moderate to very high psychological distress is further dichotomized by whether nor not they meet the criteria for any 12-month mental disorder,
-
Strengths and difficulties (used as the measure of childhood difficulties), which models the prevalence of behavioral and emotional difficulties among children aged 0–11 years as measured by the Strengths and Difficulties Questionnaire (SDQ),
-
Social cohesion, which models the population level of social cohesion according to the Scanlon–Monash Index of Social Cohesion,
-
Suicidal behaviors, which models the rates of suicide attempts and suicide deaths, and
-
Mental health services, which models mental health services delivered by health professionals and online mental health services.
Supplementary Fig. 1 in Supplementary Information part A provides an overview of the sectors and the causal connections between them. Supplementary Information part A also contains a detailed description of each sector, including its structure, sources of input data and calibration graphs.
Hypothetical improvements in each social determinant of 5% and 10% were chosen as attainable but meaningful levels of improvement that could be set by a policymaker as targets to strive toward. Table 1 contains further details of each determinant and what the levels of improvement mean for each scenario. Additional detail is provided in Supplementary Information part B, where the projection for each social determinant is provided over the 11-year time horizon along with the expected changes with 5% and 10% improvements.
Costs
Supplementary Information part B contains a detailed itemization of each unit cost, its source and derivation methods (Supplementary Tables 4 and 5). In brief, the cost of health services was obtained from the Australian Institute of Health and Welfare and the Independent Health and Aged Care Pricing Authority. Costs associated with homelessness and substance misuse were obtained from gray literature reports estimating the associated economic burden. Employee earnings used in the calculation of productivity estimates were obtained from the Australian Bureau of Statistics.
Health measures and QALYs
The detailed sector descriptions in Supplementary Information part A describe the calculation methods by which key health outcomes are estimated: suicide deaths, ED presentations and self-harm hospitalizations. The QALY is an additional measure of final health outcomes that is useful because it is a composite measure of health that includes both changes in survival and quality of life, reflecting the preference-based utilities of distress-related health states. The prevalence of people experiencing higher levels of distress is a key driver of accumulated QALYs over the timeframe of the model. Because the K10 measure is used to quantify levels of distress in the model, utilities for people aged 12 years and over were derived by using a mapping algorithm to convert low, moderate, high and very high distress levels based on the K10 to the EQ-5D multiattribute utility instrument65, applying mapped utility decrements to Australian age-based population norms66 (Supplementary Table 6 in Supplementary Information part B). Distressed health states for children aged 11 years and younger were based on the SDQ67. A mapping algorithm developed by Sharma et al., with a study population of Australian children, was used to transform SDQ scores to CHU9D utilities (Supplementary Table 7 in Supplementary Information part B)68. The CHU9D has strong psychometric performance in both mental health69 and general pediatric70 populations. A recent systematic review confirmed this was the most recent and relevant mapping algorithm with the SDQ as the starting measure71.
Other economic methods
The time horizon was set to 11 years to allow sufficient time for cost and health consequences to play out after a change to a social determinant but short enough to minimize the uncertainty in future states of the world beyond this timeframe. Sensitivity analysis using a time horizon of 3 years was also conducted and reported here for health outcomes and INMB. A conventional lifetime time horizon is not relevant due to the dynamic nature of the population, where births and positive net migration ensure the population continues to grow. Costs and health consequences were discounted at 5%, based on the reference discount rate set by the Pharmaceutical Benefits Advisory Committee72. Both health care and societal perspectives were adopted due to the diverse stakeholders and decision-makers involved in the participatory model building process, and all results are presented for both perspectives. The societal perspective is broader than, and fully incapsulates, the health care perspective. One of the key differences between the two perspectives is the inclusion of productivity costs in the societal perspective. Costs incurred by nonhealth sectors are also included in the societal perspective. The costs that apply to each perspective are detailed in Supplementary Information part B. Neither univariate nor probabilistic sensitivity analyses were carried out for this Analysis (beyond alternative timeframes, degrees of improvement, utility values and costs related to homelessness and substance misuse). Our choice to exclude sensitivity analysis is predominantly due to the hypothetical nature of the improvements to social determinants. In conventional cost-effectiveness analysis where specific, defined interventions are included, the primary purpose of the sensitivity analysis is to establish the degree of uncertainty around summary economic measures based on the joint probability of all relevant uncertain parameters (probabilistic), or to what degree conclusions may change when individual parameters are varied within plausible ranges, that is, to establish the degree of confidence in whether the binary choice of implementing an intervention represents allocative efficiency. For the present Analysis, the degree of improvement in a social determinant is arbitrary, so the choice of distribution around this would also be arbitrary. Similarly, any univariate change in a parameter would only serve to change the magnitude in anticipated health or cost consequences.
