Abstract
Postpartum depression and mother-to-infant bonding difficulties (MIBD), two issues crucial to maternal and infant mental health, often coexist and affect each other. Our study aims to dissect their complex relationship through a graphical LASSO network analysis of individual symptoms in 5594 Japanese postpartum women, whose geographical distribution was nationally representative. We identified ‘fear’, ‘enjoyment’, ‘overwhelm’, and ‘insomnia’ as common bridge symptoms linking postpartum depression and MIBD across three distinct postpartum periods. Moreover, ‘self-harm’ emerged as a bridge symptom in the first 6 months and the 7–12 month period, while ‘laugh’ was a bridge symptom in the first 6 months and the 13–24 month period. Notably, ‘self-blame’ was identified as a unique bridge symptom specific to the 13–24 month period. Our analysis highlights the complexities of symptom connectivity across postpartum stages and underscores the critical need for interventions that address both common and stage-specific bridge symptoms to effectively support maternal mental health and strengthen mother-to-infant bonding.
Similar content being viewed by others
Introduction
The periods following childbirth are critical for both maternal and infant mental health, with postpartum depression and mother-to-infant bonding difficulties (MIBD) having been recognized as two major challenges1,2. Postpartum depression, characterized by deep sadness, anhedonia, and anxiety, affects 14–18% of women3,4,5, a figure that rose to 27–34% during the COVID-19 pandemic6,7,8. MIBD, which includes symptoms such as a lack of affection or the presence of feelings of anger towards the infant, similarly affects 11–14% of women9,10, with rates increasing to as high as 27% during the pandemic11. The high prevalence of these issues highlights a considerable public health concern due to their influences on family dynamics, child development, and maternal well-being12,13,14,15.
The situation is further complicated by the frequent coexistence of the two conditions. Studies indicated that 54–57% of women with symptoms of postpartum depression also experience MIBD11,16, while 28–40% of those with MIBD have postpartum depression9,11. This significant overlap is also highlighted by cross-sectional correlation coefficients ranging between 0.27 and 0.47 across different postpartum stages, as revealed by a recent meta-analysis of 85 studies using continuous measures of the two conditions17. In some cases, individual studies have reported correlation coefficients as high as 0.7618. These findings have spurred investigations into the underlying mechanisms of their coexistence.
Emerging evidence points to shared risk factors between postpartum depression and MIBD, including insufficient partner and family support11,19, prenatal depression19,20, and adverse childhood experiences21. Additionally, longitudinal studies have identified both a temporal link from postpartum depression to MIBD22,23,24 and a chronological connection from MIBD to postpartum depression25,26. This interconnectedness is further supported by evidence showing that interventions aimed at reducing postpartum depression can improve mother-to-infant bonding27, and vice versa, interventions targeting mother-infant interactions can mitigate postpartum depression28,29.
This growing body of evidence reinforces the intricate connection between postpartum depression and MIBD, highlighting the need for an integrated approach to understanding and intervention. In response to this imperative, the current study employs a network analysis approach30,31,32,33. Network analysis allows for the examination of the complex relationships between comorbid conditions at the individual symptom level. By transcending traditional views of mental disorders as isolated entities explained by underlying latent variables, network analysis reveals the dynamic interplay of interrelated symptom networks. Specifically, this methodological shift emphasizes the identification of ‘bridge symptoms’ that serve as crucial links between two comorbid conditions, thus pointing to potential focal points for intervention30,33. These insights allow for the precise targeting of symptoms that are central to the nexus of these conditions, which enables more strategic and effective therapeutic interventions.
This study aims to map out the intricate connections between symptoms of postpartum depression and MIBD through network analysis using data of 5594 Japanese postpartum women within two years since childbirth. Notably, the sample’s geographical distribution spanned all 47 prefectures in Japan, ensuring a demographic representation that reflects the national female population (Supplementary Fig. 1). By identifying bridge symptoms within these conditions, we seek to provide a deeper understanding of the relationship between these phenomena and offer actionable insights for targeted interventions and more effective strategies for addressing the challenges of postpartum mental health.
Methods
Participants
We utilized data from the Japan COVID-19 and Society Internet Survey (JACSIS), a Japanese nationwide survey conducted in July and August 2021. Our analysis focused specifically on data collected from the pregnant/postpartum mother panel21,24, which ultimately included 5594 postpartum women within two years since childbirth. In brief, an initial screening survey was distributed to 440,323 panelists of a leading Japanese market research company, Rakuten Insight, Inc., to identify pregnant or postpartum women and their partners. The criteria for eligibility included women who or men whose partners were expected to give birth by December 2021 or had delivered after July 2019. A total of 14,086 pregnant or postpartum women and 3436 partners met the criteria and received an invitation to participate between July 28 and August 30, 2021. Due to budget and time constraints, data collection was concluded at the first 10,000 respondents, including 6256 postpartum women. Of these postpartum women, 568 were excluded due to responses flagged as inconsistent or unnatural by a predefined exclusion algorithm developed by JACSIS24,25. Specifically, this algorithm included an attention check (i.e., “Please choose the second option from the bottom of the following”) and flagged straight-lining responses, where participants either answered uniformly to all nine substance use queries or to all sixteen comorbidity items. Among the remaining postpartum women, 5594 had given birth within the past two years. Participants were compensated for their involvement in the study with credit points (“Epoints”) upon completing the questionnaire. All participants provided informed consent and the study’s protocol received approval from the Research Ethics Committee of the Osaka International Cancer Institute. The study was not preregistered.
The socio-demographic characteristics of the participants are shown in Table 1. The average age of participants was 32.2 ± 4.4 (standard deviation, SD) years and 98.6% were married. Participants were grouped into three postpartum periods: 1832 (32.7%) were within six months postpartum, 2045 (36.6%) were 7–12 months postpartum, and 1717 (30.7%) were 13–24 months postpartum. The youngest group was within 6 months postpartum, and the oldest group ranged from 13 to 24 months postpartum, with the age difference being about one year. Marital status varied slightly, with 0.9% more participants in the 7–12 months group being married compared to the 13–24 months group.
Regarding postpartum depression and bonding, participants within the first 6 months postpartum had the lowest scores on the Edinburgh Postnatal Depression Scale (EPDS, 5.18 ± 4.58) and Mother-to-Infant Bonding Scale (MIBS, 2.26 ± 3.06, both p < 0.05 after Bonferroni correction, Kruskal–Wallis test). Additionally, this group had the smallest proportion of individuals exceeding the established cutoff points for postpartum depression (19.1%) or MIBD (14.4%, both p < 0.05 after Bonferroni correction, Chi-square test). Conversely, those in the 13–24 month postpartum category demonstrated the highest scores on both scales (6.64 ± 5.29 and 3.80 ± 3.90, respectively, both p < 0.05 after Bonferroni correction, Kruskal–Wallis test), along with the greatest proportion of participants surpassing the cutoff values (28.7% and 29.2%, respectively, both p < 0.05 after Bonferroni correction, Chi-square test). No significant differences were observed across the three groups concerning other characteristics. The EPDS scores showed a significant correlation with the MIBS scores for the entire dataset (rho = 0.470, 95% confidence interval [0.447, 0.493], p < 0.001) and across various postpartum periods (rho = 0.460, 95% confidence interval [0.422, 0.501] for the first 6 months, rho = 0.451, 95% confidence interval [0.414, 0.492] for 7–12 months, rho = 0.465, 95% confidence interval [0.423, 0.503] for 13–24 months, all p < 0.001).
The rationale for dividing the sample into three postpartum periods—the first 6 months, 7–12 months, and 13–24 months—is based on the infant’s developmental stages, established mental health service guidelines, and changes in the mother’s life circumstances. The first 6 months marks the early stages of child-rearing, which is characterized by limited infant mobility and communication. It aligns with the World Health Organization’s (WHO) recommendation for exclusive breastfeeding and is commonly defined as the “postpartum” period34. During the 7–12 months, infants exhibit increased mobility, such as sitting up and crawling, and begin understanding simple words and imitating others35. In Japan, this period is considered part of the postpartum phase, with governmental mental health services supporting mothers throughout the first year36, which coincides with the official maternity leave period as defined by Japanese law. However, research shows that postpartum mental health challenges can extend well beyond the first year, with many studies examining maternal mental health up to two years postpartum37. During the period from 13 to 24 months, infants typically start walking, develop fine motor skills, and show heightened curiosity and independence35. They also begin speaking a few words, engage in more complex interactions with their mothers, and often express a desire to do things independently. This increased communication and independence can further influence the maternal experience. In addition, as infants grow, particularly after turning one year old—the official end of the maternity leave period in Japan—many mothers return to work, adding the challenge of balancing professional responsibilities with family care. Therefore, our decision to separate the postpartum periods is grounded in the infant’s developmental stages, evolving life circumstances, and the framework of mental health services.
Postpartum depression and MIBD
We measured the incidence of postpartum depression symptoms within the last week using the Edinburgh Postnatal Depression Scale (EPDS)38,39. The EPDS demonstrated robust reliability in our study, evidenced by a Cronbach’s alpha coefficient of 0.848. In studies involving Japanese participants, achieving a score of 9 or above is frequently interpreted as a sign of postpartum depression39,40. The possible score range on the EPDS is from 0 to 30.
To assess the mother-infant bonding quality, we utilized the Mother-to-Infant Bonding Scale (MIBS)41,42. In our analysis, the MIBS demonstrated robust reliability, with a Cronbach’s alpha coefficient of 0.819. Research with Japanese participants often suggests that scores of 5 or higher are commonly seen as indicative of challenges in forming MIB10,43. The possible score range on the MIBS is from 0 to 30.
Statistical analysis
To construct and visualize the symptom network, we employed the qgraph (Version 1.6.5)44 and bootnet (Version 1.4.3)45 packages in R. The network’s structure was identified using the graphical Least Absolute Shrinkage and Selection Operator (LASSO) technique46, which is designed to estimate a sparsely connected network through regularized partial correlations. Model selection was guided by the Extended Bayesian Information Criterion (EBIC)47.
Visualization of the network was achieved using the Fruchterman-Reingold algorithm45, which organizes symptoms (i.e., called nodes) such that those with stronger and more frequent connections (called edges) are positioned closer to each other, thus indicating their concentration within the network. The strength of a connection is depicted by the thickness of its edge, while its directionality (positive or negative associations) is indicated by color coding (e.g., green for positive, red for negative associations). The mgm package48 was utilized to estimate node predictability or the proportion of variance in a node accounted for by its connections to other nodes in the network. This predictability was visually represented through ring-shaped pie charts.