One way sensitivity analysis was conducted on a select group of parameters expected to have the most influential impact on the rank order of social determinants: utility values for ages 12+ varied ±10%; utility values for ages 0–11 varied ±10%; costs related to homelessness varied ±20%; costs related to substance misuse varied ±20%. Results for this sensitivity analysis are reported in Supplementary Information part B.
Economic summary measures
Net monetary benefit (NMB) is a conversion of health into financial units to aid the comparability of strategies and presentation of results. NMB is given by multiplying QALYs by the willingness to pay for a QALY, AUD$83,004, then subtracting costs. The willingness to pay per QALY was obtained from Shiroiwa et al.73 and indexed to the 2021–2022 financial year. We adopted the social value of a QALY (demand for health) approach for valuing the threshold rather than an opportunity cost (supply side) approach74. This is relevant for the present context because the social determinants operate outside the health care sector, so any intervention or policy change would be happening at a broader level than the health sector that is not constrained by the health care budget. Using a willingness to pay for a QALY value from the literature gives us the added benefit of using a threshold based on empirical evidence, rather than an arbitrary threshold (usually AUD$50,000 per QALY in Australia, although this has never been publicly set by a government agency in Australia). INMB is the difference in NMB for a scenario of change compared with business as usual. Although INMBs reported here cannot be interpreted in the conventional manner because the costs of interventions have not been accounted for, they do provide useful estimates of the collective economic value of both health and cost consequences in a single figure.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
This simulation model used data from a variety of sources, all of which are referenced in the Supplementary Information.
Code availability
The model file is not available online; however, we welcome sharing of our models and methods with interested researchers who wish to collaborate with us. One of the reasons for a collaborative approach to sharing our models is the ability to provide training and support to users.
References
Meadows, G. N. et al. Resolving the paradox of increased mental health expenditure and stable prevalence. Aust. N. Z. J. Psychiatry 53, 844–850 (2019).
Budget 2021-22: Generational change and record investment in the health of Australians. Department of Health and Aged Care https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/budget-2021-22-generational-change-and-record-investment-in-the-health-of-australians (2021).
The National Children’s Mental Health and Wellbeing Strategy (National Mental Health Commission, 2021).
Cuijpers, P. Preventing the onset of depressive disorders: state of the art and future directions. Curr. Dir. Psychol. Sci. 34, 51–56 (2025).
GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2133–2161 (2024).
Wilkins, R., Vera-Toscano, E. & Botha, F. The Household, Income and Labour Dynamics in Australia Survey: Selected Findings from Waves 1 to 21 (Melbourne Institute: Applied Economic and Social Research, 2024).
Causes of death, Australia. Australian Bureau of Statistics https://www.abs.gov.au/statistics/health/causes-death/causes-death-australia/2023 (2024).
Biddle, N., Edwards, B. & Rehill, P. The Relationship between COVID-19 Policies and Subjective Wellbeing—August 2022 (The ANU Centre for Social Research and Methods, 2022).
Skinner, A., Occhipinti, J. A., Song, Y. J. C. & Hickie, I. B. Population mental health improves with increasing access to treatment: evidence from a dynamic modelling analysis. BMC Psychiatry 22, 692 (2022).
Haidt, J. The Anxious Generation: How the Great Rewiring of Childhood Is Causing an Epidemic of Mental Illness (Random House, 2024).
McGorry, P. D. et al. The Lancet Psychiatry Commission on youth mental health. Lancet Psychiatry 11, 731–774 (2024).
Patel, V. et al. The Lancet Commission on global mental health and sustainable development. Lancet 392, 1553–1598 (2018).
Scott, K. M. et al. Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry 73, 150–158 (2016).
Clark, C. et al. Impact of childhood and adulthood psychological health on labour force participation and exit in later life. Psychol. Med. 47, 1597–1608 (2017).