We calculated four key centrality measures to determine the significance of each symptom within the network: strength, expected influence, betweenness, and closeness33. The strength of a node is quantified by aggregating the absolute values of edge weights linked to it, reflecting its total level of connectivity. Expected influence sums the edge weights while incorporating their direction, which offers insight into the node’s overall positive connectivity within the network. Betweenness evaluates a node’s intermediary function and is defined by its frequency of occurrence on the shortest paths connecting any two other nodes. Closeness measures the average shortest distance of a node to all other nodes, indicating its accessibility within the network. Furthermore, we extended these centrality metrics to analyze bridge networks, identifying connections that span the divide between symptoms of postpartum depression and MIBD. In this context, bridge strength, bridge expected influence, bridge betweenness, and bridge closeness were computed to illuminate how certain symptoms act as pivotal links between these two conditions.
To enhance the robustness and reliability of our network analysis, the precision of edge weights and the stability of the centrality measures were assessed using the bootnet package45. Firstly, the precision of edge weights was determined by calculating confidence intervals through non-parametric bootstrapping techniques. Following previous studies45, the number of bootstraps was set to 2500. This approach allowed us to evaluate the reliability of the connections between symptoms within the network by providing a range within which the true value of edge weights is likely to fall. Secondly, the stability of the centrality measures was evaluated using the correlation stability coefficient (CS-C). This metric offers a quantitative measure of how stable the centrality indices remain when subsets of the data are considered, with values exceeding 0.5 denoting a level of robust stability45.
Based on the centrality metric deemed most dependable in this analysis—specifically, bridge expected influence, as detailed in our results—we identified the top bridge symptoms within the network. Here, for the definition of bridge symptoms, previous studies have employed a threshold method, in which the top three symptoms with the highest centrality measures49,50 or the symptoms scoring above the 80th percentile in centrality measures33 are selected. However, this threshold method is arbitrary and may not adequately distinguish between symptoms with very similar centrality values (e.g., the fourth-ranked symptom might be nearly identical to the third).
To address this issue, we employed an alternative method for identifying bridge symptoms: clustering. Specifically, we utilized k-means clustering, an unsupervised machine learning algorithm that partitions data into a predefined number of clusters based on feature similarity. In our case, we set the number of clusters to k = 2 in order to separate symptoms into two distinct groups—those with higher and lower bridge expected influence values. The k-means algorithm works by initializing cluster centers (centroids) and then iteratively updating them to minimize the within-cluster sum of squared distances (variance). We used MATLAB R2022b’s k-means clustering function, which employs the squared Euclidean distance as the metric for calculating the distance between data points and cluster centers. Additionally, we utilized the k-means++ initialization method51, which selects initial cluster centers in a way that speeds up convergence and improves clustering performance.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Network accuracy
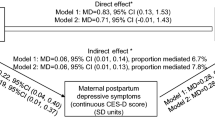
The network’s accuracy is assessed using two metrics: accuracy of edge weights and stability of centrality measures. Regarding the accuracy of edge weights, Fig. 1 (left panel) displays bootstrapped confidence intervals (CIs) for the entire dataset while Supplementary Fig. 2 (upper panels) show those of separate postpartum periods. These visualizations reveal that the estimated strengths—represented as sample values—and the bootstrapped means closely align for each edge, accompanied by narrowly defined bootstrapped CIs. These findings suggest a high level of accuracy in the estimated edge weights within our network.
Left panel: The precision of edge weight estimations using non-parametric bootstrapping to calculate confidence intervals. Sample values are depicted by red lines, whereas the bootstrapped averages are indicated by a black line. The gray shaded regions represent the confidence intervals derived from bootstrapping. The graphs are organized vertically by the y-axis, which orders network edges by their weight, from highest to lowest. Right panel: The stability of centrality statistics estimated through a case-dropping subset bootstrap method. On the x-axis, the graph displays the proportion of the original dataset utilized at each iteration. The y-axis shows the mean correlation values between centrality measures calculated from the original network and those derived from networks re-estimated after sequentially omitting varying percentages of the dataset. n = 5594 participants.
Among the four centrality statistics, the correlation-stability coefficients (CS-C) of bridge strength and bridge expected influence were consistently above 0.5, a common threshold for the CS-C indicating robust stability45, for both the entire dataset (Fig. 1, right panel) and those of separate postpartum periods (Supplementary Fig. 2, lower panels). For instance, the mean CS-C values of bridge strength and bridge expected influence were both 0.75 for the entire dataset, indicating that 75% of the sample could be dropped without significant changes in the network structure. The mean CS-C values of bridge strength and bridge expected influence were both 0.672 for all three postpartum periods, indicating that 67.2% of the sample could be dropped without significant changes in the network structure. Given that bridge expected influence demonstrated the strongest average correlation with the initial dataset with narrow confidence intervals, as shown in Fig. 1 & Supplementary Fig. 2 (lower panels), we selected this metric for identifying bridge symptoms.