Santomauro, D. F., Purcell, C., Whiteford, H. A., Ferrari, A. J. & Vos, T. Grading disorder severity and averted burden by access to treatment within the GBD framework: a case study with anxiety disorders. Lancet Psychiatry 10, 272–281 (2023).
Lund, C. et al. Social determinants of mental disorders and the Sustainable Development Goals: a systematic review of reviews. Lancet Psychiatry 5, 357–369 (2018).
Occhipinti, J.-A. et al. The influence of economic policies on social environments and mental health. Bull. World Health Org. 102, 323–329 (2024).
Braveman, P. & Gottlieb, L. The social determinants of health: it’s time to consider the causes of the causes. Publ. Health Rep. 129, 19–31 (2014).
Occhipinti, J.-A. et al. Estimating the Mental Wealth of nations: valuing social production and investment. Nat. Ment. Health 1, 247–253 (2023).
Occhipinti, J. A. et al. Measuring, modeling, and forecasting the mental wealth of nations. Front. Publ. Health 10, 879183 (2022).
Bloom D. E. et al. The Global Economic Burden of Noncommunicable Diseases (World Economic Forum, 2011).
Roehrig, C. Mental disorders top the list of the most costly conditions in the United States: $201 billion. Health Aff. 35, 1130–1135 (2016).
Knapp, M. et al. Investing in recovery: making the business case for effective interventions for people with schizophrenia and psychosis. LSE Research Online Documents on Economics 56773 (London School of Economics and Political Science, LSE Library, 2014).
Mental Health (Productivity Commission, 2020); https://www.pc.gov.au/inquiries/completed/mental-health/report
Kularatna, S. et al. Cost-effectiveness analysis of paediatric mental health interventions: a systematic review of model-based economic evaluations. BMC Health Serv. Res. 22, 542 (2022).
McDaid, D., Park, A. L. & Wahlbeck, K. The economic case for the prevention of mental illness. Annu. Rev. Publ. Health 40, 373–389 (2019).
Le, L. K. et al. Cost-effectiveness evidence of mental health prevention and promotion interventions: a systematic review of economic evaluations. PLoS Med. 18, e1003606 (2021).
Feldman, I., Gebreslassie, M., Sampaio, F., Nystrand, C. & Ssegonja, R. Economic evaluations of public health interventions to improve mental health and prevent suicidal thoughts and behaviours: a systematic literature review. Adm. Policy Ment. Health 48, 299–315 (2021).
Knapp, M. & Wong, G. Economics and mental health: the current scenario. World Psychiatry 19, 3–14 (2020).
Lathe, J., Silverwood, R. J., Hughes, A. D. & Patalay, P. Examining how well economic evaluations capture the value of mental health. Lancet Psychiatry 11, 221–230 (2024).
Ha, N. T., Huong, N. T., Anh, V. N. & Anh, N. Q. Modelling in economic evaluation of mental health prevention: current status and quality of studies. BMC Health Serv. Res. 22, 906 (2022).
National Report Card 2023: Monitoring the Performance of Australia’s Mental Health System (National Mental Health Commission, 2024).
Rosenberg, S. & Salvador-Carulla, L. PERSPECTIVES: accountability for mental health: the Australian experience. J. Ment. Health Policy Econ. 20, 37–54 (2017).
Crosland, P. et al. Incorporating complexity and system dynamics into economic modelling for mental health policy and planning. Pharmacoeconomics 42, 1301–1315 (2024).
Allen, J., Balfour, R., Bell, R. & Marmot, M. Social determinants of mental health. Int. Rev. Psychiatry 26, 392–407 (2014).
Lund, C. Global mental health and its social determinants: how should we intervene?. Behav. Res. Ther. 169, 104402 (2023).
Kirkbride, J. B. et al. The social determinants of mental health and disorder: evidence, prevention and recommendations. World Psychiatry 23, 58 (2024).
Ridley, M., Rao, G., Schilbach, F. & Patel, V. Poverty, depression, and anxiety: causal evidence and mechanisms. Science 370, eaay0214 (2020).
Na, P. J. et al. Social determinants of health and suicide-related outcomes: a review of meta-analyses. JAMA Psychiatry 82, 337–346 (2025).