Specifically, expected influence measures a node’s overall connectivity within the network, considering both positive and negative relationships. Unlike the traditional centrality measure of strength, which sums the absolute values of all connections, expected influence accounts for the direction of these connections. This provides a more precise measure of a symptom’s influence by distinguishing between connections that contribute to symptom activation (positive influence, e.g., self-blame increasing fear) and those that contribute to symptom reduction (negative influence, e.g., indifference mitigating anxiety).
Bridge expected influence specifically quantifies a node’s aggregate connectivity to nodes associated with the other condition. Similar to expected influence, bridge expected influence sums the weights of edges but focuses only on edges that link nodes across different conditions (here, postpartum depression versus MIBD). Thus, this metric identifies “bridges” symptoms that facilitate interactions between these different conditions. Bridge symptoms are crucial as they can transmit activation or suppression between conditions, and thus play a key role in symptom co-occurrence and maintenance.
Network for the entire dataset
We first estimated the network structure for the full dataset. The mean predictability score for all symptoms was 0.411, indicating that, on average, 41.1% of the variance in each symptom could be explained through its interconnections with other symptoms in the network. Figure 2 displays the network structure showing bridge connections between symptoms of postpartum depression and MIBD.
Left panel: Nodes within the network are depicted using ring-shaped pie charts to denote predictability; a fully filled color ring signifies that a symptom’s variance is wholly explained by its interrelations within the network. Symptoms serving as bridges are identified in yellow, setting them apart from the other symptoms related to postpartum depression and mother-to-infant bonding, which are colored red and blue, respectively. Connections indicating positive correlations are represented by dark green lines, whereas negative correlations are shown with red lines. The thickness of these lines indicates the strength of the relationships between symptoms. Right panel: The bridge expected influence scores for each symptom are plotted. Symptoms with values above 0.15 fell into a single cluster (colored in orange) in the k-means clustering and are considered bridge symptoms. n = 5594 participants.
To define bridge symptoms, we employed a clustering method using the k-means algorithm. We partitioned the bridge expected influence values into two clusters and considered symptoms within the cluster with higher values as bridge symptoms. As a result, symptoms with bridge expected influence values above 0.15 fell into this higher cluster (Fig. 2, right panel) and were considered bridge symptoms. These bridge symptoms, listed in decreasing order of their bridge expected influence values, included:
-
‘fear’ (MIBS2): “Feel scared or panicky when I have to do something for my baby”
-
‘enjoyment’ (MIBS6): “Enjoy doing things with my baby”
-
‘self-harm’ (EPDS10): “The thought of harming myself has occurred to me”
-
‘insomnia’ (EPDS7): “I have been so unhappy that I have had difficulty sleeping”
-
‘laugh’ (EPDS1): “I have been able to laugh and see the funny side of things” (indicative of anhedonia)
-
‘overwhelm’ (EPDS6): “Things have been getting on top of me”
Network for specific postpartum periods
We then estimated the network structure for different postpartum periods. The average predictability of all symptoms was recorded at 0.388, 0.409, and 0.428 for the three distinct postpartum periods, respectively. This suggests that 38.8–42.8% of the variability in each symptom can be accounted for by its connections to other symptoms within the network across different postpartum intervals.
Based on clustering analysis, symptoms with bridge expected influence values above 0.14 consistently fell into this higher cluster across all three postpartum periods (Fig. 3, lower panel) and were considered bridge symptoms. As illustrated in Fig. 3 and Table 2, four symptoms consistently acted as bridge symptoms throughout all postpartum stages: ‘fear’ (MIBS2), ‘enjoyment’ (MIBS6), ‘overwhelm’ (EPDS6), and ‘insomnia’ (EPDS7). Moreover, ‘self-harm’ (EPDS10) was identified as a bridge symptom during the first 6 months and the 7–12 month period, while ‘laugh’ (EPDS1, indicative of anhedonia) emerged as a bridge symptom in the first 6 months and the 13–24 month period. In contrast, ‘self-blame’ (EPDS3, “I have blamed myself unnecessarily when things went wrong”) was a unique bridge symptom only in the 13–24 month period.
Upper left panel: within 6 postpartum months (n = 1832 participants). Upper middle panel: postpartum months from 7 to 12 (n = 2045 participants). Upper right panel: postpartum months from 13 to 24 (n = 1717 participants). To facilitate comparison of bridge symptoms across different postpartum periods, we have fixed the spatial positions of nodes based on the full dataset. Nodes within the network are depicted using ring-shaped pie charts to denote predictability. Symptoms serving as bridges are identified in yellow, setting them apart from the other symptoms related to postpartum depression and mother-to-infant bonding, which are colored red and blue, respectively. Connections indicating positive correlations are represented by dark green lines, whereas negative correlations are shown with red lines. The thickness of these lines indicates the strength of the relationships between symptoms. Lower panels: the bridge expected influence scores for each symptom across different postpartum periods. Symptoms with values above 0.14 fell into a single cluster (colored in orange) in the k-means clustering and are considered bridge symptoms.
Discussion
In the present study, we conducted a network analysis to explore the intricate relationship between postpartum depression and MIBD. Our findings underscore the complexity of postpartum depression and MIBD and shed light on both common and period-specific symptoms across various stages after childbirth.