Guidance on Mental Health Policy and Strategic Action Plans (World Health Organization, 2025).
Littleton, C. & Reader, C. To what extent do Australian child and youth health, and education wellbeing policies, address the social determinants of health and health equity?: a policy analysis study. BMC Public Health 22, 2290 (2022).
Oswald, T. K. et al. Interventions targeting social determinants of mental disorders and the Sustainable Development Goals: a systematic review of reviews. Psychol. Med. 54, 1475–1499 (2024).
Occhipinti, J.-A. et al. Mental health: build predictive models to steer policy. Nature 597, 633–636 (2021).
Occhipinti, J. A. et al. Reducing youth suicide: systems modelling and simulation to guide targeted investments across the determinants. BMC Med. 19, 61 (2021).
Skinner, A., Osgood, N. D., Occhipinti, J.-A., Song, Y. J. C. & Hickie, I. B. Unemployment and underemployment are causes of suicide. Sci. Adv. 9, eadg3758 (2023).
Nordt, C., Warnke, I., Seifritz, E. & Kawohl, W. Modelling suicide and unemployment: a longitudinal analysis covering 63 countries, 2000–11. Lancet Psychiatry 2, 239–245 (2015).
Davies, C. et al. Prenatal and perinatal risk and protective factors for psychosis: a systematic review and meta-analysis. Lancet Psychiatry 7, 399–410 (2020).
Grummitt, L., Baldwin, J. R., Lafoa’i, J., Keyes, K. M. & Barrett, E. L. Burden of mental disorders and suicide attributable to childhood maltreatment. JAMA Psychiatry 81, 782–788 (2024).
Danese, A. & Widom, C. S. Associations between objective and subjective experiences of childhood maltreatment and the course of emotional disorders in adulthood. JAMA Psychiatry 80, 1009–1016 (2023).
Holt‐Lunstad, J. Social connection as a critical factor for mental and physical health: evidence, trends, challenges, and future implications. World Psychiatry 23, 312–332 (2024).
Breedvelt, J. J. F. et al. The effects of neighbourhood social cohesion on preventing depression and anxiety among adolescents and young adults: rapid review. BJPsych Open 8, e97 (2022).
Fone, D. et al. Does social cohesion modify the association between area income deprivation and mental health? A multilevel analysis. Int. J. Epidemiol. 36, 338–345 (2007).
Birrell, L., Werner-Seidler, A., Davidson, L., Andrews, J. L. & Slade, T. Social connection as a key target for youth mental health. Ment. Health Prev. 37, 200395 (2025).
Iorfino, F. et al. Multidimensional outcomes in youth mental health care: what matters and why? Med. J. Aust. 211, S4–S11 (2019).
Iorfino, F. et al. Patterns of emergency department presentations for a youth mental health cohort: data-linkage cohort study. BJPsych Open 9, e170 (2023).
Jonsson, B. Ten arguments for a societal perspective in the economic evaluation of medical innovations. Eur. J. Health Econ. 10, 357–359 (2009).
Neumann, P. J., Sanders, G. D., Russell, L. B., Siegel, J. E. & Ganiats, T. G. Cost-Effectiveness in Health and Medicine 2nd edn (Oxford Univ. Press, 2017).
Duevel, J. A. et al. Considering the societal perspective in economic evaluations: a systematic review in the case of depression. Health Econ. Rev. 10, 32 (2020).
Husereau, D. et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Int. J. Technol. Assess. Health Care 38, e13 (2022).
Occhipinti, J. A. et al. Which social, economic, and health sector strategies will deliver the greatest impacts for youth mental health and suicide prevention? protocol for an advanced, systems modelling approach. Front. Psychiatry 12, 759343 (2021).
Lawson, K. D. et al. A dynamic approach to economic priority setting to invest in youth mental health and guide local implementation: economic protocol for eight system dynamics policy models. Front. Psychiatry 13, 835201 (2022).
Freebairn, L. et al. Participatory methods for systems modeling of youth mental health: implementation protocol. JMIR Res. Protoc. 11, e32988 (2022).
Powell, M. The BOBYQA Algorithm for Bound Constrained Optimization Without Derivatives: Technical Report (Department of Applied Mathematics and Theoretical Physics, Univ. Cambridge, 2009).
Kessler, R. C. et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 32, 959–976 (2002).
Gamst-Klaussen, T., Lamu, A. N., Chen, G. & Olsen, J. A. Assessment of outcome measures for cost-utility analysis in depression: mapping depression scales onto the EQ-5D-5L. BJPsych Open 4, 160–166 (2018).
McCaffrey, N., Kaambwa, B., Currow, D. C. & Ratcliffe, J. Health-related quality of life measured using the EQ-5D-5L: South Australian population norms. Health Qual. Life Outcomes 14, 133 (2016).
Goodman, A. & Goodman, R. Strengths and Difficulties Questionnaire as a dimensional measure of child mental health. J. Am. Acad. Child Adolesc. Psychiatry 48, 400–403 (2009).
Sharma, R., Gu, Y., Sinha, K., Aghdaee, M. & Parkinson, B. Mapping the Strengths and Difficulties questionnaire onto the child health utility 9D in a large study of children. Qual. Life Res. 28, 2429–2441 (2019).
O’Loughlin, R. et al. Comparing the psychometric performance of generic paediatric health-related quality of life instruments in children and adolescents with ADHD, anxiety and/or depression. Pharmacoeconomics 42, 57–77 (2024).
Jones, R. et al. Comparative psychometric performance of common generic paediatric health-related quality of life instrument descriptive systems: results from the Australian paediatric multi-instrument comparison study. Pharmacoeconomics 42, 39–55 (2024).
Oliveira Goncalves, A. S., Werdin, S., Kurth, T. & Panteli, D. Mapping studies to estimate health-state utilities from nonpreference-based outcome measures: a systematic review on how repeated measurements are taken into account. Value Health 26, 589–597 (2023).
Guidelines for Preparing a Submission to the Pharmaceutical Benefits Advisory Committee Version 5.0 (Pharmaceutical Benefits Advisory Committee, 2016).
Shiroiwa, T. et al. International survey on willingness-to-pay (WTP) for one additional QALY gained: what is the threshold of cost effectiveness? Health Econ. 19, 422–437 (2010).
Vallejo-Torres, L. et al. On the estimation of the cost-effectiveness threshold: why, what, how? Value Health 19, 558–566 (2016).
O’Donnell, J. Mapping Social Cohesion 2023 (Scanlon Foundation Research Institute, 2023).
Markus, A. & Arnup, J. Mapping Social Cohesion 2009—The Scan Foundation Surveys (Monash Univ., 2010).
Growing up in Australia—The Longitudinal Study of Australian Children—data and documentation. The Australian Institute of Family Studies https://growingupinaustralia.gov.au/data-and-documentation (2018).
Growing up in Australia: Longitudinal Study of Australian Children (LSAC) Release 9.1 C2 (Waves 1-9C) [ADA Dataverse]. The Australian Institute of Family Studies https://growingupinaustralia.gov.au/(2022).
Homelessness operational groups (OPGP). Australian Bureau of Statistics https://www.abs.gov.au/census/guide-census-data/census-dictionary/2021/variables-topic/housing/homelessness-operational-groups-opgp (2021).
Estimating homelessness: census. Australian Bureau of Statistics https://www.abs.gov.au/statistics/people/housing/estimating-homelessness-census (2021).
Labour force, Australia, detailed. Australian Bureau of Statistics https://www.abs.gov.au/statistics/labour/employment-and-unemployment/labour-force-australia-detailed/ (2023).
Labour force, Australia. Australian Bureau of Statistics https://www.abs.gov.au/statistics/labour/employment-and-unemployment/labour-force-australia/ (2023).
Education and work [Tablebuilder]. Australian Bureau of Statistics https://www.abs.gov.au/statistics/microdata-tablebuilder/tablebuilder (2014–2022).
Enrolments by Grade 2008 to 2021 (Australian Curriculum Assessment and Reporting Authority, 2021).
Education and Work, Australia (Reference Period: May 2021) (Australian Bureau of Statistics, 2021).
National study of mental health and wellbeing. Australian Bureau of Statistics https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/2020-2022 (2022).
National Survey of Mental Health and Wellbeing: summary of results, 2007. Australian Bureau of Statistics https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/2007 (2008).