Central to our analysis was the identification of fear, enjoyment, overwhelm, and insomnia as common bridge symptoms linking postpartum depression and MIBD. Fear, a symptom characterized by feeling scared or panicky about performing tasks for one’s infant, stands out as the strongest bridge symptom. It may be a direct reflection of parenting stress, particularly in terms of anxiety about adequately caring for and protecting the infant. This fear may stem from a lack of confidence in parenting abilities, concerns over the infant’s well-being, or the overwhelming responsibility of caring for a dependent child52. On the other hand, enjoyment in parenting tasks is generally seen as a protective factor against parenting stress, which suggests a positive adaptation to the parenting role and a healthy emotional connection with the infant53. A lack of enjoyment can signal difficulties in bonding with the infant, which contributes to increased parenting stress53 and depressive symptoms25. Moreover, the recognition of overwhelm as a common bridge symptom illuminates the overwhelming nature of new motherhood. This transition is marked by a confluence of external pressures, internal expectations, and sudden lifestyle changes following childbirth54,55. These findings speak to the critical need for supportive interventions that not only address emotional regulation and stress management but also provide practical support and guidance to navigate the complexities of caring for a newborn28,56,57. The pivotal role of insomnia is supported by a recent report that identified a direct correlation between maternal insomnia and later worsened mother-to-infant bonding58. Addressing these bridge symptoms could therefore offer a strategic point for integrated interventions aimed at mitigating the dual challenges of depression and impaired bonding at various postpartum stages.
We also identified self-harm as a bridge symptom during the first 6 months and the 7–12 months postpartum period. Thoughts of self-harm can provoke feelings of anger and indifference towards the infant59, due to heightened parenting stress and compromised ability to regulate negative emotions60. Additionally, mothers with thoughts of self-harm may exhibit passive or hopeless responses to the infant’s needs61. Conversely, thoughts of self-harm may also serve as a mediator in the causal relationship between bonding difficulties and the wider spectrum of depressive symptoms. Women experiencing intense anger or apathy towards their infant may feel overwhelmed by their emotional responses, which can lead to a sense of isolation, guilt, and shame and increase the risk of self-harm as a maladaptive coping mechanism61,62. In light of these considerations, there is an urgent need for targeted interventions that address both self-harm ideation and the emotional disconnect between mother and infant at these early stages.
Laugh emerged as a bridge symptom in the first 6 months and the 13–24 months period. Given that items representing positive sentiments were reverse-coded, laugh in this context denotes an inability to experience pleasure, or anhedonia, which is a hallmark of depressive symptoms. This lack of positive emotional engagement poses a significant barrier to mother-infant bonding and suggests that depressive symptoms remain a critical concern well beyond the initial postpartum period. Addressing anhedonia through therapeutic strategies that promote positive affect and engagement is essential for enhancing maternal mental health and bonding.
Lastly, self-blame occurred as a unique bridge symptom during the 13–24 months period. A core component of the cognitive theory of depression63, self-blame reflects internalized negative beliefs about oneself (e.g., one’s parenting abilities) and is associated with feelings of guilt and inadequacy. The prominence of self-blame in the second year postpartum suggests that maternal mental health challenges not only persist but may evolve or intensify, underscoring the need for ongoing psychological support that addresses cognitive distortions and promotes self-compassion.
Our findings stress the long-term nature of some postpartum mental health challenges and the necessity for interventions that promote joy, engagement, and connection, even well beyond the immediate postpartum period. It also calls into question the existing guidelines, both nationally in Japan36 and internationally34, which recommend monitoring postpartum mental health only within the first six months to one year after childbirth. This comprehensive approach of our study, which considers the common, period-specific, and interconnected nature of symptoms, affirms the complexity of the two conditions. The identification of period-specific bridge symptoms emphasizes the importance of temporal context in tailoring interventions.
Limitations
While our study offers important insights, it is not without limitations. The cross-sectional design limits our ability to infer causality between symptoms of postpartum depression and MIBD. Additionally, although we identified network differences related to the postpartum period, our findings do not capture changes over time. Future research should consider longitudinal designs to elucidate the causal relationships between symptoms and explore how the network evolves during different postpartum periods. A refined understanding of how symptoms and their networks evolve over time can enhance the efficacy of treatments and support mechanisms, by ensuring that they meet the changing emotional, psychological, and physiological needs of mothers with postpartum depression and bonding difficulties. Moreover, in reflecting upon the broader context of our study, it is important to consider the potential influence of the COVID-19 pandemic. The exposure to the pandemic, and its associated psychological stressors such as increased fear of the virus and feelings of loneliness25,64, may have disproportionately affected participants in the latter periods of the study. Those with longer exposure to the pandemic could have experienced heightened symptoms, confounding the interpretation of the temporal progression of postpartum depression and MIBD symptoms. This may partially explain our finding that symptoms overall increased over the postpartum period.
Although it is commonly believed that postpartum depressive symptoms diminish over time, recent evidence suggests a more complex trajectory. Parenting stress often rises during the first year due to the infant’s rapid developmental changes and increased activities, such as heightened mobility and emerging social behaviors65. These developmental milestones demand more attention and energy from parents, which potentially lead to elevated stress levels. Furthermore, as infants grow and especially after they turn one year old—the official maternity leave period in Japan as determined by law—, many mothers return to work and face the added challenge of balancing professional responsibilities with family care. This dual burden can result in increased workload and fewer opportunities for self-care, both of which contribute to heightened mental health issues66. These findings align with a recent meta-analysis showing that marital satisfaction typically declines from pregnancy to 12 months postpartum, with a further decrease observed at 24 months postpartum67. Such stressors can amplify the risk of persistent or worsening depressive symptoms and difficulties in mother-infant bonding. Future research should consider longitudinal designs to elucidate the causal relationships between symptoms and clarify their evolving trajectories, while also taking into account external factors such as global health crises.