Goodhue, R., Dakin, P. & Noble, K. What’s in the nest? Exploring Australia’s wellbeing framework for children and young people. Canberra ARACY https://ihcsupportagency.org.au/wp-content/uploads/2021/09/WhatsInTheNest2021_EVersion.pdf(2021).
Hogan, M., Hatfield-Dodds, L., Barnes, L. & Struthers, K. Systems Leadership for Child Wellbeing Project: Stage 1 Synthesis Report (Every Child and Australia and New Zealand School of Government (ANZSOG), Australia, 2021).
Veronese, N. et al. Interventions for reducing loneliness: an umbrella review of intervention studies. Health Social Care Commun. 29, e89–e96 (2021).
Li, N., Peng, J. & Li, Y. Effects and moderators of Triple P on the social, emotional, and behavioral problems of children: systematic review and meta-analysis. Front. Psychol. 12, 709851 (2021).
Sampaio, F. et al. Population cost-effectiveness of the Triple P parenting programme for the treatment of conduct disorder: an economic modelling study. Eur. Child Adolesc. Psychiatry 27, 933–944 (2018).
Crosland, P. et al. Cost-effectiveness of system-level mental health strategies for young people in the Australian Capital Territory: a dynamic simulation modelling study. Lancet Psychiatry 11, 123–133 (2024).
Loblay, V. et al. Enhancing equitable engagement for digital health promotion: Lessons from evaluating a childrearing app in Indonesia. Digit. Health 9, 20552076231222112 (2023).
LaMonica, H. M. et al. Developing a parenting app to support young children’s socioemotional and cognitive development in culturally diverse low- and middle-income countries: protocol for a co-design study. JMIR Res. Protoc. 11, e39225 (2022).
Walsh, E. H., McMahon, J. & Herring, M. P. Research review: the effect of school-based suicide prevention on suicidal ideation and suicide attempts and the role of intervention and contextual factors among adolescents: a meta-analysis and meta-regression. J. Child Psychol. Psychiatry 63, 836–845 (2022).
Walsh, E. H., Herring, M. P. & McMahon, J. A systematic review of school-based suicide prevention interventions for adolescents, and intervention and contextual factors in prevention. Prev. Sci. 24, 365–381 (2023).
Breet, E., Matooane, M., Tomlinson, M. & Bantjes, J. Systematic review and narrative synthesis of suicide prevention in high-schools and universities: a research agenda for evidence-based practice. BMC Public Health 21, 1116 (2021).
Dunning, D. et al. Do mindfulness-based programmes improve the cognitive skills, behaviour and mental health of children and adolescents? An updated meta-analysis of randomised controlled trials. Evid. Based Ment. Health 25, 135–142 (2022).
Caldwell, D. M. et al. School-based interventions to prevent anxiety and depression in children and young people: a systematic review and network meta-analysis. Lancet Psychiatry 6, 1011–1020 (2019).
Werner-Seidler, A. et al. School-based depression and anxiety prevention programs: an updated systematic review and meta-analysis. Clin. Psychol. Rev. 89, 102079 (2021).
Gunawardena, H., Voukelatos, A., Nair, S., Cross, S. & Hickie, I. B. Efficacy and effectiveness of universal school-based wellbeing interventions in australia: a systematic review. Int. J. Environ. Res. Public Health 20, 6508 (2023).
Schmidt, M. et al. Universal mental health interventions for children and adolescents: a systematic review of health economic evaluations. Appl. Health Econ. Health Policy 18, 155–175 (2020).
Foulkes, L. & Stringaris, A. Do no harm: can school mental health interventions cause iatrogenic harm? BJPsych Bull 47, 267–269 (2023).
Frederick, D. E. & VanderWeele, T. J. Supported employment: meta-analysis and review of randomized controlled trials of individual placement and support. PLoS ONE 14, e0212208 (2019).
Brinchmann, B. et al. A meta-regression of the impact of policy on the efficacy of individual placement and support. Acta Psychiatr. Scand. 141, 206–220 (2020).
Bond, G. R. Cost-Effectiveness of Individual Placement and Support (Advancing State Policy Integration for Recovery and Employment, 2023).
Zheng, K., Stern, B. Z., Wafford, Q. E. & Kohli-Lynch, C. N. Trial-based economic evaluations of supported employment for adults with severe mental illness: a systematic review. Adm. Policy Ment. Health 49, 440–452 (2022).