Conclusions
Our study contributes to a more comprehensive understanding of the coexistence of postpartum depression and MIBD, adding to the broader evidence on shared risk factors and the bidirectional influence of these conditions. It underscores the need for an integrated, multifaceted approach to intervention, reflecting the complex, interconnected nature of maternal mental health challenges and their impact on the mother-infant relationship.
Data availability
The data analyzed in this study, as well as the numerical data underlying plots in the manuscript, are available on https://osf.io/bc37e/. In accordance with the institutional ethical approval, to reuse the data, a formal application must be submitted to Dr Takahiro Tabuchi, tabuchitak@gmail.com.
Code availability
The code for this study is available on https://osf.io/bc37e/.
References
Brockington, I., Aucamp, H. M. & Fraser, C. Severe disorders of the mother-infant relationship: Definitions, frequency, and treatment. Br. J. Psychiatry 189, 477–479 (2006).
O’Hara, M. W. & McCabe, J. E. Postpartum depression: Current status and future directions. Annu. Rev. Clin. Psychol. 9, 379–407 (2013).
Hahn-Holbrook, J., Cornwell-Hinrichs, T. & Anaya, I. Economic and health predictors of national postpartum depression prevalence: a systematic review, meta-analysis, and meta-regression of 291 studies from 56 countries. Front. Psychiatry 8, 301051 (2018).
Shorey, S. et al. Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. J. Psychiatr. Res. 104, 235–248 (2018).
Liu, X., Wang, S. & Wang, G. Prevalence and risk factors of postpartum depression in women: a systematic review and meta‐analysis. J. Clin. Nurs. 31, 2665–2677 (2022).
Pariente, G. et al. Risk for probable post-partum depression among women during the COVID-19 pandemic. Arch. Women’s. Ment. Health 23, 767–773 (2020).
Chen, Q., Li, W., Xiong, J. & Zheng, X. Prevalence and risk factors associated with postpartum depression during the COVID-19 pandemic: a literature review and meta-analysis. Int. J. Environ. Res. public health 19, 2219 (2022).
Safi‐Keykaleh, M. et al. Prevalence of postpartum depression in women amid the COVID‐19 pandemic: a systematic review and meta‐analysis. Int. J. Gynecol. Obstet. 157, 240–247 (2022).
Edhborg, M., Nasreen, H. E. & Kabir, Z. N. Impact of postpartum depressive and anxiety symptoms on mothers’ emotional tie to their infants 2–3 months postpartum: a population-based study from rural Bangladesh. Arch. Womens. Ment. health 14, 307–316 (2011).
Matsunaga, A., Takauma, F., Tada, K. & Kitamura, T. Discrete category of mother-to-infant bonding disorder and its identification by the Mother-to-Infant Bonding Scale: A study in Japanese mothers of a 1-month-old. Early Hum. Dev. 111, 1–5 (2017).
Chen, C., Okawa, S., Okubo, R., Nakagawa, S. & Tabuchi, T. Risk factors for persistent versus episodic mother-to-infant bonding difficulties in postpartum women in a nationwide Japanese longitudinal study. J. Affect. Disord. 349, 370–376 (2024).
Slomian, J., Honvo, G., Emonts, P., Reginster, J. Y., & Bruyère, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Womens Health 15, 1745506519844044 (2019).
Le Bas, G. A. et al. The role of antenatal and postnatal maternal bonding in infant development: A systematic review and meta‐analysis. Soc. Dev. 29, 3–20 (2020).
Rogers, A. et al. Association between maternal perinatal depression and anxiety and child and adolescent development: a meta-analysis. JAMA Pediatrics 174, 1082–1092 (2020).
Murakami, K. et al. Maternal postnatal bonding disorder and developmental delays in children: the Tohoku Medical Megabank Project Birth and Three-Generation Cohort Study. Arch. Womens. Ment. Health 26, 219–226 (2023).
Gilden, J. et al. Mother-to-infant bonding in women with postpartum psychosis and severe postpartum depression: a clinical cohort study. J. Clin. Med. 9, 2291 (2020).
O’Dea, G. A., et al. Associations between maternal psychological distress and mother-infant bonding: a systematic review and meta-analysis. Arch. Womens Mental Health, 26, 441–452 (2023)
Høivik, M. S., Burkeland, N. A., Linaker, O. M. & Berg‐Nielsen, T. S. The Mother and Baby Interaction Scale: a valid broadband instrument for efficient screening of postpartum interaction? A preliminary validation in a Norwegian community sample. Scand. J. Caring Sci. 27, 733–739 (2013).
Edwards, L. M., Le, H. N. & Garnier-Villarreal, M. A systematic review and meta-analysis of risk factors for postpartum depression among Latinas. Matern. Child Health J. 25, 554–564 (2021).
Chen, C., Okawa, S., Okubo, R., Nakagawa, S. & Tabuchi, T. Risk factors for mother-to-infant bonding difficulties and maternal anger/rejection towards the infant in a Japanese longitudinal study. Asian J. Psychiatry 89, 103778 (2023).
Chen, C. et al. Broad impact of adverse childhood experiences on postpartum maternal mental health, child-rearing behaviors, and child development in Japan. Psychiatry Clin. Neurosci. 77, 569–571 (2023).
Moehler, E., Brunner, R., Wiebel, A., Reck, C. & Resch, F. Maternal depressive symptoms in the postnatal period are associated with long-term impairment of mother-child bonding. Arch. Womens. Ment. Health 9, 273–278 (2006).
Doyle, F. L. et al. Towards preventative psychiatry: concurrent and longitudinal predictors of postnatal maternal-infant bonding. Child Psychiatry Hum. Dev. 54, 1723–1736 (2023).
Chen, C., et al Postpartum loneliness predicts future depressive symptoms: a nationwide Japanese longitudinal study. Arch. Womens Mental Health, 27, 447–457 (2024)
Chen, C. et al. Mother-to-infant bonding difficulties are associated with future maternal depression and child-maltreatment behaviors: A Japanese nationwide longitudinal study. Psychiatry Res. 334, 115814 (2024).
Hiraoka, D., Kawanami, A., Sakurai, K., & Mori, C. Within-individual relationships between mother-to-infant bonding and postpartum depressive symptoms: a longitudinal study. Psychological Med. 54, 1749–1757 (2024)
Höflich, A., Kautzky, A., Slamanig, R., Kampshoff, J. & Unger, A. Depressive symptoms as a transdiagnostic mediator of mother-to-infant bonding: Results from a psychiatric mother-baby unit. J. Psychiatr. Res. 149, 37–43 (2022).
Loh, A. H. Y., Ong, L. L., Yong, F. S. H. & Chen, H. Y. Improving mother-infant bonding in postnatal depression− The SURE MUMS study. Asian J. Psychiatry 81, 103457 (2023).
Shieh, P. L., Cheng, L. Y., Hsu, W. S., & Li, R. H. Mother-Infant Group Intervention on Maternal Depression and Bonding: A Quasi-Experimental Study. Maternal Child Health J. 27, 1114–1125 (2023).
Cramer, A. O., Waldorp, L. J., Van Der Maas, H. L. & Borsboom, D. Comorbidity: A network perspective. Behav. Brain Sci. 33, 137–150 (2010).
Borsboom, D. & Cramer, A. O. J. Network analysis: An integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 9, 91–121 (2013).
Schmittmann, V. D. et al. Deconstructing the construct: A network perspective on psychological phenomena. N. Ideas Psychol. 31, 43–53 (2013).
Jones, P. J., Ma, R. & McNally, R. J. Bridge centrality: A network approach to understanding comorbidity. Multivar. Behav. Res. 56, 353–367 (2021).
World Health Organization. Guide for integration of perinatal mental health in maternal and child health services (World Health Organization, 2022).
Altmann, T. R., Hill, D. L., & American Academy of Pediatrics. Caring for your baby and young child: birth to age 5 (American Academy of Pediatrics, 2019).
The Japan Society of Obstetrics and Gynecology. Manual For Maternal Mental Health Care, Revised. Chugai-Igakusha, Tokyo (The Japan Society of Obstetrics and Gynecology, 2021).
Goodman, J. H. Postpartum depression beyond the early postpartum period. J. Obstet. Gynecologic Neonatal Nurs. 33, 410–420 (2004).
Cox, J. L., Holden, J. M. & Sagovsky, R. Detection of postnatal depression. Development of the 10‐item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 150, 782–786 (1987).
Okano, T. Validation and reliability of a Japanese version of the EPDS. Arch. Psychiatr. Diagnosis Clin. Evaluation 7, 525–533 (1996).
Yamashita, H., Yoshida, K., Nakano, H. & Tashiro, N. Postnatal depression in Japanese women: detecting the early onset of postnatal depression by closely monitoring the postpartum mood. J. Affect. Disord. 58, 145–154 (2000).
Taylor, A., Atkins, R., Kumar, R., Adams, D. & Glover, V. A new Mother-to-Infant Bonding Scale: links with early maternal mood. Arch. Womens. Ment. Health 8, 45–51 (2005).
Yoshida, K., Yamashita, H., Conroy, S., Marks, M. & Kumar, C. A Japanese version of Mother-to-Infant Bonding Scale: factor structure, longitudinal changes and links with maternal mood during the early postnatal period in Japanese mothers. Arch. Womens. Ment. Health 15, 343–352 (2012).
Chen, C. et al. Determining the optimal cutoff point for the Japanese Mother-to-Infant Bonding Scale: A data-driven approach. Asian J. Psychiatry 91, 103874 (2023).
Epskamp, S., Cramer, A. O., Waldorp, L. J., Schmittmann, V. D. & Borsboom, D. qgraph: Network visualizations of relationships in psychometric data. J. Stat. Softw. 48, 1–18 (2012).
Epskamp, S., Borsboom, D. & Fried, E. I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 50, 195–212 (2018).
Friedman, J., Hastie, R., & Tibshirani, R. glasso: Graphical lasso estimation of Gaussian graphical models. R package version 1.11. Retrieved from https://cran.r-project.org/packages/glasso (2019).