Thomson, R. M. et al. How do income changes impact on mental health and wellbeing for working-age adults? A systematic review and meta-analysis. Lancet Public Health 7, e515–e528 (2022).
Acknowledgements
We acknowledge the attendees of the participatory systems modeling workshops who provided vital skills and expertise, particularly young people with a lived experience of mental health conditions and their carers. We acknowledge the staff of the Statistical Services Branch, Queensland Health, the Healthcare Improvement Unit, Queensland Health and the Mental Health Alcohol and Other Drugs Branch, Queensland Health for the datasets used for this project: the Emergency Data Collection, the Queensland Hospital Admitted Patient Data Collection and the Consumer Integrated Mental Health Application. We acknowledge the staff of the Australian Curriculum, Assessment and Reporting Authority for providing Student Enrolment and Senior Secondary Outcomes data, and the staff of Brisbane South Primary Health Network for providing headspace occasions of service data. This Analysis uses unit record data from Growing Up in Australia, the Longitudinal Study of Australian Children. The study is conducted in partnership between the Department of Social Services (DSS), the Australian Institute of Family Studies (AIFS) and the Australian Bureau of Statistics (ABS). The findings and views reported in this Analysis are those of the authors and should not be attributed to DSS, AIFS or the ABS. I.B.H. discloses support for the research of this work from NHMRC (APP2016346). D.A.M. discloses partial salary support for the research of this work from the Svare Chair in Health Economics, Value and Impact.
Funding
Open access funding provided by the University of Sydney
Author information
Authors and Affiliations
Contributions
P.C.: conceptualization, methodology, software, formal analysis, investigation, writing—original draft, writing for Box 3, visualization. N.H.: methodology, software, formal analysis, investigation, data curation, writing—review and editing. K.-H.N.: validation, writing—review and editing, investigation. K.T.: validation, writing—review and editing, investigation, data curation. S.H.H.: methodology, software, data curation, writing—review and editing. C.V.: methodology, software, investigation, writing—review and editing. AS: writing—review and editing, supervision. J.v.R.: writing for Box 1, writing—review and editing. S.R.: writing—review and editing. F.I.: writing—review and editing. V.L.: writing—review and editing. O.I.: investigation, writing—review and editing. S.P.: writing—review and editing. Y.J.C.S.: conceptualization, supervision, project administration, funding acquisition and resources. S.M.: writing for Box 2, writing—review and editing. J.M.G.P.: writing—review and editing. A.C.: writing—review and editing. D.A.M.: writing—review and editing, supervision. I.B.H.: conceptualization, writing—review and editing, supervision, funding acquisition. J.-A.O.: conceptualization, resources, supervision, project administration, funding acquisition, writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
This study was conducted under the Right care, first time, where you live Program (Brain and Mind Centre, University of Sydney), supported by a AUD$12.8 million grant provided by the BHP Foundation. The program is developing decision support infrastructure to guide investments and actions to foster the mental health and well-being of young people in their communities. J.-A.O. is both Head of Systems Modelling, Simulation & Data Science at the University of Sydney’s Brain and Mind Centre and Managing Director of Computer Simulation & Advanced Research Technologies (CSART). I.H. is the Co-Director, Health and Policy at the Brain and Mind Centre (BMC) University of Sydney. The BMC operates an early-intervention youth services at Camperdown under contract to headspace. He is the Chief Scientific Advisor to, and a 3.2% equity shareholder in, InnoWell Pty Ltd, which aims to transform mental health services through the use of innovative technologies. V.L. is a board member for Matana Foundation, a philanthropic organization that provides funding to programs for disadvantaged young people. She does not receive any financial benefit for this role.
Peer review
Peer review information
Nature Mental Health thanks Laura Shields-Zeeman and the other, anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Information part A with Supplementary Figs. 1–22; Supplementary Information part B with Supplementary Figs. 1–8 and Supplementary Tables 1–9.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Crosland, P., Ho, N., Nguyen, KH. et al. Modeled estimates of the health outcomes and economic value of improving the social determinants of mental health. Nat. Mental Health 3, 943–956 (2025). https://doi.org/10.1038/s44220-025-00459-7
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44220-025-00459-7