Foygel, R., & Drton, M. Extended Bayesian information criteria for Gaussian graphical models. In Advances in neural information processing systems, 23 (NIPS, 2010)
Haslbeck, J. & Waldorp, L. J. mgm: Estimating time-varying mixed graphical models in high-dimensional data. J. Stat. Softw. 93, 1–46 (2020).
Cai, H. et al. Network analysis of depressive and anxiety symptoms in adolescents during the later stage of the COVID-19 pandemic. Transl. Psychiatry 12, 98 (2022).
Jin, Y. et al. Network analysis of comorbid depression and anxiety and their associations with quality of life among clinicians in public hospitals during the late stage of the COVID-19 pandemic in China. J. Affect. Disord. 314, 193–200 (2022).
Arthur, D. & Vassilvitskii, S. K-means++: The Advantages of Careful Seeding. In SODA ‘07: Proceedings of the Eighteenth Annual ACM-SIAM Symposium on Discrete Algorithms, pp. 1027–1035 (ACM, 2007).
Thomason, E. et al. Parenting stress and depressive symptoms in postpartum mothers: Bidirectional or unidirectional effects? Infant Behav. Dev. 37, 406–415 (2014).
Louie, A. D., Cromer, L. D. & Berry, J. O. Assessing parenting stress: Review of the use and interpretation of the parental stress scale. Fam. J. 25, 359–367 (2017).
Lévesque, S., Bisson, V., Charton, L. & Fernet, M. Parenting and relational well-being during the transition to parenthood: Challenges for first-time parents. J. Child Fam. Stud. 29, 1938–1956 (2020).
Nomaguchi, K. & Milkie, M. A. Parenthood and well‐being: A decade in review. J. Marriage Fam. 82, 198–223 (2020).
Holt, C., Gentilleau, C., Gemmill, A. W. & Milgrom, J. Improving the mother-infant relationship following postnatal depression: a randomised controlled trial of a brief intervention (HUGS). Arch. Womens. Ment. Health 24, 913–923 (2021).
Sangsawang, B., Deoisres, W., Hengudomsub, P. & Sangsawang, N. Effectiveness of psychosocial support provided by midwives and family on preventing postpartum depression among first‐time adolescent mothers at 3‐month follow‐up: A randomised controlled trial. J. Clin. Nurs. 31, 689–702 (2022).
Kalmbach, D. A. et al. Mother-to-infant bonding is associated with maternal insomnia, snoring, cognitive arousal, and infant sleep problems and colic. Behav. Sleep. Med. 20, 393–409 (2022).
Reid, H. E., Pratt, D., Edge, D. & Wittkowski, A. Maternal suicide ideation and behaviour during pregnancy and the first postpartum year: a systematic review of psychological and psychosocial risk factors. Front. Psychiatry 13, 349 (2022).
Brown, S. A., Williams, K. & Collins, A. Past and recent deliberate self‐harm: Emotion and coping strategy differences. J. Clin. Psychol. 63, 791–803 (2007).
Paris, R., Bolton, R. E. & Weinberg, M. K. Postpartum depression, suicidality, and mother-infant interactions. Arch. Womens. Ment. Health 12, 309–321 (2009).
Doucet, S. & Letourneau, N. Coping and suicidal ideations in women with symptoms of postpartum depression. Clin. Med. Reprod. health 3, CMRH–S3801 (2009).
Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. Cognitive therapy of depression (Guilford Press, 1979).
Ernst, M. et al. Loneliness before and during the COVID-19 pandemic: A systematic review with meta-analysis. Am. Psychologist 77, 660 (2022).
Golfenshtein, N., Hanlon, A. L., Deatrick, J. A. & Medoff-Cooper, B. Maternal parenting stress changes over the first year of life in infants with complex cardiac defects and in healthy infants. Cardiol. Young. 32, 383–389 (2022).
Dagher, R. K., McGovern, P. M., Dowd, B. E. & Lundberg, U. Postpartum depressive symptoms and the combined load of paid and unpaid work: a longitudinal analysis. Int. Arch. Occup. Environ. Health 84, 735–743 (2011).
Bogdan, I., Turliuc, M. N. & Candel, O. S. Transition to Parenthood and Marital Satisfaction: A Meta-Analysis. Front. Psychol. 13, 901362 (2022).
Acknowledgements
This study was supported by the Japan Society for the Promotion of Science KAKENHI Grants [grant numbers JP 21H04856]; the Japan Science and Technology Agency [grant number JPMJSC21U6]; Intramural fund of the National Institute for Environmental Studies; Innovative Research Program on Suicide Countermeasures [grant number: R3-2-2]; and Ready for COVID-19 Relief Fund [grant number: 5th period 2nd term 001]. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Investigation: R.O., S.O., T.T.; Data analysis: N.H., C.C.; Manuscript preparation: N.H., C.C.; Manuscript revision: N.H., C.C., S.O., R.O., T.M., S.N., T.T.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications psychology thanks Susanne Schweizer and Desiree Phua for their contribution to the peer review of this work. Primary Handling Editors: Inti Brazil and Jennifer Bellingtier. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Harasawa, N., Chen, C., Okawa, S. et al. A network analysis of postpartum depression and mother-to-infant bonding shows common and unique symptom-level connections across three postpartum periods. Commun Psychol 3, 7 (2025). https://doi.org/10.1038/s44271-024-00171-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44271-024-00171-9